A Patient’s Guide to Pain Management Medications
Introduction
There are several types of medications that can be used to treat pain. No one drug works for everyone. The medications that work best for you will depend on the type of pain you have and your response to them. Your medication regimen will need to be designed just for you.
This guide will help you understand
- what medications are commonly prescribed
- why these drugs are prescribed
- what are the risks and benefits of this treatment
Rationale
If you have lived with pain for a long time, it is common to have other conditions as well. These may include depression, anxiety, and insomnia (trouble sleeping). These conditions can make pain worse. And it’s harder for you to cope with the stress of living with pain. In order to get control over the pain, these conditions usually need to be treated at the same time as the pain.
The goal of using medication, as part of your treatment plan, is to increase your activity level. This can be done by improving pain control with drugs that you can afford while avoiding side effects.
The medications most commonly used in pain management belong to the following groups
- Opioid (narcotic)
- Non-opioid (non-narcotic)
- Acetaminophen (Tylenol®)
- Non-steroidal antiinflammatory (NSAID)
- Steroidal anti-inflammatory
- Antiepileptic (anticonvulsant)
- Antidepressant and antianxiety agents (anxiolytics)
- Muscle relaxants (antispasmodics)
- Sleep aids (hypnotics)
- Topical agents
Opioid (Narcotic) Pain Medications
Pain management experts prefer the term opioid to describe narcotic medication. The word narcotic is a legal term that is often linked with the illegal use of drugs.
Rationale
Opioid medications are expected to improve your activity level. They do this by decreasing the pain you feel when you are active.
Expected Benefit
Opioids such as morphine (MSContin), fentanyl (Duragesic), and methadone reduce pain by binding to opioid receptors in the brain. Most pain is responsive to opioid medications. However, some types of pain respond better than others. Nociceptive pain refers to skeletal or muscular pain. This type of pain is usually more responsive than neuropathic (nerve) pain.
Some problems such as fibromyalgia with diffuse (widely spread) myofascial (inflamed muscle and fascia) pain may respond at first. But studies show that patients with fibromyalgia do not do better over time on these drugs. Pain caused by headache may be relieved by opioids, but they can cause worse headaches later. These are called rebound headaches.
Potential Risks
There are some possible risks associated with opioid use. Not everyone will have all of these problems. With the right management, you may not have any problems. Risks can include
- Addiction
- Physical dependence
- Tolerance
- Hyperalgesia
- Decreased hormone levels
- Change in mood
- Sleep apnea
- Theft
- Death
Addiction is defined by craving, uncontrolled or compulsive use, and continuing to use the substance despite harm. Addiction is a complicated chronic disease. Simply taking an opioid does not cause addiction. If you have no risk factors, it is rare to develop the disease of addiction.
However, addiction is a possibility if you have the right (or wrong) genetics. Psychological and social stressors are also important factors. Family history must be reviewed before taking an opioid. There are ways to lower the risk of addiction or relapse if you are at risk for this disease. If you have an active addiction, the risk may outweigh the benefit of taking an opioid. Other options for pain control should be explored.
Substance abuse is a term used for unusual or abnormal behavior that does not meet the definition of addiction. Pain experts watch closely for any signs of this kind of behavior. These behaviors include reports of lost or stolen medication or use of medication in ways other than directed. Not taking the medication according to the directions would also fall into this category. Requesting early refills or taking a medication despite serious side effects are red flag behaviors. Taking the drug to deal with stress such as after a heated argument with someone is also a warning sign. These behaviors are often a signal that you may be getting into trouble with your medication. Your treatment plan may need to be altered. The goal is to get the most benefit with the least risk of side effects.
Pseudo-addiction is the term used to describe what appears to be dangerous or unusual behavior but occurs when pain is not being fully treated. Think about this idea. You have constant pain. It lasts all day and night. You are given a pain medication and told to take one every eight hours. The pain medication that you are prescribed is effective and allows you to be active. But it only works for about four hours. Four hours before the next dose is due, you are in great pain again. How would you respond?
Some people take more drug than is prescribed. Then they run out of pills early. Others complain bitterly at every appointment. They demand a refill. To the doctor it seems as if the person is “drug seeking”. Some may go to more than one doctor to get what they think they need to relieve the pain. When these behaviors are caused by under-treatment of pain, an increase in the dose stops the behavior. If these behaviors start up shortly (within days to weeks) after the dose increase, then there may be other reasons for the behavior.
Physical dependence occurs in everyone on opioids. This happens when you take them regularly for more than two to three weeks. Physical dependence does not mean that you are addicted. Physical dependence means that your body has become used to the drug. You feel withdrawal symptoms if the medication is stopped suddenly.
