A Patient’s Guide to Shoulder Dislocations
Introduction
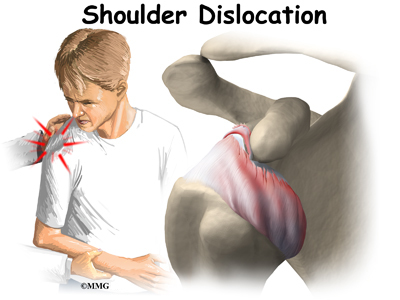
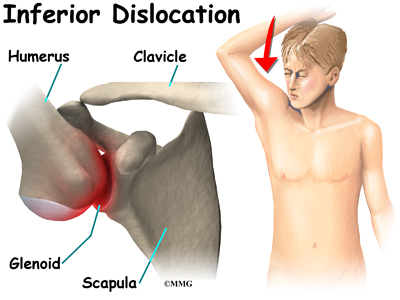
A shoulder dislocation is a painful and disabling injury of the glenohumeral joint. Most dislocations are anterior (forward) but the shoulder can dislocate posteriorly (backwards). Inferior and posterolateral dislocations are possible but occur much less often. The specific type of dislocation is based on the position of the humeral head in relation to the glenoid (shoulder socket) at the time of the diagnosis.
This guide will help you understand
- what parts of the shoulder are involved
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the body are involved?
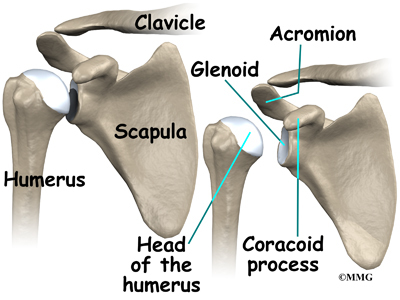
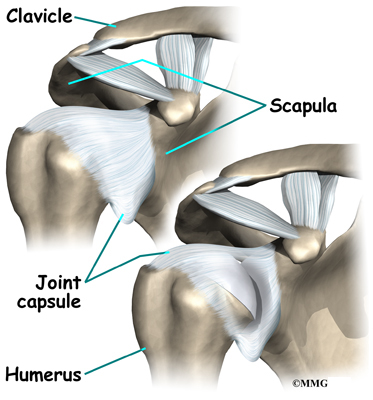
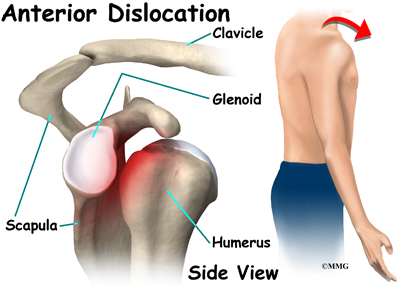
The shoulder has unique and complex anatomy that allows range of motion and coordination needed for reaching, lifting, throwing, and many other movements. The bones of the shoulder are the humerus (the upper arm bone), the scapula (the shoulder blade), and the clavicle
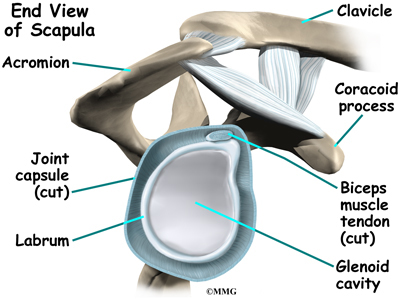
(the collar bone).The roof of the shoulder is formed by a part of the scapula called the acromion.
