A Patient’s Guide to Unicompartmental Knee Replacement
Introduction
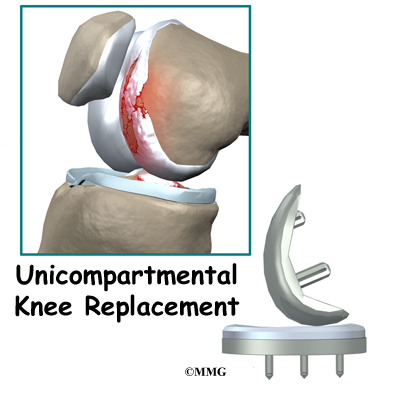
A painful knee can severely affect your ability to lead a full, active life. Over the last 25 years, major advancements in artificial knee replacement have improved the outcome of the surgery greatly. One of the more recent advances in knee replacement surgery is the unicompartmental knee replacement (also known as a unicondylar knee replacement). This type of knee replacement is less invasive than a full knee replacement. The operation is designed to replace only the portions of the joint that are most damaged by arthritis. This can have significant advantages, especially in younger patients who may need to have a second artificial knee replacement as the first one begins to wear out. Removing less bone during the initial operation makes it much easier to perform a revision artificial knee replacement later in life.
This guide will help you understand:
- what your surgeon hopes to achieve
- what happens during the procedure
- what to expect after your operation