Symptoms of withdrawal can range from mild irritability to sweating, diarrhea, vomiting, and muscle cramps. You may feel like you have a severe case of the flu. You may feel like you are dying. But withdrawal from opioids is not fatal. It can be avoided by slowly decreasing the amount of drug you take. This can be done over several days up to several weeks. The time it takes to get off the medication without having unpleasant symptoms depends on how much medication you are on and how long you have been on it.
Many opioids require a hand signed prescription every time you need it refilled. It is very important to plan ahead for holidays. You don’t want to run out.
Tolerance to a medication occurs when an individual requires more medication to achieve the same amount of pain relief. Tolerance is not the same as addiction. Not everyone develops tolerance to pain relief. If you should have tolerance to your pain medication, there are ways to deal with it. For example, your doctor may increase the amount you are taking. Or you may be switched to a different drug. Sometimes treating other conditions such as depression and anxiety is helpful. Adding a non-opioid drug can help, too. The best approach depends on your situation. You and your healthcare provider will decide together what’s best for you.
Hyperalgesia is an increase in painful sensation. If you become less functional and feel more pain after starting or increasing an opioid, you may be having hyperalgesia. If hyperalgesia develops, decreasing the opioid or stopping it will improve pain control. Other non-opioid medications and non-medication treatments can be useful should you experience hyperalgesia.
Decreased hormone (testosterone and estrogen) levels can develop over time. Let your healthcare provider know if you feel a decrease in energy, increased depression, or new sexual problems. Simple blood tests can be ordered to see if you are having a decrease in hormone levels. Treatment for this problem is possible. It might mean replacing the hormone or stopping the opioid medication.
A change in mood can occur with opioid medications. You may feel worse (depressed mood). Or you may feel better (elevated mood). If you have a mood disorder such as depression or anxiety, an opioid can make you feel better. This can be hard to sort out. You may not be able to tell if you feel better because of the mood elevation or because you are getting pain relief.
But opioids only improve mood for a short period of time such as several weeks to several months. It is not possible for this mood elevation to last very long without an increase in opioid dose on a regular basis. This complicates therapy. And it can be dangerous. If you have a mood disorder, it needs to be treated in order to get good pain relief from an opioid. Mood disorders or worsening of the spinal condition are more often behind dose increases than tolerance to the pain relief. Short-acting opioids such as hydrocodone found in Lortab® and oxycodone found in Percocet® are useful for pain that only lasts a short time (less than three to four hours). These drugs are good choices when pain doesn’t occur very often. The short-acting opioids are linked with mood changes. It is best to use long-acting opioids whenever possible. This will help you avoid the ups and downs of the short-acting medication. First it kicks in and then it wears off within hours.
Sleep apnea can get worse while taking opioids. If you think you have sleep apnea, you should have it checked before starting an opioid medication.
Theft. Opioid medications have value in the illegal drug market. People have been known to open medicine cabinets, go through drawers, and attend open houses just to look for these drugs. Family members have been known to do the same thing. They may go through your medicine cabinets and steal medications to either take for themselves or sell for profit. Be sure to keep your opioid medications safely locked away. This step is for your benefit and for the safety of others. Many healthcare providers will not replace stolen medications.
Death can be caused by taking more of the medication than prescribed. If you take too large of a dose, an opioid can stop your breathing. However, the benefits of the correct dose include the fact that they do not damage organs such as your liver or kidneys. Opioids must be started at a low dose and slowly increased as you become used to them. Methadone is unusual as it builds up in the body over three to seven days. As methadone builds up in the body, it becomes more effective. This means that the full effect of the current dose doesn’t occur for three to seven days. Methadone causes accidental overdoses and death when patients take extra doses. They do this while trying to get more pain relief now. It is extremely important to take opioids only as directed. Never take extra. Talk to your doctor if you aren’t getting the pain relief you need.
Potential Side Effects
The most common side effects from daily use of opioids are constipation, stomach upset, itching, and drowsiness. All of these side effects (except constipation) become milder. They can be treated if needed. They usually go away over five to10 days.
Exercise and eat a healthy diet to prevent constipation. Drink plenty of water and eat fiber-rich foods such as vegetables and fruits. Prunes are an excellent choice. Even with a good diet and exercise, you will most likely need a stimulant laxative while on an opioid.
