Cervical Spine
Transcutaneous Electrical Stimulation (TENS) for Cervical Spine Pain
A Patient’s Guide to Transcutaneous Electrical Stimulation (TENS) for Cervical Spine Pain
Introduction
Neck (cervical spine) pain due to musculoskeletal disorders, is the second largest cause of time off work – low back pain being first. It is generally worse in the morning and evening. The most commonly prescribed intervention is rest and analgesics, and often a referral to physical therapy. Among the rehabilitation intervention treatments for neck pain is the transcutaneous electrical nerve stimulation (TENS) unit.
Electrical nerve stimulation is a treatment for pain that is used primarily for chronic pain. The electrical stimulation is delivered through electrodes or patches placed on the skin. The technique and the device used is called transcutaneous electrical stimulation or TENS for short.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
This guide will help you understand
- who may benefit from a TENS unit
- how a TENS unit works
- what to expect with a TENS unit
Who may benefit from a TENS unit
TENS can be used for relief of pain associated with a wide variety of painful conditions. This may include back pain caused by spine degeneration, disc problems, or failed back surgery. Nerve pain from conditions such as chronic regional pain syndrome (CRPS) and neuropathies caused by diabetes or as a side effect of cancer treatment may also be managed with TENS.
TENS has been used for people suffering from cancer-related pain, phantom-limb pain (a chronic pain syndrome following limb amputation), and migraine or chronic tension-type headaches.
TENS can also be used for muscle soreness from overuse, inflammatory conditions, and both rheumatoid and osteoarthritis. Athletes with painful acute soft tissue injuries (e.g., sprains and strains) may benefit from TENS treatment.
Sometimes it is used after surgery for incisional or post-operative pain from any type of surgery (e.g., joint replacement, cardiac procedures, various abdominal surgeries, cesaerean section for the delivery of a baby). Studies show that TENS can significantly reduce the use of analgesics (pain relievers, including narcotic drugs) after surgery.
TENS is usually used along with other forms of treatment and pain control such as analgesics, relaxation therapy, biofeedback, visualization or guided imagery, physical therapy and exercise, massage therapy, nerve block injections, and/or spinal manipulation.
The effectiveness of TENS remains controversial. The American Academy of Neurology (AAN) findings published in Dec. 30, 2009 issue of Neurology claims it is not effective and cannot be recommended. But, many patients find TENS effective for pain relief, easy to use, and with very low side effects. It may be worth a try for those who suffer from chronic low back pain. It can be discontinued easily if it doesn’t work. TENS cannot correct an underlying problem; it is only used for temporary relief of symptoms.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
To summarize, the benefits from TENS treatment can include:
- pain relief
- increased circulation and healing
- decreased use of pain relievers or other analgesic drugs
- increased motion and function
How does TENS work?
TENS produces an electrical impulse that can be adjusted for pulse, frequency, and intensity. The exact mechanism by which it works to reduce or even eliminate pain is still unknown. It is possible there are several different ways TENS works. For example, TENS may inhibit (block) pain pathways or increase of the secretion of the pain reducing substances (e.g., endorphins, serotonin) in the CNS.
Electrical nerve stimulation is a treatment for pain that is used primarily for chronic pain. The electrical stimulation is delivered through electrodes or patches placed on the skin. The technique and the device used is called transcutaneous electrical neurostimulation or TENS for short.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
Recent research has also shown that autosuggestion or the placebo effect is a powerful way many people experience pain relief or improvement in symptoms. Simply by believing the treatment (any treatment, including TENS) will work has a beneficial effect on the nervous system. Many studies have shown that people get pain relief through the placebo effect alone.
How do I use my TENS unit?
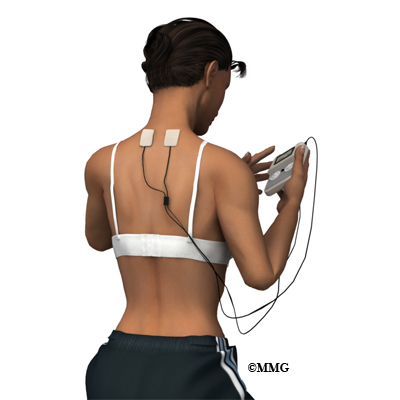
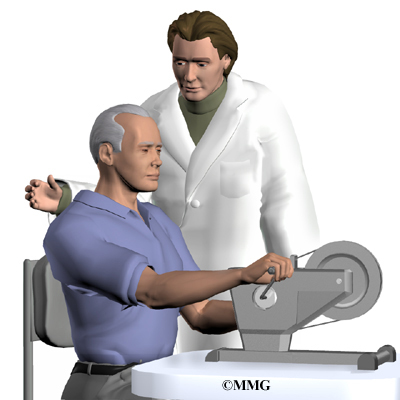
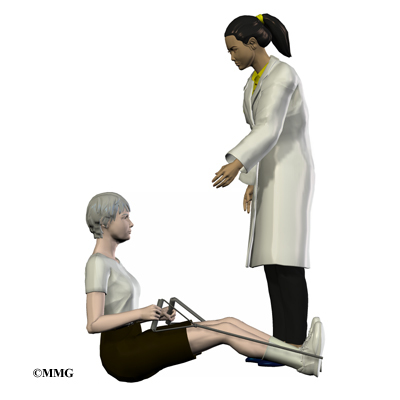
You will be shown how to use your TENS device by your healthcare provider trained in the set-up and use of this modality. Round or square rubber electrodes are applied to the skin over or around the painful area. Usually four electrodes (two pairs) are used to get maximum benefit from this treatment.
The electrodes are self-adhesive with a protective layer of gel built in to prevent skin irritation or burning. The unit is battery-operated with controls you manipulate yourself to alter the strength of the electrical signal. The unit can be slipped into a pocket or clipped to your belt. You may use two or four electrodes.
The electrodes will be placed on your body at positions selected by a physician or physical therapist. The electrode placement is determined based on the location of the involved nerves and/or the location of your pain.
The first place to try the electrodes is either directly over the painful area or on either side of the pain. You will slowly turn up the intensity of the unit until you feel a buzzing, tingling, or thumping sensation strong enough to override the pain signals.
If that doesn’t work, you may get better results putting the electrodes over the area where the spinal nerve root exits the vertebra. Sometimes it takes a bit of trial and error to find the right settings and best electrode placement for you.
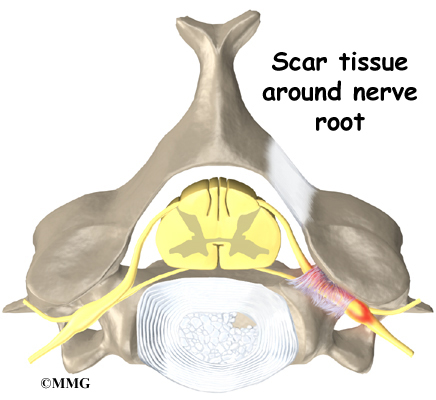
Be sure and let your healthcare provider know if you experience increased pain. Electrodes placed below the level of a peripheral nerve impairment might actually block the input from the TENS unit and cause increased pain. Or placement over an area of scar tissue from surgery can cause increased skin resistance and decreased transmission of the electrical impulses.
Another way to use TENS is over spots in the muscles that trigger pain called trigger points (TrPs). Trigger points are areas of hyperirritability in the muscles that can cause chronic pain. The healthcare provider will identify any TrPs present during your exam. Usually TrPs are taken care of with a treatment designed to eliminate them. In some patients they are chronic and don’t go away or come back easily. In such cases, TENS may be helpful.
Your health care team will guide you through the trial-and-error process for finding the best electrode placement for you and make any changes needed in the program.
When you should NOT use TENS
- If you have loss of skin sensation or even decreased sensation, you should not use TENS. With altered sensation, there is a risk of turning the unit up too high and causing injury or harm.
- The use of TENS is not recommended for older adults with Alzheimer’s, dementia, or other cognitive problems.
- If you have a cardiac pacemaker, you should not use TENS as the electrical signals could interfere with your pacemaker. Cardiac patients should not use TENS without their physician’s approval.
Some guidelines when using TENS
- Before applying the electrodes, it is important to remove all lotions, oils, or other applications to the skin. You may want to shave hair from the local area where the electrode will be applied.
- Daily use of TENS for several hours at a time is recommended. You should not wear the unit for long periods of time (e.g., 24 hours) or during extended sleep time (napping is okay but TENS should not be used while sleeping at night or for more than a couple of hours).
- Never place an electrode over an open wound or area of skin irritation. Report any skin problems or burns immediately.
- Do not place electrodes near your eyes or over your throat.
- Do not use TENS in the shower or bathtub.
- Move the electrodes a bit each time you put them on to avoid skin irritation.
- You should experience a comfortable tingling sensation that is comfortable enough to allow you to complete daily tasks and activities.
- You may want to keep a daily journal of your pain levels, the settings you use, and a record of the medications you are taking for pain relief. By reviewing your notes, you may find the best combination of electrode placement and unit settings that gives you the most pain relief.
What you can expect with TENS
You should feel a mild to moderately strong tingling or buzzing sensation. Some people experience a more unpleasant sensation described as burning or prickling. Depending on the intensity and duration of your pain, you may or may not get results right away.
It can take several days to even several weeks to get the desired results. Differences in results may occur based on properties of skin resistance, type of pain, and individual differences in the mechanism of pain control. Be patient and persistent. Do not hesitate to contact your healthcare provider as often as it takes to get the desired results.
Many patients do report good-to-excellent results, first with pain control, then pain relief, and finally reduction in the use of medications. Although it doesn’t happen for everyone, some chronic pain patients are “cured” permanently from their pain.
As each of these benefits from the TENS treatment occur, you may find yourself increasing your activity level – either with the same level of TENS usage or even with reduced frequency of use, intensity of signal, or duration (length of time the unit is turned on).
If for any reason your pain starts to increase in frequency, duration, or intensity, don’t assume the treatment isn’t working for you. First, check the TENS unit for any malfunction, need to recharge, or replace the electrodes with new ones. If your unit is battery-operated, you may find it necessary to turn the intensity up to obtain the same sensation when the batteries are low. This should alert you to the need for battery replacement.
Finally, be aware that some patients experience “breakthrough pain,” referring to a situation in which you get pain relief at first but then even with the TENS unit, you start to have pain once again. Turning the intensity up high enough to cause muscle contraction is an indication of breakthrough pain.
Sometimes a different setting for the stimulator may be needed when this happens. Most units have a setting that allows for random pulse frequency, duration, and amplitude. The use of this setting helps keep the nervous system from getting used to a specific amount of stimulation and ignoring it. This phenomenon is called habituation or adaptation.
Summary
TENS is an effective method of pain control for chronic pain when you want to maintain your normal routine of daily activities that would otherwise be hampered by too high of pain levels. TENS helps many people reduce and sometimes even eliminate the use of pain medications, thus avoiding side-effects of long-term drug use.
Even without complete pain relief, TENS makes it possible to stay active and participate in work, family, and even recreational activities. There are no significant adverse effects from the use of TENS. The ability of this treatment technique to moderate pain and reduce the use of pain medications is a real benefit — especially with the potential for serious or adverse effects from long-term use of pain relievers.
Cervical Burners and Stingers (Brachial Plexus Injuries)
A Patient’s Guide to Burners and Stingers (Brachial Plexus Injuries)
Introduction
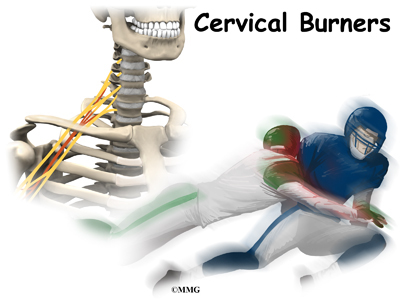
Injury to the nerves of the neck and shoulder that cause a burning or stinging feeling are called burners or stingers. Another name for this type of nerve injury is brachial plexus injury. Football players are affected most often. Up to half of all college football players have had at least one burner or stinger. Many of these occurred during high school football. Fortunately, it’s not a serious neck injury.
This guide will help you understand
- what parts of the body are involved
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the body are involved?
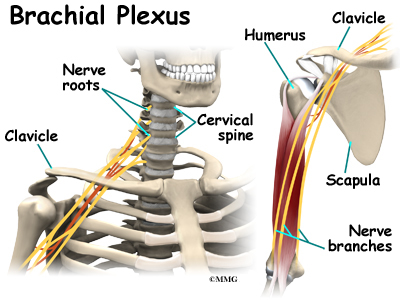
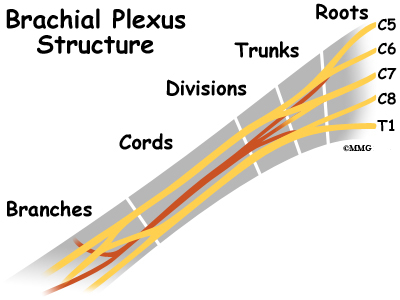
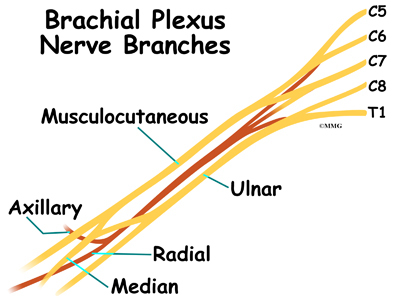
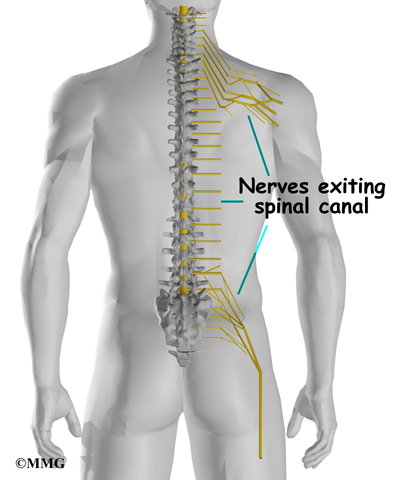
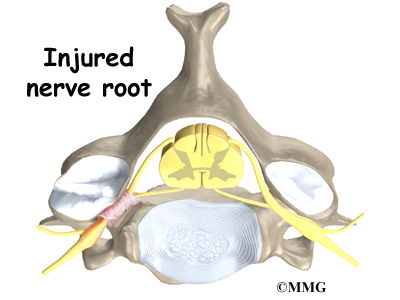
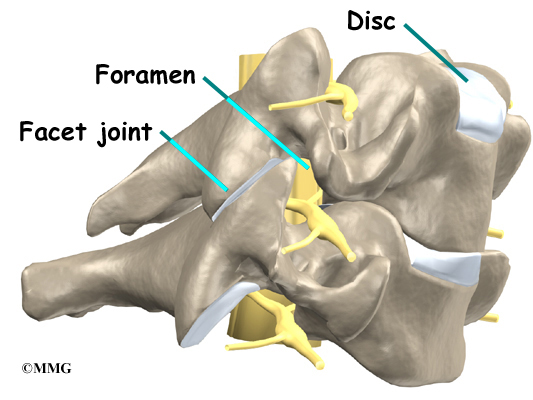
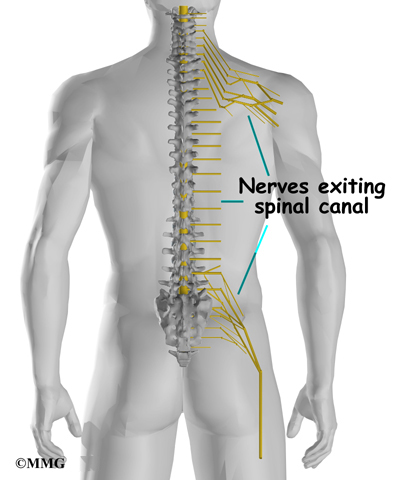
The brachial plexus is affected most often by a downward or backward force against the shoulder. A nerve plexus is an area where nerves branch and rejoin. The brachial plexus is a group of nerves in the cervical spine from C5 to C8-T1. This includes the lower half of the cervical nerve roots and the nerve root from the first thoracic vertebra.
The nerves leave the spinal cord, go through the neck, under the clavicle
(collar bone) and armpit, and then down the arm.
The brachial plexus begins with five roots that merge or join together to form three trunks. The three trunks are upper (C5-C6), middle (C7), and lower (C8-T1). Each trunk then splits in two, to form six divisions. These divisions then regroup to become three cords (posterior, lateral, and medial).
Finally, there are branches that result in three nerves to the skin and muscles of the arm and hand: the median, ulnar, and radial nerves.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
Burners or stingers are the result of traction or compressive forces on the brachial plexus or cervical nerve roots. The usual mechanism of injury occurs when a direct blow or hard hit to the top of your shoulder pushes it down at the same time your head is forced to the opposite side.
In the process, the brachial plexus between the neck and shoulder gets stretched. The same injury can happen if a downward force hits the collarbone directly. In football, burners or stingers occur most often when you tackle or block another player. This motion overstretches the nerves of the brachial plexus.
It’s not clear exactly where in the brachial plexus the damage occurs. Some experts suggest the injury is most likely to be at the level of the trunks, rather than at the nerve root level. The results of other studies show that burners or stingers from compression forces cause nerve root damage while traction injuries result in plexus injuries. A nerve root injury would be much more serious than a burner or stinger from a trunk injury of the brachial plexus.