Anatomy
What is the normal anatomy of the knee?
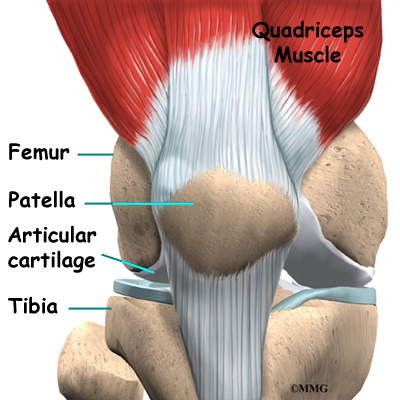
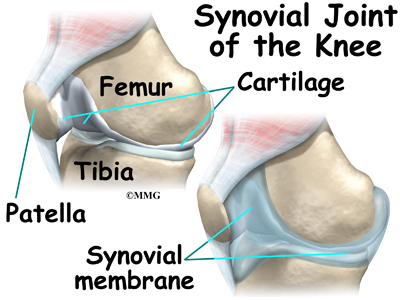
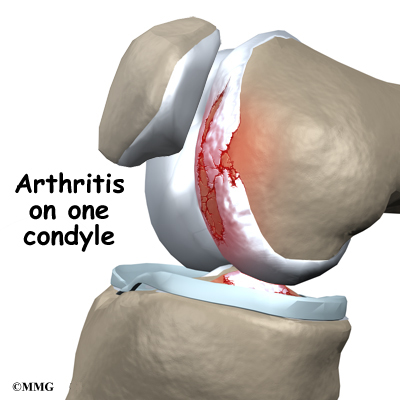
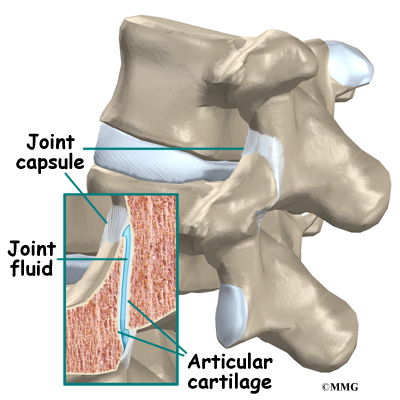
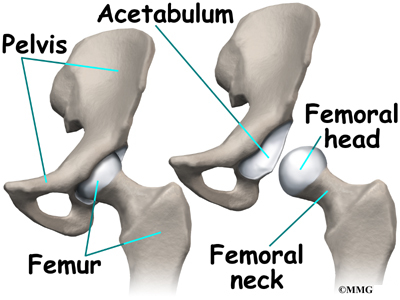
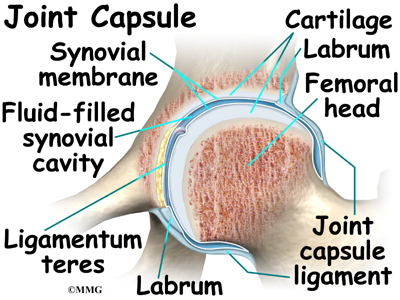
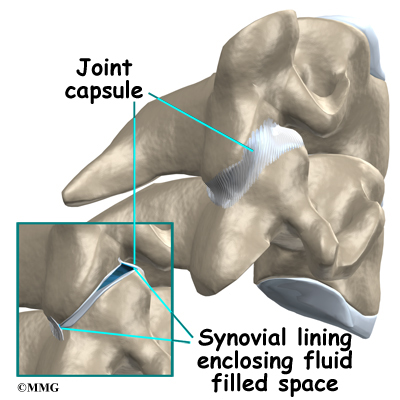
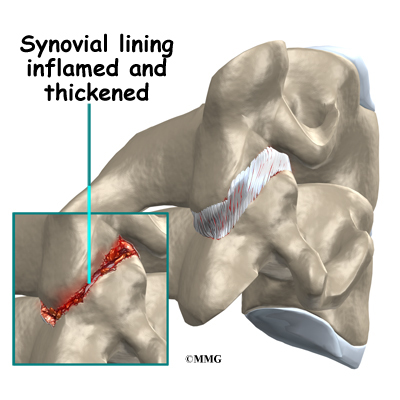
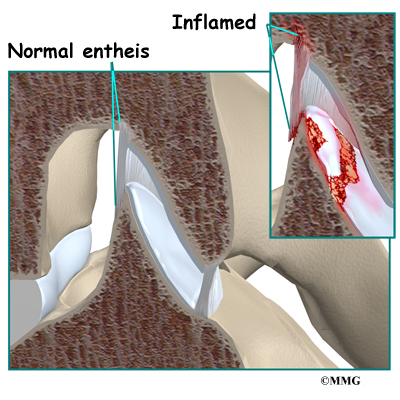
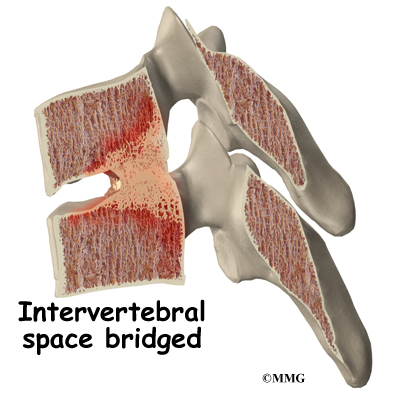
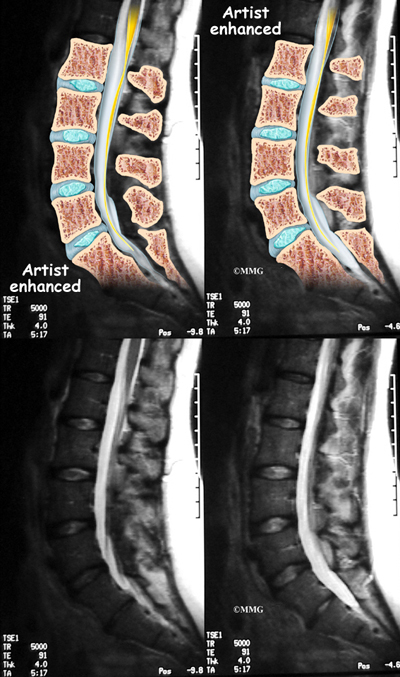
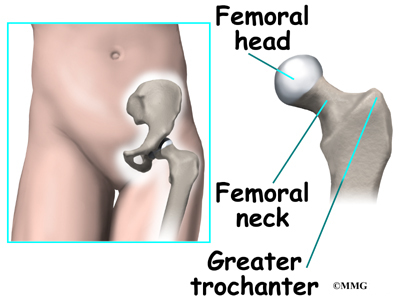
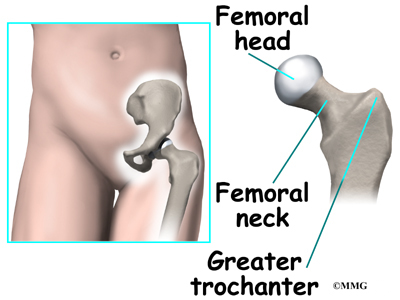
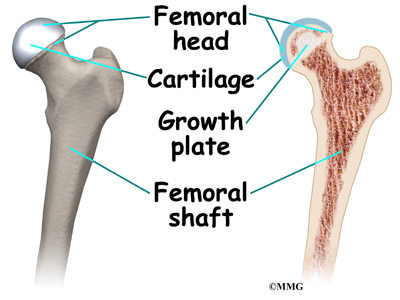
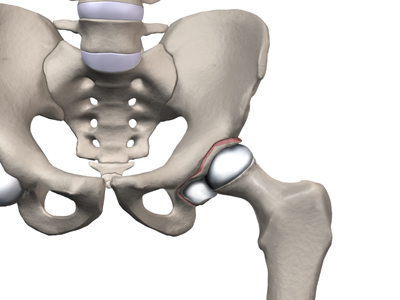
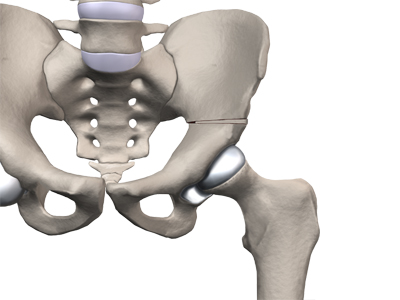
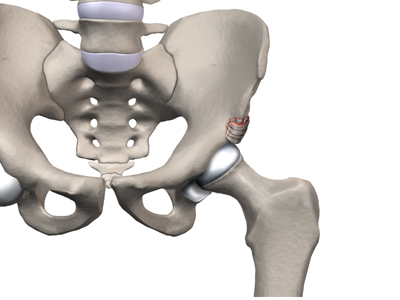
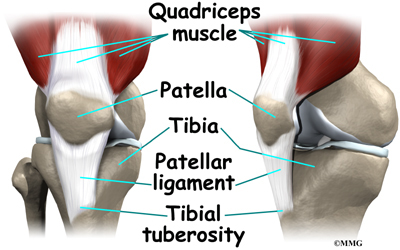
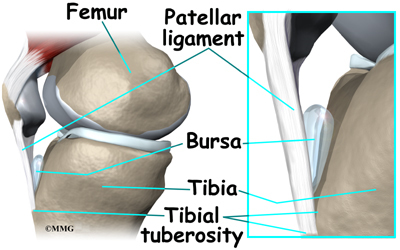
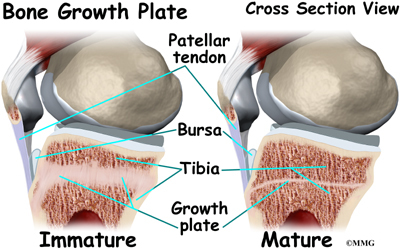
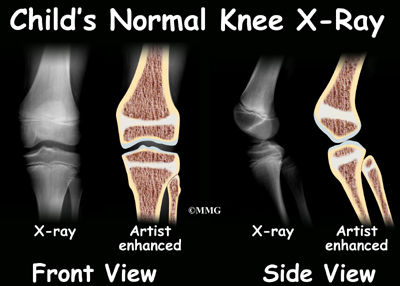
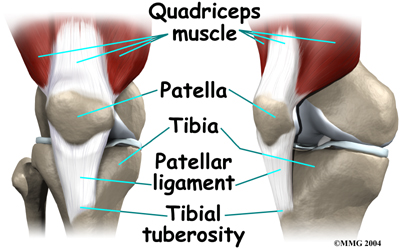
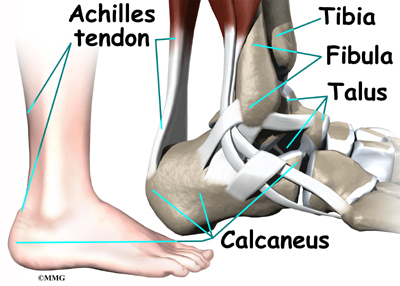
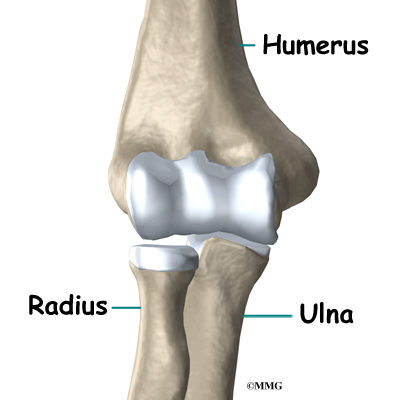
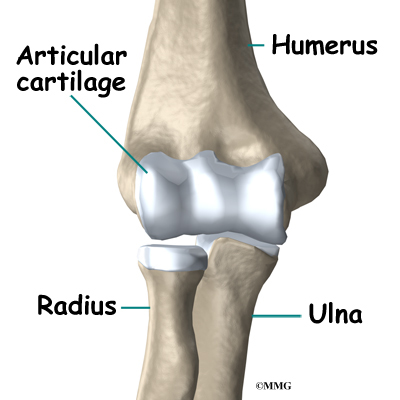