Avoid bulk laxatives such as Metamucil® because excessive bulk can worsen constipation caused by opioids. A combination of senna (stimulant laxative) with docusate (stool softener) such as is found in Senokot S® (or any generic equivalent) is recommended. Start with two tablets at bedtime and increase as needed. This will help you have a bowel movement at least every other day. Do not take more than eight tablets per day. Tell your healthcare provider if this does not prevent constipation for you. You may need a more aggressive treatment approach.
Non-Opioid (non-narcotic) Pain Medications
Acetaminophen (Tylenol®)
Rationale
Acetaminophen improves your level of activity by decreasing the pain you feel while active.
Expected Benefit
Acetaminophen or Tylenol® inhibits pain-generating substances called prostaglandins. It blocks the pain pathway to the brain. Acetaminophen works well for mild-to-moderate pain by itself. When taken with other medications, it can improve your pain control.
Potential Risks
Liver failure is the main risk linked with acetaminophen. The overuse of acetaminophen is the most common reason for liver failure and the need for a liver transplant. Acetaminophen is in many prescription and non-prescription products. So be sure to read all labels to see if it is in any of your other medications. Never take more than four grams of acetaminophen per day. Four grams is equal to eight extra-strength 500 mg tablets or 12 regular strength 325 mg tablets. Tell your healthcare provider if you have any liver disease and/or a history of alcohol abuse. You may need to limit your use to less than two grams per day. Or you may have to avoid acetaminophen entirely. This depends on your risk factors for liver disease.
Potential Side Effects
Acetaminophen is well-tolerated and unlikely to cause any significant side effects when taken as prescribed.
Nonsteroidal anti-inflammatory Drugs (NSAIDs)
Rationale
NSAIDs can improve your level of activity by decreasing pain and swelling.
Expected Benefit
NSAIDs inhibit the production of inflammatory substances such as prostaglandins. NSAIDs are commonly used for acute painful conditions such as a sprained ankle or a flare-up in back pain. They are also used to decrease the pain and stiffness you might feel with arthritis.
Potential Risks
Let your healthcare provider know if you have any problems with your stomach, intestines, or kidneys. Any problem with bleeding should also be reported. Some NSAIDs have been shown to increase the risk of cardiovascular disease resulting in heart attack or stroke. These medications can be very helpful in the short-term ranging from several days to several weeks. The benefit of using them for months-to-years needs to be carefully weighed against your personal risk factors for cardiovascular disease, kidney disease, and stomach ulceration.
If you have kidney disease, you are at an increased risk for kidney failure. If you are diabetic, you have an increased risk of developing kidney disease and kidney failure.
Bleeding can be increased as a result of taking NSAIDs. Most NSAIDs such as ibuprofen (Advil®), naproxen (Naprosyn®, Aleve®), and piroxicam (Feldene®) can increase bleeding. These drugs should be stopped before surgery. Avoid taking them if you are taking a blood thinner. Celecoxib (Celebrex®) is the only NSAID on the market at this time that does not increase bleeding and is allowed to be taken prior to surgery.
Stomach ulcers can be caused by NSAIDs irritating the stomach or intestinal lining. You may decide to take an NSAID even if you are at risk for ulcers. If this is the case, there are products that can help protect the stomach and intestinal lining such as omeprazole (Prilosec®) and esomeprazole (Nexium®).
Potential Side Effects
Stomach upset is the most common side effect. Taking NSAIDs with food usually helps. If taking the medication with food doesn’t help enough, your healthcare provider may prescribe medication to protect your stomach. While on the NSAID, you may also be given famotidine (Pepcid®), omeprazole (Prilosec®), or esomeprazole (Nexium®).
Steroidal Antiinflammatory Medications
Rationale
Steroids decrease inflammation. They do this by decreasing the body’s immune response to injury or disease.
Expected Benefit
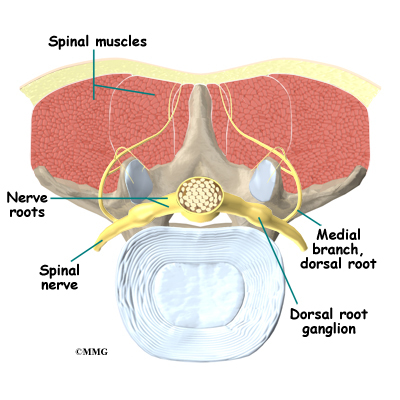
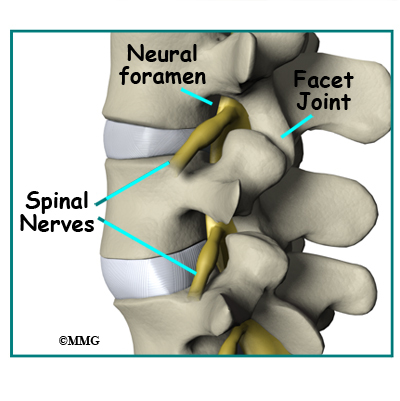
In an acute flare-up of pain, a short course of a steroidal anti-inflammatory may be helpful. Drugs such as methylprednisone (Medrol®) can decrease pain by decreasing swelling and inflammation. The effect takes place around the spinal nerves. With this treatment, you may be able to return to your activities sooner.
