A Patient’s Guide to Lumbar Spinal Stenosis
Introduction
According to the North American Spine Society (NASS), spinal stenosis describes a clinical syndrome of buttock or leg pain. These symptoms may occur with or without back pain. It is a condition in which the nerves in the spinal canal are closed in, or compressed. The spinal canal is the hollow tube formed by the bones of the spinal column. Anything that causes this bony tube to shrink can squeeze the nerves inside. As a result of many years of wear and tear on the parts of the spine, the tissues nearest the spinal canal sometimes press against the nerves. This helps explain why lumbar spinal stenosis (stenosis of the low back) is a common cause of back problems in adults over 55 years old.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the back is involved?
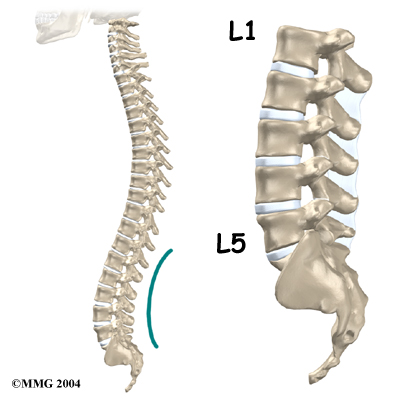
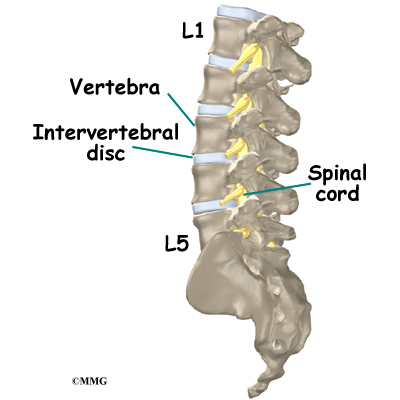
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the spinal column. The spinal column gives the body its form. It is the body’s main upright support.
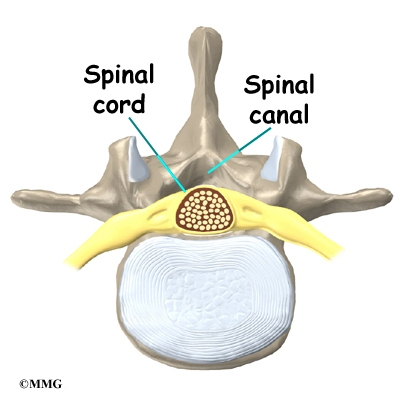
The back portion of the spinal column forms a bony ring. When the vertebrae are stacked on top of each other, these bony rings create a hollow tube. This bony tube, called the spinal canal, surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
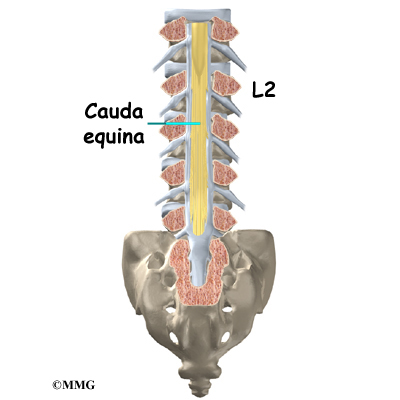
The spinal cord only extends to the second lumbar (low back) vertebra. Below this level, the spinal canal encloses a bundle of nerves that go to the lower limbs and pelvic organs. The Latin term for this bundle of nerves is cauda equina, meaning horse’s tail.
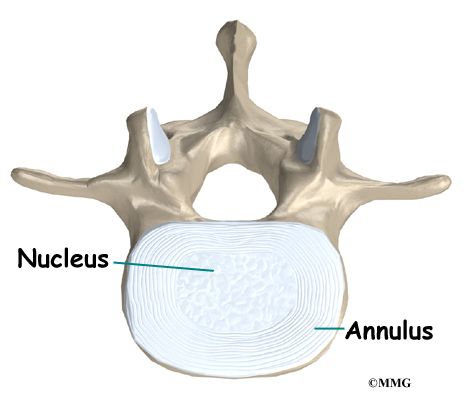
An intervertebral disc fits between each vertebral body and provides a space between the spine bones. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during heavy activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
Why do I have this problem?