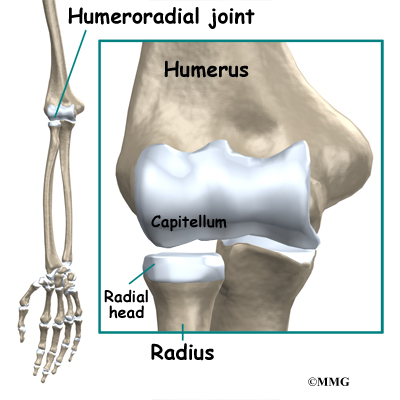
The knee joint is formed where the femur (thighbone) meets the tibia (shinbone). A smooth cushion of articular cartilage covers the end surfaces of both of these bones so that they slide against one another smoothly. The articular cartilage is kept slippery by joint fluid made by the synovial membrane (joint lining). The fluid is contained in a soft tissue enclosure around the knee joint called the joint capsule.
View animation of smooth movement
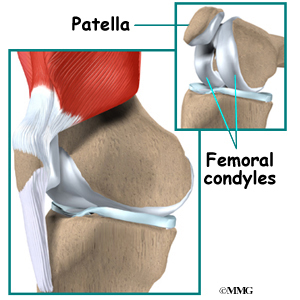
The patella, or kneecap, is the movable bone on the front of the knee. It is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The surface on the back of the patella is covered with articular cartilage. It glides within a groove on the front of the femur.
There are two femoral condyles in each knee. The medial femoral
condyle (the one closest to the other knee) and the lateral femoral condyle (on the outside half of the knee joint).
Related Document: A Patient’s Guide to Knee Anatomy
Rationale
What does the surgeon hope to achieve?
The main reason for replacing any arthritic joint with an artificial joint is to stop the bones from rubbing against each other. This rubbing causes pain. Replacing the painful and arthritic joint with an artificial joint gives the joint a new surface, which moves smoothly and without causing pain. The goal is to help people return to many of their activities with less pain and with greater freedom of movement.
View animation of smooth movement
Preparation
How should I prepare for surgery?
The decision to proceed with surgery should be made jointly by you and your surgeon. The decision should only be made after you feel that you understand as much as possible about the procedure.
Once you decide to proceed with surgery, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your regular doctor. This is to ensure that you are in the best possible condition to undergo the operation. You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery. Your therapist will begin the teaching process before surgery to make sure you are ready for rehabilitation afterwards.
