A Patient’s Guide to Lumbar Facet Joint Arthritis
Introduction
Arthritis of the lumbar facet joints can be a source of significant low back pain. Aligned on the back of the spinal column, the facet joints link each vertebra together. Articular cartilage covers the surfaces where these joints meet. Like other joints in the body that are covered with articular cartilage, the lumbar facet joints can be affected by arthritis.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the back is involved?
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the spinal column. The spinal column gives the body its form. It is the body’s main upright support.
The back portion of the spinal column forms a bony ring. When the vertebrae are stacked on top of each other, these bony rings create a hollow tube. This tube, called the spinal canal, surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
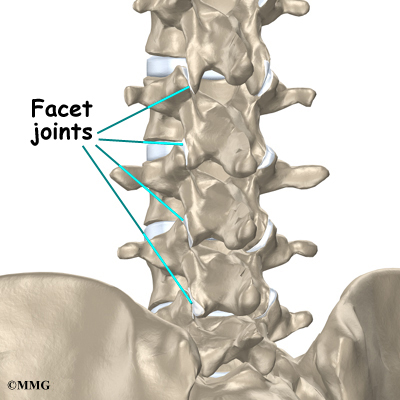
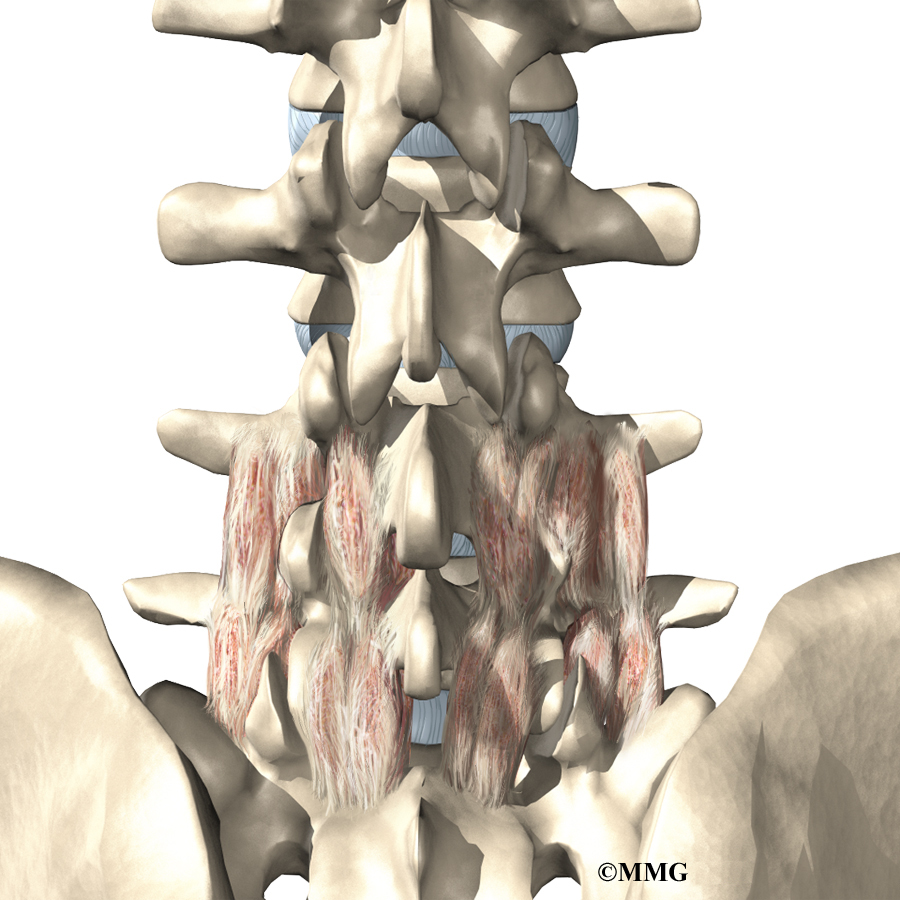
Between the vertebrae of each spinal segment are two facet joints. The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
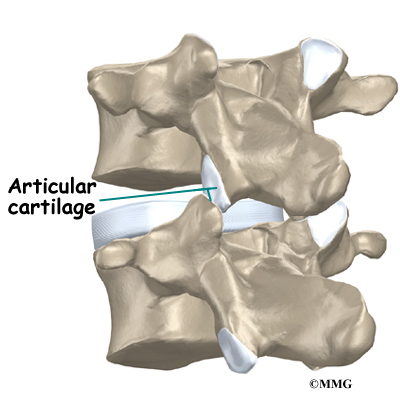
The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the bone ends to move against each other smoothly, without friction.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
Why do I have this problem?
