A Patient’s Guide to Intersection Syndrome
Introduction
Intersection syndrome is a painful condition of the forearm and wrist. It can affect people who do repeated wrist actions, such as weight lifters, downhill skiers, and canoeists. Heavy raking or shoveling can also cause intersection syndrome.
This guide will help you understand
- what part of your forearm is causing the problem
- what may have caused this condition
- what can be done to stop the pain
Anatomy
What part of the forearm is causing my pain?
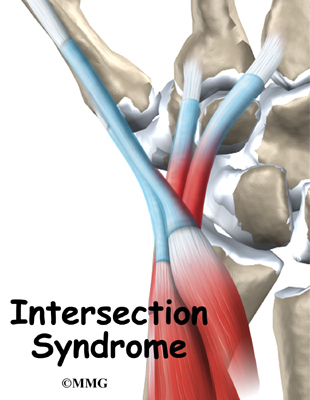
The pain from intersection syndrome is usually felt on the top of the forearm, about three inches above the wrist. At this spot, two muscles that connect to the thumb cross over (or intersect) the two underlying wrist tendons (tendons connect muscles to bones).
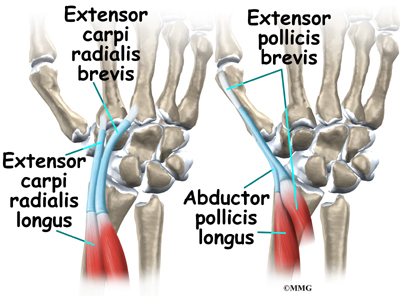
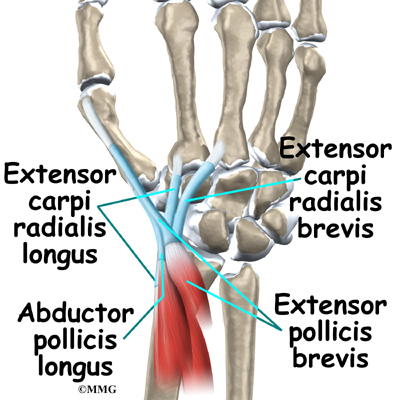
The two muscles that cross over the wrist tendons control the thumb. They are the extensor pollicis brevis and the abductor pollicis longus. These two muscles start on the forearm, cross over the two wrist tendons,
and connect on the back part of the thumb. When these muscles work, they pull the thumb out and back.
The extensor carpi radialis brevis and the extensor carpi radialis longus muscles run lengthwise along the back of the forearm. The tendons of these two muscles attach on the back of the hand. The action of these two wrist tendons pulls the wrist back, into extension.
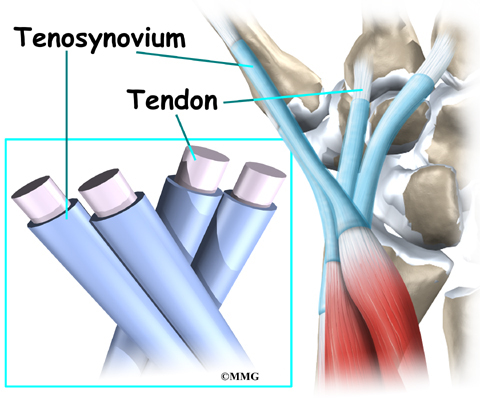
Most of the tendons around the wrist are covered with a thin tissue called tenosynovium. Tenosynovium is very slippery. It allows tendons to glide against one another and the surrounding muscles, fat, and skin with very little friction.
Related Document: A Patient’s Guide to Wrist Anatomy
Causes
What caused my condition?
If you overuse the wrist extensor tendons, the slippery tenosynovial lining may become inflamed from the constant rubbing against the two thumb muscles. As the tenosynovium becomes more irritated and inflamed, it swells and thickens. You feel pain when you move your wrist because the swollen tendons are rubbing against the thumb muscles.
Wrist extensor tendons work like the bow used by violin players. The wrist extensor tendons are like the bow, and the thumb muscles are like the strings. As the wrist curls down and in, the wrist tendons rub back and forth against the thumb muscles. The friction builds up, much like the effect of rubbing two sticks together. This leads to irritation and inflammation of the tenosynovium covering the wrist extensor tendons.
The wrist extensor tendons are strained by any activities that cause the wrist to curl down and in, toward the thumb. These wrist movements are especially common in downhill skiers when they plant their ski poles deeply in powder snow. The same movement is involved when pulling a rake against hard ground. Racket sports, weight lifting, canoeing, and rowing can also stress the wrist extensor tendons.
Symptoms
What does intersection syndrome feel like?
The friction on the wrist tendons causes pain and swelling in the tenosynovium that covers the tendons. The friction hampers the smooth gliding action. You may hear a squeaking sound and feel creaking as the tendons rub against the muscles. This is called crepitus. You may have swelling and redness at the intersection point. Pain can spread down to the thumb or up along the edge of the forearm.
Diagnosis
What tests will my doctor run?
Doctors usually make the diagnosis of intersection syndrome during a physical examination. Most of the time no special tests are required.
