A Patient's Guide to: Medication Approach to Chronic Pain

Introduction
Pain is the most common reason for visiting a doctor. Treatment for pain consists of non-drug therapy and drug therapy. Examples of the non-drug therapies are physical therapy, relaxation exercises, injections, and massage. Most patients with chronic pain will need to use both non-drug and drug therapies to get the best pain relief possible.
This guide will help you understand
- how healthcare providers choose medications
- how pain affects the decision
- what is polypharmacy
- what are the possible medication side effects
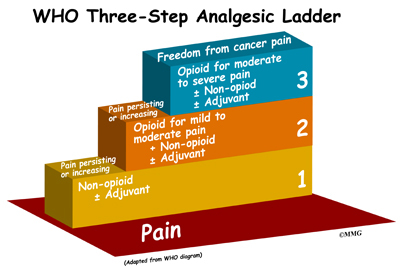
Analgesic Ladder
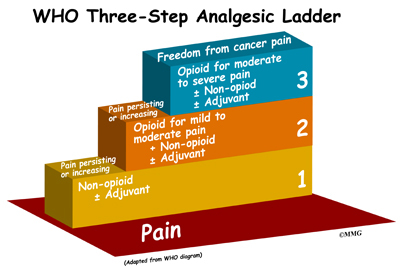
The World Health Organization (WHO) developed the analgesic ladder. It is designed to help healthcare providers manage cancer pain with medications in a systematic way.
Step 1 of the Analgesic Ladder
The WHO recommends a non-opioid (non-narcotic) medication as the first step. This can be given with an adjuvant medication. Adjuvants are medications that can give additive pain control when used with the primary pain medication. Common adjuvants include certain antidepressants, antiepileptics, and topical medications.
Non-opioid pain medications include acetaminophen (Tylenol®) and the non-steroidal antiinflammatory drugs (NSAIDs). NSAIDs include drugs such as aspirin, ibuprofen (Advil®, Motrin®) naproxen (Aleve®), Naprosyn®), piroxicam (Feldene®), meloxicam (Mobic®), celecoxib (Celebrex®), and many others.
Step 2 of the Analgesic Ladder
If pain is not controlled with a Step 1 medication, then one should proceed to Step 2. This would be adding or changing the medication to include a weak opioid. Weak opioids include the drugs such as hydrocodone or oxycodone with acetaminophen, ibuprofen, or aspirin. Common brand names are Lortab®, Vicodin®, Vicoprofen®, Bancap HC, Percocet®, and Percodan®.
Step 3 of the Analgesic Ladder
If the weak opioid is not enough, then a strong opioid should be tried. Examples of strong opioids are morphine (Kadian®, MS Contin®, Avinza®), oxycodone (OxyContin®), fentanyl (Duragesic® patches), oxymorphone (Opana®), and methadone (Dolophine®.)
Problems with the WHO Analgesic Ladder
The WHO analgesic ladder has been a helpful guide to slowly step patients up as they need stronger medications. There has been some debate over where some medications fit on the ladder.
Tramadol (Ultram®)
Tramadol is a synthetic analogue of the opioid codeine. The Drug Enforcement Agency (DEA) did not classify it as a controlled substance. This means that some see it as a Step 1 non-opioid drug. Others view it as a Step 2 opioid drug. It can be helpful for mild or moderate pain. It is one of the few medications that show benefit in patients with fibromyalgia.
The term weak opioid is a confusing term. Combining a low dose of an opioid with acetaminophen, ibuprofen, or aspirin, improves efficacy (gives the desired effect). Adding hydrocodone and oxycodone to other substances make them weak opioids. This is because there are dose limits to these products. The dose of the combined product is not limited by the opioid. It is limited by the non-opioid component. Exceeding the daily-recommended dose greatly increases the risk of dangerous side effects from the non-opioid component. Hydrocodone and oxycodone are low dose strong opioids without the added acetaminophen, ibuprofen, or aspirin.