In the lumbar spine, the spinal canal usually has more than enough room for the spinal nerves. The canal is normally 17 to 18 millimeters around, slightly smaller than a penny. Spinal stenosis develops when the canal shrinks to 12 millimeters or less. When the size drops below 10 millimeters, severe symptoms of lumbar spinal stenosis occur.
There are many reasons why symptoms of spinal stenosis develop. Some of the more common reasons include
- congenital stenosis (being born with a small spinal canal)
- spinal degeneration
- spinal instability
- disc herniation
Congenital stenosis: Some people are born with (congenital) a spinal canal that is narrower than normal. They may not feel problems early in life. However, having a narrow spinal canal puts them at risk for stenosis. Even a minor back injury can cause pressure against the spinal cord. People born with a narrow spinal canal often have problems later in life, because the canal tends to become narrower due to the effects of aging.
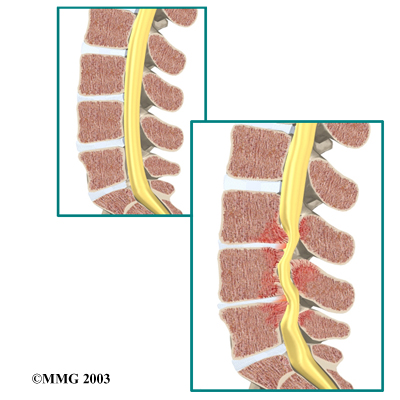
Degeneration: Degeneration is the most common cause of spinal stenosis. Wear and tear on the spine from aging and from repeated stresses and strains can cause many problems in the lumbar spine. The intervertebral disc can begin to collapse, and the space between each vertebrae shrinks. Bone spurs may form that stick into the spinal canal and reduce the space available to the spinal nerves. The ligaments that hold the vertebrae together may thicken and also push into the spinal canal. All of these conditions cause the spinal canal to narrow.
View animation of degeneration
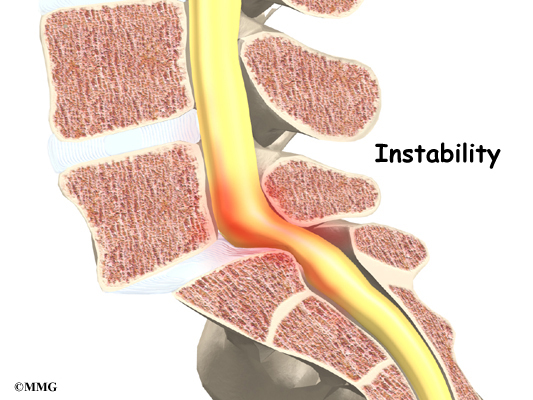
Spinal instability: Spinal instability can cause spinal stenosis. Spinal instability means that the bones of the spine move more than they should. Instability in the lumbar spine can develop if the supporting ligaments have been stretched or torn from a severe back injury. People with diseases that loosen their connective tissues may also have spinal instability. Whatever the cause, extra movement in the bones of the spine can lead to spinal stenosis.
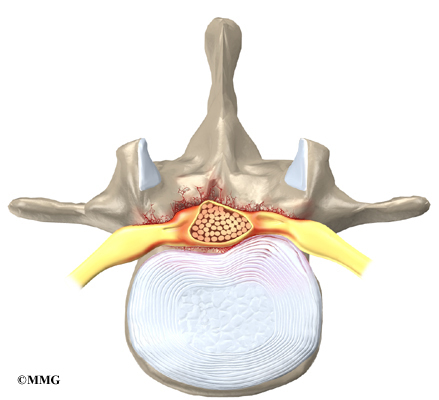
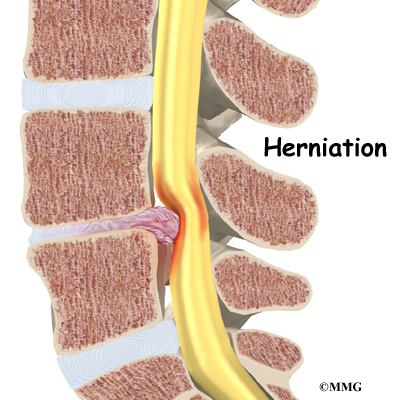
Disc herniation: Spinal stenosis can occur when an intervertebral disc in the low back herniates (ruptures). Normally, the shock-absorbing disc is able to handle the downward pressure of gravity and the strain from daily activities. However, if the pressure on the disc is too strong, such as landing from a fall in a sitting position, the nucleus inside the disc may rupture through the outer annulus and squeeze out of the disc. This is called a disc herniation. If an intervertebral disc herniates straight backward, it can press against the nerves in the spinal canal, causing symptoms of spinal stenosis.