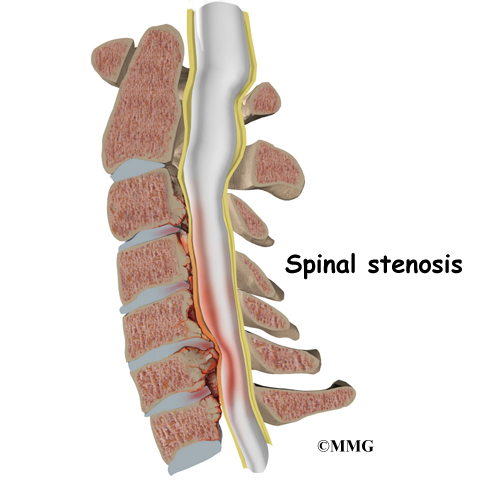
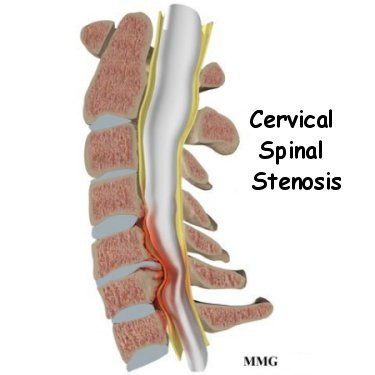
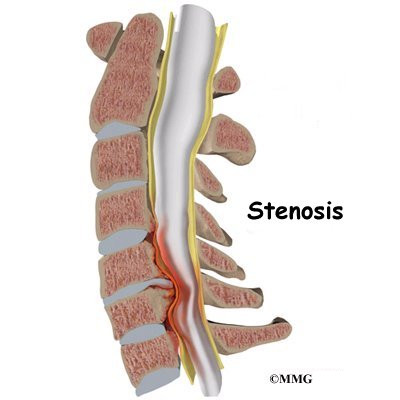
Other athletes who participate in wrestling, gymnastics, snow skiing, and martial arts can also experience burners or stingers. Some studies suggest that athletes with a narrow cervical canal may be at increased risk for this type of injury.
Symptoms
What does this condition feel like?
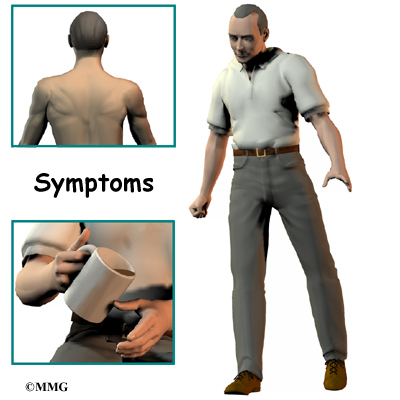
A burning or stinging feeling between the neck and shoulder is the hallmark finding in this condition. True neck pain is more likely to be an injury to the neck itself. With burners or stingers, the painful symptoms start above the shoulder and go down the arm and even into the hand.
The shoulder and arm may feel numb or weak. You may feel as if this area is tingling. Weakness may be present at the time of the injury. Some patients report the arm feels and appears to be “dead”. This paralysis and other symptoms may be transient or temporary. They may only last a few seconds or minutes. But for some patients, healing takes days or weeks. In rare cases, the damage can be permanent.
Diagnosis
How do doctors diagnose this condition?
A careful history and physical exam are needed to diagnose stingers or burners. By assessing areas of weakness, the examiner may be able to tell whether a stretch injury of the brachial plexus has occurred. Nerve function and reflexes are also evaluated. If the physician suspects a cervical spine injury, further testing may be needed.
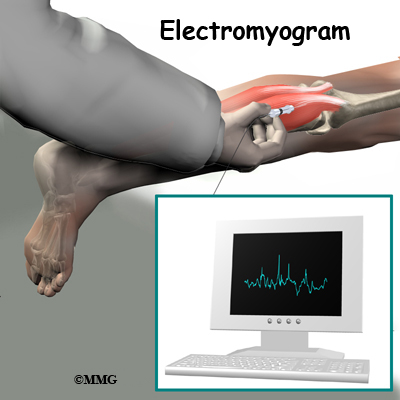
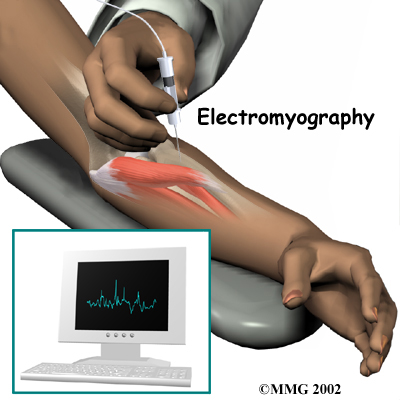
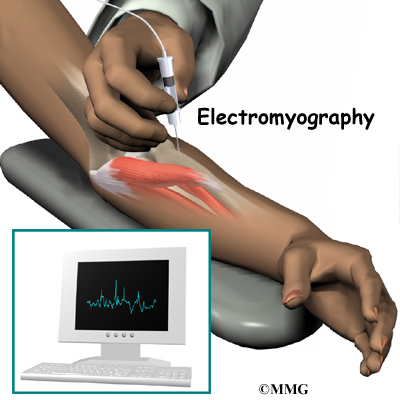
X-rays, MRI, and electrodiagnostic studies such as an electromyogram (EMG) can help make the final diagnosis. The EMG will confirm a problem, pinpoint the area of damage, and give an idea of how long recovery will take for each individual.
Treatment
What treatment options are available?
Nonsurgical Treatment
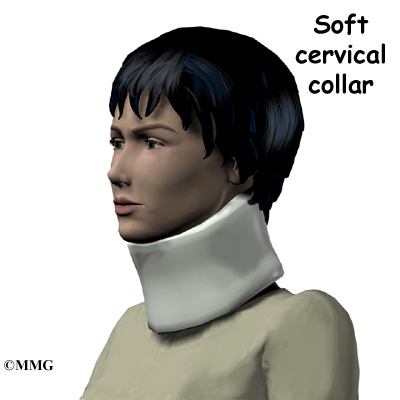
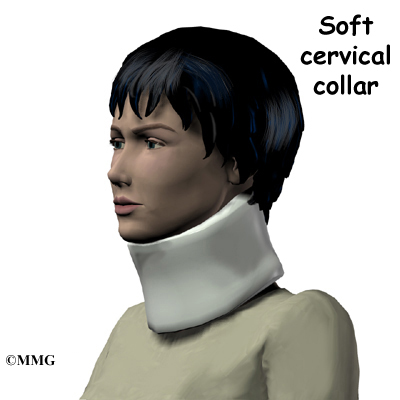
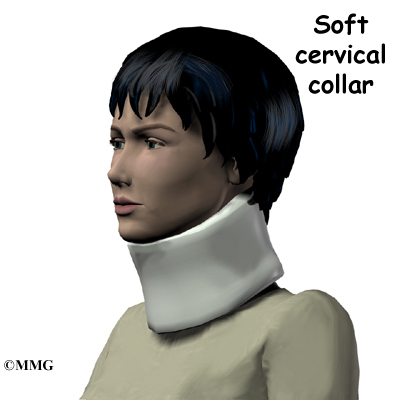
Protecting the neck with a soft collar is the first step in the acute phase of burners or stingers. If the injury occurs on the playing field, the player is placed in a protective collar before being moved off the field. This is worn until X-rays are taken to rule out fracture, dislocation, or other more serious neck injury.
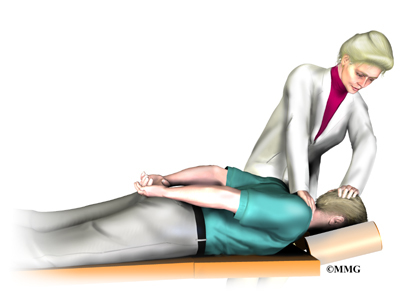
Rest and gentle neck and shoulder range of motion are advised until symptoms resolve. If this does not occur within a few days, then physical therapy may be needed. Your therapist will use modalities such as biofeedback, electrical nerve stimulation, and manual therapy to help restore the natural function of the nerves.
Range of motion and strengthening exercises will be added as tolerated. Posture is very important during the healing phase. A chest-out position helps open the spinal canal, thus giving more room for the spinal cord. This posture also decreases pressure on the nerve roots. Your therapist will provide sport-specific therapy when the symptoms resolve (go away).
Surgery
Surgery is not a treatment option for burners or stingers. Management remains conservative (nonsurgical). Patients are followed through the athletic season until recovery is complete.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Burners and stingers are self-limiting. This means that with treatment, they will resolve over time. You will likely be able to return to full sports participation when you no longer have any symptoms. Full neck and shoulder motion must be present. And you should be able to participate in practice without any problems before entering a game.
It is possible to get another burner or stinger but it could be something more serious. If you experience these types of symptoms again, slowly lie down on the ground. Wait for the team trainer or physician to examine you before moving your head and neck.
Some football players choose to wear extra padding, special shoulder pads, or a neck roll to protect the neck and avoid reinjury. All equipment should be in good condition and fit properly. Daily stretching of the neck is advised. Players should avoid using spearing or head tackling, which has been prohibited since 1979.
Dropped Head Syndrome
A Patient’s Guide to Dropped Head Syndrome
Introduction
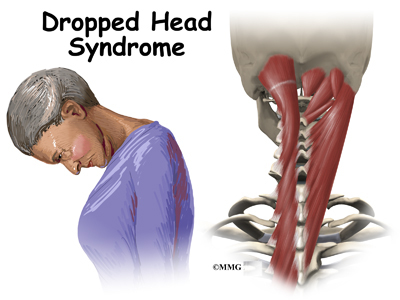
Dropped Head Syndrome is characterized by severe weakness of the muscles of the back of the neck. This causes the chin to rest on the chest in standing or sitting. Floppy Head Syndrome and Head Ptosis are other names used to describe the syndrome.
Most of the time, Dropped Head Syndrome is caused by a specific generalized neuromuscular diagnosis. When the cause is not known, it is called isolated neck extensor myopathy, or INEM.
This guide will help you understand
- what parts make up the cervical spine
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts make up the cervical spine?
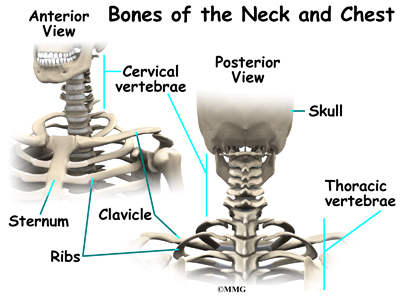
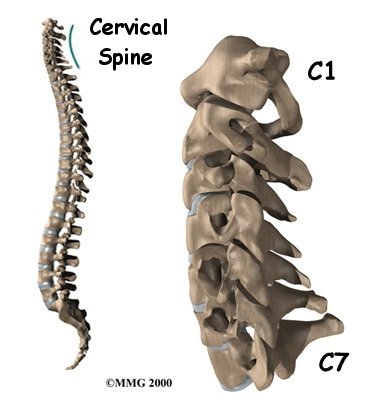
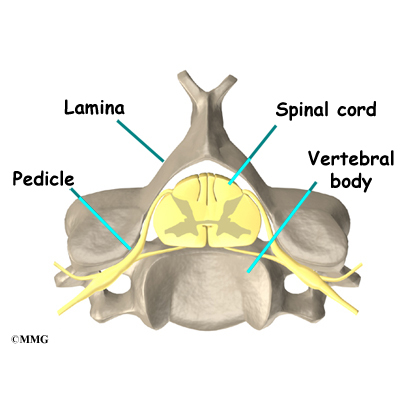
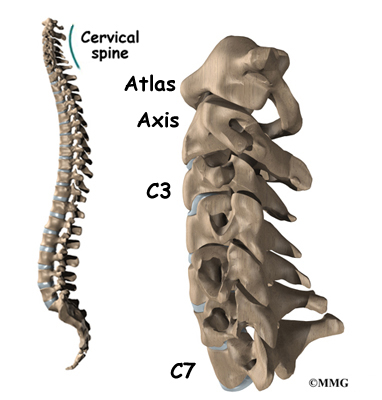
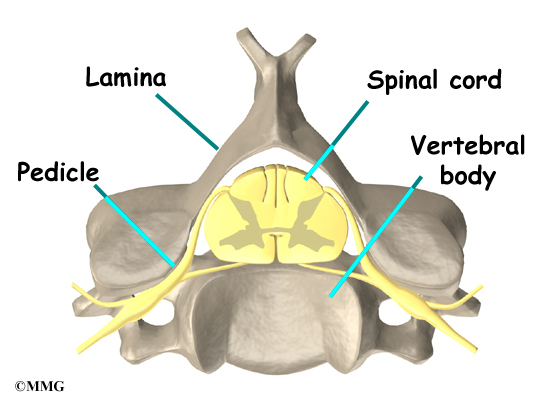
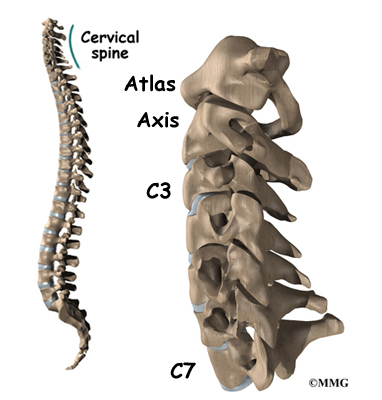
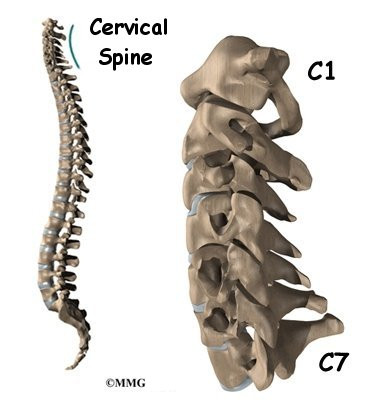
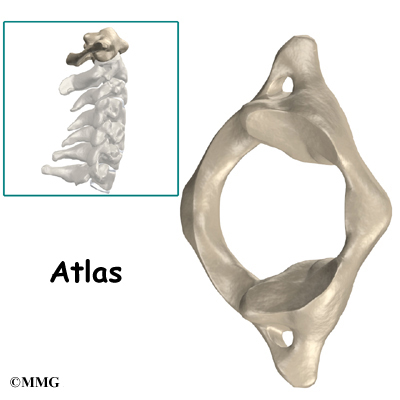
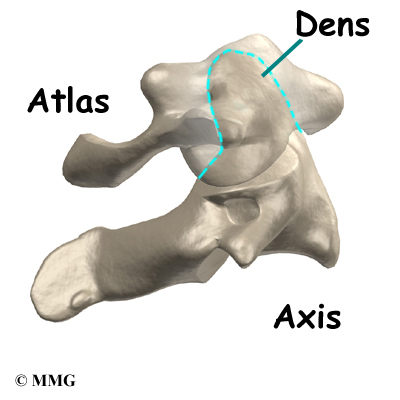
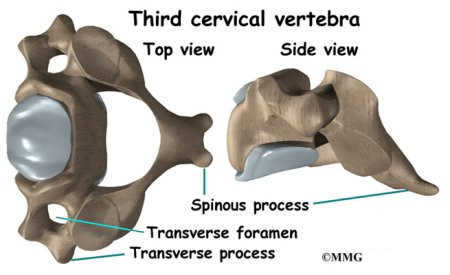
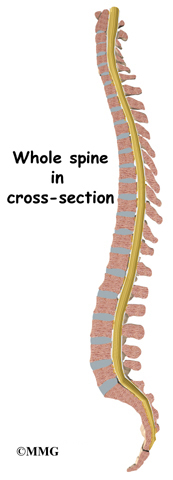
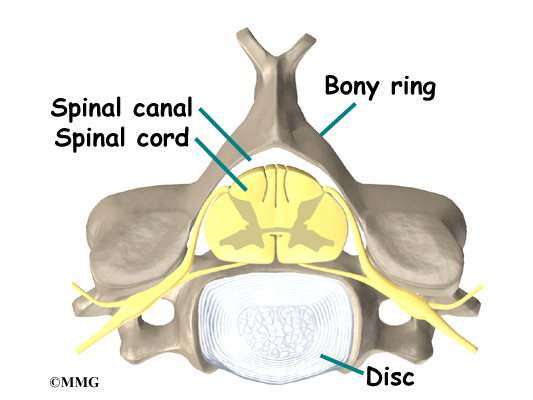
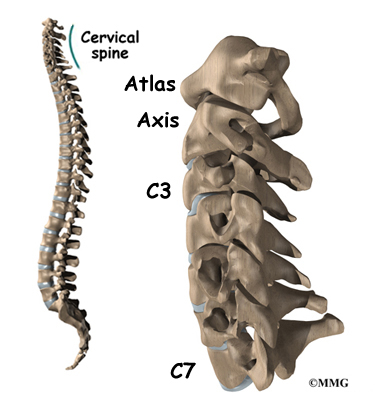
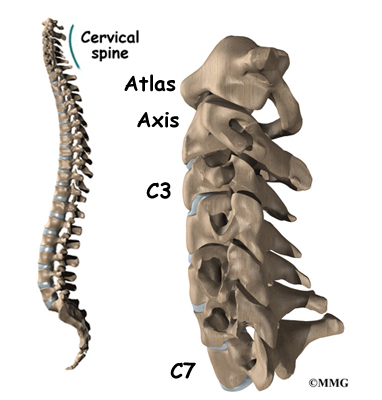
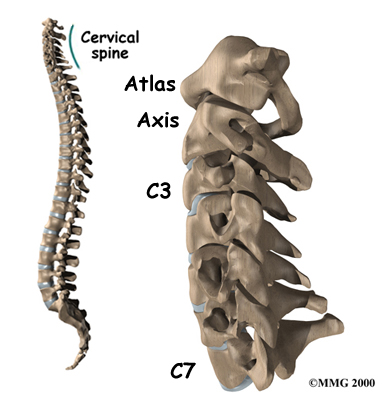
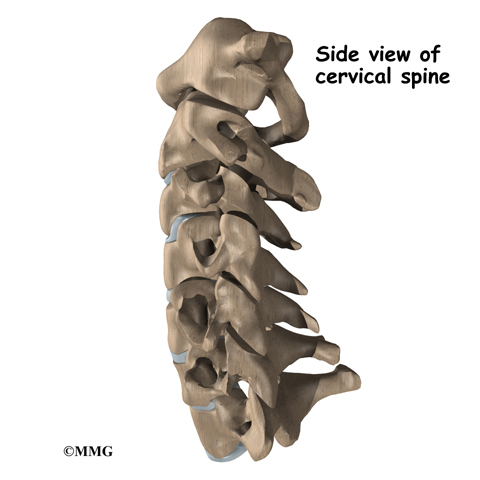
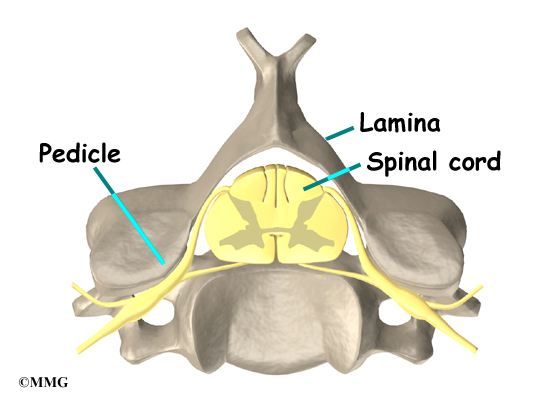
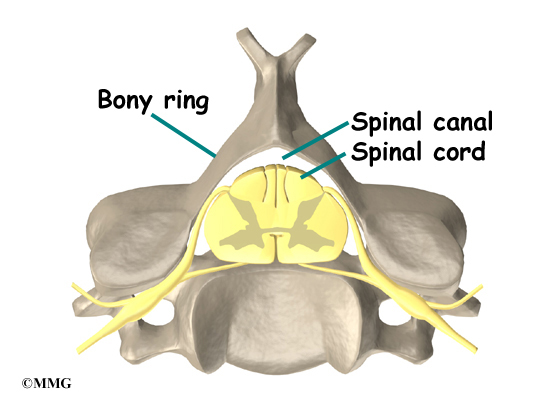
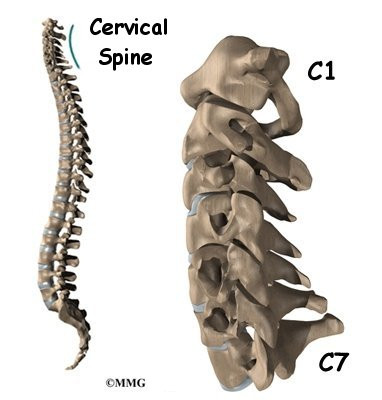
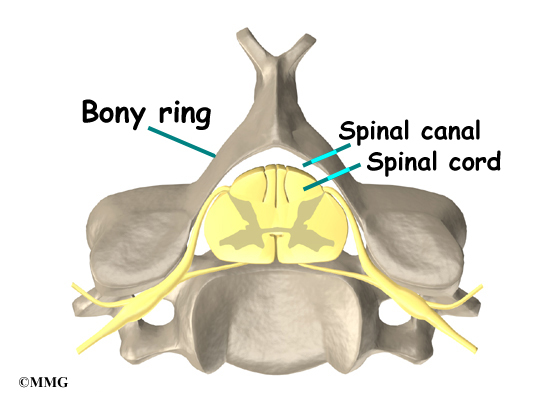
The spine is made up of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord. The spinal cord is a made up of nerve cells which grow to look like a rope or cord about one half inch in diameter. The spinal cord attaches to the base of the brain. The base of the brain is called the
brainstem.