At first propoxyphene (Darvon®, Darvocet®, Balacet®) was called a Step 2 weak opioid on the analgesic ladder. However, it is no longer recommended for use in chronic pain. The potential side effects of this drug outweigh the benefits. It gives little pain relief and can cause serious heart and lung problems when taken for long periods of time.
Just because medications are listed as Step 1 or Step 2 does not mean that they are safer medications than Step 3 medications. All medications have risks. The risks, or side effects, need to be balanced with their possible benefit. In chronic pain, the benefit you hope to get is pain control.
Side Effects of Non-opioid (Step 1) Medications
Acetaminophen
Excessive doses of acetaminophen can cause liver failure. Accidental overdose is the most common reason for liver transplants. In healthy individuals the daily dose limit is 4,000 mg per day (8 extra-strength 500 mg tablets or 12 regular strength 325 mg tablets.) The dose limit for patients with a history of liver problems or a history of alcoholism (or heavy drinking) is 2,000 mg per day. This includes acetaminophen from all sources. You must read the labels very carefully. Acetaminophen is often included in other medications such as cold, flu, and sinus preparations.
Ibuprofen and Aspirin (NSAIDs)
Ibuprofen and aspirin belong to the NSAID (non-steroidal antiinflammatory) group. The recommended dose limit for ibuprofen is 3,200 mg daily in healthy adults. This is about 16 of the over-the-counter 200 mg tablets per day. For aspirin, the daily recommend dose is 4,000 mg per day. The problem with all NSAIDs, not just ibuprofen and aspirin, is that major side effects can occur at doses lower than the recommended daily limit. The most concerning side effects are stomach ulcers, kidney failure, and making congestive heart failure worse. The side effects are related not only to the dose but also to the length of time you take the medication. Long-term use of any NSAID can increase the risk of heart attacks and strokes.
Side Effects with Opioids (Step 2 & 3) Medications
Although opioids do not cause liver or kidney damage, they have their own unique set of possible problems.
Common Side Effects
The most common side effects of all opioids are constipation, nausea, vomiting, and drowsiness. Rash, itch and mood changes can also occur. None of these side effects are allergies. Except for constipation, all of these side effects are expected to go away over five to seven days. This works best if the opioid is started at a low dose and your body is allowed to adjust to it. Most patients need to take a daily laxative to prevent constipation. You must do so for as long as you are on an opiate.
Sleep Disorders
Inadequate sleep increases the intensity of pain and decreases your ability to cope with pain. Pain can cause sleep disorders. Anxiety, depression, and fibromyalgia are also linked with sleep disorders. And opioid pain medications can cause sleep disorders. The most common disorders associated with opioids are sleep apnea and altered sleep patterns.
Sleep apnea is a condition in which you stop breathing during the night. The symptoms are loud snoring, gasping, and snorting while sleeping. Daytime drowsiness, fatigue, and/or falling asleep easily such as when driving a car or reading can occur. Opioids can make sleep apnea worse even to the point of causing death. If you think you may have sleep apnea, be sure to discuss it with your healthcare provider. If you have sleep apnea, you will need to treat it before starting an opioid medication.
Opioids can change sleep patterns. Even though you could be getting the same amount of sleep, it may not be restful sleep. While tiredness the first few days on an opioid is common, it should go away quickly. If you find that you are still tired, it is likely that the medication is altering your normal sleep pattern. Changing the medication should improve sleep. It can also improve pain management and your ability to cope with the pain.
Mood Changes
Opioids can cause mood changes. Some patients feel dysphoric (unhappy or sad) or in a worse mood. The biggest problem with opioids is that they can cause euphoria (intense happiness) or improve mood. Some patients describe this as getting energy from the medication. This would be great if this energy high didn’t go away after one to three weeks. Many patients think that euphoria is the same thing as pain relief. Once the euphoria wears off, it’s easy to think the opioid isn’t working any more. This is what causes people to start increasing doses. It takes more drugs over time to get the same change in mood.
Addiction
Addiction is defined by craving, uncontrolled, or compulsive use of a drug. and using it even though it causes harm. Addiction is a complex chronic disease. Simply taking an opioid does not cause addiction. If you have no risk factors, it is rare to develop the disease of addiction. However, if you have the right (or wrong) genetics and psychological and social stressors, addiction can occur.
