A Patient’s Guide to Congenital Flatfoot (Pes Planus) in Children
Introduction
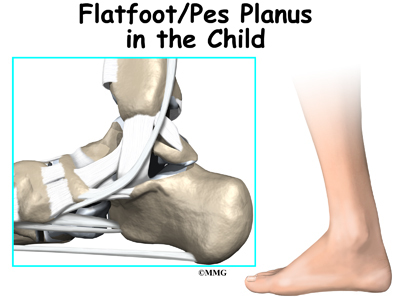
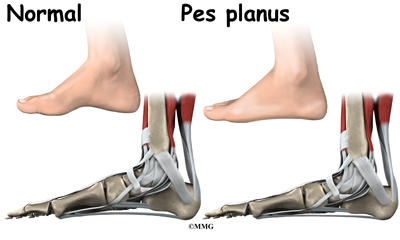
Flatfeet (also known as pes planus) describes a condition in which the longitudinal (lengthwise) and/or medial (crosswise) arches of the foot are dropped down or flat. The entire bottom of the bare foot is in contact with the floor or ground surface during standing, walking, and other weight bearing activities.
The condition is often present at birth (congenital) in one or both feet. When only one foot is affected, the problem is referred to as unilateral pes planus or flatfoot. When both feet are involved, the condition is bilateral flatfeet.
This guide will help you understand
- what parts of the foot are affected
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the foot are involved?
The anatomy of the foot is very complex. When everything works together, the foot functions correctly. When one part becomes damaged, it can affect every other part of the foot and lead to problems. With a flatfoot deformity, bones, ligaments, and muscles are all affected. A combination of malalignments results in the flatfoot appearance.
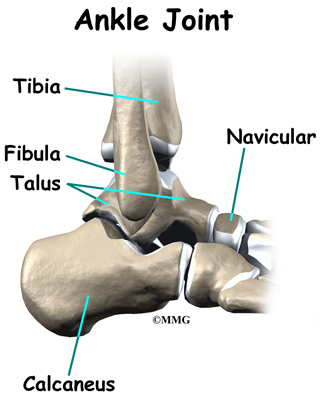
Bones
The skeleton of the foot begins with the talus, or ankle bone, that forms part of the ankle joint. The two bones of the lower leg, the large tibia and the smaller fibula, come together at the ankle joint to form a very stable structure known as a mortise and tenon joint.
The two bones that make up the back part of the foot (sometimes referred to as the hindfoot) are the talus and the calcaneus, or heel bone. The talus is connected to the calcaneus at the subtalar joint. The ankle joint allows the foot to bend up and down.
The subtalar joint allows the foot to rock from side to side. People with flatfeet usually have more motion at the subtalar joint than people who do not have flatfeet. The increased flexibility of the subtalar joint results in many compensatory actions of the foot and ankle in order to keep proper foot alignment during standing and walking.
Just down the foot from the ankle is a set of five bones called tarsal bones. The tarsal bones work together as a group. They are unique in the way they fit together. There are multiple joints between the tarsal bones. When the foot is twisted in one direction by the muscles of the foot and leg, these bones lock together and form a very rigid structure. When they are twisted in the opposite direction, they become unlocked and allow the foot to conform to whatever surface the foot is contacting.
The tarsal bones are connected to the five long bones of the foot called the metatarsals. The two groups of bones are fairly rigidly connected, without much movement at the joints. Finally, there are the bones of the toes, the phalanges.
Ligaments and Tendons
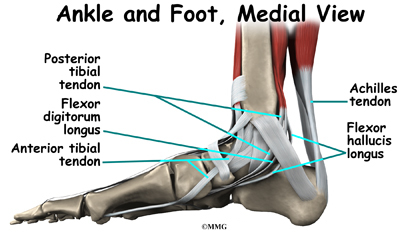
Ligament are the soft tissues that attach bones to bones. Ligaments are very similar to tendons. The difference is that tendons attach muscles to bones. Both of these structures are made up of small fibers of a material called collagen. The collagen fibers are bundled together to form a rope-like structure.
The large Achilles’ tendon is the most important tendon for walking, running, and jumping. It attaches the calf muscles to the heel bone to allow us to rise up on our toes. The posterior tibial tendon attaches one of the smaller muscles of the calf to the underside of the foot. This tendon helps support the arch and allows us to turn the foot inward. Failure of the posterior tibial tendon is a major problem in many cases of pes planus.