Potential Risks
Short-term use, such as several days to several weeks is usually safe. Long-term use (months to years) can cause major problems. Osteoporosis, diabetes, poor wound healing, and increased risk of infection are among the most common problems.
Potential Side Effects
There are some common side effects from taking steroids. These include mood changes (either feeling better or worse), increased appetite, indigestion, increased nervousness, and decreased sleep. If you have diabetes, you will need to check your blood sugar closely.
Antiepileptic Medications (Anticonvulsants)
Rationale
Anti-epileptic Drugs (AEDs) are expected to improve your activity level. They do this by decreasing the pain you feel. They also help you cope with the stresses of living with pain.
Expected Benefit
Anti-epileptic Drugs (AEDs) are used to treat epilepsy, stabilize moods, and manage neuropathic (nerve) pain. Nerves can become pain generators. AEDs quiet the nervous system. If you have lived with pain for very long, you most likely have some nerve pain. Pain described as streaking, lightening, burning, tingling, pins and needles, or pain radiating down legs or arms is most likely neuropathic pain. Many people get good pain relief when given a medication from this group such as gabapentin (Neurontin®) or pregabalin (Lyrica®.)
Potential Risks
Abruptly stopping the medication can bring on seizures. This can be avoided. Slowly decrease the medication before stopping. There are many different medications in this group. Some have specific risks associated with them. Topiramate (Topamax®) is linked with an increased risk of kidney stones. Lamotrigine (Lamictal®) can cause a severe skin rash. Carbamazepine (Tegretol®) has rare reports of blood disorders. Be sure to ask your healthcare provider about the specific risks of any AED you are thinking about taking.
Potential Side Effects
Most AEDs are well-tolerated if they are started at a low dose and slowly increased. Drowsiness, dizziness, tiredness, swelling, and stomach upset are the most common side effects. Tremor, blurred vision, dry mouth, constipation, anxiety, and weight gain are also common.
Antidepressant and Anti-anxiety Medications
Rationale
Antidepressants decrease pain while improving mood and your ability to cope with the pain. Some antidepressants also improve neuropathic pain.
Expected Benefit
Pain is very much affected by mood and mood is very much affected by pain. Both need to be taken care of in order to get good pain relief. Most antidepressants also treat anxiety. In addition to anxiety and depression, certain antidepressants are good at treating neuropathic pain. The antidepressants that are good at decreasing neuropathic pain are the ones that increase both serotonin and norepinephrine activity. These include the older tricyclic antidepressants (TCAs) such as amitriptyline (Elavil®) and nortriptyline (Pamelor®) and the newer serotonin norepinephrine reuptake inhibitors (SNRIs) duloxetine (Cymbalta®) and venlafaxine (Effexor®). The selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac), paroxetine (Paxil®), and sertraline (Zoloft®) are good antidepressants and anti-anxiety medications. They do not specifically treat neuropathic pain.
Potential Risks
If you are bipolar, adding an antidepressant without a mood stabilizer can bring on mania. Most of these medications can cause withdrawal symptoms if stopped abruptly. Because of a few reports of liver failure, duloxetine (Cymbalta®) should be avoided in alcoholics and anyone with liver disease.
Benzodiazepines are not antidepressants but are very effective anti-anxiety agents. They have the additional risks of addiction and physical dependence. They are only used when other drugs fail. Examples of benzodiazepines used to treat anxiety are lorazepam (Ativan®) and clonazepam (Klonopin®). Be sure to ask your healthcare provider about the specific risks associated with any antidepressant or anti-anxiety agent that you are planning to take.
Potential Side Effects
The most common side effects are stomach upset, feeling wired, drowsiness, and tiredness. Sexual dysfunction, flat mood, insomnia, headache, and appetite changes can also occur. Some cause carbohydrate craving and weight gain. When first starting one of these medications, some people feel increased anxiety. But these medications are generally well-tolerated if started at a low dose and slowly increased. If you do not respond well to one of these drugs, changing to a different one may give you better results.