There is no test for addiction. Addiction reveals itself by aberrant (abnormal) behaviors over time. Your healthcare provider looks for any of the following as a sign of a developing problem
- reporting that prescriptions have been lost or stolen
- asking for early refills
- not following medication directions
- taking extra medication without being told to
- increasing the dose without approval
- obtaining medications from multiple healthcare providers
- wanting to continue a medication despite major side effects
- wanting to continue a medication despite worse function
- using a drug for a reason other than it was prescribed (such as using a pain medication to calm down after a heated argument)
Physical Dependence
Physical dependence occurs when your body becomes used to a medication. Stopping the medication suddenly causes withdrawal symptoms. Withdrawal can occur with many medications including antidepressants and blood pressure medications. Physical dependence is not addiction. Physical dependence can occur in anyone on a regular dose of an opioid for more than one or two weeks. Withdrawal from an opioid can be mild or severe. Symptoms can range from mild irritability to sweating, diarrhea, vomiting and muscle cramps. You may feel like you have a severe case of the flu. Withdrawal may be miserable but it is not life threatening. It can always be avoided. Slowly decrease the medication over several days to several weeks. Let your body readjust to the lower dose.
Pseudo-addiction
Pseudo-addiction is the term used to describe what looks like dangerous or aberrant behavior but occurs when pain is not adequately treated. For example: you are prescribed a pain medication and told that you can only take two tablets per day. You have constant pain all day and night. The pain medication that you are prescribed works and allows you to be active but it only relieves pain for four hours. You are only allowed two tablets per day. How would you respond? Some people take more medication than is prescribed. They run out early. Others complain bitterly at every appointment. They demand more medication, and appear to be drug seeking. Some may go to more than one physician to get what they think they need to relieve the pain. Under-treatment of pain can cause this type of behavior. An increase in the dose stops the behavior.
Therapeutic Trial
It would be wonderful if your healthcare provider could pick the right drug at the right dose at your first appointment. This doesn’t happen very often. Everyone responds differently to different drugs. Pain will respond to some drugs in some people and not in other people. In some people, the pain responds, but they get side effects. Others don’t have any side effects. It really becomes a process of trial and error. It can take several visits and perhaps several trials of different drugs for you to get enough pain relief with side effects you can handle. It is not uncommon to feel like a guinea pig. Don’t give up. Keep telling your healthcare provider how the medication is working for you.
Polypharmacy
It would also be wonderful if one drug worked well. However, most patients with chronic pain will not get enough pain relief from a single medication. Using two or more medications that complement each other is called polypharmacy. The drugs have different mechanisms of action and can give better pain relief. As the WHO Analgesic Ladder suggests, pain specialists often combine opioid medications with other adjuvant medications. The goal is order to treat chronic pain adequately. The most common adjuvants are the following
- Antidepressants: The two groups that are used in pain management are the serotonin norepinephrine reuptake inhibitors (SNRIs) and the tricyclic antidepressants (TCAs). The SNRIs are duloxetine (Cymbalta®) and venlafaxine (Effexor®). The commonly used TCAs include amitriptyline (Elavil®), nortriptyline (Pamelor®), and desipramine (Norpramin®).
- Antiepileptics (anticonvulsants): These drugs are used to treat epilepsy and stabilize mood. They also work well treating nerve pain. Some of the antiepileptics commonly used in pain management are gabapentin (Neurontin®), pregabalin (Lyrica®), carbamazepine (Tegretol®), topiramate (Topamax®), levetiracetam (Keppra®), and lamotrigine (Lamictal®).
- Topicals: Capsaicin ointment and lidocaine patches are some of the medications that can be effective when applied to the skin.
Choosing the Right Medication
How do doctors choose the right medication?
There are many things to consider when choosing the right drug(s) for patients. Patient safety and ability to tolerate the drug come first. Efficacy (how well the medication works for the condition being treated) is also important. Affordability and ease of use (such as how many pills need to be taken daily) are important factors, too.