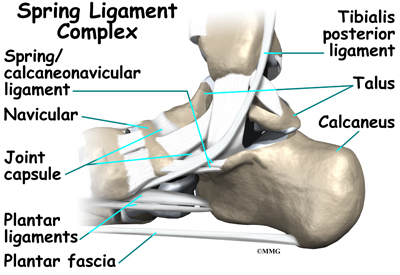
Many small ligaments hold the bones of the foot together. Most of these ligaments form part of the joint capsule around each of the joints of the foot. A joint capsule is a watertight sac that forms around all joints. It is made up of the ligaments around the joint and the soft tissues between the ligaments that fill in the gaps and form the sac.
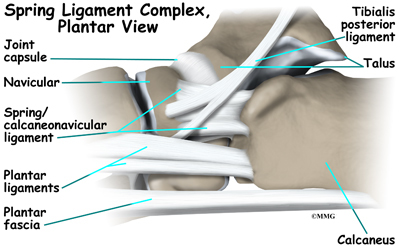
The spring ligament complex is often involved in the flatfoot condition. This group of ligaments supports the talonavicular joint. The spring ligament complex works with the posterior tibial tendon and the plantar fascia to support and stabilize the longitudinal arch of the foot.
Failure of the ligaments that support this arch can contribute to flatfoot deformity. Injury, laxity (looseness), or other dysfunction of the ligament and tendon structures can result in deformity of the foot and/or ankle resulting in pes planus.
Muscles
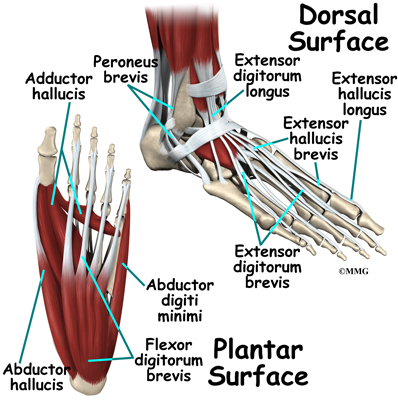
Most of the motion of the foot is caused by the stronger muscles and tendons in the lower leg that connect to the foot. Contraction of the muscles in the leg is the main way that we move our feet to stand, walk, run, and jump.
There are numerous small muscles in the foot. While these muscles are not nearly as important as the small muscles in the hand, they do affect the way that the toes work. Damage to some of these muscles can cause problems.
Most of the muscles of the foot are arranged in layers on the sole of the foot (the plantar surface). There they connect to and move the toes as well as provide padding underneath the sole of the foot.
Related Document: A Patient’s Guide to Foot Anatomy
Causes
What causes this problem?
Flexible flatfoot refers to a foot that looks flat when standing but appears to have an arch when the foot isn’t resting on the floor or against a flat surface. Sometimes the term fallen arches is used, but doctors prefer not to use this term in favor of the more accurate medical term pes planus.
Most babies and young children have what looks like flat feet. This is normal. Before the bones are formed, much of the foot and ankle are still made up of soft tissue, fat, and cartilage. The arch has not formed fully yet. The joints are still hypermobile when the child starts to get up on feet to walk. This is when the flatfoot deformity becomes obvious and parents may become concerned that something is wrong with their child’s foot. The vast majority of children will grow out of their flat foot deformity. Even if the deformity does not fully correct with age, it is unlikely to cause the child any difficulty in the future.
Stress and activities during early childhood requiring strength in the feet are actually the training needed to develop normal muscle, tendon, ligaments, and bone in the foot and ankle. But in some cases, the arch doesn’t form and the foot remains flat into adulthood. Flatfeet do tend to occur in families as an inherited condition.
There are many possible causes for the flatfoot condition. Biomechanically, many soft tissue structures must connect and support one another to prevent a flatfoot deformity. Tibial (lower leg bone) rotation, hindfoot alignment, and position of the joints of the foot, midfoot, hindfoot, and ankle are all important factors. There is no one cause of flatfoot deformity that can be identified.
In the flexible flatfoot, the bones are usually normal – but the supporting ligaments are lax or loose. The joints are hypermobile. As the soft tissues and joints of the foot and ankle try to maintain a normal foot position, increased stress is placed on them. This can lead to fatigue and loss of strength resulting in a sagging of the arch. This can affect the chain of anatomical structures all the way up the leg.
There are some uncommon causes of flatfoot that do affect the bones. A tarsal coalition refers to a condition where two or more bones in the midfoot or hindfoot fail to form separately during development. They remain connected together, altering the bone structure of the foot and limiting flexibility of the foot. This is a different type of flatfoot deformity altogether and is commonly referred to as a spastic flatfoot. This type of flatfoot deformity is not flexible. In fact, the foot is quite rigid due to the abnormal connection between the bones of the foot. This condition can be painful.
Related Document: A Patient’s Guide to Tarsal Coalition
Symptoms
What does the condition feel like?
For most children, the flexible flatfoot deformity causes no symptoms. They do not suffer from pain, swelling, or sore feet. Children with flexible flatfoot deformity may wear out shoes a bit different from a normal person, but there usually is not any reason to be concerned.