Symptoms
What does the spinal stenosis feel like?
Spinal stenosis usually develops slowly over a long period of time. This is because the main cause of spinal stenosis is spinal degeneration in later life. Symptoms rarely develop quickly when degeneration is the source of the problem. A severe injury or a herniated disc may cause symptoms to develop immediately.
Patients with stenosis don’t always feel back pain. Primarily, they have severe pain and weakness in their legs, usually in both legs at the same time. Some people say they feel that their legs are going to give out on them.
Symptoms mainly affect sensation in the lower limbs. Nerve pressure from stenosis can cause a feeling of pins and needles in the skin where the spinal nerves travel. Reflexes become slowed. Some patients report charley horses in their leg muscles. Others report strange sensations like water trickling down their legs.
Symptoms change with the position of the low back. Flexion (bending forward) widens the spinal canal and usually eases symptoms. That’s why people with stenosis tend to get relief when they sit down or curl up to sleep. Activities such as reaching up, standing, and walking require the spine to straighten or even extend (bend back slightly). This position of the low back makes the spinal canal smaller and often worsens symptoms.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history and physical examination. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities. This will include questions about your pain or if you have feelings of numbness or weakness in your legs.
Your doctor will also want to know whether your symptoms are worse when you’re up standing or walking and if they go away when you sit down. If your pain does not get worse when walking, then you probably don’t have stenosis. There may be some other cause of the painful symptoms.
The doctor does a physical examination to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested. A wide-based gait (legs far apart) is often observed. Special clinical tests can be done such as the Romberg test, hip extension test, and tests of neuromuscular function.
The Romberg test is a neurologic test for joint proprioception (sense of position). The nerve pathways for this sensation travel up the dorsal columns of the spinal cord. Dorsal means they are located towards the back where stenosis is more likely to occur. The test is done standing with feet together, eyes open, and hands by your sides. You will be asked to close your eyes for one full minute while your doctor observes you. Romberg’s test is positive if you can stand with your eyes open but fall (or start to fall, someone will be there to make sure you don’t fall down) when your eyes are closed. The test is not positive if you start to sway with your eyes closed but don’t lose your balance.
X-rays can show if the problems are from changes in the bones of the spine. The images can show if degeneration has caused the space between the vertebrae to collapse. X-rays may also show any bone spurs sticking into the spinal canal.
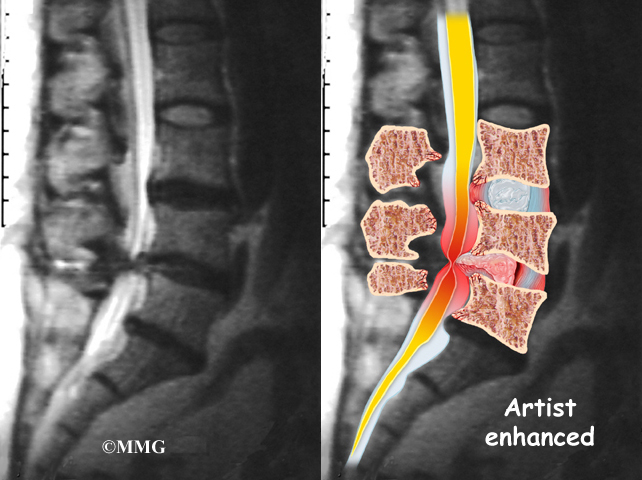
The best way to see the effects and extent of lumbar spinal stenosis is with a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the spinal canal and whether the nerves inside are being squeezed. This machine creates pictures that look like slices of the area your doctor is interested in. The test does not require dye or a needle.