It may not be possible to use only one medication. But it is still best to treat with the fewest medications possible. Most chronic pain patients also suffer from depression, anxiety, and sleep disorders. It may be possible to pick a medication that not only helps with pain but could also help with the other problems.
Classifications of Pain
Pain can be defined by the underlying mechanism. It can be classified as either nociceptive pain or neuropathic pain. Nociceptive means unpleasant pain. It occurs when the nervous system is working as it should. Pain is a signal that something is wrong. Pain is caused by a stimulus such as injury, infection, or inflammation. The pain signal is sent to your spinal cord and then to your brain. Your brain then interprets the pain and acts on it. Your brain can release substances such as your own natural opioid-like endorphins to calm the initial pain signal down and help you deal with it. The pain intensity is usually related to the degree of injury and amount of actual tissue damage. Nociceptive pain generally responds to opioid medications, NSAIDs, and acetaminophen.
Neuropathic pain is caused by a nervous system that isn’t working right. Think of it as irritable nerve cells that react for no reason. The pain can arise from the central nervous system (spinal cord or brain) or from the peripheral nervous system such as in the legs, arms, skin, and so on. Insults such as trauma, inflammation, or diseases such as shingles, diabetes, and HIV can cause it. Neuropathic pain can be constant or episodic(comes and goes). It is often described as burning, streaking, lightening, tingling, or pins and needles.
Neuropathic pain serves no known purpose. It is not related to the degree of injury or disease. Neuropathic pain is meaningless outside the amount of suffering it causes. It is usually more difficult to treat than nociceptive pain. Most often more than one drug is needed to control neuropathic pain. Opioids aren’t as effective for this type of pain as they are for nociceptive pain. The drugs that are considered first-line choices are the antiepileptics and the antidepressants listed in the previous section.
Controversies About Opiate Treatment of Nonmalignant Chronic Pain
Acute pain lasts a short time. This is the kind of pain you may have after breaking a leg or after surgery. Acute pain goes away as the injury heals. Chronic pain is pain that lasts longer than expected after an injury. Cancer pain can be both acute and chronic. With both acute and chronic cancer pain, there is an expectation that the pain will go away sooner or later. As the injury heals or the cancer is cured (or the patient dies) there is an expectation of an end to the pain. Chronic nonmalignant (or non-cancer) pain is different. The pain can result from an acute injury that lasts beyond the healing or simply appears without a known reason. A few examples are diabetic neuropathy, post-herpetic neuralgia (shingles), low back pain, and fibromyalgia. Patients can have these painful syndromes for decades.
It is acceptable to treat severe acute and cancer pain with opioid medications. However there is debate about treating chronic nonmalignant pain (CNP) with opioids. All medications carry risks. The hoped for benefit of a medication must outweigh the possible risk. Opioids have great risk for abuse and addiction, especially when used for long periods of time. Because of these risks, opioids are only used in CNP after other appropriate medications and non-medication therapies have failed. Most experts consider opioids as the treatment of last resort for CNP.
Risk-Benefit Analysis of Opiates and Sedatives
The biggest risks of taking opiates and sedatives are addiction and death. The overall risk of substance abuse in the general population is around 10%. Your specific risk depends on your own risk factors. If you have no history of addiction and no significant history of mental health problems, then you have a low risk of addiction. If you have a history of addiction or substance abuse, then you are at greater risk for addiction. But if you are in remission and have good support systems, you may still do well on opioids. You are at high risk for abusing an opioid or sedative medication if you are actively abusing alcohol and other substances. Untreated mental health issues and poor support systems add to your risk.
There are ways to decrease the risk of addiction or substance abuse. Diagnosing and successfully treating any mood disorder reduces the risk. The most common mood disorders include depression and anxiety. Avoiding short acting opioids reduces the risk of addiction or abuse. Long acting opioids are safer as they are less likely to feed into the changes in mood that fuel substance abuse. The long acting opioid, methadone is considered the safest of the opioids. It causes little to no mood alteration. Long-acting morphine is usually the second choice.