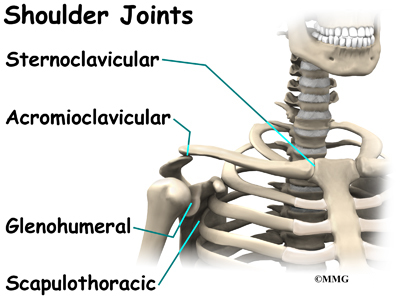
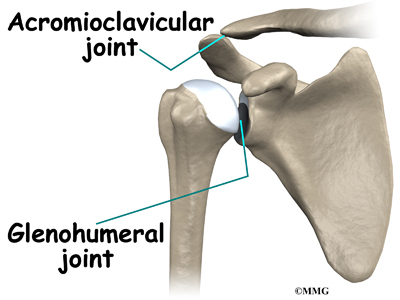
There are actually four joints that make up the shoulder. The main shoulder joint, called the glenohumeral joint, is formed where the ball of the humerus fits into a shallow socket on the scapula. This shallow socket is called the glenoid. Understanding the remaining anatomical structures
discussed will help you understand why your shoulder dislocated.
The acromioclavicular (AC) joint is where the clavicle meets the acromion. The sternoclavicular (SC) joint supports the connection of the arms and shoulders to the main skeleton on the front of the chest. The scapulothoracic joint is formed where the shoulder blade glides against the thorax (the rib cage). This joint is important because it requires that the muscles surrounding the shoulder blade work together to keep the socket lined up during shoulder movements.
Ligaments, Joint Capsule, and Labrum
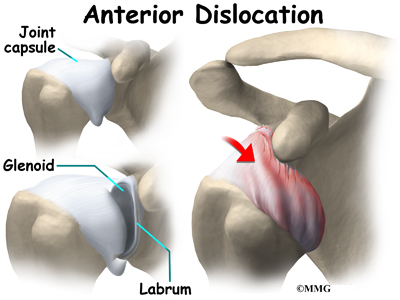
There are several important ligaments in the shoulder. Ligaments are soft tissue structures that connect bones to bones. A joint capsule is a watertight sac that surrounds a joint. In the shoulder, the joint capsule is formed by a group of ligaments that connect the humerus to the glenoid. These ligaments are the main source of stability for the shoulder. They help hold the shoulder in place and keep it from dislocating.
The labrum is a special cartilaginous structure inside the shoulder. It is attached almost completely around the edge of the glenoid. When viewed in cross section, the labrum is wedge-shaped. The shape and the way the labrum is attached create a deeper cup for the glenoid socket. This is important because the glenoid socket is so flat and shallow that the ball of the humerus does not fit tightly. The labrum creates a deeper cup for the ball of the humerus to fit into and helps prevent dislocation.
The labrum is also where the biceps tendon attaches to the glenoid. Tendons are much like ligaments, except that tendons attach muscles to bones. Muscles move the bones by pulling on the tendons. The biceps tendon runs from the biceps muscle, up the front of the upper arm, to the glenoid. At the very top of the glenoid, the biceps tendon attaches to the bone and actually becomes part of the labrum. This connection can be a source of problems when the biceps tendon is damaged and pulls away from its attachment to the glenoid.
The Rotator Cuff
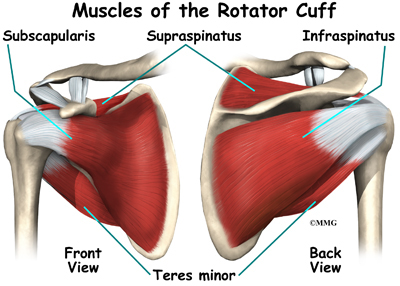
The tendons of the rotator cuff are the next layer in the shoulder joint. Four rotator cuff tendons connect the deepest layer of muscles to the humerus. This group of muscles lies just outside the shoulder joint. These muscles help raise the arm from the side and rotate the shoulder in the many directions. They are involved in many day-to-day activities. The rotator cuff muscles and tendons also help keep the shoulder joint stable by holding the humeral head in the glenoid socket.