One purpose of the preoperative visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, the presence of swelling, and the available movement and strength of each knee.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will practice some of the exercises used just after surgery. You will also be trained in the use of either a walker or crutches. Whether the surgeon uses a cemented or uncemented artificial knee will determine how much weight you will initially apply through your foot while walking. Finally, an assessment will be made of any needs you will have at home once you’re released from the hospital.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the unicompartmental artificial knee itself.
There are two major types of artificial knee replacements:
- cemented prosthesis
- uncemented prosthesis
Both are still widely used. In many cases a combination of the two types is used. The decision to use a cemented or uncemented artificial knee is usually made by the surgeon based on your age, your lifestyle, and the surgeon’s experience.
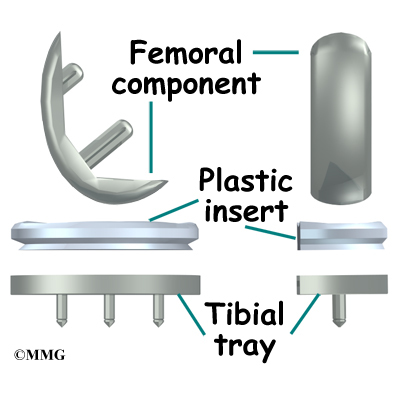
Each prosthesis is made up of two main parts.
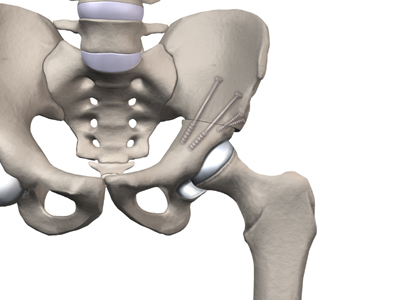
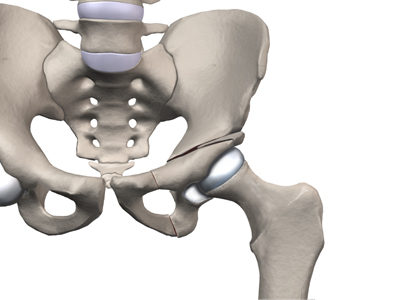
The tibial component (bottom portion) replaces the top surface of the lower bone, the tibia. The femoral component (top portion) replaces the bottom surface of the upper bone (the femoral condyle).
The femoral component is made of metal. The tibial component is usually made of two parts: a metal tray that is attached directly to the bone, and a plastic spacer that provides the slick surface. The plastic used is so tough and slick that you could ice skate on a sheet of it without much damage to the material.
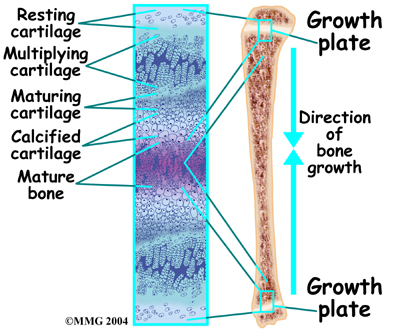
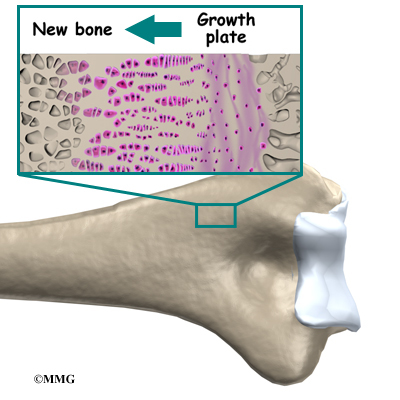
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis has a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
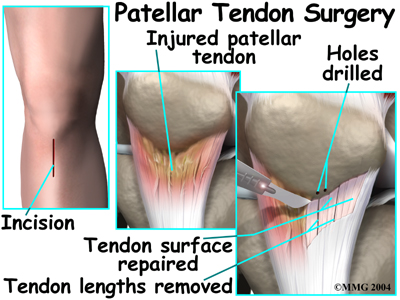
The Operation
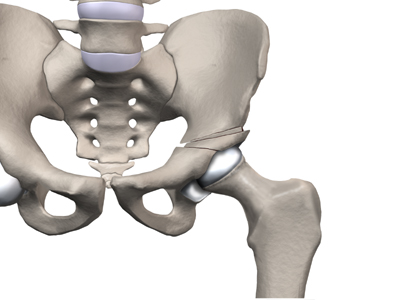
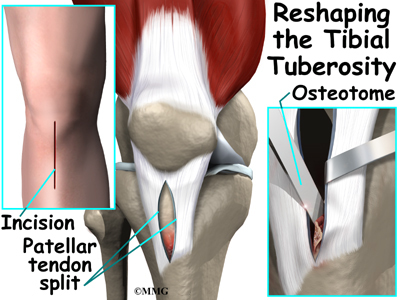