Opioids cause death by stopping the body’s drive to breathe. This can happen as an intentional overdose such as in suicide. It can also be the result of an accidental overdose when an addict tries to get high. Combining an opioid with another substance such as alcohol also decreases the desire to breathe, or makes sleep apnea worse. Death can be avoided. Don’t take extra medication without approval from your healthcare provider. Let your healthcare provider know about all other medications and drugs you take including alcohol. Finding out if you have sleep apnea and treating it is also important in preventing death.
The benefit of these medications is better function and improved quality of life. If, after weighing your specific risks, you and your healthcare provider decide that the possible benefit is greater than the potential risk, then a medication trial is indicated.
Careful monitoring of your response to a medication trial is essential. Risky behavior or serious side effects can be caught early. Preventing and solving problems before there is a bad outcome is important.
Hyperalgesia
Hyperalgesia is described as an extreme sensitivity to what is normally not painful such as a simple touch. This comes from nerves sending pain messages of increasing frequency and intensity to your brain. It can be from the same area that was previously hurt. Or it can expand beyond the initial painful area. Opioids can cause hyperalgesia. If you feel more pain after starting or increasing an opioid, you may be experiencing hyperalgesia. If hyperalgesia develops, stopping the opioid will improve pain control. Other treatment options can then be explored.
Detoxification
Detoxification (detox) is letting your body get back to its natural state without any pain medications in it. There are several reasons you might want to detox. One reason is hyperalgesia. Another reason is if you are on several medications and you aren’t sure if they are helping or not. Or you might be having a side effect and you aren’t sure which drug is causing it. By slowly going off one drug at a time, you can find out if the medication was helping or not. Likewise, you’ll see if it was causing any side effects. If the pain is worse when you’re off the drug, it can be restarted. It is surprising how many patients feel better after stopping many of their drugs.
Some experts believe that your body stops making its own natural painkillers (endorphins) when it is given artificial ones. Stopping the medications for one or two months lets your body rest and reset its own natural response.
Opiate rotation
Opiate rotation is changing from one opioid to another. Opiate rotation is used when tolerance to the pain relief develops after several dose increases. If this happens to you, be sure to explore all the possible reasons for the medications no longer working as well. One reason for medications not working as well is if the there is a new injury or the underlying disease is getting worse. An example is a new compression fracture in someone with low back pain and osteoporosis. Once that is ruled out, keep in mind anything that makes you feel worse such as worsening depression, increasing anxiety, or stresses at home will make pain feel more intense. The best treatment is to treat the underlying problem.
Once those issues are sorted out, it may be a good idea to switch from one opiate to another. Changing to a different pain medication can result in better pain control at a lower comparative dose and help keep opioid creep (when the dose of the opioid keeps slowly but relentlessly
increasing over time) under control.
Opiate Holiday
Similar to detoxification, giving you a holiday from opiates for four to eight weeks can be a good idea. It helps reset your body’s natural ability to cope with pain. And it can help you decide if you even still need the medication. A drug holiday can also reduce tolerance and allow you to restart the medication at a lower dose.
Some surgeons are reluctant to operate on patients taking high doses of opiates. Patients on high doses cope less well with surgical pain and recover more slowly after surgery. Tapering off the medications three weeks before surgery can be a good idea for two reasons. First, you may respond better to lower doses of the pain medication. And second, the surgery may give you significant relief so that you no longer need such a high dose anymore.
Summary
Chronic pain management is a complex process. Most chronic pain patients have both neuropathic and nociceptive pain, along with depression, anxiety, and sleep disorders. Chronic pain can also cause social stresses such as the loss of a job or contribute to the failure of a marriage. When constant pain is combined with these types of stresses, the overall suffering becomes much larger than just the physical pain. It can be a vicious circle as these stresses make the physical pain seem stronger.
The risks associated with the medications used to treat pain also increase the complexity of the problem. However, with careful drug selection and close monitoring, it is possible to decrease pain, increase function, improve quality of life, and decrease the suffering associated with chronic pain.
|