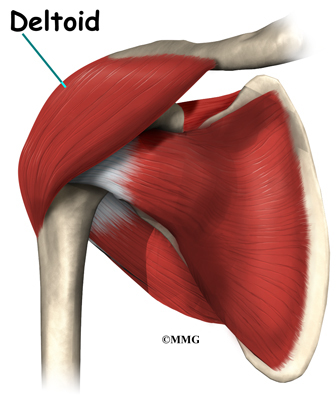
The large deltoid muscle is the outer layer of shoulder muscle. The deltoid is the largest, strongest muscle of the shoulder. The deltoid muscle takes over lifting the arm once the arm is away from the side.
Types of Shoulder Dislocations
Anterior Dislocation
With an anterior dislocation, the head of the humerus is driven forward from inside the glenoid cavity to a place under the coracoid process. This type of dislocation is sometimes referred to as a subcoracoid dislocation. The joint capsule is usually avulsed (torn away) from the margin of the glenoid cavity.
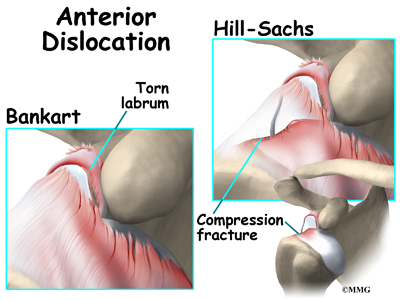
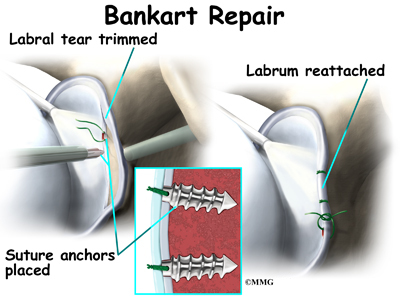
Anterior shoulder dislocation can also be the result of a detached labrum. When both the labrum and the capsule along the anterior margin of the glenoid cavity are avulsed, the injury is called a Bankart lesion. Compression fracture of the humeral head from the force of hitting the hard glenoid is called a Hill-Sach’s lesion. Three-fourths of the patients with a Bankart lesion will also have a Hill-Sach’s lesion.
Posterior and Inferior Dislocations
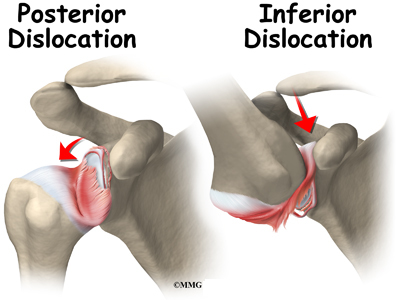
When the shoulder dislocates posteriorly, the head of the humerus moves backward behind the glenoid. An inferior dislocation describes the position of the humeral head down below the glenoid cavity. Posterior and inferior shoulder dislocations only account for about five to 10 per cent of all shoulder dislocations. Most shoulder dislocations are in the anterior direction.
Related Document: A Patient’s Guide to Shoulder Anatomy
Causes
What causes this problem?
The shoulder is a very mobile joint and more vulnerable to dislocation than other joints. The glenoid cavity is small in relation to the head of the humerus. Muscles, ligaments, and the bony anatomy of the shoulder all work together to maintain shoulder stability and prevent dislocation. Dislocation can occur when any of these structures are injured or altered in any way.
Tears or ruptures of the rotator cuff are the most common injuries that lead to shoulder dislocation. Fractures of the humerus and damage to any of the nerves (e.g., axillary, brachial plexus) supplying the rotator cuff can also result in shoulder dislocation. A fall on an outstretched hand or directly on the posterolateral aspect (back and side) of the shoulder can cause an anterior dislocation. Violent uncoordinated muscle contractions during a grand mal seizure can also cause shoulder dislocations.
Forceful motions that cause soft tissue structures to tear or rupture lead to dislocation. Forceful abduction, external rotation, and extension are the most common load resulting in shoulder dislocation. The joint capsule may be lifted off the bone and the head of the humerus gets lodged between the capsule and the bone.