Normally, the facet joints fit together snugly and glide smoothly, without pressure. If pressure builds where the joint meets, the cartilage on the joint surfaces wears off, or erodes.
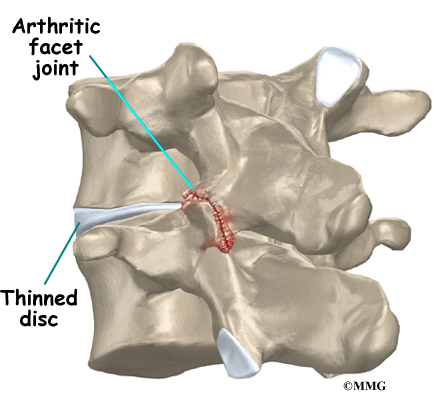
Each segment in the spine has three main points of movement, the intervertebral disc and the two facet joints. Injury or problems in any one of these structures affects the other two. As a disc thins with aging and from daily wear and tear, the space between two spinal vertebrae shrinks. This causes the facet joints to press together.
Facet joints can also become arthritic due to a back injury earlier in life. Fractures, torn ligaments, and disc problems can all cause abnormal movement and alignment, putting extra stress on the surfaces of the facet joints.
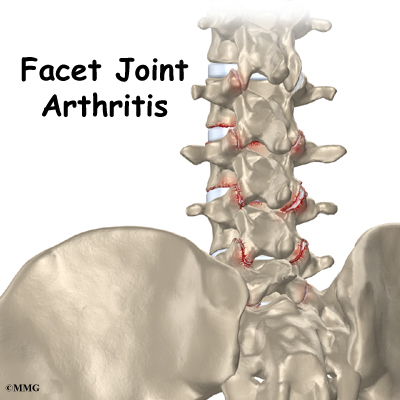
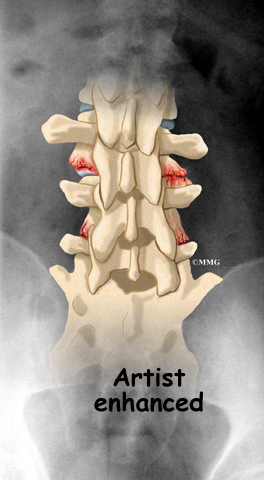
The body responds to this extra pressure by developing bone spurs. As the spurs form around the edges of the facet joints, the joints become enlarged. This is called hypertrophy. Eventually, the joint surfaces become arthritic. When the articular cartilage degenerates, or wears away, the bone underneath is uncovered and rubs against bone. The joint becomes inflamed, swollen, and painful.
View animation of facet arthritis
Facet joint arthritis develops slowly over a long period of time. This is partly because spinal degeneration in later life is the main cause of facet joint arthritis. Symptoms rarely develop immediately when degeneration is causing the problems. However, rapid movements, heavy twisting, or backward motions in the low back can injure a facet joint, leading to immediate symptoms.
Symptoms
What does the condition feel like?
Pain from facet joint arthritis is usually worse after resting or sleeping. Also, bending the trunk sideways or backward usually produces pain on the same side as the arthritic facet joint. For example, if you lie on your stomach on a flat surface and raise your upper body, you hyperextend the spine. This increases pressure on the facet joints and can cause pain if there is facet joint arthritis.
