A Patient’s Guide to Compression Fixation for a Fractured Hip
Introduction
A fractured hip can be a life-threatening problem. The hip fracture itself isn’t usually a difficult problem to treat with surgery. But once the fracture occurs, it brings with it all the potential medical complications that can arise when aging adults are confined to bed. The goal of treatment is to get patients moving as quickly as possible after surgery. Fixing the fracture with a compression hip screw and metal plate is fairly simple and usually allows patients to get up and start moving shortly after surgery.
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the operation
- what to expect during your recovery
Anatomy
What part of the hip is involved?
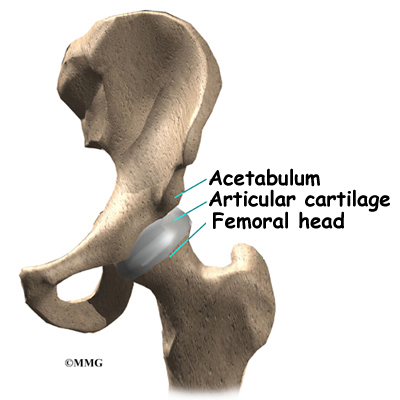
The femur is the large bone in the thigh. The ball-shaped femoral head fits into a socket in the pelvis, called the acetabulum. The femoral neck is a thinner part of the femur. It is the short section of bone next to the femoral head that connects the femoral head to the main shaft of the femur.
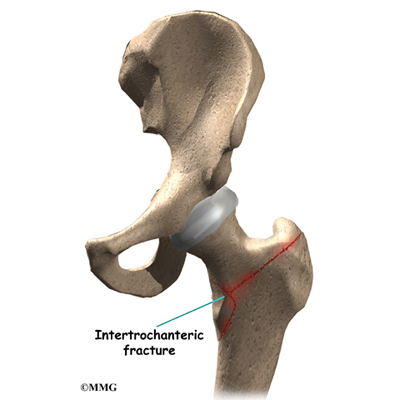
The intertrochanteric region of the hip is just below the femoral neck. A fracture in this area is called an intertrochanteric hip fracture. This type of fracture is most common when a person falls and fractures the hip. There is usually more than one fracture with more pieces of broken bone to be held together.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
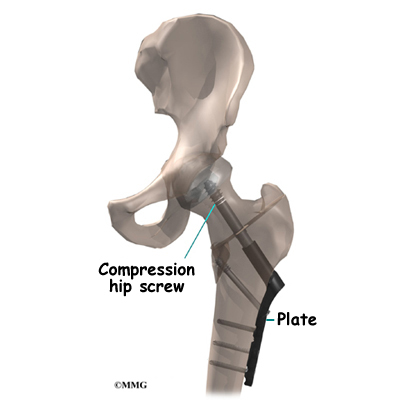
Fixing the hip fracture surgically with a special type of metal plate and screw, called a compression screw, does two things. First, it helps align the bone fragments and hold them in the proper position. Second, the fixation device is strong enough to keep the bones in place as you begin to move about. Before these devices were used, a patient needed to remain in bed usually with traction to hold the bones in alignment. The fixation now holds the bones in place while the bone heals. This allows you to get out of bed sooner because the metal plate and screw are strong enough to hold the bone fragments in place as you move.
The procedure requires only a small incision on the side of the hip, and the plate and screw usually provide a solid connection for the broken bones. Since patients are able to get moving right away after surgery, they are more likely to avoid the serious complications that can arise with being immobilized in bed.
Preparation
What happens before surgery?
Compression fixation for a fractured hip is usually an emergency surgery, so it is likely you may not have had time to plan and prepare. Ideally a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital.
The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, make sure you have needed supplies, and make follow-up appointments with your surgeon, doctor, and physical therapist.
Surgical Procedure
What happens during the operation?
Sometimes, a fractured hip only requires a simple pinning procedure. The procedure for the compression hip screw, however, is more involved. There are usually several fragments of bone that need to be held together. There is also more blood lost during the surgery, which could require that you have a blood transfusion during the operation.
Related Document: A Patient’s Guide to Hip Pinning Surgery for a Fractured Hip
This operation can be done using either a general anesthetic or a spinal block. A general anesthetic puts you completely to sleep. A spinal block puts your body to sleep only from the waist down. The anesthesiologist will also give you medications so that you won’t be aware the operation is being done.
Once you have anesthesia, your surgeon will make sure the skin of your hip is free of infection by cleaning the skin with a germ-killing solution.
With the patient lying flat on a special table, the foot and leg are supported. Tension is applied to get the fractured bones to line up. The surgeon checks the alignment using a fluoroscope, a type of X-ray machine that shows the image on a TV screen.
Next, the surgeon makes an incision over the side of the thigh. A large metal screw is placed through the side of the hip into the femoral head. With the help of the fluoroscope, the surgeon attaches a metal plate to the side of the femur with four to eight small metal screws. The procedure can usually be finished in less than an hour depending on how many fragments of bone are involved in the fracture.
The soft tissues are put back in place, and metal staples or sutures are used to close the incision.
Complications
What might go wrong?
Complications after a hip fracture are sometimes the result of being immobilized in bed. These may include pneumonia, bed sores, mental confusion, and blood clots (deep venous thrombosis).
Related Document: A Patient’s Guide to Hip Fracture
Complications that can result from the compression fixation surgery itself include
- anesthesia complications
- infection
- thrombophlebitis (DVT)
- nerve or blood vessel injury
- nonunion of the bones
This is not intended to be a complete list of possible complications.
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any surgery carries the risk of infection. You will probably be given antibiotics before the procedure to reduce the risk. If you get an infection, you will need more antibiotics. If the areas around the metal screws or plate become infected, you may need surgery to drain the infection.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Nerve or Blood Vessel Injury
Several nerves and blood vessels travel in the area where the surgery is performed. It is possible to injure either the nerves or the blood vessels during surgery, but this is extremely unlikely during this type of procedure. Nerve problems may be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to either the nerves or the blood vessels, but it is possible.
Nonunion
Sometimes the bones do not bond together as planned. This is called a nonunion, or pseudarthrosis. This condition requires another operation to add more fixation or to replace the head of the femur, a procedure called hemiarthroplasty.
Related Document: A Patient’s Guide to Hemiarthroplasty of the Hip
After Surgery
What happens after the operation?
After surgery, your hip will be covered with a padded dressing. If your surgeon used a general anesthesia, a nurse or respiratory therapist will guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
A physical therapist will direct your recovery after surgery. You’ll be encouraged to move from your hospital bed to a chair several times the first day after surgery. You’ll be encouraged to begin getting up and walking with your crutches or walker, but you may need to keep from placing too much weight on your foot while you stand or walk. You’ll be ready to go home when you can move about safely with your walker or crutches, you are able to do your exercises, and your caregiver has made all the needed preparations for you at home.
You should keep the dressing on your hip until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery. Remember to support your outer hip with a pillow when you sit or recline.
Rehabilitation
What should I expect during my recovery?
Once discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure that you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on walking and strength. In some cases you may require additional visits at home before beginning outpatient physical therapy. Home therapy visits end when you are safe to get out of the house.
Additional outpatient physical therapy visits are sometimes needed for patients who are still having problems walking or who need to get back to physically heavy work or activities.
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, and thigh. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip. Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
The therapist’s goal is to help you maximize hip range of motion and strength, restore a normal walking pattern, and do your activities without risking further injury. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.