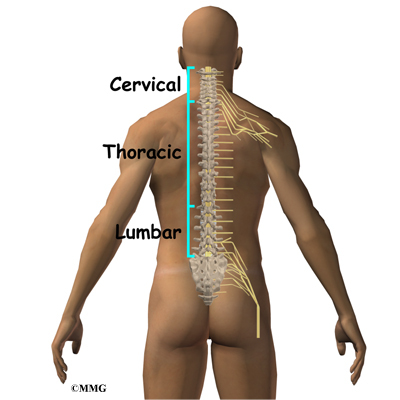
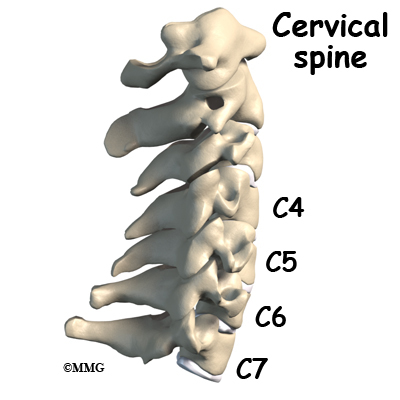
The vertebral column is divided into three distinct portions. The cervical, or neck portion attaches to the base of the skull at the upper end. The lower end of the cervical portion connects with the thoracic spine. There are seven cervical vertebrae.
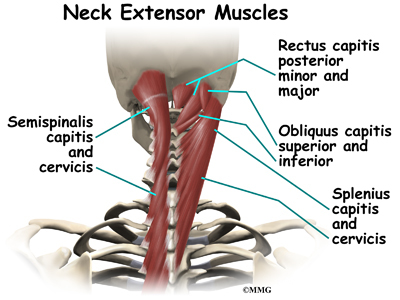
There are many muscles that lie in the neck region. Some attach from the base of the skull, others to the spine, ribs, collar bone, and shoulder blade. Extension of the neck happens when the top of the head tilts backward. This causes the face and eyes to look up. Flexion of the neck is when the top of the head tilts forward. This causes the eyes to look down. It also lowers the chin to the chest.
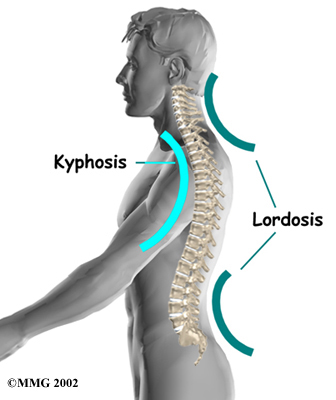
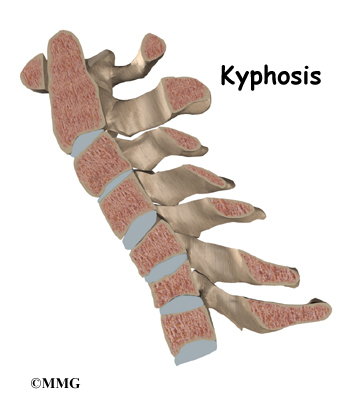
The vertebrae stack on top of one another. When looking at the spine from the side, or from the sagittal view, the vertebral column is not straight up and down, but forms an “S” curve. The cervical spine has an inward curve called a lordosis. The thoracic spine curves outward. This curve is called a kyphosis. The lumbar spine usually has an inward curve or a lordosis. The “S” curve seen in the sagittal or side view allows for shock-absorption and acts as a spring when the spine is loaded with weight.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
Most of the time, Dropped Head Syndrome is caused by a specific generalized neuromuscular diagnosis. These include amyotrophic lateral sclerosis (ALS) also known as Lou Gehrig’s disease, Parkinson’s disease, myasthenia gravis, polymyositis, and genetic myopathies. Other specific causes can include motor neuron disease, hypothyroidism, disorders of the spine, and cancer.
When the cause of Dropped Head Syndrome is not known, it is called isolated neck extensor myopathy, or INEM.
The INEM form of Dropped Head Syndrome usually happens in older persons. The weakness of the muscles in the back of the neck usually occurs gradually over one week to three months.
Symptoms
What does the condition feel like?
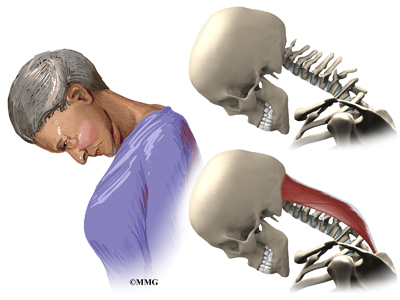
The symptoms of dropped head syndrome are usually painless. It most often occurs in the elderly. The weakness is limited to the muscles that extend the neck. Dropped Head Syndrome usually develops over a period of one week to three months. The head is then tilted downward. Because of the weakness of the extensors of the neck, the chin rests on the chest. Lifting or raising the head in sitting or standing is impossible. When lying down however, the neck is able to extend.
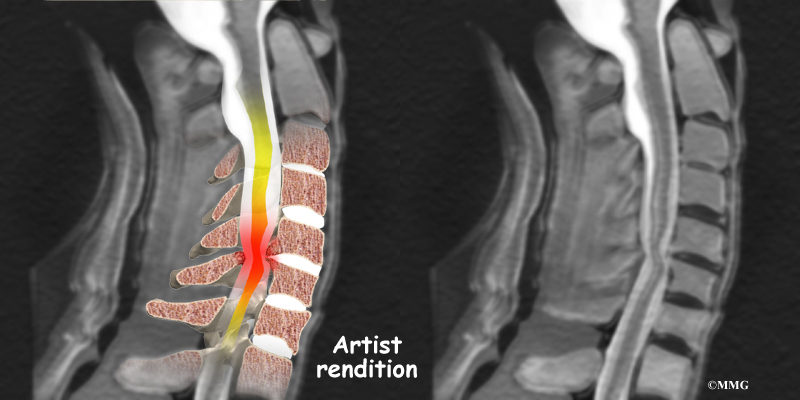
Gaze is down at the floor, instead of forward. The face is downward. The neck appears elongated, and the curve at the base of the neck is accentuated. This can cause over stretching or pinching of the spinal cord. When this happens, there may be weakness and numbness of the arms or entire body.
Dropped head syndrome can also cause difficulty swallowing, speaking, and breathing.
Diagnosis
How will my doctor diagnose this condition?
Diagnosis begins with a complete history and physical exam. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities.
Your doctor will do a physical examination to test your reflexes, skin sensation, muscle strength.
Most of the time, loss of of neck extension occurs as part of a more generalized neurological disorder. Neurological conditions must be considered first because some are treatable. A neurologist will usually be involved to help decide what is causing the chin-on-chest deformity.
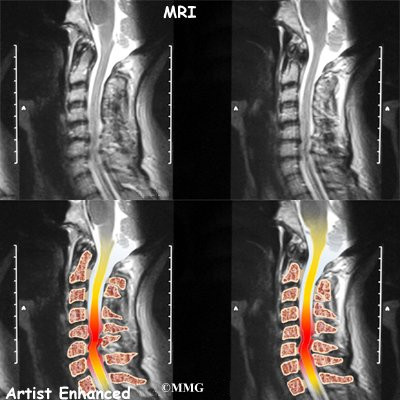
Your doctor will likely ask that you have magnetic resonance imaging (MRI) of your neck. The MRI machine uses magnetic waves rather than X-rays. It shows the anatomy of the neck. It is very good at showing the spinal cord and nerves. The test does not require a dye or a needle.
Electromygraphy (EMG) uses small diameter needles in the muscle belly being tested. It helps determine how well the nerve conducts signals to the muscles.
A muscle biopsy may be needed. A small piece of muscle is removed and examined under a microscope. A closer look at the muscle fibers can be helpful in making a diagnosis.
In isolated neck extensor myopathy (INEM), the muscle biopsy is non-specific. EMG shows some myopathic changes. Labs are normal.
If no other associated neurologic disorders are found, then the diagnosis of isolated neck extensor myopathy (INEM) is made. It is a diagnosis of exclusion, meaning that everything else that could caused it has been ruled out. It is not known what causes isolated neck extensor myopathy (INEM).
Some doctors feel that isolated neck extensor myopathy (INEM) is caused by either a non-specific non-inflammatory or inflammatory response that is restricted to the neck extensor muscles. Another possible cause is thoracic kyphosis. When the natural curve of the thoracic spine is increased, it may place the extensor muscles at a disadvantage given the weight of the head. This may cause over stretching and weakness of the extensor muscles.
Treatment
What treatment options are available?
Isolated neck extensor myopathy (INEM) is considered benign because it does not spread or get worse. Symptoms can improve in some cases. It is most often treated conservatively.
Nonsurgical Treatment
Treatment of Dropped Head Syndrome is mainly supportive. The weakness remains localized to the neck extensor muscles, physical therapy may help with this. There are some cases that improve dramatically, but most usually do not improve.
The most useful treatment is use of a neck collar. It can partially correct the chin-on-chest deformity. This improves the forward gaze and activities of daily living. It also can help prevent contractures of the neck in a fixed flexed posture. However, it can be uncomfortable and cause sores under the chin. Some use a baseball cap attached to straps around the trunk. This avoids the chin discomfort from using a collar.
Prednisone is a potent anti-inflammatory that may be prescribed. It may be beneficial when there is local myositis, or inflammation of the muscles. It can be taken in a pill form by mouth or intravenously.
Surgery
Unless fusion is necessary, surgery is usually not recommended in Dropped Head Syndrome.
When there is damage to the nerves in the neck or spinal cord, surgery to fuse the neck may be necessary. This usually requires a fusion from C2-T2. The loss of neck movement after fusion leaves patients unable to see the ground in front of their feet. This makes them at greater risk for falls. The inconvenience caused by having a rigid neck may prove to be a greater problem than the original dropped head deformity.
Osteoporosis, particularly in older females also poses a problem with surgery. The soft bone may allow the metal used to stabilize the spine to pull out.
Rehabilitation
What should I expect as I after treatment?
Nonsurgical Rehabilitation
Physical therapy is usually recommended. Neck extension strengthening exercises may provide some improvement. However, most patients will find the strengthening both tiring and frustrating. When lying down on your back you can move the neck to maintain range of motion. This helps to avoid unnecessary stiffness and shortening of the muscles in the front of the neck.
Range of motion exercises should be done on an ongoing basis to avoid contractures of the neck. Wearing a neck collar when up will likely improve activities of daily living.
Speech therapy may be recommended for swallowing, feeding, and breathing problems. Some people may need to have a feeding tube inserted through the stomach.
Your doctor may want to repeat imaging of the spine. There is the possibility of over stretching or pinching the spinal cord when the neck extensors are so weak. You will need to watch for symptoms such as weakness or numbness in the arms or other portions of the body. Bowel and bladder function could become a problem.
After Surgery
If surgery is recommended, you will probably require an overnight hospital stay or a few days stay. Initially, you will not be allowed to lift, and you will have to move carefully. Most likely your neck will be placed in a fairly rigid brace. You will eventually be able to resume your normal activities. You can expect healing of the fusion in three to nine months.
Physical therapy is usually recommended after surgery. Neck extension strengthening exercises are prescribed to prevent contracture of the neck. Occupational therapy may be recommended to help with arm strengthening. It can also help with dressing, and other activities of daily living. Equipment needs can be evaluated by the occupational therapist. Speech therapy may also be recommended after surgery.
Your surgeon will want to follow up with you on a regular basis. Imaging studies may need to be repeated on occasion. Assessment of the fusion is usually done with X-rays.
Whiplash
A Patient’s Guide to Whiplash
Introduction
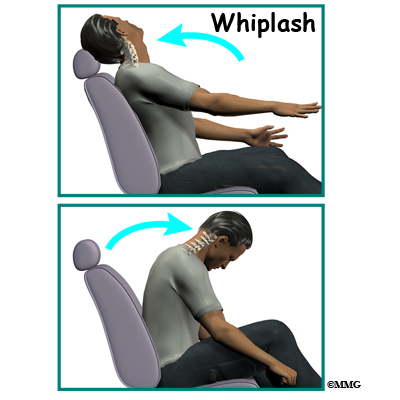
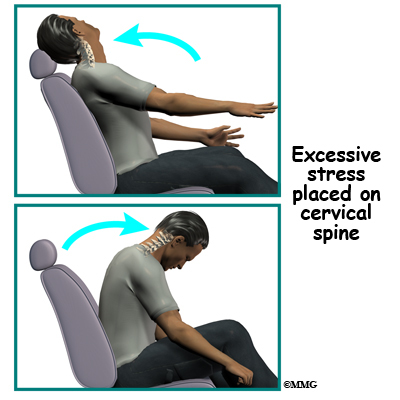
Whiplash is defined as a sudden extension of the cervical spine (backward movement of the neck) and flexion (forward movement of the neck). This type of trauma is also referred to as a cervical acceleration-deceleration (CAD) injury. Rear-end or side-impact motor vehicle collisions are the number one cause of whiplash with injury to the muscles, ligaments, tendons, joints, and discs of the cervical spine.
This guide will help you understand
- what parts make up the spine and neck
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts of the spine are involved?
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
The cervical spine is formed by the first seven vertebrae referred to as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom edge of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine. This is where the chest begins.
A bony ring attaches to the back of the vertebral body. When the vertebrae are stacked on top of each other, the rings form a hollow tube. This bony tube surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
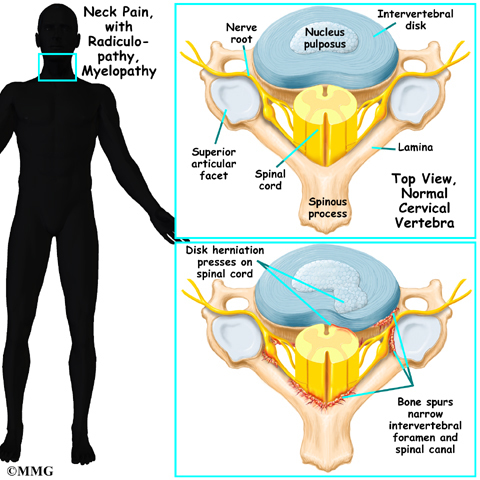
As the spinal cord travels from the brain down through the spine, it sends out nerve branches between each vertebrae called nerve roots. The nerve roots that come out of the cervical spine form the nerves that go to the arms and hands.
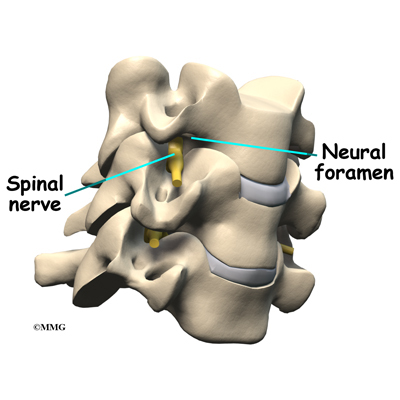
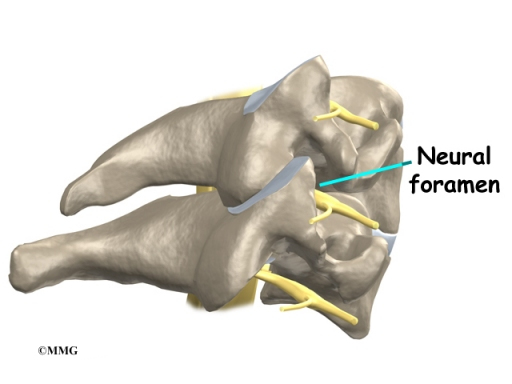
Two spinal nerves exit the sides of each spinal segment, one on the left and one on the right. As the nerves leave the spinal cord, they pass through a small bony tunnel on each side of the vertebra, called a neural foramen. (The term used to describe more than one opening is neural foramina.)