To begin the procedure, the surgeon makes an incision on the front of the knee to allow access to the joint. Several different approaches can be used to make the incision depending on whether the outer half (the lateral compartment) or the inner half (the medial compartment) is being replaced. The incisions used to perform the unicompartmental knee replacement are much smaller than those used to perform a traditional artificial knee replacement. For this reason, this surgery is sometimes referred to as minimally invasive.
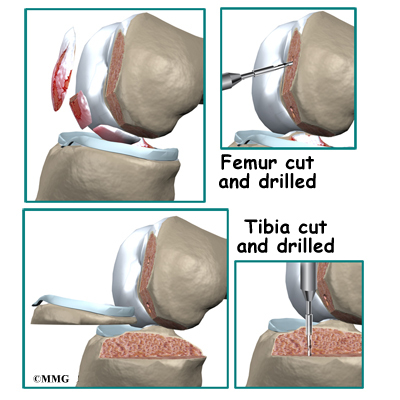
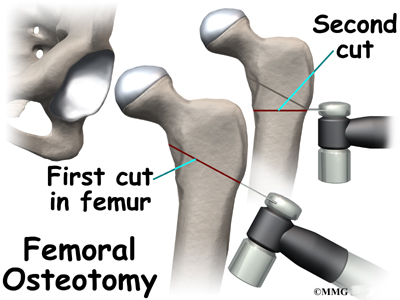
Once the knee joint is opened, a special positioning device (a cutting guide) is placed on the end of the femur. This cutting guide is used to ensure that the bone is cut in the proper alignment to the leg’s original angles, even if the arthritis has made you bowlegged or knock-kneed. With the help of the cutting guide, the surgeon cuts several pieces of bone from the end of the femur. The artificial knee will replace these worn surfaces with a metal surface.
View animation of removing the femoral joint surfaces
View animation of preparing the femoral joint surfaces
Next, the surface of the tibia is prepared. Another type of cutting guide is used to cut the tibia in the correct alignment.
View animation of preparing the tibial joint surfaces
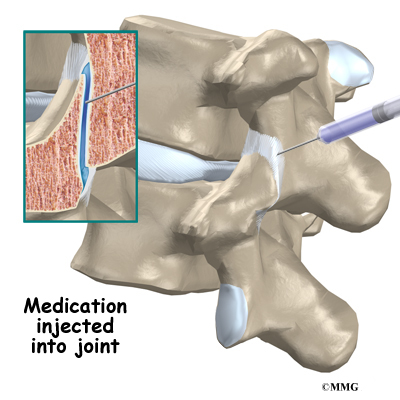
The metal femoral component is then placed on the femur. In the uncemented prosthesis, the metal piece is held snugly onto the femur because the femur is tapered to accurately match the shape of the prosthesis. The metal component is pushed onto the end of the femur and held in place by friction. In the cemented variety, epoxy cement is used to attach the metal prosthesis to the bone.
The metal tray that holds the plastic spacer is then attached to the top of the tibia. This metal tray is either cemented into place or held with screws if the component is of the uncemented variety. The screws are primarily used to hold the tibial tray in place until bone grows into the porous coating. The screws remain in place and are not removed.