Once the shoulder has been dislocated the first time, there is a high probability (90 per cent chance) of a second shoulder dislocation (recurrence). The force of the first dislocation dislodging the head of the humerus forward leaves a pocket formed by sagging soft tissues that the humeral head can slip back into. Some people with very lax ligaments can dislocate the shoulder and reduce it over and over. This is referred to as habitual dislocation and should be discouraged.
The highest incidence of recurrence is in young people (under the age of 20 at the time of the injury). Sixty per cent of patients between 20 and 40 years will have a recurrence. Only 10 per cent of patients over 40 years will have another shoulder dislocation. Participation in contact sports activity increases the risk of reinjury. After a second dislocation, frequent recurrence of shoulder dislocation can occur with less and less force, load, or stress.
Symptoms
What does the condition feel like?
Most people with a shoulder dislocation experience sudden, severe pain in the shoulder after a fall, injury, or other traumatic event. It’s a natural response to hold and support the arm against the body with the other hand.
Pain and a feeling of extreme apprehension with any movement of the arm are common. This type of apprehension is present when instability remains after the shoulder has been reduced (manually put back in place). You may be constantly aware that if you move the arm in just the right way, it will pop out again.
With an inferior dislocation, it is difficult (and sometimes impossible) to bring the arm down to the side. This is because the head of the humerus is caught under the glenoid cavity.
Diagnosis
How do doctors diagnose the problem?
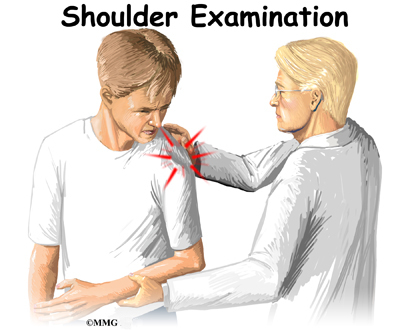
The history and physical examination are probably the most important tools the physician uses to diagnose a ruptured or deficient rotator cuff and/or bone fracture. Any of these injuries in the shoulder complex can lead to (and will be present along with) shoulder dislocation.
Your physician will visually inspect the shoulder. When there is a shoulder dislocation, the normal rounded contour of the shoulder and upper arm is lost. Instead, the outside edge of the shoulder looks flat or square. There are changes in the appearance of the surface anatomy. For example, instead of the greater tuberosity (bony bump along top of shoulder), there is a gap under the acromion. The head of the humerus may be observed and felt as a large bump in front or behind the shoulder. The area is usually extremely tender to palpation.
Range of motion, strength, and sensation will be tested if possible. Any changes or loss of sensation may point to nerve damage. The physician will also check the pulses in your arm in order to detect the possibility of vascular complications.
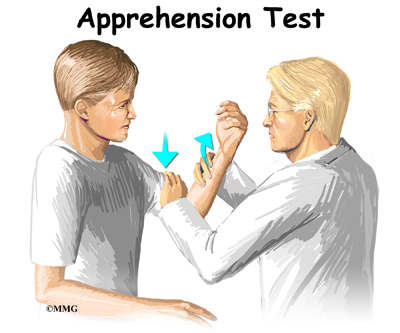
There are many clinical tests that can be performed to identify which soft tissue structures have been damaged or ruptured. A positive apprehension test is very diagnostic of an unstable shoulder that might dislocate again after a first dislocation injury. The arm is abducted (moved away from the body) and externally (outwardly) rotated. Just before the joint is about to dislocate, the patient becomes extremely anxious. At that point, the test is considered positive for shoulder instability and therefore discontinued.
X-rays are an important diagnostic tool to show the displaced head of the humerus and any bone fractures. Several views may be needed to reveal the exact direction of the dislocation and fracture lines when present. Magnetic resonance imaging (MRI) is used to diagnose and define the extent of the lesion. MRIs are very accurate in detecting Hill-Sach’s lesions.