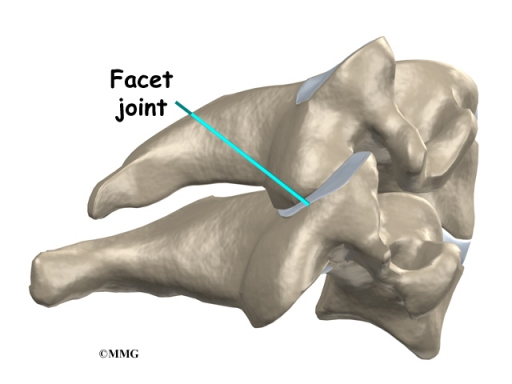
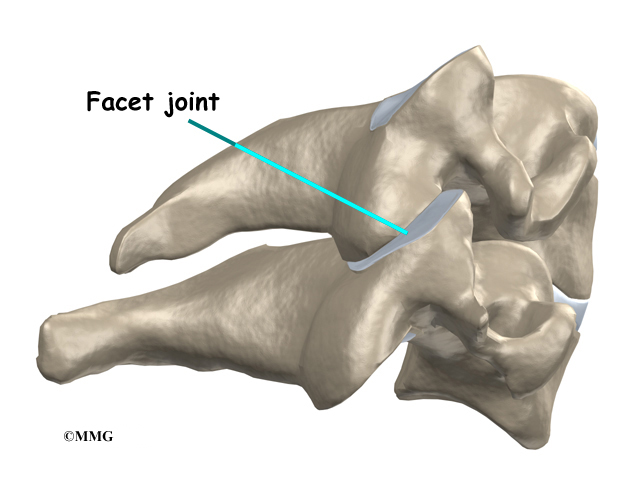
Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at that level, and the small facet joints that link each level of the spinal column.
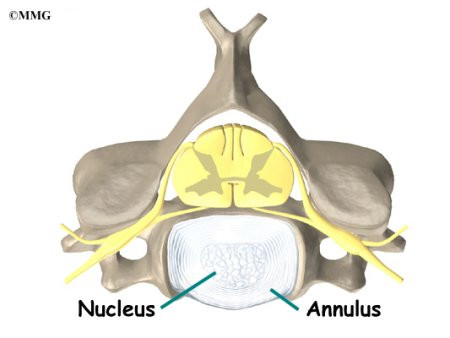
An intervertebral disc is made of connective tissue. Connective tissue is the material that holds the living cells of the body together. The disc is a specialized connective tissue structure that separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
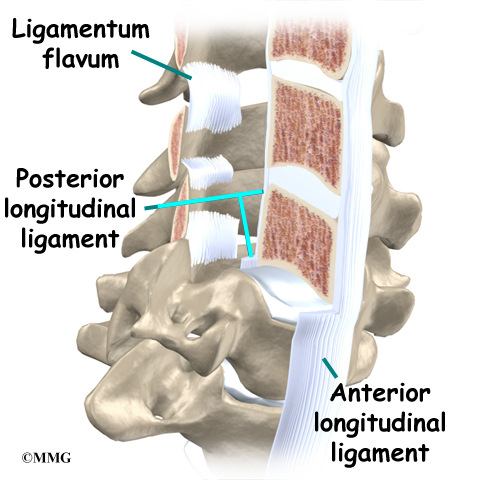
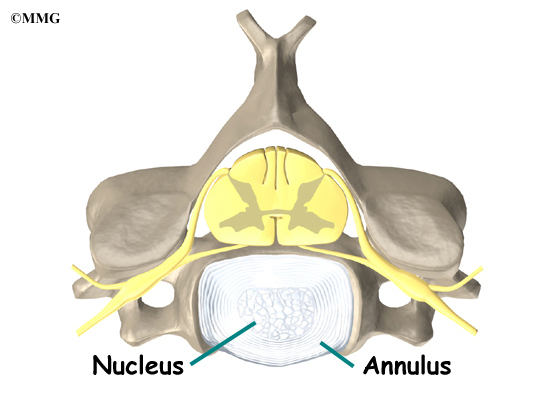
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
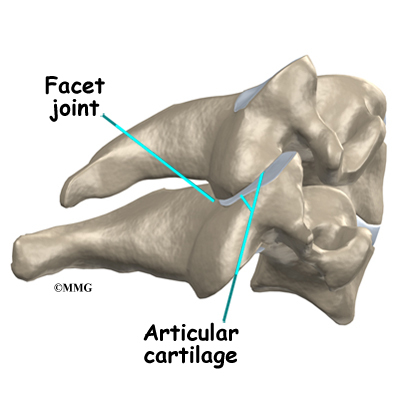
There are two facet joints between each pair of vertebrae–one on each side of the spine. The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the bone ends to move against each other smoothly, without pain. The alignment of the facet joints of the cervical spine allows freedom of movement as you bend and turn your neck.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
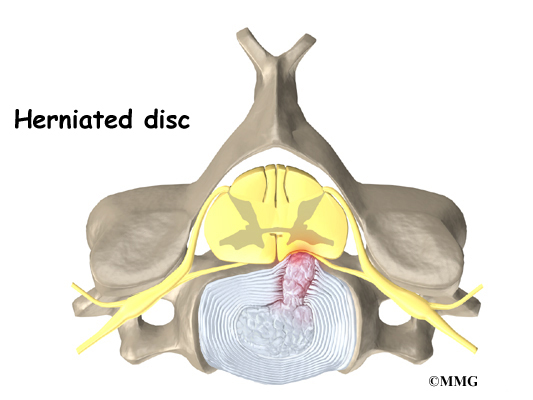
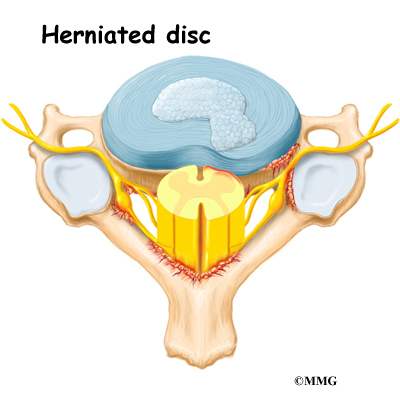
When the head and neck are suddenly and forcefully whipped forward and back, mechanical forces place excessive stress on the cervical spine. Traumatic disc rupture and soft tissue damage can occur.
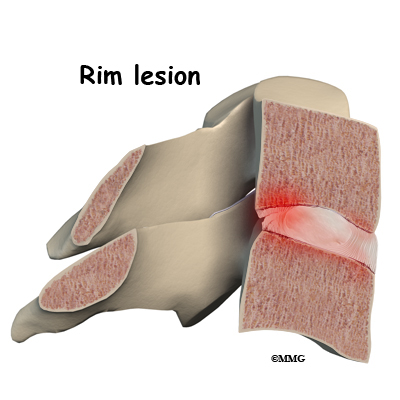
The cartilage between the disc and the vertebral bone is often cracked. This is known as a rim lesion.
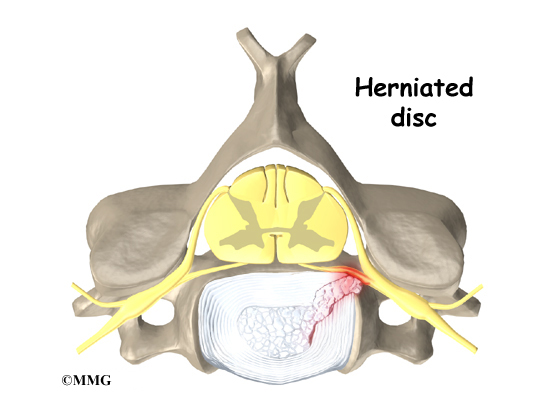
Damage to the disc can put pressure on the nerves as they exit the spine. The pressure or irritation can be felt as numbness on the skin, weakness in the muscles, or pain along the path of the nerve. Most people think of these symptoms as indications of a pinched nerve. Health care providers call this condition cervical radiculopathy.
Soft tissue around the facet joint can be injured. Many of the pain-sensing nerves of the spine are in the facet joints. The normally smooth surfaces on which these joints glide can become rough, irritated, and inflamed. Studies show that neck pain often comes from the damaged facet joints.
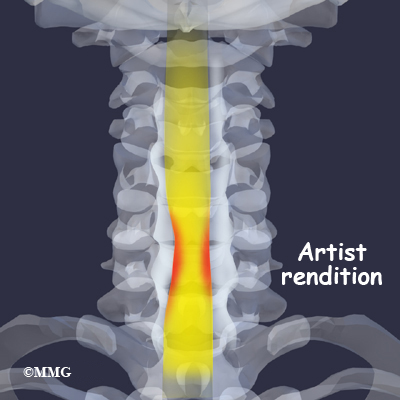
Low back pain is a common feature after a whiplash injury. Studies show that there is significant electrical activity in the muscles of the lumbar spine when the neck is extended. This effect increases when there is neck pain, possibly as a way to help stabilize the spine when neck pain causes weakness.
More than anyplace else in the body, the muscles of the neck sense sudden changes in tension and respond quickly. Tiny spindles in the muscles signal the need for more muscle tension to hold against the sudden shift in position.
The result is often muscle spasm as a self-protective measure. The increased muscle tone prevents motion of the inflamed joint. You may experience neck stiffness as a result.
Risk Factors
Each year, about three million people experience whiplash injuries to their neck and back. Of these three million people, only about one-half, will fully recover. About 600,000 of those individuals will have long-term symptoms, and 150,000 will actually become disabled as a result of the injury.
There are many factors that come into play when a person is injured in a rear-end motor vehicle accident. Any one or more of the following factors can affect recovery:
- Head turned one way or the other at the time of the impact (increases risk of nerve
involvement with pain down the arm) - Getting hit from behind (rear-impact collision)
- Previous neck pain or headaches
- Previous similar injury
- Being unaware of the impending impact
- Poor posture at the time of impact (head, neck, or chest bent forward)
- Poor position of the headrest or no headrest
- Crash speed under 10 mph
- Being in the front seat as opposed to sitting in the back seat of the car
- Collision with a vehicle larger than yours
- Being of slight build
- Wearing a seatbelt (a seat belt should always be worn, but at lower speeds, a lap and shoulder type seat belt will increase the chances of injury)
Symptoms
What are some of the symptoms of whiplash?
- Neck pain or neck pain that travels down the arm (radiculopathy)
- Headaches
- Low back pain (LBP)
- Jaw pain
- Dizziness
Ninety percent of patients involved in whiplash type accidents complain of neck pain. This is by far the most common symptom. The pain often spreads into the upper back, between the shoulder blades, or down the arm. Neck pain that goes down the arm is called radiculopathy.
Low back pain (LBP) can occur as a result of a whiplash injury. The Insurance Research Council reports that LBP occurs in 39 per cent of whiplash patients. Some studies found LBP to be present in 57 per cent of rear-impact collisions in which injuries were reported and 71 per cent of side-impact collisions.
Jaw pain as a result of temporomandibular joint (TMJ) injury can also cause painful headaches. The TMJ is formed by the bone of the mandible (lower jaw) connecting to the temporal bone at the side of the skull. The TMJ is a hinge joint that allows the jaw to open and close and to move forward, back, and sideways. Pain in this joint in called temporomandibular joint disorder (TMD).
Dizziness is quite common with a sense of lost balance being reported. It is caused by an injury to the joints of the neck called facet or zygapophyseal joints. When dizziness is reported, it should be distinguished from vertigo (also known as benign paroxysmal positional vertigo (BPPV), which results from an injury to the inner ear.
Other symptoms often reported include, but are not limited to: shoulder pain; numbness or tingling in the arms, hands, legs or feet; facial pain, fatigue, confusion, poor concentration, irritability, difficulty sleeping, forgetfulness, visual problems, and mood disorders.
It is not uncommon to have a delay in your symptoms. It is actually more common to have a 24 to 72 hour delay as opposed to immediate symptoms or pain. This is most likely due to the fact that it takes the body 24 to 72 hours to develop inflammation. Disc injuries may take even longer to manifest themselves. It is not uncommon for a disc injury to remain pain free and unnoticed for weeks to months.
Simply because there is little or no damage to your car does not mean that you were not injured. In fact, more than half of all whiplash injuries occur where there was little or no damage to one or both of the vehicles involved.
When we see visible damage to a car, it means that the car has absorbed much of that force and less force is transmitted to the occupant. On the other hand, if there is little or no damage to the car, the force is not absorbed but transferred to the driver or passengers, potentially resulting in greater injury.
Diagnosis
How do doctors diagnose the problem?
The diagnosis of neck problems begins with a thorough history of your condition and the involved car accident. You might be asked to fill out a questionnaire describing your neck problems. Then your doctor will ask you questions to find out when you first started having problems, what makes your symptoms better or worse, and how the symptoms affect your daily activity. Your answers will help guide the physical examination.
Your doctor will then physically examine the muscles and joints of your neck. It is important that your doctor see how your neck is aligned, how it moves, and exactly where it hurts.
Your doctor may do some simple tests to check the function of the nerves. These tests measure your arm and hand strength, check your reflexes, and help determine whether you have numbness in your arms, hands, or fingers.
The information from your medical history and physical examination will help your doctor decide which tests to order. The tests give different types of information.
Radiological Imaging
Radiological imaging tests help your doctor see the anatomy of your spine. There are many kinds of imaging tests including:
- X-rays
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Digital motion x-ray (DMX)
- Myelogram
- Bone Scan
- Electromyogram
X-rays
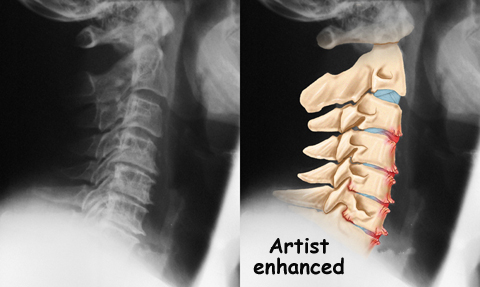
X-rays show problems with bones, such as infection, bone tumors, or fractures. X-rays of the spine also can give your doctor information about how much degeneration has occurred in the spine, such as the amount of space in the neural foramina and between the discs.
X-rays are usually the first test ordered before any of the more specialized tests. Special x-rays called flexion/extension x-rays may help to determine if there is instability between vertebrae. These x-rays are taken from the side as you bend as far forward and then as far backward as you can. Comparing the two x-rays allows the doctor to see how much motion occurs between each spinal segment.
Magnetic resonance imaging (MRI)
If more information is needed, your doctor may order an MRI. The MRI machine uses magnetic waves rather than x-rays to create pictures of the cervical spine in slices. MRIs show the cervical spine vertebrae, as well as the soft tissue structures, such as the discs, joints, and nerves. MRI scans are painless and don’t require needles or dye. MRI scan has become the most common test to look at the cervical spine after x-rays have been taken.
Computed Tomography (CT)
CT scan is a special type of x-ray that lets doctors see slices of bone tissue. The machine uses a computer and x-rays to create these slices. It is used primarily when problems are suspected in the bones.
Digital motion x-ray (DMX)
DMX is a new fluoroscopic based x-ray system designed to objectively detect and document soft tissue/ligament injury most commonly associated with whiplash injuries of the spine. DMX evaluates biomechanical relationships and abnormal movements of the cervical spine. Specifically, DMX:
- Shows abnormal movement of vertebral bodies, facets, and other spinal elements
- Shows joint hypermobility, hypomobility, or restriction
- Shows normal or abnormal initiation of cervical motion
DMX uses digital and optic technology now available. DMX is the latest generation of videofluoroscopy (VF) that uses low doses of radiation. The images have improved clarity and resolution over VF and are recorded digitally on CD or DVD disc. DMX digital images can be replayed and studied on standard computer systems. DMX images are simply x-ray images taken at 30 frames per second to form a multiple radiographic array or series that can be run as a movie file to display real time motion of the joints of the body.
DMX radiographic series can be paused at any location and the measurements and interpretation common to radiology can be applied to the still images. These images would be identical to plain film images if plain film radiography were performed at the same location at the same moment in motion. DMX acquires approximately 2700 images for the same amount of radiation as seven regular x-rays.
For more information visit http://www.dmxofmontana.com
Myelogram
The myelogram is a special kind of x-ray test where a special dye is injected into the spinal sac. The dye shows up on an x-ray. It helps a doctor see if there is a herniated disc, pressure on the spinal cord or spinal nerves, or a spinal tumor. Before the CT scan and the MRI scan were developed, the myelogram was the only test that surgeons had to look for a herniated disc. The myelogram is still used today but not nearly as often. The myelogram is usually combined with CT scan to give more detail.
Bone Scan
A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special x-rays of your neck. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem and other tests such as the CT scan or MRI scan are then used to look at the area in detail.
Electromyogram (EMG)
An electromyogram (EMG) is a special test used to determine if there are problems with any of the nerves going to the upper limbs. EMGs are usually done to see if one or more nerve roots have been pinched by a herniated disc. During the test, small needles are placed into certain muscles that are supplied by each nerve root. If there has been a change in the function of the nerve, the muscle will send off different types of electrical signals. The EMG test reads these signals and can help determine which nerve root is involved.
Grading the Severity of Injury
The physical exam combined with the imaging studies help determine the severity or grade of the injury. There is more than one way to assign a grade to a patient’s whiplash. Here are two examples of the more commonly used models used to classify or grade whiplash injuries:
Croft Guidelines
- Grade I: Minimal – No limitation of motion, no ligamentous injury, no neurological findings
- Grade II: Slight – Slight limitation of motion, no ligamentous injury, no neurologic findings
- Grade III: Moderate – Limitation of motion, ligamentous instability, neurologic symptoms present
- Grade IV: Moderate-to-Severe – Limitation of motion, some ligamentous injury, neurological symptoms, fracture or disc derangement
Quebec Whiplash Classification
- Grade 0: No complaint or physical sign
- Grade I: Neck complaint of pain, stiffness or tenderness, no physical signs
- Grade II: Neck pain and musculoskeletal signs
- Grade III: Neck pain and neurological signs
- Grade IV: Neck pain and fracture or dislocation
Treatment
What treatment options are available?
Nonsurgical Treatment
Whenever possible, doctors prefer to use treatments other than surgery. The first goal of these nonsurgical treatments is to ease your pain and other symptoms.