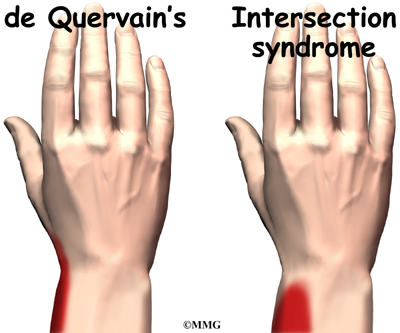
The main challenge is distinguishing intersection syndrome from de Quervain’s tenosynovitis. De Quervain’s tenosynovitis is a condition that is very similar to intersection syndrome.
Related Document: A Patient’s Guide to de Quervain’s Tenosynovitis
Both syndromes involve inflammation in the tendons of the wrist. However, the pain begins in different spots. Intersection syndrome causes pain at the intersection point, about three inches up the forearm. De Quervain’s tenosynovitis causes pain along the edge of the wrist, closer to the hand. Your doctor will examine your forearm and wrist carefully to locate exactly where your pain is coming from.
Treatment
What treatment options are available?
Nonsurgical Treatment
It is most important to stop or change activities that are causing your symptoms. Take frequent breaks when doing repeated hand and thumb movements. Avoid repetitive hand motions such as heavy grasping, wringing, or turning and twisting movements of the wrist. Downhill skiers may get relief by avoiding heavy planting and dragging of their ski poles and by getting a shorter pole with a smaller basket diameter.
Keep your wrist in a neutral alignment. In other words, keep it in a straight line with your arm, without bending it down and in. You may be issued a special forearm and thumb splint called a thumb-spica splint. It keeps the wrist and lower joints of the thumb from moving. By resting the wrist extensor tendons and the thumb muscles, it allows the area to begin healing.
Anti-inflammatory medications may help control the swelling of the tenosynovium and ease symptoms. These medications include common over-the-counter medications such as ibuprofen and aspirin. Ice treatments can also help decrease swelling and relieve pain.
If these simple measures fail to control your symptoms, your doctor may suggest an injection of cortisone. Cortisone is a very effective anti-inflammatory medication. Cortisone injections will usually control the inflammation in the early stages of the problem. However, cortisone’s effects are generally temporary, lasting from several weeks to months.
Related Document: A Patient’s Guide to Joint Injections for Arthritis
Your doctor may have you work with a physical or occupational therapist. The main focus of treatment is to reduce or eliminate the cause of the irritation to the thumb tendons. Your therapist may check your workstation and the way you do your work tasks. Your therapist may give you suggestions about healthy body alignment and wrist positions, helpful exercises, and tips on how to prevent future problems.
Surgery
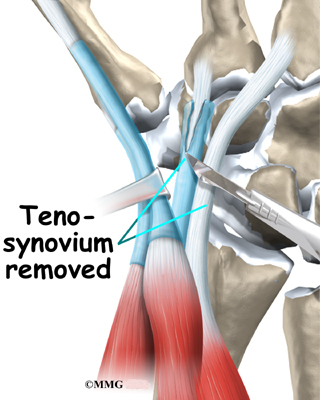
Surgery is rarely necessary to treat intersection syndrome. In extremely difficult cases, a surgeon may remove some of the thickened tenosynovium around the tendons. The operation is called a tendon release.
The tendon release procedure can usually be done on an outpatient basis, which means that you won’t have to spend the night in the hospital. It can be done using a general anesthetic, which puts you to sleep, or a regional anesthetic. A regional anesthetic blocks the nerves going to only a certain part of the body. Injection of medications similar to lidocaine can block the nerves for several hours.
You may get an axillary block, which puts the arm to sleep, or a wrist block, which puts only the hand to sleep. It is even possible to perform the surgery by simply injecting lidocaine around the area of the incision.
The first step is to make a small incision over the spot where the two muscles cross over the two wrist tendons.
The surgeon identifies the irritated tendons, and then separates and removes the inflamed tenosynovium from the tendons.
The skin is then stitched together, and your hand is wrapped in a bulky dressing.
Rehabilitation
What can I expect after treatment?
Nonsurgical Rehabilitation
If nonsurgical treatment is successful, you may see improvement in four to six weeks. You may need to continue wearing your thumb splint to control symptoms. Try to do your activities using healthy body and wrist alignment. Limit activities that require repeated motions of the wrist and thumb.
After Surgery
A period of rehabilitation is needed after surgery. Pain and symptoms generally begin to improve after surgery, but you may have tenderness in the area of the incision for several months.
At first, take time during the day to support your arm with your hand elevated above the level of your heart. You should gently move your fingers and thumb from time to time during the day. Keep the dressing on your hand until you return to the doctor. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery.
You will probably need to attend occupational or physical therapy sessions for six to eight weeks, and you should expect full recovery to take several months. You’ll begin by doing active hand movements and range-of-motion exercises. Therapists also use ice packs, soft-tissue massage, and hands-on stretching to help with the range of motion. When the stitches are removed, you may start carefully strengthening your hand and thumb by squeezing and stretching special putty. Therapists also use a series of gentle stretches to encourage the wrist tendons to glide smoothly under the thumb muscles.
As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints in your wrist and thumb. Other exercises are used to improve fine motor control and dexterity. Some of the exercises you’ll do are designed to get your hand working in ways that are similar to your work tasks and sport activities.
Your therapist will help you find ways to do your tasks that don’t put too much stress on your thumb and wrist. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.