Muscle Relaxants (Antispasmodics)
Rationale
Muscle relaxants decrease the pain associated with muscle spasms. This should allow you to be more active such as being able to participate in physical therapy.
Expected Benefit
Surgery, injury, or increasing activity often causes muscle spasms. Pain caused by muscle spasms does not respond well to other pain medications. Use of a muscle relaxant helps keep pain from muscle spasms under control.
Potential Risks
The muscle spasm agents do not usually work well for long periods of time. After an initial injury, they often serve as tranquilizers rather than as effective treatment for muscle spasms. Methocarbamol (Robaxin®) and cyclobenzaprine (Flexeril®) are examples of commonly prescribed muscle relaxants. Physical dependence and addiction are risks with the benzodiazepine group of antispasmodics. Examples of benzodiazepines used to treat muscle spasms are diazepam (Valium®) and lorazepam (Ativan®).
Potential Side Effects
Drowsiness, dizziness, lightheadedness, upset stomach, blurred vision, insomnia, low blood pressure, and dry mouth are all potential side effects associated with muscle relaxants.
Sleeping Aids (Hypnotics)
Rationale
Many patients have trouble sleeping. Sleeping aides help you sleep. Improving sleep should help you cope with pain and the stresses that come with the pain.
Expected Benefit
Lack of sleep makes everything worse, including pain. You may have trouble falling asleep. Or you may wake up during the night unable to fall back asleep. Which sleep aid is best for you depends on your sleep pattern. Other factors such as pain and depression can make a difference. Short-term use of sleeping aids is very helpful for some people. However, learning good sleep habits and treating the pain properly are the preferred long-term solutions.
Potential Risks
The risks depend on the medication chosen to improve sleep. Diphenhydramine (Benadryl®) is in many products such as Tylenol PM®. Diphenhydramine is an antihistamine. Because its main side effect is drowsiness, it is also used for sleep. It causes more problems in elderly patients than in young patients. Urinary retention, low blood pressure resulting in falls, and confusion are risks for the elderly. You should not take products containing diphenhydramine if you are over 65 years old.
Some medications such as zolpidem (Ambien®) come with the risk of withdrawal or rebound insomnia when they are abruptly stopped.
Some medications can cause sleepwalking and amnesia. Or you may forget what you have done during the night. This has been associated with several medications including zolpidem (Ambien®) and triazolam (Halcion®).
Trazodone (Desyrel®) is an antidepressant that causes drowsiness. In low doses, it is used for sleep. It is considered safe for older patients to use. Young males are at risk for priapism. This is a painful erection that does not go away and can require a visit to the emergency room. Occasionally surgery is needed to resolve the problem.
Potential Side Effects
Daytime drowsiness, nightmares, and dry mouth are the most common side effects. Eszopiclone (Lunesta®) can cause such a severe bad after taste that patients refuse to take it. If you experience a bad taste with Lunesta®, try taking it with orange juice.
Topical Agents
Rationale
Topical medications can improve pain control without causing the side effects that result from taking an oral medication.
Expected Benefit
Some medications such as diclofenac (Voltaren®) can be absorbed through the skin allowing it to be mixed into a lotion or a cream and applied directly to the area that hurts. The drug acts locally and doesn’t have to be absorbed into the blood stream. If it doesn’t go throughout the body, side effects such as stomach ulcers can be avoided.
Capsaicin (Zostrix®) is made from hot peppers. Applying it for 4-6 weeks depletes substance P in the painful area. Substance P stimulates nerves to transmit the pain signal to the brain. By eliminating substance P, nerve pain can be drastically reduced. It has also been beneficial for pain caused by osteoarthritis in the joints such as in the knees. Lidocaine can be mixed into a lotion such as in Emla® or absorbed from a patch such as in Lidoderm®. Lidocaine can decrease the pain you feel by numbing the painful area.
Potential Risks
Most of these are considered safe when applied to the skin. The cost can go up if they have to be mixed by a pharmacist. Excessive use can result in too much absorption. When that happens you can get the same side effects as the oral medication. Be sure to follow the instructions as with any medication.
Potential Side Effects
Skin irritation is the most common side effect. Capsaicin works well but has to be used very carefully. Using too much at first can cause a severe burning sensation. You can avoid this by applying a tiny amount to a dime-sized area one to two times per day. Slowly increase the amount you use over several weeks. Do not give up too soon. It takes four to six weeks of daily use for it to work. The pain control is worth the patience it requires. It is doesn’t cost very much. It doesn’t need a prescription. And it delivers good neuropathic pain control without any other side effects.