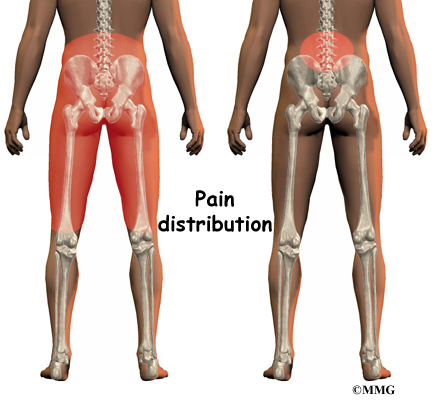
Pain may be felt in the center of the low back and can spread into one or both buttocks. Sometimes the pain spreads into the thighs, but it rarely goes below the knee. Numbness and tingling, the symptoms of nerve compression, are usually not felt because facet arthritis generally causes only mechanical pain. Mechanical pain comes from abnormal movement in the spine.
However, symptoms of nerve compression can sometimes occur at the same time as the facet joint pain. The arthritis can cause bone spurs at the edges of the facet joint. These bone spurs may form in the opening where the nerve root leaves the spinal canal. This opening is called the neural foramen. If the bone spurs rub against the nerve root, the nerve can become inflamed and irritated. This nerve irritation can cause symptoms where the nerve travels. These symptoms may include numbness, tingling, slowed reflexes, and muscle weakness.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history and physical examination. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities. This will include questions about where you feel pain and if you have numbness or weakness in your legs. Your doctor will also want to know what positions or activities make your symptoms worse or better.
Then the doctor performs a physical exam to determine which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested.
X-rays can show if there are problems in the bone tissue in and near the facet joints. The images can show if degeneration has caused the space between the vertebrae to collapse and may show if bone spurs have developed near the facet joints.
When more information is needed, your doctor may order magnetic resonance imaging (MRI). The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the facet joints to see whether they are enlarged or swollen. This machine creates pictures that look like slices of the area your doctor is interested in. The test does not require dye or a needle.
A computed tomography (CT) scan may be ordered. This is a detailed X-ray that lets your doctor see slices of bone tissue. The image can show whether the surface of the joint has eroded and whether bone spurs have developed.
A diagnostic injection may be used to locate the source of pain. The doctor uses a long needle to inject a local anesthetic (numbing medication) into either the joint or into the nerve that goes to the joint. The doctor watches the needle on a fluoroscope to make sure it reaches the correct spot. A fluoroscope is a special X-ray television that allows the doctor to see your spine and the needle as it moves. Once the doctor is sure the needle is in the right place, the medicine and a special dye are injected. The doctor watches the dye to make sure the medication is correctly placed. The results from the injection help the doctor make the diagnosis. If pain goes away, it helps confirm the source of pain.
Treatment Options
What treatment options are available?
Nonsurgical Treatment
Facet joint arthritis is mainly treated nonsurgically. At first, doctors may prescribe a short period of rest, one to two days at most, to calm inflammation and pain. Patients may find added relief by curling up to sleep on a firm mattress or by lying back with their knees bent and supported. These positions take pressure off the facet joints.
Your doctor may prescribe anti-inflammatory medication, such as a nonsteroidal anti-inflammatory drug (NSAID) or aspirin. Muscle relaxants are occasionally used to calm muscles that are in spasm. Oral steroid medicine in tapering dosages may also be prescribed for pain.
Patients often work with a physical therapist. By evaluating a patient’s condition, the therapist can assign positions and exercises to ease symptoms. The therapist may recommend traction. Traction is a common treatment for this condition. It gently stretches the low back and takes pressure off the facet joints. The therapist may also prescribe strengthening and aerobic exercises. Strengthening exercises focus on improving the strength and control of the back and abdominal muscles. Aerobic exercises are used to improve heart and lung health and increase endurance in the spinal muscles. Stationary biking offers a good aerobic treatment and keeps the spine bent slightly forward, a position that gives relief to many patients with lumbar facet joint arthritis.
Patients who still have pain after trying various treatments may require injections into the facet joint or the small nerves that go to the joint. An anesthetic is used to block pain coming from the facet joint. The procedure to inject the medication into the joint is similar to the diagnostic injection described earlier. A steroid medication is occasionally used instead of the anesthetic. There is no strong evidence that these injections work. However, they seem to have some good short-term results with few side effects, so they shouldn’t be abandoned completely. Doctors often have their patients resume physical therapy treatments following an injection.