Computed tomography (a CT scan) may be ordered for those patients who can’t have an MRI for some reason, when the results of the MRI are unclear, or symptoms don’t match the MRI findings. The CT scan is a detailed X-ray that lets your doctor see slices of bone tissue. The image can show any bone spurs that may be sticking into the spinal column and taking up space around the spinal nerves.
When there is a concern about neurologic problems, doctors may recommend electrodiagnostic tests of the nerves that go to the legs and feet. An electromyogram (EMG) checks whether the motor pathway of a nerve is working correctly. Motor impulses travel down the nerve and work to energize muscles.
Doctors may also order a somatosensory evoked potential (SSEP) test to locate more precisely where the spinal nerves are being squeezed. The SSEP is used to measure nerve sensations. These sensory impulses travel up the nerve, informing the body about sensations such as pain, temperature, and touch. The function of a nerve is recorded by an electrode placed over the skin in the area where the nerve travels.
Not all causes of spinal stenosis are from degenerative conditions. Doctors use blood tests to determine whether symptoms are coming from other conditions, such as arthritis or infection.
Treatment
What treatment options are available?
Nonsurgical Treatment
Unless your condition is causing significant problems or is rapidly getting worse, most doctors will begin with nonsurgical treatments. Up to one-half of all patients with mild-to-moderate lumbar spinal stenosis can manage their symptoms with conservative (nonsurgical) care. Neurologic decline and paralysis in this group is rare.
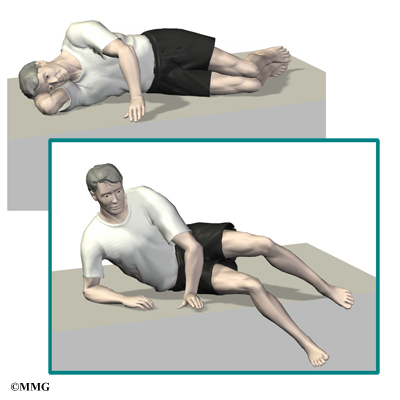
At first, doctors may prescribe ways to immobilize the spine. Keeping the back still for a short time can calm inflammation and pain. This might include one to two days of bed rest. Patients may find that curling up to sleep or lying back with their knees bent and supported gives the greatest relief. These positions flex the spine forward, which widens the spinal canal and can ease symptoms.
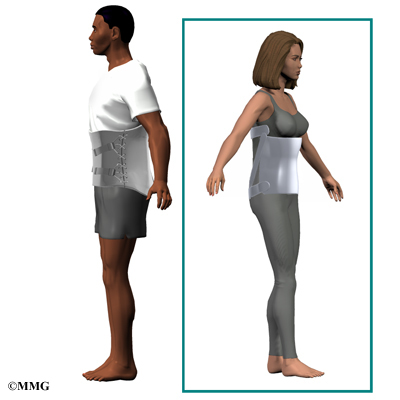
A lumbar support belt or corset may be prescribed, though their benefits are controversial. Lumbosacral corsets do not appear to offer any long-term benefits. The support provides symptom relief only while you are wearing it. The support can limit pressure in the discs and prevent extra movement in the spine. But it can also cause the back and abdominal muscles to weaken. Some doctors have their patients wear a rigid brace that holds the spine in a slightly flexed position, widening the spinal canal. Health care providers normally only have patients wear a corset for one to two weeks.
Doctors sometimes prescribe medication for patients with spinal stenosis. Patients may be prescribed anti-inflammatory medication such as nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin. These medications can cause side effects in the kidneys and gastrointestinal tract. Also, because most stenosis patients are elderly, doctors closely monitor patients who are using these medications to avoid complications.
