A Patient’s Guide to Shoulder Arthroscopy
Introduction
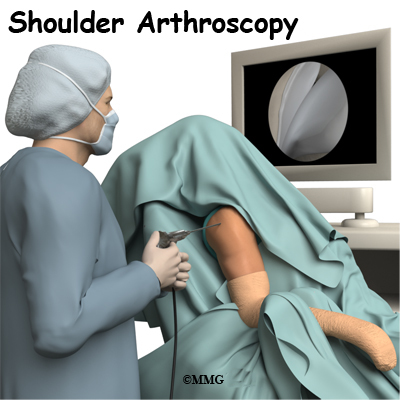
The use of arthroscopy (arthro means joint and scopy means look) has revolutionized many different types of orthopedic surgery. During a shoulder arthroscopy, a small video camera attached to a fiber-optic lens is inserted into the shoulder joint to allow a surgeon to see without making a large incision. Today the shoulder is one of the joints in which the arthroscope is commonly used to both diagnose problems and to perform surgical procedures inside the joint.
This guide will help you understand
- how the condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
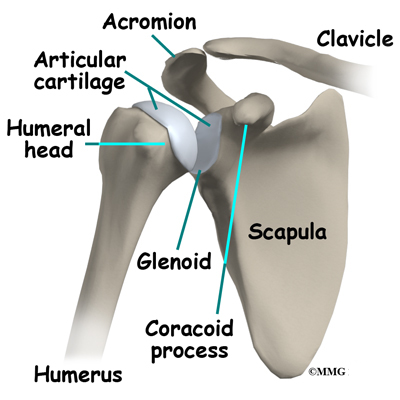
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone). A part of the scapula, called the glenoid, forms the socket of the shoulder. The glenoid is very shallow and flat, shaped somewhat like a dinner plate rather than a bowl. The humeral head forms the ball portion of the joint. Both the glenoid and the humeral head are covered with articular cartilage. Articular cartilage is the smooth, white material that covers the ends of bones in most joints. Articular cartilage provides a slick, rubbery surface that allows the bones to glide over each other as they move. Articular cartilage also functions as a shock absorber.
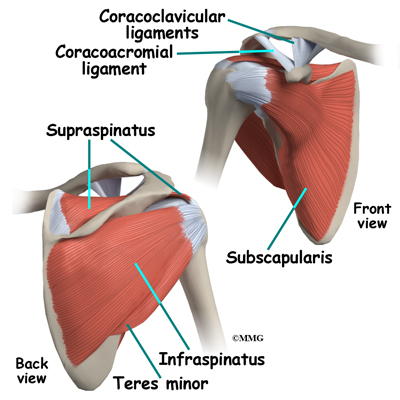
The rotator cuff connects the humerus to the scapula. The rotator cuff is formed by the tendons of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis. Tendons attach muscles to bones. Muscles move the bones by pulling on the tendons. The rotator cuff helps raise and rotate the arm. As the arm is raised, the rotator cuff also keeps the humerus tightly in the shoulder socket, the glenoid. The upper part of the scapula that makes up the roof of the shoulder is called the acromion.
The shoulder joint is surrounded by a water tight pocket called the joint capsule. This capsule is formed by the rotator cuff tendons, ligaments, connective tissue and synovial tissue. When the joint capsule is filled with sterile saline and is distended, the surgeon can insert the arthroscope into the pocket that is formed, turn on the lights and the camera and see inside the shoulder joint as if looking into an aquarium. The surgeon can see nearly everything that is inside the shoulder joint including: (1) the joint surfaces of the glenoid socket and the humeral head (2) the rotator cuff tendons, (3) the glenoid labrum and (4) the synovial lining of the joint.
The arthroscope can also be placed in the space outside the shoulder joint known as the subacromial bursa. This bursa is a water tight pocket that sits above the shoulder joint. By placing the arthroscope into this space, the surgeon can see the underside of the distal end of the clavicle (collarbone) and the acromion as well as the joint that is formed where the clavicle and acromion meet, the acromioclavicular (AC) joint.
Related Document: A Patient’s Guide to Shoulder Anatomy
Rationale
What does my surgeon hope to accomplish??
When shoulder arthroscopy first became widely available, it was used primarily to look inside the shoulder joint and make a diagnosis. Today, shoulder arthroscopy is used in performing a wide range of different types of surgical procedures on the shoulder joint including confirming a diagnosis, removing loose bodies, removing or repairing a torn labrum, reconstructing torn ligaments to prevent recurrent dislocation, repairing torn rotator cuff tendons and washing out debris from a shoulder that has become infected. Surgery can also be performed outside the joint in the subacromial bursa including removing bone spurs from the acromion and reconstructing an arthritic acromioclavicular joint.
Your surgeon’s goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeons ability to perform that procedure. The arthroscope image is magnified and allows the surgeon to see better and clearer. The arthroscope allows the surgeon to see and perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. But remember, the arthroscope is only a tool. The results that you can expect from a shoulder arthroscopy depend on what is wrong with your shoulder, what can be done inside your shoulder to improve the problem and your effort at rehabilitation after the surgery.
Preparations
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, ability to do your activities, and the movement and strength of each shoulder.
A second purpose of the preoperative visit is to prepare you for surgery. The therapist will teach you the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted for surgery early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during shoulder arthroscopy?