Related Document: A Patient’s Guide to Facet Joint Injections
Surgery
People with facet joint arthritis rarely need surgery. However, facet joint arthritis is a primary source of chronic low back pain about 15 percent of the time. After trying other types of treatment, some of these patients may eventually require surgery. There are several types of surgery for facet joint arthritis. The two primary operations are
- facet rhizotomy
- posterior lumbar fusion
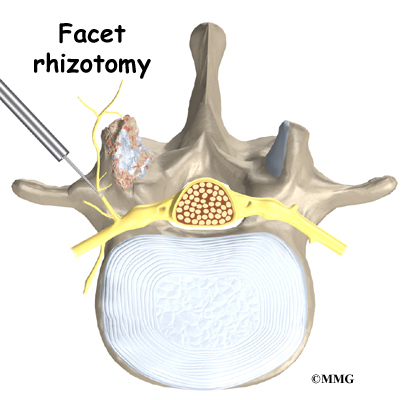
Facet Rhizotomy
Rhizotomy describes a surgical procedure in which a nerve is purposely cut or destroyed. Facet rhizotomy involves severing one of the small nerves that goes to the facet joint. The intent of the procedure is to stop the transmission of pain impulses along this nerve. The nerve is identified using a diagnostic injection (described earlier). Then the surgeon inserts a large, hollow needle through the tissues in the low back. A special probe is inserted through the needle, and a fluoroscope is used to guide the probe toward the nerve. The probe is slowly heated until the nerve is severed.
Posterior Lumbar Fusion
Facet joint arthritis mainly causes mechanical pain, the type of pain caused by wear and tear in the parts of the lumbar spine. Posterior lumbar fusion for facet joint arthritis is mainly used to stop movement of the painful joints by joining two or more vertebrae into one solid bone (fusion). This keeps the bones and painful facet joints from moving.
In this procedure, the surgeon lays small grafts of bone over the back of the spine. Most surgeons will also apply metal plates and screws to prevent the two vertebrae from moving. This protects the graft so it can heal better and faster.
Related Document: A Patient’s Guide to Posterior Lumbar Fusion
Rehabilitation
Nonsurgical Rehabilitation
Even if you don’t need surgery, your doctor may recommend that you work with a physical therapist. Patients are normally seen a few times each week for four to six weeks. In severe and chronic cases, patients may need a few additional weeks of care.
Therapists create programs to help patients regain back movement, strength, endurance, and function. Treatments for facet joint arthritis often include lumbar traction, described earlier. Hands-on treatments such as massage and specialized forms of soft-tissue mobilization may be used initially. They are used to help patients begin moving with less pain and greater ease.
Spinal manipulation can sometimes provide short-term relief of pain from facet arthritis. Commonly thought of as an adjustment, spinal manipulation stretches the tissues surrounding the facet joint and helps reset the sensitivity of the spinal nerves and muscles. It involves a high-impulse stretch of the spinal joints and is characterized by the sound of popping as the stretch is done. However, it doesn’t seem to provide effective long-term help when used routinely for chronic conditions.
Patients are shown how to improve strength and coordination in the abdominal and low back muscles. Therapists can also evaluate their patients’ workstations or the way they use they use their bodies when they do their activities.
After Surgery
Outpatient physical therapy is usually prescribed only for patients who have extra pain or show significant muscle weakness and deconditioning.
Patients usually don’t require physical therapy after facet rhizotomy. Surgeons may prescribe a short period of therapy when patients have lost muscle tone in their back and abdominal muscles, when they have problems controlling pain, or when they need guidance about returning to work.
If patients require formal rehabilitation after facet rhizotomy, they will probably only need to attend sessions for two to four weeks. They should expect full recovery to take up to three months.
Patients who have had lumbar fusion surgery normally need to wait at least six weeks before beginning a rehabilitation program. They typically need to attend therapy sessions for six to eight weeks and should expect full recovery to take up to six months.
During therapy after surgery, the therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. Then patients begin learning how to move safely with the least strain on the healing back.
As the rehabilitation program evolves, patients do more challenging exercises. The goal is to safely advance strength and function.
As the therapy sessions come to an end, the therapist helps patients get back to the activities they enjoy. Ideally, patients are able to resume normal activities. They may need guidance on which activities are safe or how to change the way they go about their activities.
When treatment is well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource. But patients are in charge of doing their exercises as part of an ongoing home program.