The plastic spacer is then attached to the metal tray of the tibial component. If this component should wear out while the rest of the artificial knee is sound, it can be replaced. The replacement procedure is sometimes called a retread.
View animation of component placement
View animation of completed unicompartmental knee replacement
Finally, the soft tissues are sewn back together, and staples are used to hold the skin incision together.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following artificial knee replacement are
- anesthesia complications
- thrombophlebitis
- infection
- stiffness
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
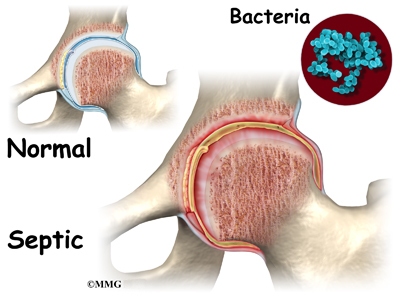
Infection
Infection can be a very serious complication following an artificial joint surgery. The chance of getting an infection following artificial knee replacement is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want you to take antibiotics when you have dental work or surgical procedures on your bladder and colon to reduce the risk of spreading germs to the joint.
Stiffness
In some cases, the ability to bend the knee does not return to normal after knee replacement surgery. To be able to use the leg effectively to rise from a chair, the knee must bend at least to 90 degrees. A desirable range of motion is greater than 110 degrees.
The most important factor in determining range of motion after surgery is whether the ligaments and soft tissues were balanced during surgery. The surgeon tries to get the knee in the best alignment so there is equal tension on all the ligaments and soft tissues.
Sometimes extra scar tissue develops after surgery and can lead to an increasingly stiff knee. If this occurs, your surgeon may recommend taking you back to the operating room, placing you under anesthesia once again, and manipulating the knee to regain motion. Basically, this allows the surgeon to break up and stretch the scar tissue without you feeling it. The goal is to increase the motion in the knee without injuring the joint.
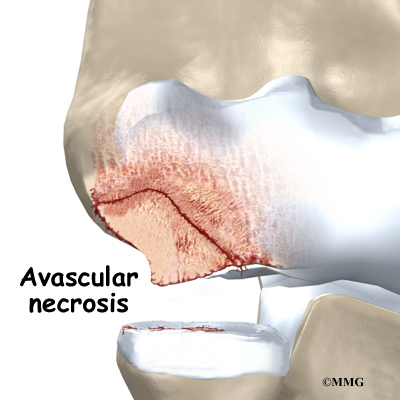
Loosening
The major reason that artificial joints eventually fail continues to be a process of loosening where the metal or cement meets the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from an artificial knee, but in some cases the knee will loosen earlier than that. A loose prosthesis is a problem because it usually causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the knee replacement.
Related Document: A Patient’s Guide to Revision Arthroplasty of the Knee
After Surgery
What happens after surgery
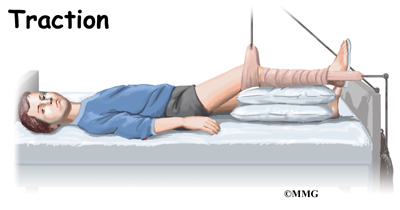
Some orthopedic surgeons recommend a device known as a continuous passive motion (CPM) machine immediately after surgery. The unit is thought to help prevent blood clots and speed healing of the wound. It may help patients get by with less need for medication. The unit may help improve knee mobility after knee replacement surgery. However, patients seem to do equally well in regaining knee motion by doing their exercises.
You may also have physical therapy treatments once or twice each day as long as you are in the hospital. Therapy treatments will address the range of motion in the knee. Gentle movement will be used to help you bend and straighten the knee. If you are using a CPM device, it will be checked for alignment and settings. Your leg may be elevated to help drain extra fluid in the leg.
Your therapist will also go over exercises to help improve knee mobility and to start exercising the thigh and hip muscles. Ankle movements are used to help pump swelling out of the leg and to prevent the possibility of a blood clot.
When you are stabilized, your therapist will help you get up for a short outing using your crutches or your walker.