If surgery is being considered, then the surgeon may perform a diagnostic arthroscopic exam. A log, thin scope with a tiny fiber-optic TV camera on the end is inserted into the shoulder joint, allowing the orthopedic surgeon to look at the structures inside the joint directly.
Treatment
What treatment options are available?
Nonsurgical Treatment
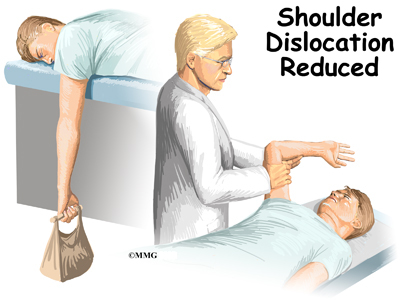
In many cases, the shoulder can be reduced without surgery. This is called a closed reduction. Many health care professionals (especially those trained in emergency procedures) know how to manipulate the shoulder back into the socket. However, without the aid of a general anesthetic, this maneuver can be very painful.
One simple technique to reduce an anterior shoulder dislocation is done in the prone (face down) position. The injured arm is supported at the edge of the table. The arm is allowed to dangle over the edge of the table with a weight attached. As the shoulder muscles relax, the humeral head slips back to its normal position. This may take several minutes.
If passive positioning doesn’t work for an anterior dislocation, then a general anesthetic is administered and traction is applied to the upper limb. The arm is held in a position of shoulder abduction (away from the body) while lateral (sideways) and backward pressure is applied to the head of the humerus. Posterior shoulder dislocation can be treated in a similar fashion. Under anesthesia, the shoulder is rotated outwardly and forward pressure is applied on the dislocated humeral head.
Some patients who have recurrent dislocations know how to pop the joint back in place without help. When performed by someone else, the procedure is done quickly in order to prevent further pain or soft tissue damage. Functional outcome is better if the dislocation is reduced early.
Following closed reduction, X-rays are used to confirm correct placement of the humeral head in the glenoid cavity. After reduction, immobilization of the arm in a sling against the chest is usually recommended. Immobilization of the reduced shoulder is applied for several weeks up to a month. This approach will give the soft tissues a chance to heal. For older adults, passive exercises called Codman’s or pendulum exercises may be prescribed to prevent stiffness. These are usually done once or twice a day with the sling removed.
Recurrent dislocation is the most common complication after dislocation, especially in young people. Older adults are more likely to experience chronic pain and stiffness. When conservative care is unable to restore shoulder stability and normal function, then surgical intervention may be needed.
Surgery
If the shoulder can’t be reduced manually or if a sling and rehabilitation program does not control symptoms of instability, then surgery may be suggested. The main goal of surgery is to reduce and/or stabilize the shoulder. Restoring normal motion and function and preventing recurrent dislocations are important outcomes of surgical intervention.
Even when surgery is needed, your surgeon may have you see a physical therapist for several visits before the surgery. This is done to reduce swelling, strengthen the muscles, and stabilize the shoulder as much as possible before surgery. This practice also reduces the chances of scarring inside the joint and can speed recovery after surgery.
There are many different ways to repair a chronically unstable shoulder following a first dislocation or after many recurrent shoulder dislocations. The direction of instability (anterior, posterior, inferior, or some combination) is taken into consideration when choosing the best reconstructive technique. The site, type, and extent of damage are major determining factors in how the surgeon approaches the repair.
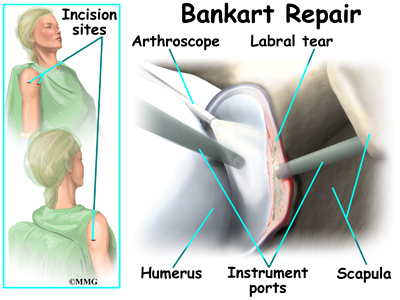
One of the most common procedures is the Bankart operation. During the Bankart reconstruction procedure, the labrum and capsule are reattached to the anterior margin of the glenoid cavity.