Before surgery you will be placed under either general anesthesia or a type of regional anesthesia. In simple cases, local anesthesia may be adequate. Sterile drapes are placed to create a sterile environment for the surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments.
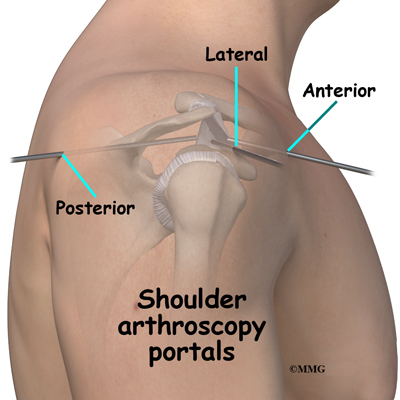
The surgeon begins the operation by making two or three small openings into the shoulder, called portals. These portals are where the arthroscope and surgical instruments are placed inside the shoulder joint. Care is taken to protect the nearby nerves and blood vessels. A small metal or plastic tube (or cannula) will be placed through one of the portals to inflate the shoulder joint with sterile saline.
The arthroscope is a small fiber-optic tube that is used to see and operate inside the joint. The arthroscope is a small metal tube about 1/4 inch in diameter (slightly smaller than a pencil) and about seven inches in length. The fiber-optics inside the metal tube of the arthroscope allows a bright light and TV camera to be connected to the outer end of the arthroscope. The light shines through the fiber-optic tube and into the shoulder joint. A TV camera is attached to the lens on the outer end of the arthroscope.
The TV camera projects the image from inside the shoulder joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the shoulder) while moving the arthroscope to different places inside the shoulder joint.
Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be one with much smaller incisions. For example, simple removal of a torn labrum or loose body can be done using two or three small 1/4 inch incisions. More extensive surgical procedures such as ligament reconstruction or rotator cuff repair may require larger incisions.
Once the surgical procedure is complete, the arthroscopic portals and surgical incisions will be closed with sutures or surgical staples. A bandage will be applied to the shoulder. Once the bandage has been placed, you will be taken to the recovery room.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur during shoulder arthroscopy. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following shoulder arthroscopy are
- anesthesia complications
- thrombophlebitis
- infection
- equipment failure
- slow recovery
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
Animation of DVT…View animation
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following shoulder arthroscopy, it is possible that a postoperative infection may occur. This is very uncommon and happens in less than 1% of cases. You may experience increased pain, swelling, fever and redness, or drainage from the incisions. You should alert your surgeon if you think you are developing an infection.
Infections are of two types: superficial or deep. A superficial infection may occur in the skin around the incisions or portals. A superficial infection does not extend into the joint and can usually be treated with antibiotics alone. If the shoulder joint itself becomes infected, this is a serious complication and will require antibiotics and possibly another surgical procedure to drain the infection.
Equipment Failure
Many of the instruments used by the surgeon to perform shoulder arthroscopy are small and fragile. These instruments can be broken resulting in a piece of the instrument floating inside of the shoulder joint. The broken piece is usually easily located and removed, but this may cause the operation to last longer than planned. There is usually no damage to the shoulder joint due to the breakage.
Different types of surgical devices (screws, pins, and suture anchors) are used to hold tissue in place during and after arthroscopy. These devices can cause problems. If one breaks, the free-floating piece may hurt other parts inside the shoulder joint, particularly the articular cartilage. The end of the tissue anchor may poke too far through tissue and the point may rub and irritate nearby tissues. A second surgery may be needed to remove the device or fix problems with these devices.
Slow Recovery
Not everyone gets quickly back to routine activities after shoulder arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the shoulder without making large incisions. How fast you recover from shoulder arthroscopy depends on what type of surgery was done inside your shoulder.
Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the shoulder ligaments, rotator cuff tendons, or articular cartilage tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss this with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic shoulder surgery.
After Surgery
What happens after surgery?
Shoulder arthroscopy is usually done on an outpatient basis meaning that patients go home the same day as the surgery. More complex reconstructions that require larger incisions and surgery that alters bone may require a short stay in the hospital to control pain more aggressively and monitor the situation more carefully. You may also begin physical therapy while in the hospital.
The portals are covered with surgical strips, the larger incisions may have been repaired with either surgical staples or sutures and may be covered with a bandage.
Patients who have had more complex reconstructive surgery may need to wear a sling or shoulder immobilizer for several weeks. The shoulder immobilizer helps to protect the healing tissue inside the shoulder joint. You may be allowed to remove the brace at times during the day to do gentle range-of-motion exercises and bathe.
Rehabilitation
What will my recovery be like?
Your rehabilitation will depend on the type of surgery required. You may not need formal physical therapy after simple procedures. Some patients may simply do exercises as part of a home program after some simple instructions. But, many surgeons have patients take part in formal physical therapy after any type of shoulder arthroscopy procedure. Generally speaking, the more complex the surgery the more involved and prolonged your rehabilitation program will be. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery.
Today, the arthroscope is used to perform quite complicated major reconstructive surgery using very small incisions. Remember, just because you have small incisions on the outside, there may be a great deal of healing tissue on the inside of the shoulder joint. If you have had major reconstructive surgery, you should expect full recovery to take several months. Your physical therapist’s goal is to help you keep your pain under control and improve the range of motion and strength of your shoulder. When you are well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.