Narcotic drugs, such as codeine or morphine, are generally not prescribed for stenosis patients. They are addictive when used too much or improperly. Muscle relaxants are occasionally used to calm muscles in spasm.
Symptoms of stenosis can lead to mood changes. As a result, doctors sometimes prescribe anti-depressant medication, called tricyclics. Tricyclics help steady peoples’ moods, and some tricyclics even improve sleep by helping the body make an important hormone called serotonin. These medications also seem to calm back pain by affecting the membranes around pain nerves.
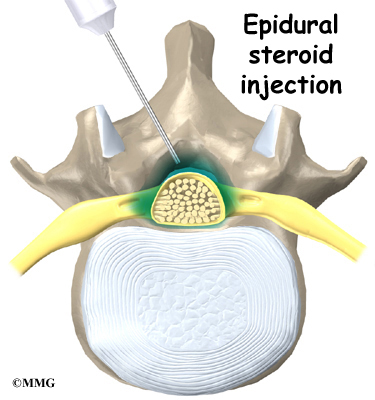
Some patients are given an epidural steroid injection (ESI). The spinal cord is covered by a material called dura. The space between the dura and the spinal column is called the epidural space. It is thought that injecting steroid medication into this space fights inflammation around the nerves, the discs, and the facet joints. This can reduce swelling and give the nerves more room inside the spinal canal.
Research shows that a single steroid injection offers only short-term relief. Multiple injections can produce long-term, lasting pain relief. Epidural injections should be given using contrast-enhanced fluoroscopy. Fluoroscopy is an imaging technique used by the surgeon to guide the needle to the right spot during the procedure. This type of imaging improves the accuracy of medication delivery.
Patients often work with a physical therapist. By evaluating your condition, your therapist can assign positions and exercises to ease your symptoms. Your therapist may suggest using traction. Traction is a common treatment for stenosis. It gently stretches the low back, taking pressure off the spinal nerves. Your therapist may also suggest strengthening and aerobic exercises. Strengthening exercises focus on improving the strength and control of the back and abdominal muscles. Aerobic exercises are used to improve heart and lung health and increase endurance in the spinal muscles. Stationary biking offers a good aerobic treatment and keeps the spine bent slightly forward, a position affording relief to many patients with lumbar stenosis.
Surgery
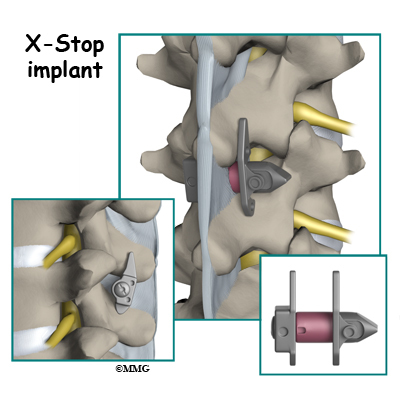
If the symptoms you feel are mild and there is no danger they’ll get worse, surgery is not usually recommended. Some patients may benefit from the use of a device called the X-STOP®. The X-STOP® is a metal implant made of titanium. The implant is inserted through a small incision in the skin of your back. It is designed to fit between the spinous processes of the vertebrae in your lower back. It stays in place permanently without attaching to the bone or ligaments in your back.
There are several advantages of the X-STOP®. It can be inserted using local anesthesia on an outpatient basis. A small incision is made so the procedure is minimally invasive and no bone or soft tissue is removed. The implant is not close to nerves or the spinal cord. With the implant in place, you won’t have to bend forward to relieve your symptoms. The X-STOP® keeps the space between your spinous processes open. With the implant in place, you stand upright without pinching the nerves in your back.
But for anyone with severe symptoms of lumbar spinal stenosis, surgery may be needed. When there are signs that pressure is building on the spinal nerves, decompressive surgery may be required, sometimes right away. Decompression means that bone and/or soft tissue are removed from around the spinal nerves to take the pressure off. The signs doctors watch for when reaching this decision include weakening in the leg muscles, pain that won’t ease up, and problems with the bowels or bladder.