Your health care providers will work with you to improve your neck movement and strength. They will also encourage healthy body alignment and posture. These steps are designed to enable you to get back to your normal activities. Conservative care may include:
- Immobilization
- Medication
- Injection
- Physical therapy
- Chiropractic care
Immobilization
At first, your doctor may prescribe immobilization of the neck. Keeping the neck still for a short time can calm inflammation and pain. This might include one to two days of bed rest and the use of a soft cervical (neck) collar.
The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. A soft cervical collar may be used for the first 24 to 48 hours to help provide support and reduce pain. There is no need for a hard or rigid cervical collar unless the neck is fractured.
Soft collars should not be worn after 48 hours without a physician’s approval. Studies show that prolonged immobilization can delay healing and promote disability. Wearing it longer tends to weaken the neck muscles and reduces the facet joints’ sense of position called proprioception.
A cervical support pillow may offer some additional support while sleeping and helps to keep the neck in a more neutral position. Cervical pillows can be used any time by anyone for improved alignment while sleeping.
Medication
Your doctor may prescribe certain types of medication if the nerves are irritated or compressed and you have neck pain that travels down your arm (radiculopathy). Severe symptoms may be treated with narcotic drugs, such as codeine or morphine. But these drugs should only be used for the first few days or weeks after problems with radiculopathy start because they are addictive when used too much or improperly. Muscle relaxants may be prescribed to calm neck muscles that are in spasm. You may be prescribed anti-inflammatory medications such as aspirin or ibuprofen.
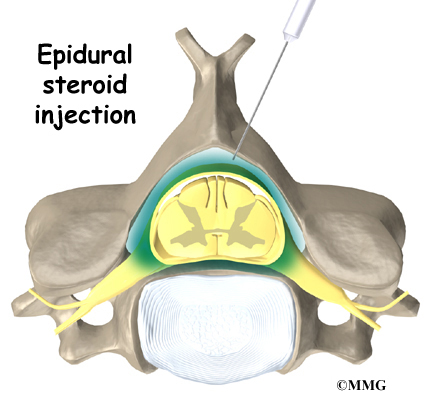
Injection
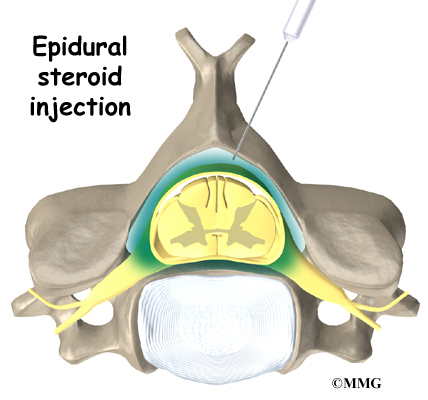
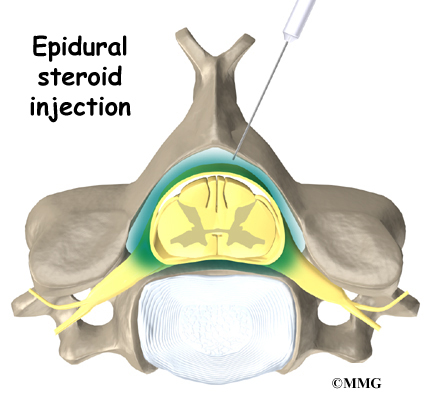
Pain resulting from irritation of the facet joints may be alleviated with injection of an anesthetic agent similar to Novacaine such as Bipuvacaine. This numbing agent both confirms the source of pain as coming from the joint and helps reduce or eliminate the pain.
Physical Therapy
Some doctors have their patients work with a physical therapist. If you require outpatient physical therapy, you will probably only need to attend therapy sessions for two to four weeks. Your rate of recovery helps determine the length of time in physical therapy. Patients with delayed recovery may need longer time in rehab.
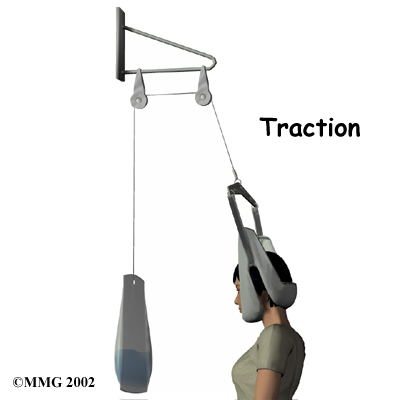
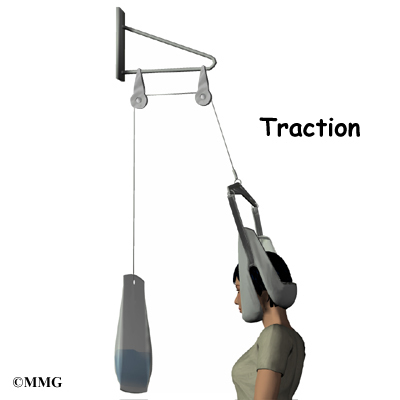
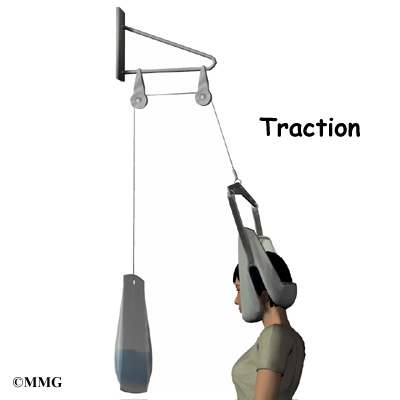
At first, treatment is focused on easing pain and reducing inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Electrical stimulation treatments can help calm muscle spasm and pain. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or the therapist can apply the traction pull by hand. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are added within the comfortable range of motion. The therapist will teach you specific exercises to help tone and control the muscles that stabilize the neck and upper back.
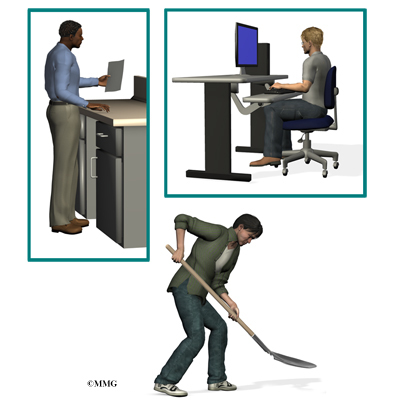
Your therapist will work with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. You’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job. Your therapist can also provide ideas for alternate forms of work. You’ll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Chiropractic care
Chiropractic care also offers another opportunity for relief of pain from a whiplash injury. Chiropractors adjust misalignments of the facet joints and vertebrae to restore the nerve signals and improve spinal health, which can impact overall physical health. Many chiropractors make these adjustments using a thrust technique called manipulation.
Chiropractors also take into account how nutrition, emotion, and environment affect our health. The chiropractor will assess your posture during daily activities, work, and sleep and offer you suggestions for ways to improve your day-to-day spinal alignment. You may be given some additional advice about the use of heat, cold, and exercise to help maintain the results of your chiropractic treatment.
Surgery
Most people with lingering effects from whiplash or cervical radiculopathy from whiplash get better without surgery. In rare cases, surgery may be suggested.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
You should expect full recovery to take up to three months. Integration of rehabilitation and manipulative therapy is central in getting back to your pre-injury status.
There is a strong emphasis on keeping as active as possible, which includes incorporating manual treatments and exercise. Before your rehab program ends, your healthcare team will teach you how to maintain any improvements you’ve made and ways to avoid future problems.
Cervical Artificial Disc Replacement
A Patient’s Guide to Cervical Artificial Disc Replacement
Introduction
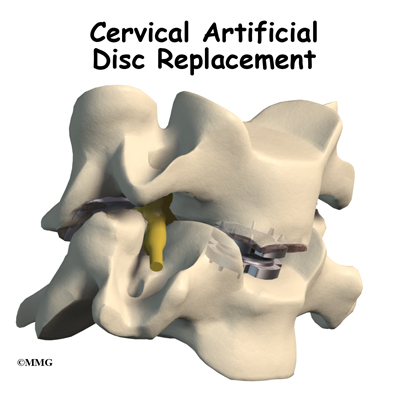
Artificial disc replacement (ADR) is relatively new. In June 2004, the first ADR for the lumbar spine (low back) was approved by the FDA for use in the US. Replacing a damaged disc in the cervical spine (neck) is a bit trickier. The disc is part of a complex joint in the spine. Making a replacement disc that works and that will last is not an easy task. There are now several Cervical artificial disc replacement devices that have been approved by the FDA for use in the United States.
The artificial disc is inserted in the space between two vertebrae. The goal is to replace the diseased or damaged disc while keeping your normal neck motion. The hope is that your spine will be protected from similar problems above and below the affected spinal level.
This guide will help you understand:
- what parts of the spine are involved
- what your surgeon hopes to achieve
- who can benefit from this procedure
- how do I prepare for surgery
- what happens during the procedure
- what to expect as you recover
Anatomy
What parts of the spine are involved?
Disc replacement typically occurs at cervical spine levels C4-5, C5-6, or C6-7. The first seven vertebrae make up the cervical spine. Doctors often refer to the cervical vertebrae as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine (the chest area) at the first thoracic vertebra, T1.
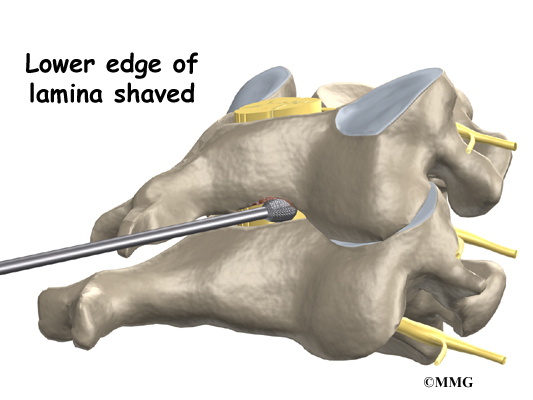
Each vertebra is made of the same parts. The main section of each cervical vertebrae, from C2 to C7,
is formed by a round block of bone, called the vertebral body. A bony ring attaches to the back of the vertebral body. This ring has two parts. Two pedicles connect directly to the back of the vertebral body. Two lamina bones join the pedicles to complete the ring. The lamina bones form the outer rim of the bony ring. When the vertebrae are stacked on top of each other, the bony rings form a hollow tube that surrounds the spinal cord. The laminae provide a protective wall around the spinal cord.
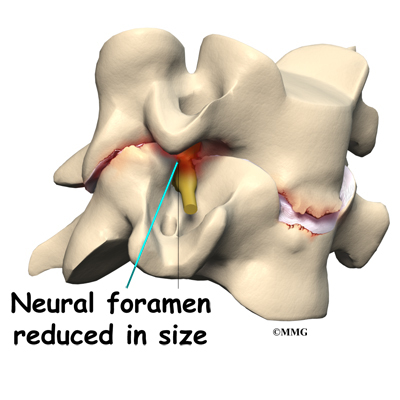
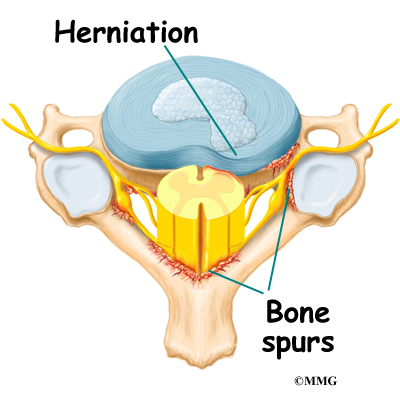
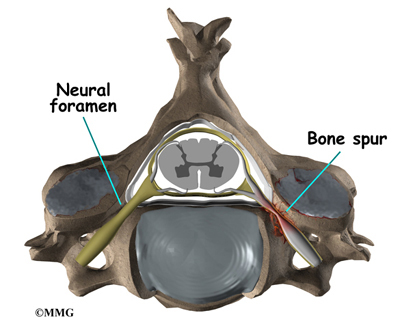
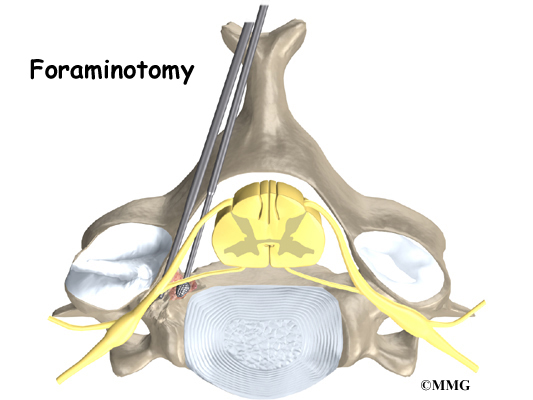
On the left and right side of each vertebra is a small tunnel called a neural foramen. (Foramina is the plural term.) The two nerves that leave the spine at each vertebra go through the foramina, one on the left and one on the right. The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits behind the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
A special type of structure in the spine called an intervertebral disc has two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption in the spine. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What does the surgeon hope to achieve?
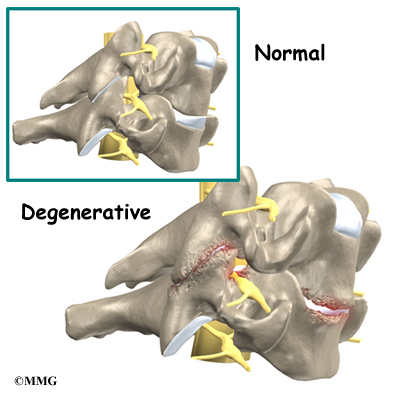
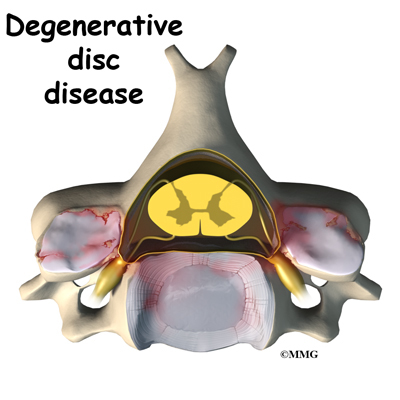
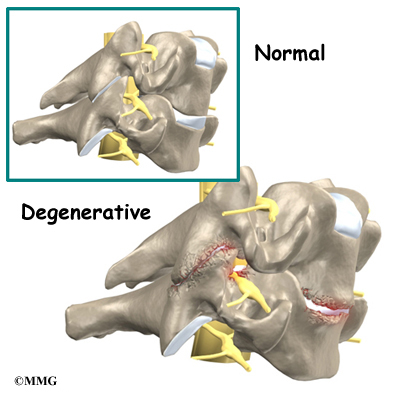
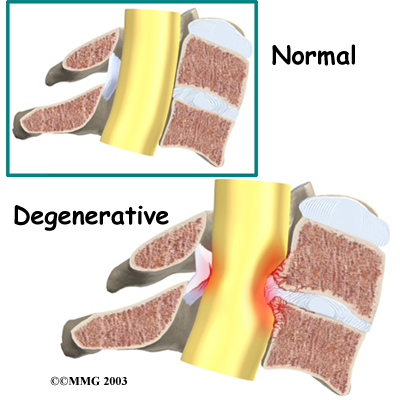
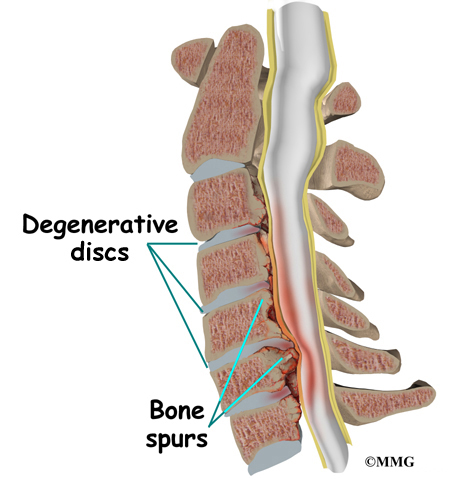
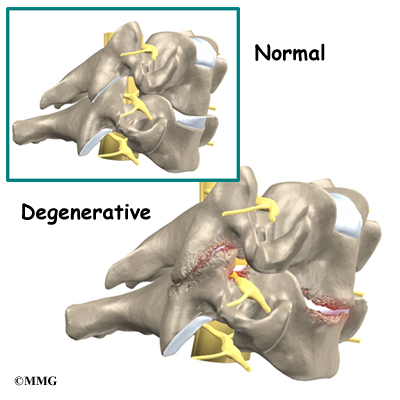
Disc replacement surgery is done to stop the symptoms of degenerative disc disease. Discs wear out or degenerate as a natural part of aging and from stress and strain on the neck. Eventually, the problem disc collapses. This causes the vertebra above to sink toward the one below. This loss of disc height affects the nearby structures – especially the facet joints.
When the disc collapses, it no longer supports its share of the load in the cervical spine. The facet joints of the spine begin to support more of the force that is transmitted between each vertebra. This increases the wear and tear on the articular cartilage that covers the surface of the joints. The articular cartilage is the smooth, slippery surface that covers the surface of the bone in any joint in the body. Articular cartilage is tough, but it does not tolerate abnormal pressure well for long. When damaged, articular cartilage does not have the ability to heal. This wear and tear is what is commonly referred to as arthritis.
Shrinking disc height also reduces the size of the neural foramina, the openings between each vertebral pair where the nerve roots leave the spinal column. The arthritis also results in the development of bone spurs that may protrude into these openings, further narrowing the space that the nerves have to exit the spinal canal. The nerve roots can end up getting squeezed where they pass through the neural foramina.