Most patients are able to go home after spending one to two days in the hospital. In some cases, minimally invasive unicompartmental surgery can be done as an outpatient – meaning you can go home the same day.
You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and access the bathroom. It is also important that you regain a good muscle contraction of the quadriceps muscle and that you gain improved knee range of motion. Patients who still need extra care may be sent to a different unit until they are safe and ready to go home.
Most orthopedic surgeons recommend regular checkups after your artificial joint replacement. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends. You should always consult your orthopedic surgeon if you begin to have pain in your artificial joint, or if you begin to suspect something is not working correctly.
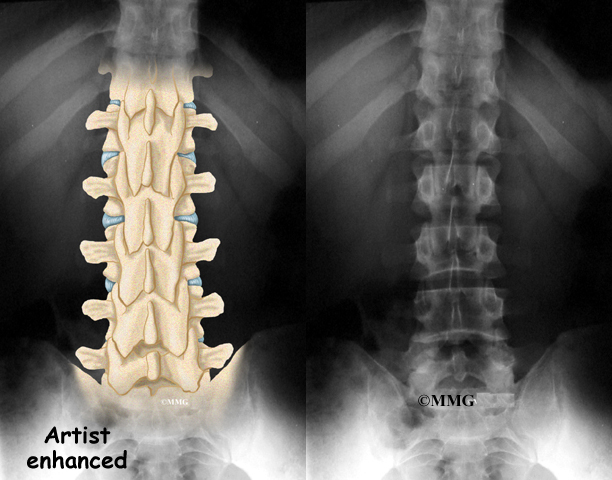
Most patients who have an artificial joint will have episodes of pain, but when you have pain that lasts longer than a couple of weeks you should consult your surgeon. The surgeon will examine your knee in search of reasons for the pain. X-rays may be taken of your knee to compare with x-rays taken earlier to see whether the artificial joint shows any evidence of loosening.
Rehabilitation
What should I expect during my rehabilitation?
Once discharged from the hospital, you may see your therapist for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on knee range of motion. In some cases you may require additional visits at home before beginning outpatient physical therapy. Home therapy visits end when you can safely leave the house.
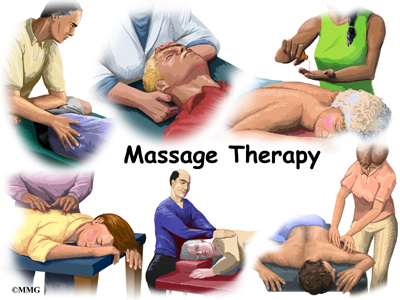
Visits to the physical therapist’s office come next. Your therapist may use heat, ice, or electrical stimulation to reduce any remaining swelling or pain.
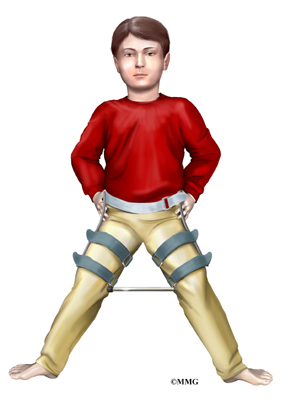
You should continue to use your walker or crutches as instructed. If you had a cemented procedure, you’ll advance the weight you place through your sore leg as much as you feel comfortable. If yours was a noncemented procedure, place only the toes down until you’ve had a follow-up x-ray and your surgeon or therapist directs you to put more weight through your leg (usually by the fifth or sixth week postoperatively).
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, thigh, and calf muscles. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the knee joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the knee.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, rising on your toes, and bending down. Specific exercises may then be chosen to simulate work or hobby demands.
Many patients have less pain and better mobility after having knee replacement surgery. Your therapist will work with you to help keep your knee joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new knee joint. Heavy sports that require running, jumping, quick stopping or starting, and cutting are discouraged. Cycling, swimming, and level walking are encouraged, as are low impact sports like golfing or bowling.
Your therapist’s goal is to help you improve knee range of motion, maximize strength, and improve your ability to do your activities. When you are well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.