Pressure on the spinal nerves can cause a loss of control in the bowels or bladder. This is an emergency. If the pressure isn’t relieved, it can lead to permanent paralysis of the bowels and bladder. Surgery is recommended to remove pressure from the nerves.
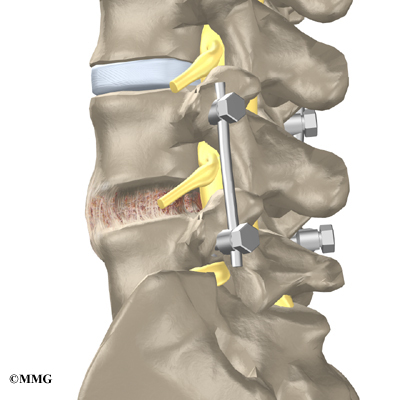
The main surgical procedure used to treat spinal stenosis is lumbar laminectomy. Some patients also require fusion surgery immediately after the laminectomy procedure if spinal instability is present.
Lumbar Laminectomy
The lamina is the covering layer of the bony ring of the spinal column. It forms a roof-like structure over the back of the spinal canal. When the nerves in the spinal canal are being squeezed by a herniated disc or bone spurs, a lumbar laminectomy removes the entire lamina to release pressure on the spinal nerves. This is the primary type of surgery used for lumbar spinal stenosis.
Related Document: A Patient’s Guide to Lumbar Laminectomy
Posterior Lumbar Fusion
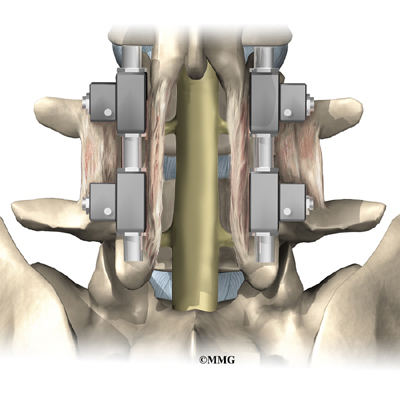
A posterior lumbar fusion may be needed after a surgeon performs a lumbar laminectomy. The fusion procedure is recommended when a spinal segment has become loose or unstable.
A fusion surgery joins two or more bones into one solid bone. This keeps the bones and joints from moving. In this procedure, the surgeon lays small grafts of bone over the back of the spine. Most surgeons also apply metal plates and screws to prevent the two vertebrae from moving.
This protects the graft so it can heal better and faster.
Related Document: A Patient’s Guide to Posterior Lumbar Fusion
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Even if you don’t need surgery, your doctor may recommend that you work with a physical or occupational therapist. Patients are normally seen a few times each week for one to two months. In severe cases, patients may need a few additional weeks of care.
Your therapist creates a program to help you regain back movement, strength, endurance, and function. Treatments for lumbar spinal stenosis often include lumbar traction, described earlier. Hands-on treatments such as massage and specialized forms of soft-tissue mobilization may be used initially. They are used to help you begin moving with less pain and greater ease. Therapists also guide patients in a program of exercise designed to widen the spinal canal and take pressure off the spinal nerves.
It is important to improve the strength and coordination in the abdominal and low back muscles. Your therapist can also evaluate your workstation or the way you use your body when you do your activities and suggest changes to avoid further problems.
After Surgery
After surgery, surgeons may have their patients work with a physical or occupational therapist. Patients who’ve had fusion surgery normally need to wait two to three months before beginning a rehabilitation program. They will probably need to attend therapy sessions for six to eight weeks and should expect full recovery to take up to six months.
During therapy after surgery, the therapist may use treatments such as heat or ice, electrical stimulation, and massage to help calm pain and muscle spasm. Then patients begin learning how to move safely with the least strain on their healing back.
As the rehabilitation program evolves, patients do more challenging exercises. The goal is to safely advance strength and function. As the therapy sessions come to an end, therapists help patients get back to the activities they enjoy.
Ideally, patients are able to resume normal activities. Patients may need guidance on which activities are safe or how to change the way they go about certain activities.
When treatment is well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource. But patients are in charge of doing their exercises as part of an ongoing home program.