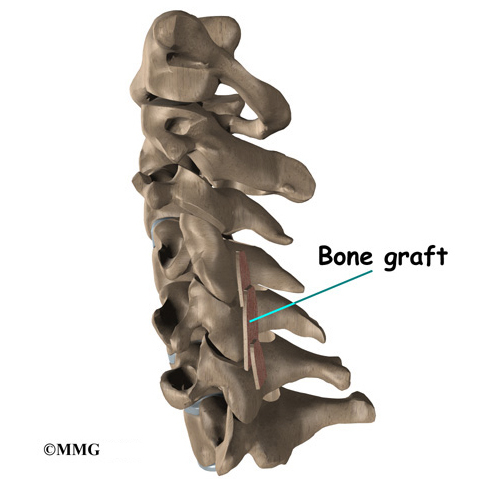
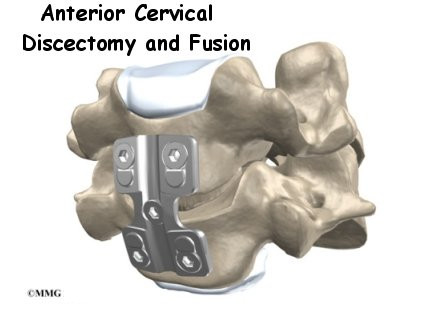
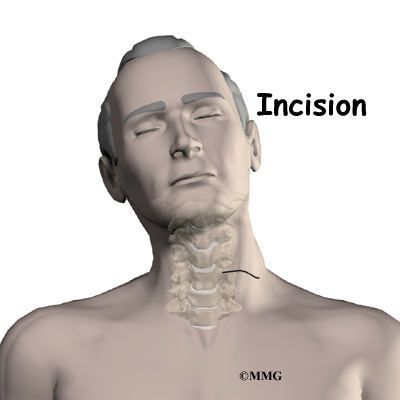
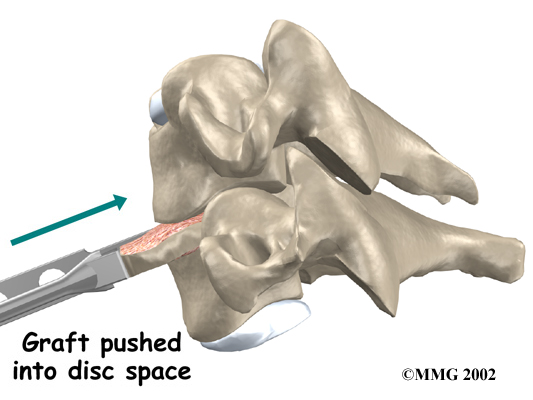
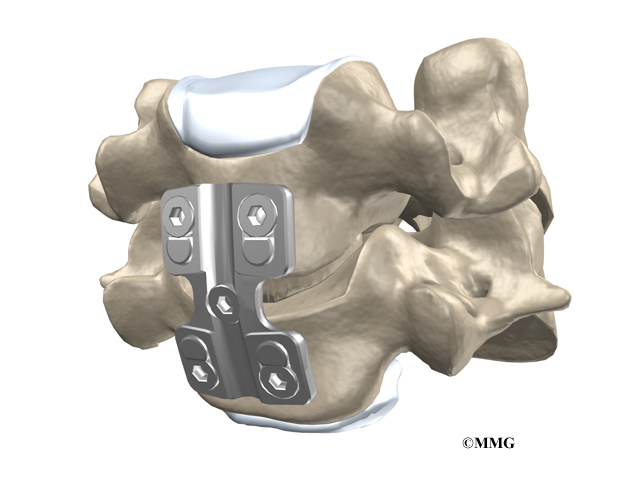
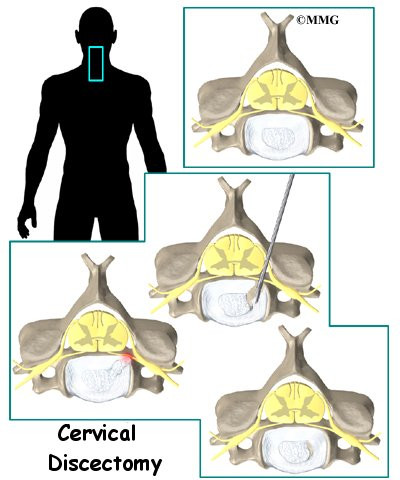
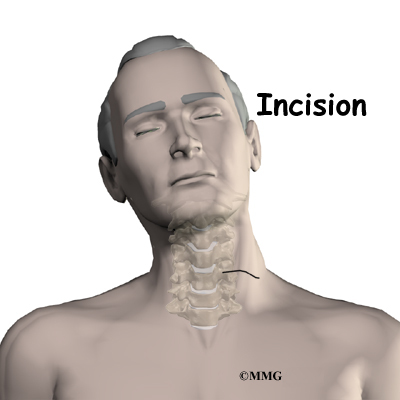
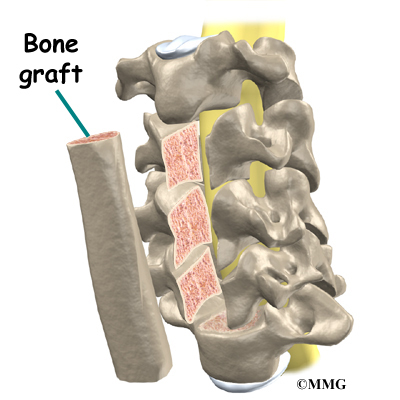
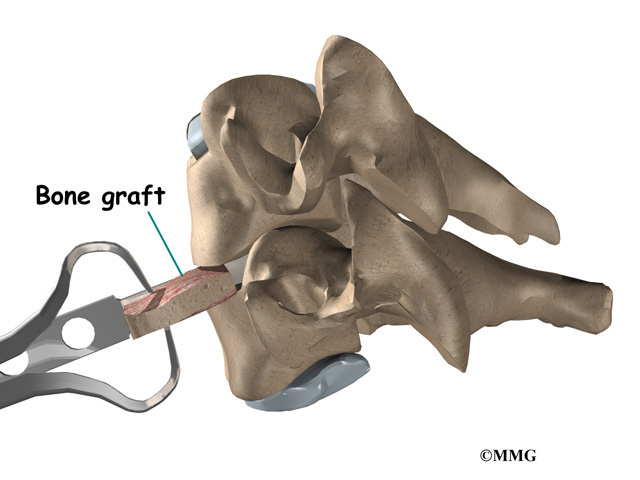
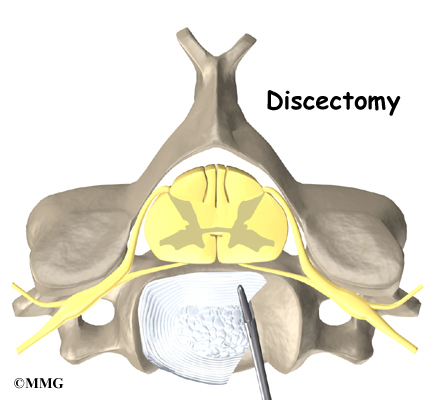
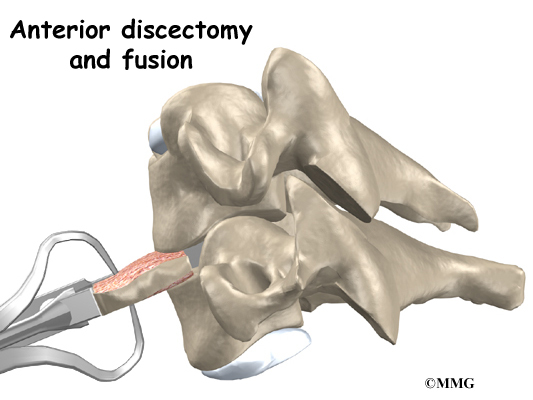
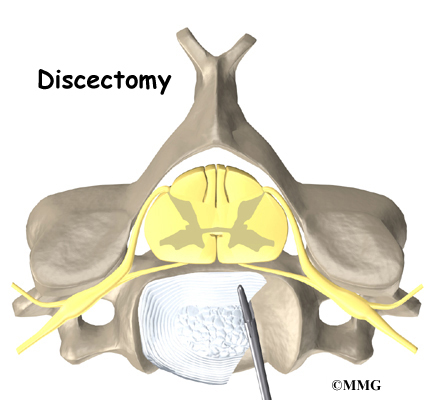
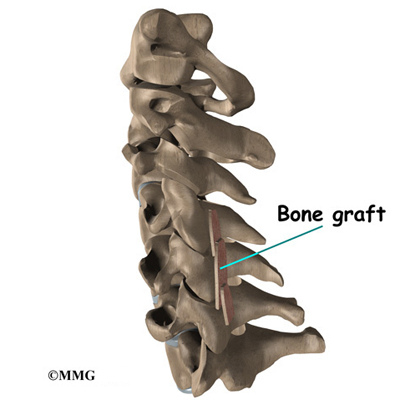
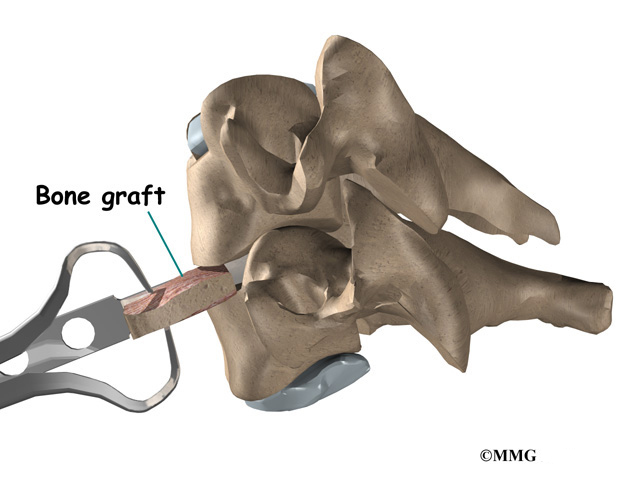
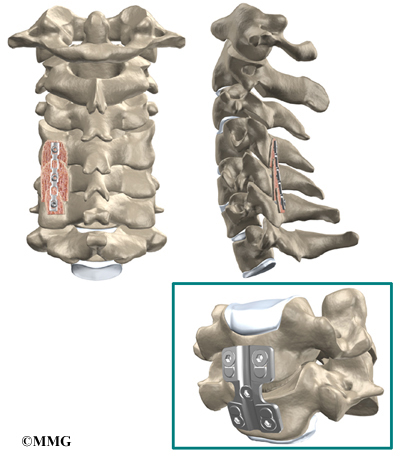
The traditional way of treating severe neck pain caused by disc degeneration is a procedure called an anterior cervical discectomy and fusion. In this procedure, the surgeon makes an incision in the anterior (front) of the neck, performs a discectomy (removes the disc) and fuses the two vertebrae together. A fusion simply means that two bones grow together. Usually, when two vertebrae are fused together, a small piece of bone called a bone graft is inserted between the two vertebrae where the disc has been removed. This bone graft serves to both separate the vertebrae and to stimulate the two bones to grow together – or fuse.
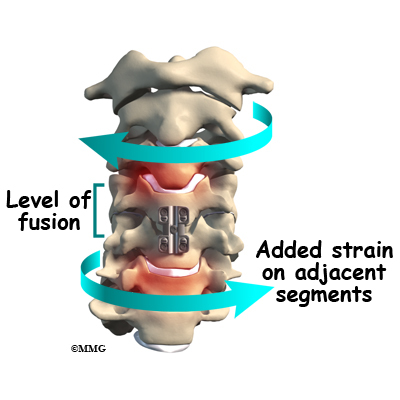
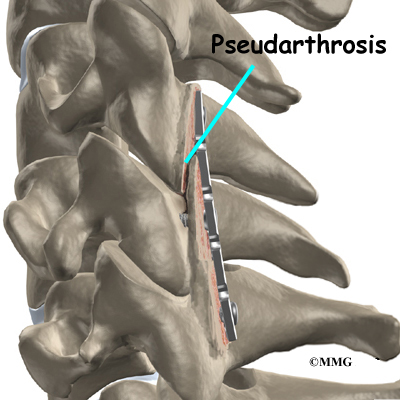
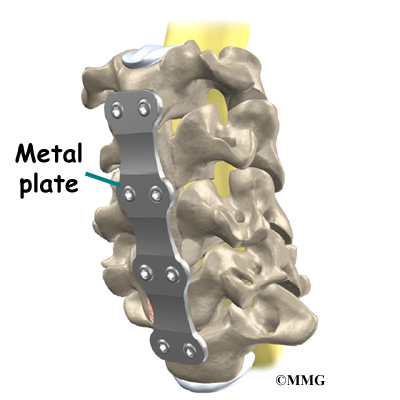
The fusion procedure usually involves the use of hardware, such as screws, plates, or cages to keep the bones from moving. Fusion restricts movement in the problem area, but it creates greater strain on the healthy spinal segments above and below. The added strain may eventually cause these segments to wear out. This is called adjacent-segment degeneration.
Replacing the damaged disc with an artificial disc, or implant, called a prosthesis can restore the normal distance between the two vertebrae. The artificial disc sits between the two vertebrae and “jacks up” the upper vertebra. Enlarging the disc space relieves pressure on the facet joints. It also opens up the space around the spinal nerve roots where they pass through the neural foramina.
Another benefit of the artificial disc replacement is that it mimics a healthy disc. Natural motion is preserved in the spine where the new disc is implanted. And it helps maintain stability in the spinal joints above and below it.
Who can benefit from this procedure
The indications for a cervical disc replacement are generally the same as for a cervical discectomy and fusion. A person must have symptoms from a cervical disc problem. Symptoms include neck and/or arm pain, arm weakness, or arm and hand numbness. These symptoms may be due to a herniated disc and/or bone spurs called osteophytes pressing on adjacent nerves or the spinal cord. This condition typically occurs at cervical spine levels C4-5, C5-6, or C6-7.
Artificial disc replacement is still somewhat new in the United States. In the United States, surgeons are currently only replacing one cervical disc in a patient’s cervical spine at this time. In Europe, surgeons are replacing more than one disc. More surgeons in the United States will probably start replacing more than one cervical disc in the near future.
Cervical artificial disc replacement is indicated for the treatment of radiculopathy (pressure on the spinal nerve) and myelopathy (pressure on the spinal cord) at one or two levels. In the future, it may be used for the treatment of three or more symptomatic levels or levels adjacent to a cervical spine fusion. This use is still under investigation.
More data is needed before the uses of cervical artificial disc replacements are expanded to other problems in the cervical spine. Cervical artificial disc replacement is not advised when there is cervical spine instability, significant facet joint damage, or infection.
Preparation
How should I prepare for surgery?
Your spine surgeon will gather a variety of information before recommending disc replacement surgery. In addition to taking a history and doing a physical exam, your surgeon may order various diagnostic studies, such as x-rays, magnetic resonance imaging (MRI) scans, CT scans, or discograms.
Once you and your surgeon have agreed that disc replacement surgery is indicated, certain preparations for the surgery are important. Your doctor may tell you to be NPO for a certain amount of time before the procedure. This means that you should not eat or drink anything for a certain amount of time before your procedure. This means no water, no coffee, no tea – not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You should tell your doctor if you are taking any medications that thin your blood or interfere with blood clotting. The most common blood thinner is Coumadin. Other medications also slow down blood clotting. Aspirin, ibuprofen, and nearly all of the anti-inflammatory medications affect blood clotting. So do medications used to prevent strokes such as Plavix. These medications usually need to be stopped seven days prior to the procedure. Be sure to let your doctor know if you are on any of these medications.
You should stop smoking or using tobacco in any form as soon as possible before surgery. This is very important to reduce complications from heart and lung problems. Tobacco use, especially smoking, also decreases the success rate of spine surgery. Stopping smoking will increase your chances of a successful result.
Discussions will be held with your family and people who may be assisting you once you return from the hospital. You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition possible prior to the surgery.
Hospitals often have preoperative teaching for patients undergoing major spinal operations. These teaching sessions can help you understand what to expect both while you are in the hospital and after you return home. A doctor who will be performing your anesthesia (an anesthesiologist) will evaluate and counsel you regarding anesthesia.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the artificial disc itself.
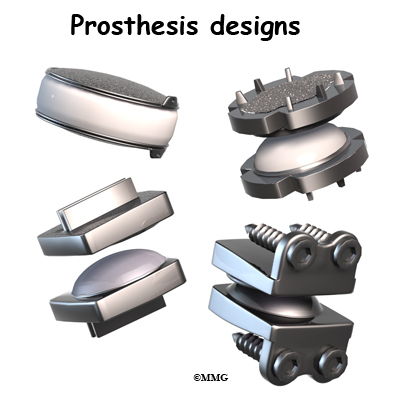
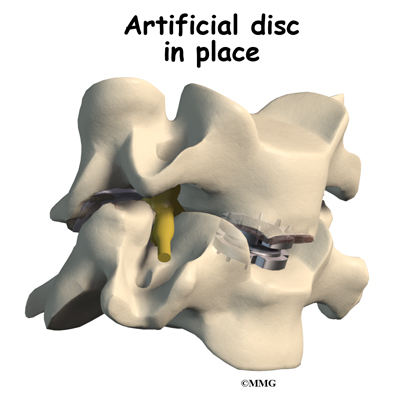
The cervical artificial disc has several different designs. Some look like a sandwich with two endplates separated by a plastic spacer. The two endplates are made of cobalt chromium alloy, a safe material that has been used for many years in replacement joints for the hip and knee.
A plastic (polyethylene) core fits in between the two metal endplates. The core acts as a spacer and is shaped so that the endplates pivot in a way that imitates normal motion of the two vertebrae. There are small prongs on one side of each endplate. The prongs help anchor the endplate to the surface of the vertebral body.
Another artificial disc replacement design is a ball and socket articulation to allow for normal translation of motion at that segment. The implant may be made of titanium and polyurethane in a metal-on-plastic design. Some are made of stainless steel and are all metal-on-metal.
Inserted between two vertebrae, the prosthesis reestablishes the height between two vertebrae. As a result of enlarging the disc space, the nearby spinal ligaments are pulled tight, which helps hold the prosthesis in place. The prosthesis is further held in place by the normal pressure through the spine.
The Operation
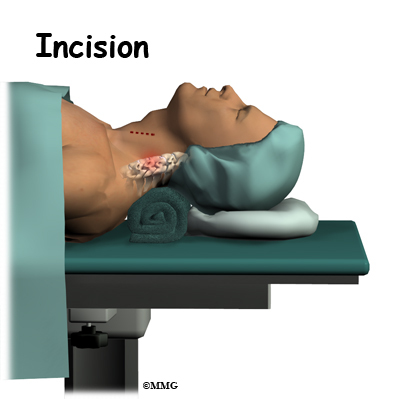
The operation is done from the anterior (front) of the body. This surgical approach is the same as that presently used for a discectomy and fusion operation. To do this, the patient is placed on his or her back. An incision is made through the skin and the thin muscles of the front of the neck. The blood vessels, the trachea (windpipe), and the esophagus are moved to the side so that the surgeon can see the front of the cervical spine. The disc that is to be replaced is identified using the fluoroscope. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure.