Shoulder reconstruction surgery may be done with an open incision method or with the aid of an arthroscope. Incisions are usually still required with arthroscopic technique, but the surgery doesn’t require the surgeon to open the joint. The arthroscope is used to view the inside of the shoulder joint as the surgeon performs the work.
Older adults who have a fracture and shoulder dislocation may need a shoulder replacement instead of shoulder reconstructive surgery to reduce the dislocation and repair the fracture.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Patients may receive physical therapy after having a dislocation. Therapists treat swelling and pain and help minimize tension on inflamed structures with the use of ice, supportive taping, electrical stimulation, and rest periods. Symptoms are addressed in the acute phase but restoring normal function rather than eliminating symptoms is the focus for chronic shoulder instability.
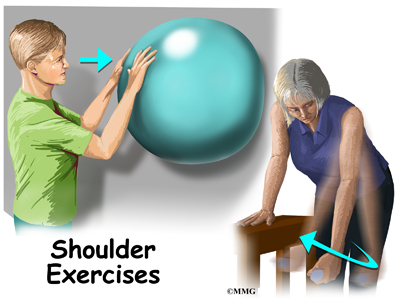
Exercises are used to help you regain normal movement of joints and muscles. Range-of-motion exercises should be started right away with the goal of helping you swiftly regain full movement in your shoulder. This includes the use of gentle stretching and motion through the full range available.
As your symptoms ease and strength improves, you will be guided in specialized exercises to improve posture, shoulder stability, and normal motor control. The desired final outcome is a return to full function. For athletes, this means full participation in sports activities.
In the later phase of rehab, the therapist will use a combination of kinetic chain exercises to decrease shear forces on the joint while enhancing strength. Plyometrics, a specific type of exercise to produce fast, powerful movements needed for sports performance will also be included.
You can return to your sporting activities when your muscles are back to nearly their full strength and control, you are not having swelling that comes and goes, and you aren’t having problems with the shoulder popping out of the joint.
After Surgery
Many shoulder reconstructive surgeries are now done on an outpatient basis. Patients go home the same day as the surgery. Some patients stay one or two nights in the hospital if necessary.
After any surgery to stabilize the shoulder your shoulder will be immobilized. You will probably wear a sling or hard brace for three to six weeks. A large abduction wedge under the armpit holds the arm in just the right position. The soft tissues must be given enough time to heal and form scar tissue to support and stabilize the shoulder joint.
Some studies are being done to investigate the use of early motion (within two to three days) after the operation. This accelerated rehab protocol has not been adopted routinely by all surgeons. Athletes may be most likely to try early rehab in order to return to sports participation as soon as possible. Functional recovery without immobilization has been proven possible. There is less postoperative pain with early motion.
Most doctors have their patients take part in formal physical therapy after shoulder reconstruction. You will probably be involved in a progressive functional rehabilitation program. The phases of rehabilitation include acute, early recovery, late recovery, and functional phase.
You should expect functional rehab to last four to six months after surgery. This will ensure the best result from your reconstruction. During the acute phase (one to three weeks), you may expect to see the physical therapist two to three times a week. The goal is to control pain and inflammation. The therapist will address any postural abnormalities and begin muscle re-education.
When you have minimal pain and adequate soft tissue healing, you’ll be advanced to the early recovery phase. This phase usually lasts from three to six weeks after the surgery. During this time, the therapist will work with you to increase motion, strength, and control.
When you have full, pain free motion and improved strength, then you’ll enter the late recovery phase. This phase extends from six to 12 weeks post-operatively. Improving strength, power, endurance, and dynamic kinetics (movement) is the main thrust of the late recovery phase.
The functional phase begins about three months after surgery. This phase is directed at the sports athlete. The therapist will put you through a series of drills designed to improve coordination, speed, and agility. In order to participate in this level of rehab, you must have normal range of motion, flexibility needed for your sport or activity, and 90 per cent of normal strength. You must also be free of symptoms during activities or sport-specific drills.