In moderate to severe cases, the patient may report fatigue and tired, sore feet after standing on them all day. During those times, they may limit their own activities.
In the uncommon severe cases, calluses may appear where pressure occurs as the bones make contact with the floor or hard surface. The loss of joint stability may alter the foot’s ability to absorb the load and conform to uneven ground or surfaces.
Rarely, the flatfoot deformity may get worse with age. Excess pressure on the surrounding soft tissues (ligaments, capsules, tendons, muscles) can lead to other problems such as malalignment of the patella (kneecap), hallux valgus (bunions), and rotation of the knee and hip.
When the flatfoot deformity is the result of a tarsal coalition, the situation is different. The foot may become painful. The child may begin to complain of foot and ankle pain after a minor twisting injury and the pain not resolve after a normal healing period. The symptom of pain combined with decreased motion and flatfoot deformity should suggest a more serious problem in the foot.
Diagnosis
How do doctors diagnose the problem?
The history and physical examination are probably the most important tools the physician uses to diagnose this condition. Clinical tests can be done to differentiate flexible flatfoot from rigid flatfoot. The examiner will check mobility in the forefoot, hindfoot, and ankle. Muscle weakness and/or muscle tightness will be assessed. The wear pattern on the shoes can offer some helpful clues.
X-rays or other more advanced imaging such as CT scans or MRIs may be ordered but these are rarely needed. The examiner may be able to see and feel a prominent bump with tenderness around the area when an accessory navicular bone is present. X-rays will show if there is an accessory navicular or tarsal coalition as part of the problem.
A very simple test called the wet footprint can be done at home or in the doctor’s office. The patient places the foot in water and then places the foot down on a piece of paper or thin cardboard. After making a footprint, the foot is lifted off the paper. Someone with a flat foot will leave a complete footprint where the sole makes contact with the paper.
The physician may have you perform a single heel raise. You will be asked to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the calcaneus (heel bone) in the middle with slight inversion (turned inward).
Treatment
What treatment options are available?
Nonsurgical Treatment
There may be no treatment needed for mild cases of flatfeet, especially flexible flatfeet. This condition often corrects itself in time as the child grows and develops. Young children should be encouraged to walk barefoot whenever it is safe to do so. This will increase sensory input into the foot. At the same time, navigating various floor and ground surfaces helps build strength and stability.
For older children and adults, a simple modification to the shoe may reduce the fatigue and discomfort in the foot. Sometimes purchasing shoes with a good arch support is sufficient. Try to find a comfortable shoe with an arch support, firm heel counter (back of the heel), and a flexible sole (bottom). Supporting the arch helps decrease the tension in the posterior tibialis tendon. Stretching the Achilles’ tendon helps maintain normal motion of the hindfoot, which in turn, helps maintain alignment of the midfoot.
For other patients, an off-the-shelf (prefabricated) shoe insert works well. The goal is to support the foot and prevent further stretching of lax ligaments and tendons. These supports will not reverse the structural deformity and they will not build and arch by wearing them over time. These inserts simply help the shoe better fit the foot and support the structures of the foot. Improving alignment can take tension off the soft tissue structures, reduce fatigue, and improve the biomechanics of standing and gait (walking).
Further treatment is usually not needed for the flexible flatfoot deformity. Surgery is rarely needed for this condition. Patients with severe symptoms that do not respond to conservative care may benefit from further orthopedic evaluation and treatment. In rare cases, surgical intervention to correct the problem and realign the foot may be suggested.
Surgery
For children with a shortened Achilles’ tendon, a program of stretching exercises or serial casting may help reduce pressure on the talus bone and offer significant pain relief. Severe cases of flatfoot (pes planus) may require surgery to reconstruct the arch or fuse the bones. This is very rare as conservative (nonoperative) care is usually sufficient.
Children with tarsal coalition or an accessory navicular bone require orthopedic evaluation and management. Surgery is done to correct the problem by the early teen years (before skeletal maturity).
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Flatfeet seen in very young children just starting to walk often resolve with time. The very act of gripping with the toes to maintain support and balance along with the development of the bones forms the arches.
For older children who still have flatfeet, stretching and strengthening exercises won’t cause an arch to form where there isn’t one anatomically. But these activities can help ease any pain or discomfort caused by the condition. The same is true for any supports or shoe inserts that are used.
After Surgery
Corrective surgery is only done in cases of severe, painful and disabling flatfoot position. This is very rare. Reconstructive surgery for tarsal coalition or an accessory navicular bone requires a period of immobilization in a cast followed by rehabilitation to restore strength in the foot and ankle. In some cases, more than one operation is needed as the child grows and develops. Pain relief and joint stability are the goals.