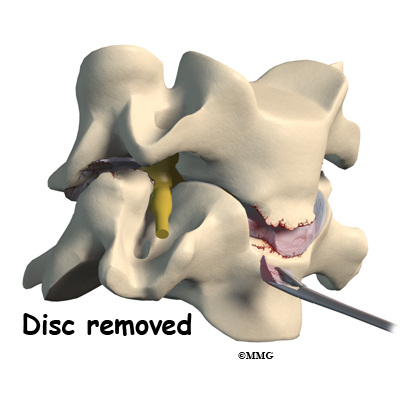
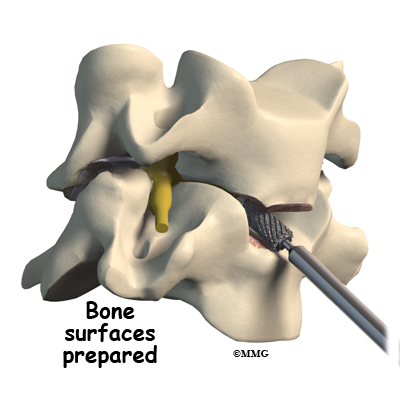
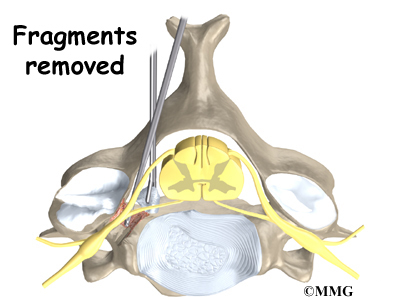
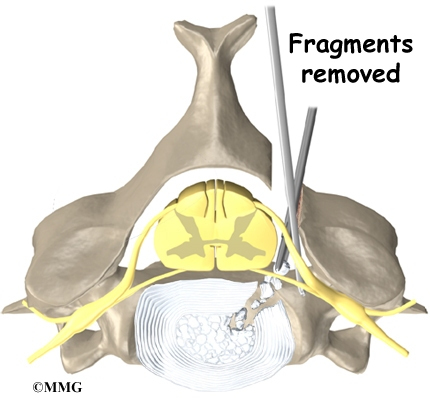
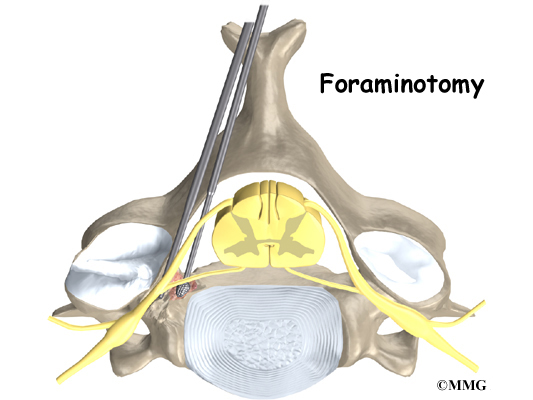
Working from the front of the spine, the spine surgeon removes a large section from the middle of the damaged disc. Next, the bones of the spine are spread apart to make more room to see and work inside the disc space. Using a surgical microscope, any remaining disc material toward the back of the disc is removed. The surgeon will also remove any disc fragments pressing against the nerve and shave off any osteophytes (bone spurs).
The disc space is distracted (jacked up) to its normal disc height. This step helps decompress or take pressure off the nerves. At this point, x-rays or a fluoroscope, is used to insert the artificial disc device into the prepared disc space. This allows the doctor to watch where the implant goes as it is inserted. This makes the procedure much safer and much more accurate.
Finally, the prosthesis is tested by moving the spine in various positions. An X-ray may be taken to double check the location and fit of the new disc.
View animation of artificial disc replacement
Complications
What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Weigh these as you gather advice and information. Be sure to discuss the possible risks of disc replacement with your spine surgeon.
Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
However, information from the disc replacement operations shows a low rate of complications. There have been no reports of death, significant infection, or major neurological problems.
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are
- anesthesia complications
- thrombophlebitis
- infection
- blood loss
- nerve injury or paralysis
- spontaneous ankylosis (fusion)
- subsidence (sinking)
- implant failure (need for further surgery)
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Blood Loss
Cervical disc replacement surgery carries risks associated with operating from the front of the spine. Blood vessels that travel near the front of the spine may be injured during anterior cervical surgery.
Nerve Injury
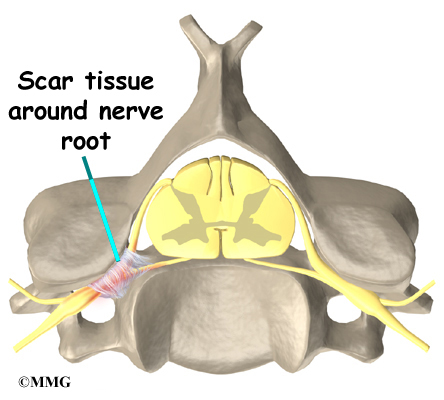
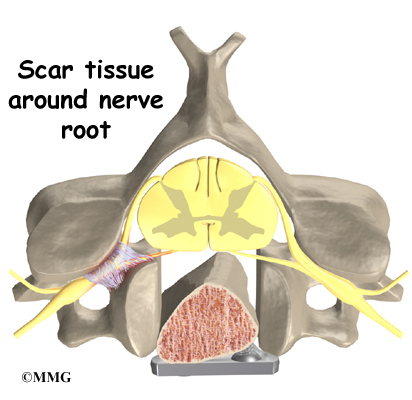
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Spontaneous Ankylosis (fusion)
Some things can go wrong with any implant. In the case of artificial disc replacements for the cervical spine, sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of neck motion is the main side effect of this problem.
Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may not affect the implant or your final results in terms of motion or function.
Some patients are left with pain, numbness, and weakness. This can occur when there’s been incomplete neurologic decompression. In other words, there is still pressure on the spinal cord or spinal nerves.
Subsidence (sinking)
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Implant Failure (need for further surgery)
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal artificial disc replacements. In rare cases, the artificial disc replacement can dislocate.
After Surgery
What happens after surgery
Most people spend one or two days in the hospital. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty. Patients generally recover quickly after the artificial disc procedure.
You should be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your neck (bending backward). You may need to wear a brace or soft collar for a short while after the operation to support your neck muscles.
As you recover in the hospital, a physical therapist may see you one or two times each day until you go home. You’ll be shown ways to move, dress, and do activities without putting extra strain on your neck. Your therapist will help you begin a walking program in the hospital. You are encouraged to continue the walking program when you return home.
When you leave the hospital, there are very few activity restrictions. You should be safe to sit, walk, and drive. However, you should avoid lifting items for at least four weeks. Your surgeon will probably release you to return to work in two to four weeks. If your job requires moving and lifting heavy items, you may require a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery.
If you spend large amounts of time in front of a computer or other machine, you may need to change the height and angle of your work surface and/or the computer. Finding a position that puts minimal stress on your neck is important. You should avoid spending hours in one position reading, sewing, or doing other handwork. The therapist can help you find optimal positions and advise you about ways to stretch your neck muscles.
Rehabilitation
What should my recovery be like?
Your surgeon may prescribe outpatient physical therapy within one to two weeks after surgery. Plan on attending therapy two to three times each week for four to six weeks.
The first few visits include treatments to calm soreness and pain from the operation. Your therapist may apply gentle soft-tissue treatments such as massage. Ice and electrical stimulation are also commonly used to calm muscle spasm and to help take away any lasting pain.
Your therapist will teach you how to protect your neck. You’ll learn ways to position your neck when you sleep, sit, and drive. And you’ll be shown ways to keep your neck safe during routine activities, such as getting in or out of bed, getting dressed, and washing your hair.
Many patients are afraid to move the head and neck for fear of damaging or dislodging the disc. Using normal motion for everyday activities will not harm your new disc in any way. Your therapist will help you learn how to move your neck and show you any limits necessary.
Active treatments are used to improve flexibility, strength, and endurance. Gentle stretching exercises for the neck are commonly prescribed. You’ll begin a series of strengthening exercises to help tone and control the muscles that stabilize the neck and upper back. It is also important to build strength in your arms. Endurance exercises may include treadmill walking, swimming, or stationary biking.
When your symptoms are under control and you’re comfortable doing your exercises, your formal therapy sessions will end. You’ll continue your exercises as part of a home program.
Summary
Artificial disc replacement offers an alternative to cervical fusion for some patients who have chronic neck pain from degenerative disc disease. While fusion stops pain by eliminating movement in the problem spinal segment, ADR allows natural motion in the part of the spine where the disc is implanted. This is because the prosthesis is designed to imitate normal movement between adjacent vertebrae.
A successful result means that your painful symptoms are better but not necessarily perfect. You can expect to have significantly less neck pain and greatly improved function with the operation. You can expect to discontinue the use of strong medications.
But remember, no one can guarantee that you’ll be free of pain or that your spine will be totally flexible after this type of surgery. The idea that preserving motion will decrease adjacent segment degeneration hasn’t been proven yet. Long-term results (10 or more years) are unavailable.
Posterior Cervical Fusion
A Patient’s Guide to Posterior Cervical Fusion
Introduction
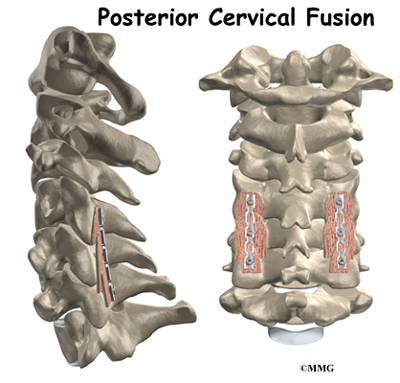
Posterior cervical fusion is done through the back (posterior) of the neck. The surgery joins two or more neck vertebrae into one solid section of bone. The medical term for fusion is arthrodesis. Posterior cervical fusion is most commonly used to treat neck fractures and dislocations and to fix deformities in the curve of the neck.
Surgeons sometimes attach metal hardware to the neck bones during posterior fusion surgery. This hardware is called instrumentation.
This guide will help you understand
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
Anatomy
What parts of the neck are involved?
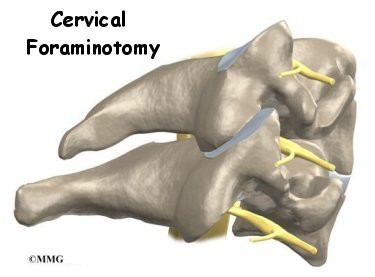
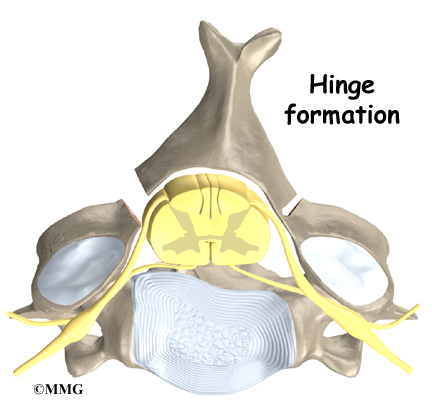
Surgeons do this surgery through the back part of the neck. The muscles on the back of the neck cover the bony ring around the spinal cord. The bony ring, formed by the pedicle and lamina bones, is called the spinal canal. The spinal canal is a hollow tube that surrounds the spinal cord as it passes through the spine.
The lamina acts like a protective roof over the back of the spinal cord. Facet joints line up on both sides along the back of the spinal column.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
Posterior cervical fusion is used to stop movement between the bones of the neck. A serious fracture or dislocation of the neck vertebrae poses a risk to the spinal cord. The spinal cord is sometimes damaged by the fractured or dislocated bones. Surgeons hope to protect the spinal cord from additional injury by fusing these bones together.
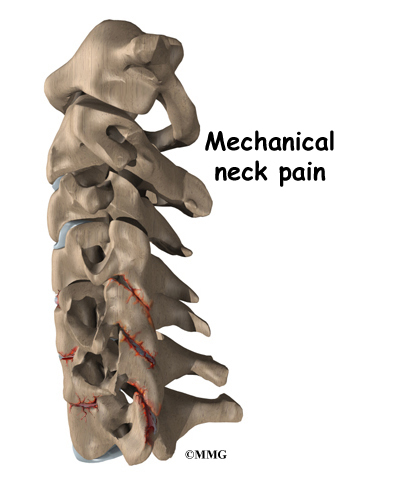
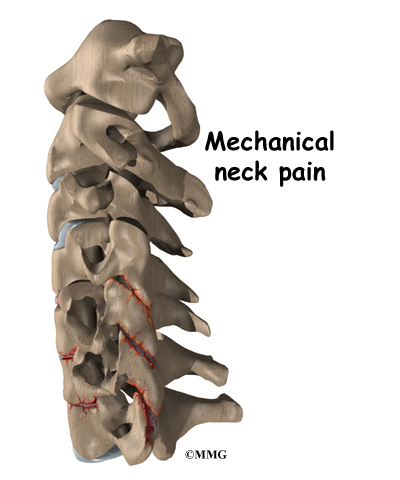
Surgeons also use posterior cervical fusion to help patients who have mechanical neck pain. Extra movement within the parts of the cervical spine can be a source of this type of neck pain. Fusing these bones together prevents the extra movement, easing pain.
Posterior fusion is also used to line up and hold the neck bones when there’s a deformity in the curve of the neck. Normally, the neck lines up with a slight inward curve from the base of the skull to the top of the thorax (the chest area). One type of deformity that changes the curve of the neck is called kyphosis.
This happens when the inward curve starts to bow outward. Some people are born with an outward bow in their neck. Kyphosis can also occur when a severe injury compresses the vertebral body into the shape of a wedge. Neck surgeries that weaken the bony ring around the spinal canal can also lead to kyphosis. When kyphosis is a problem, a posterior fusion procedure may be used to correct the curve and to fuse the bones together once they’re in the right position.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
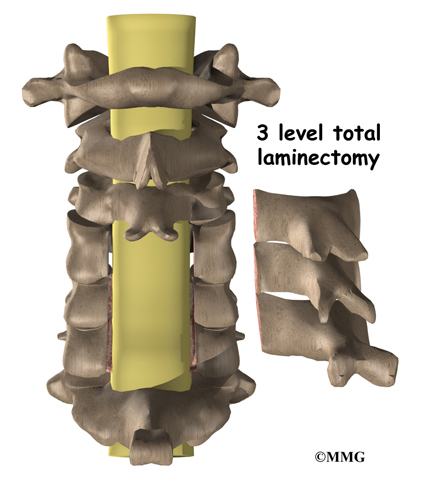
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
This surgery is usually done with the patient lying face down on the operating table. The surgeon makes an incision down the middle of the back of the neck. Retractors are used to gently separate and hold the neck muscles and soft tissues apart so the surgeon can work on the back of the spine.
A layer of bone is shaved off the surface of the outer ring (the lamina) of each vertebra to be fused. This causes the surface to bleed and to stimulate the bone to heal. (This is similar to the way the two sides of a fractured bone begin to heal.) Small strips of bone are grafted from the top part of the pelvis and laid over the back of the spinal column. This bone graft also helps stimulate the bones to heal together, or fuse.
The muscles and soft tissues are put back in place, and the skin is stitched together. Most patients are placed in a rigid neck collar to lock the bones firmly in place.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following posterior cervical fusion include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- problems with the graft
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Problems with the Graft
Fusion surgery requires bone to be grafted into the spinal column. The graft is commonly taken from the top rim of the pelvis. There is a risk of having pain, infection, or weakness in the area where the graft is taken.
After the graft is placed, the surgeon checks the position of the graft before completing the surgery. However, the graft may shift slightly soon after surgery to the point where it is no longer able to hold the spine stable. When the graft migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align the graft and to apply metal plates and screws to hold it firmly in place.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion or pseudarthrosis. (The term pseudarthrosis means false joint.) If the joint motion from a nonunion continues to cause pain, you may need a second operation. In the second procedure, the surgeon usually adds more bone graft. Metal plates and screws may also need to be added to rigidly secure the bones so they will fuse together.
Ongoing Pain
Posterior cervical fusion is an involved surgery. Not all patients get complete pain relief with this procedure. As with any surgery, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Most patients are placed in a rigid neck brace after surgery for several months. These restrictive measures may not be needed if the surgeon attached metal hardware to the spine during the surgery.
Patients usually stay in the hospital after surgery for up to one week. But they can start to get up as soon as they feel up to it. Patients are watched carefully when they begin eating. They usually drink liquids at first. If they are not having problems, they can go on to solid food.
A physical therapist will schedule daily sessions to help patients learn safe ways to move, dress, and do activities without putting extra strain on the neck.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal. Outpatient physical therapy is usually started four to six weeks after the date of surgery.
Rehabilitation
What should I expect as I recover?
Rehabilitation after posterior cervical fusion can be a slow process. If the spinal cord was injured from a neck fracture or dislocation, patients may need intensive and ongoing rehabilitation for the neurological condition. When the spinal cord has not been damaged, patients may need to attend therapy sessions for two to three months and should expect full recovery to take up to eight months.
Many surgeons prescribe outpatient physical therapy beginning a minimum of four weeks after surgery. At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are slowly added. These include exercises for improving heart and lung function. Walking and stationary cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist also works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. At first, this may be as simple as helping you learn how to move safely and easily in and out of bed, how to get dressed and undressed, and how to do some of your routine activities. Then you’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Therapists often help as a resource to suggest changes in job tasks that may enable you to go back to your previous job or to do alternate forms of work. You’ll learn new ways to do these tasks in ways that keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Anterior Cervical Discectomy and Fusion
A Patient’s Guide to Anterior Cervical Discectomy and Fusion
Introduction
Anterior cervical discectomy and fusion (ACDF) is a procedure used to treat neck problems such as cervical radiculopathy, disc herniations, fractures, and spinal instability. In this procedure, the surgeon enters the neck from the front (the anterior region) and removes a spinal disc (discectomy). The vertebrae above and below the disc are then held in place with bone graft and sometimes metal hardware. The goal is to help the bones to grow together into one solid bone. This is known as fusion. The medical term for fusion is arthrodesis.
Operating on the back of the neck is more commonly used for neck fractures. That procedure is called a posterior cervical fusion.
Related Document: A Patient’s Guide to Posterior Cervical Fusion
This guide will help you understand
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
Anatomy
What parts of the neck are involved?
Surgeons perform this surgery through the front part of the neck. Key structures include the ligaments and bones, intervertebral discs, the spinal cord and spinal nerves, and the neural foramina.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
In most cases, ACDF is used to stop symptoms from cervical disc disease. Discs start to degenerate as a natural part of aging and also from stress and strain in the structures of the neck. Over time, the disc begins to collapse, and the space decreases between the vertebrae.
When this happens, the openings (the neural foramina) around the spinal nerves narrow and may begin to put pressure on the nerves. The long ligaments in the spine slacken. They may even buckle and put pressure on the spinal cord. The outer rings of the disc, the annulus, weaken and develop small cracks. The nucleus in the center of the disc may press on the weakened annulus and actually squeeze out of the annulus. This is called a herniated disc. The herniated disc may press on ligaments, nerves, or even the spinal cord. Fragments of the disc that press against the outer annulus, spinal nerves, or spinal cord can be a source of pain, numbness, and weakness. Pressure on the spinal cord, called myelopathy, can also produce problems with the bowels and bladder, changes in the way you walk, and trouble with fine motor skills in the hands.
Discectomy is the removal of the disc (and any fragments) between the vertebrae that are to be fused. When symptoms are coming from the disc, it is hoped that this stops the symptoms.
Related Document: A Patient’s Guide to Cervical Discectomy
View animation of enlarging the space
Once the disc is removed, surgeons spread the bones of the spine apart slightly (distraction) to make room for the bone graft. This is bone material that can be taken from the top of the pelvis bone (autograft) or from a natural substitute (allograft). The bone graft separates and holds the vertebrae apart. Enlarging the space between the vertebrae widens the opening of the neural foramina, taking pressure off the spinal nerves that pass through them. Also, the ligaments inside the spinal canal are pulled taut so they don’t buckle into the spinal canal.
No movement occurs between the bones that are fused together. By holding the sore part of the neck steady, the fusion helps relieve pain. And it prevents additional wear and tear on the structures inside the section that was fused. This keeps bone spurs from forming, and it has been shown that fusion causes existing bone spurs to shrink. By fusing the bones together, surgeons hope that patients won’t have future pain and problems from cervical disc disease.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
The patient’s neck is positioned facing the ceiling with the head bent back and slightly to the right. A two-inch incision is made two to three fingers’ width above the collar bone across the left-hand side of the neck. Surgeons often choose the left side to avoid injuring the nerve going to the voice box. Retractors are used to gently separate and hold the neck muscles and soft tissues apart so the surgeon can work on the front of the spine.
A needle is inserted into the disc, and an X-ray is taken to identify the correct disc. A long strip of muscle and part of the long ligament that covers the front of the vertebral bodies are carefully pulled to the side. Forceps are used to take out the front half of the disc. Next, a tool is attached to the vertebrae to spread them apart. This makes it easier for the surgeon to see between the two vertebrae. A small rotary cutting tool (a burr) is used to carefully remove the back half of the disc. A special microscope is used to help the surgeon see and remove pieces of disc material and bone spurs near the spinal cord.
A layer of bone is shaved off the flat surfaces of the two vertebrae. This causes the surfaces to bleed. This is necessary to help the bone graft heal and join the bones together.
The surgeon measures the depth and height between the two vertebrae. A section of bone is grafted from the top part of the pelvis. It is measured to fit snugly in the space where the disc was taken out. The surgeon increases the traction pull to separate the two vertebrae, and the graft is tamped into place.
The traction pull is released. Then the surgeon tests the graft by bending and turning the neck to make sure it is in the right spot and is locked in place. Another X-ray may be taken to double check the location of the graft.
A drainage tube may be placed in the wound. The muscles and soft tissues are put back in place, and the skin is stitched together. The surgeon may place your neck in a rigid collar.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following ACDF include
- anesthesia
- thrombophlebitis
- infection
- nerve damage
- problems with the graft
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. Surgeons usually prefer to do surgery on the left side of the neck where the path of the nerve is more predictable than on the right side. During surgery, the nerve may be stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases in which the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Problems with the Graft
Fusion surgery requires bone to be grafted into the spinal column. The graft is commonly taken from the top rim of the pelvis. There is a risk of having pain, infection, or weakness in the area where the graft is taken.
After the graft is placed, the surgeon checks the position of the graft before completing the surgery. However, the graft may shift slightly soon after surgery to the point it is no longer able to hold the spine stable. When the graft migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align the graft and to apply metal plates and screws to hold it firmly in place.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) If the joint motion from a nonunion continues to cause pain, you may need a second operation. In the second procedure, the surgeon usually adds more bone graft. Metal plates and screws may also be added to rigidly secure the bones so they will fuse together.
Ongoing Pain
ACDF is a complex surgery. Not all patients get complete pain relief with this procedure. As with any surgery, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
After ACDF, patients usually wear a special neck brace for several months. These neck braces are often bulky and restrictive. However, the bone graft needs time to heal in order for the fusion to succeed. This requires the neck to be held still.
Recently, surgeons have begun using metal hardware, called instrumentation to lock the bones in place. This hardware includes metal plates and screws that are fastened to the neck bones. They hold the neck bones still so the graft can heal, replacing the need for a rigid neck brace.
Patients may stay in the hospital for one to two days after surgery. When the surgery is done on an outpatient basis, patients may even go home the same day of surgery. Patients can get out of bed as soon as they feel up to it. They are watched carefully when they begin eating to make sure they don’t have problems swallowing. They usually drink liquids at first, and if they are not having problems, they can start eating solid food.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal.
Rehabilitation
What should I expect as I recover?
Rehabilitation after ACDF can be a slow process. You will probably need to attend therapy sessions for two to three months, and you should expect full recovery to take up to eight months.
Many surgeons prescribe outpatient physical therapy beginning a minimum of four weeks after surgery. At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are slowly added. These include exercises for improving heart and lung function. Walking and stationary cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist also works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. At first, this may be as simple as helping you learn how to move safely and easily in and out of bed, how to get dressed and undressed, and how to do some of your routine activities. Then you’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job or to do alternate forms of work. You’ll learn to do these tasks in ways that keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you ways to avoid future problems.
Cervical Spine Anatomy
A Patient’s Guide to Cervical Spine Anatomy
Introduction
Knowing the main parts of your neck and how these parts work is important as you learn to care for your neck problem.
Two common anatomic terms are useful as they relate to the neck. The term anterior refers to the front of the neck. The term posterior refers to the back of the neck. The part of the spine that moves through the neck is called the cervical spine. The front of the neck is therefore called the anterior cervical area. The back of the neck is called the posterior cervical area.
In addition to reading this article, be sure to watch our Cervical Spine Anatomy Animated Tutorial Video.
This guide gives a general overview of the anatomy of the neck. It should help you understand
- what parts make up the neck
- how these parts work
Important Structures
The important parts of the cervical spine include
- bones and joints
- nerves
- connective tissues
- muscles
- spinal segments
This section highlights important structures in each category.
Bones and Joints
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
The first seven vertebrae make up the cervical spine. Doctors often refer to these vertebrae as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine (the chest area).
The base of the skull sits on top of C1, also called the atlas. Two thickened bony arches form a large hole through the center of the atlas. The opening is large because the spinal cord is wider where it first exits the brain and skull. Compared to other vertebrae, the atlas also has much wider bony projections pointing out to each side.
The atlas sits on top of the C2 vertebra. The C2 is called the axis. The axis has a large bony knob on top, called the dens. The dens points up and fits through a hole in the atlas. The joints of the axis give the neck most of its ability to turn to the left and right.
Each vertebra is made of the same parts. The main section of each cervical vertebra, from C2 to C7, is formed by a round block of bone, called the vertebral body. A bony ring attaches to the back of the vertebral body. This ring has two parts. Two pedicle bones connect directly to the back of the vertebral body. Two lamina bones join the pedicles to complete the ring. The lamina bones form the outer rim of the bony ring. When the vertebrae are stacked on top of each other, the bony rings form a hollow tube that surrounds the spinal cord. The laminae provide a protective roof over the spinal cord.
A bony knob projects out at the point where the two lamina bones join together at the back of the spine. These projections, called spinous processes, can be felt as you rub your fingers up and down the back of your spine. The largest bump near the top of your spine is the spinous process of C2. At the base of the neck where the cervical and thoracic spines join together, you’ll feel another large spinous process. That’s C7.
Each vertebra in the spine has two bony knobs that point out to the side, one on the left and one on the right. These bony projections are called transverse processes. The atlas has the widest transverse processes of all the cervical vertebrae. Unlike the rest of the spine, the neck vertebrae have a hole that passes down through each transverse process. This hole, called the transverse foramen, provides a passageway for arteries that run up each side of the neck to supply the back of the brain with blood.
Between each pair of vertebrae are two joints called facet joints. These joints connect the vertebrae together in a chain but slide against one another to allow the neck to move in many directions. Except for the very top and bottom of the spinal column, each vertebra has two facet joints on each side. The ones on top connect to the vertebra above; the ones below join with the vertebra below.
The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the ends of bones to move against each other smoothly, without friction.
On the left and right side of each vertebra is a small tunnel called a neural foramen. (Foramina is the plural term.) The two nerves that leave the spine at each vertebra go through the foramina, one on the left and one on the right. The intervertebral disc (described later) sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits in back of the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
Nerves
The hollow tube formed by the bony ring on the back of the spinal column surrounds the spinal cord as it passes through the spine. The spinal cord is a similar to a long wire made up of millions of nerve fibers. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
The spinal cord travels down from the brain through the spinal column. Two large nerves branch off the spinal cord from each vertebra, one on the left and one on the right. The nerves pass through the neural foramina. These spinal nerves group together to form the main nerves that go to the limbs and organs. The nerves that come out of the cervical spine go to the arms and hands.
Connective Tissues
Ligaments are strong connective tissues that attach bones to other bones. (Connective tissues are networks of fiber that hold the cells of the body together.) Several long ligaments connect on the front and back sections of the vertebrae. The anterior longitudinal ligament runs lengthwise down the front of the vertebral bodies. Two other ligaments run full length within the spinal canal. The posterior longitudinal ligament attaches on the back of the vertebral bodies. The ligamentum flavum is a long elastic band that connects to the front surface of the lamina bones.
A special type of structure in the spine called an intervertebral disc is also made of connective tissue. The fibers of the disc are formed by special cells, called collagen cells. The fibers may be lined up like strands of nylon rope or crisscrossed like a net.
An intervertebral disc is made of two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption in the spine. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
Muscles
The anterior cervical area is covered with muscles that run from the rib cage and collar bone to the cervical vertebrae, jaw, and skull. The posterior cervical muscles cover the bones along the back of the spine and make up the bulk of the tissues on the back of the neck.
Spinal Segment
A good way to understand the anatomy of the cervical spine is by looking at a spinal segment. Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at each vertebra, and the small facet joints that link each level of the spinal column.
The intervertebral disc separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during heavy activities that put strong force on the spine, such as jumping, running, and lifting.
The spinal segment is connected by a facet joint, described earlier. When the facet joints of the cervical spine move together, they bend and turn the neck.
Summary
Many important parts make up the anatomy of the neck. Understanding the regions and structures of the neck can help you be more involved in your health care and better able to care for your neck problem.
Cervical Foraminotomy
A Patient’s Guide to Cervical Foraminotomy
Introduction
Foraminotomy is a surgical procedure for widening the area where the spinal nerve roots exit the spinal column. A foramen is the opening around the nerve root, and otomy refers to the medical procedure for enlarging the opening. In this procedure, surgeons widen the passageway to relieve pressure where the spinal nerve is being squeezed in the foramen.
This guide will help you understand
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect as you recover
Anatomy
What parts of the neck are affected?
The spine is made of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. The spinal canal is a hollow tube formed by the bony rings of all the vertebrae. The spinal canal surrounds and protects the spinal cord within the spine. There are seven vertebrae in the neck that form the area known as the cervical spine. The vertebrae are separated by intervertebral discs.
Traveling from the brain down through the spinal column, the spinal cord sends out nerve branches through openings on both sides of each vertebra. These openings are called the neural foramina. (The term used to describe a single opening is foramen.)
The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits in back of the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
Rationale
What do surgeons hope to achieve?
Foraminotomy alleviates the symptoms of foraminal stenosis. In foraminal stenosis, a nerve root is compressed inside the neural foramen. This compression is usually the result of degenerative (or wear and tear) changes in the spine.
View animation of disc collapse
Wear and tear from repeated stresses and strains on the neck can cause a spinal disc to begin to collapse. As the space between the vertebral bodies shrinks, the opening around the nerve root narrows. This squeezes the nerve. The nerve root is further squeezed in the foramen when the facet joint lining the outer edge of the foramen becomes inflamed and enlarged as a result of the same degenerative changes.
The degenerative process can also cause bone spurs to develop and point into the foramen, causing further irritation. In a foraminotomy, the surgeon removes the tissues around the edges of the foramen, essentially widening the opening in order to take pressure off the nerve root.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. For shorter procedures such as foraminotomy, patients are usually given a gas form of anesthesia through a mask. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
This surgery is usually done with the patient lying face down on the operating table. The surgeon makes an incision down the middle of the back of the neck. The skin and soft tissues are separated on the side where the spinal nerves are compressed. Some surgeons use a surgical microscope during the procedure to magnify the area they’ll be working on.
The surgeon may use a small, rotary cutting tool (a burr) to shave the inside edge of the facet joint. This opens up the outer rim of the neural foramen. The burr is sometimes used to shave a small section of the bony ring on the back of the vertebra above and below the affected nerve root.
Small cutting instruments are used to carefully remove soft tissues within the neural foramen. The surgeon takes out any small disc fragments that are present and scrapes off nearby bone spurs. In this way, tension and pressure are taken off the nerve root.
The muscles and soft tissues are put back in place, and the skin is stitched together. Patients are sometimes placed in a soft collar after surgery to keep the neck positioned comfortably.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following foraminotomy include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal
can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Ongoing Pain
Many patients get nearly complete pain relief from the foraminotomy procedure. As with any surgery, however, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are usually able to get out of bed within an hour or two after surgery. Your surgeon may have you wear a soft neck collar. If not, you will be instructed to move your neck only carefully and comfortably.
Most patients leave the hospital the day after surgery and are safe to drive within a week or two. People generally get back to light work by four weeks and can do heavier work and sports within two to three months.
Outpatient physical therapy is usually prescribed when patients have extra pain or show significant muscle weakness and deconditioning.
Rehabilitation
What should I expect during my recovery?
Rehabilitation after foraminotomy surgery is generally needed for only a short period of time. If you require outpatient physical therapy, you will probably need to attend therapy sessions for two to four weeks. You should expect full recovery to take up to two or three months.
Many surgeons prescribe outpatient physical therapy within four weeks after surgery. At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are added slowly. These include exercises for improving heart and lung function. Walking, stationary cycling, and arm cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. At first, this may be as simple as helping you learn how to move safely and easily in and out of bed, how to get dressed and undressed, and how to do some of your routine activities. Then you’ll learn how to keep your neck safe while you lift and carry items and as you begin to do heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Therapists may suggest changes in job tasks that enable you to go back to your previous job. They may also provide ideas for alternate forms of work. You’ll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Cervical Discectomy
A Patient’s Guide to Cervical Discectomy
Introduction
Cervical discectomy is surgery to remove one or more discs from the neck. The disc is the pad that separates the neck vertebrae; ectomy means to take out. Usually a discectomy is combined with a fusion of the two vertebrae that are separated by the disc. In some cases, this procedure is done without a fusion. A cervical discectomy without a fusion may be suggested for younger patients between 20 and 45 years old who have symptoms due to a herniated disc.
This guide will help you understand
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
Anatomy
What parts of the neck are involved?
Surgeons usually perform this procedure through the front of the neck. This is called the anterior neck region. Key structures include ligaments, bones, intervertebral discs, spinal cord, spinal nerves and the neural foramina.
Surgery is occasionally done through the back, or posterior region, of the neck. Important structures in this area include the ligaments and bones, especially the lamina bones.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
Discectomy is used to alleviate symptoms of a herniated disc. A disc herniation happens when the nucleus inside the center of the disc pushes through the annulus, the ligaments surrounding the nucleus. The herniated disc material may push outward, causing pain. Numbness or weakness in the arm occurs when the nucleus pushes on the spinal nerve root. Of greater concern is a condition in which the nucleus herniates straight backward into the spinal cord, called a central herniation. Discectomy relieves pressure on the ligaments, nerves, or spinal cord.
Discectomy is also commonly used when the surgeon plans to fuse the bones of two neck vertebrae into one solid bone. Most surgeons will take the disc out and replace the empty space with a block of bone graft, a procedure called cervical fusion.
Discectomy alone is usually only used for younger patients (20 to 45 years old) whose symptoms are from herniation of the disc. But some surgeons think discectomy should always be combined with fusion of the bones above and below. They are concerned that the empty space where the disc was removed may eventually collapse and fill in with bone. Inserting a bone block during fusion surgery helps keep pressure off the spinal nerves because the graft widens the neural foramina. The neural foramina are openings on each side of the vertebrae where nerves exit the spinal canal. Most research on discectomy by itself shows good short-term benefits compared to discectomy with fusion. But more information is needed about whether the long-term results are equally as good.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Cervical discectomy is commonly done through the anterior (front) of the neck. This is called an anterior cervical discectomy. However, when many pieces of the herniated disc have squeezed into the posterior (back) of the spine, surgeons may need to operate through the back of the neck using a procedure called a posterior cervical discectomy.
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
Anterior Discectomy
The patient’s neck is positioned facing the ceiling with the head bent back and turned slightly to the right. A two-inch incision is made two to three fingers’ width above the collar bone across the left-hand side of the neck. The left side is chosen to avoid injuring the nerve going to the voice box. Retractors are used to gently separate and hold the neck muscles and soft tissues apart so the surgeon can work on the front of the spine.
A needle is inserted into the herniated disc, and an X-ray is taken to identify and confirm it is the correct disc. A long strip of muscle and the anterior longitudinal ligament that cover the front of the vertebral bodies are carefully pulled to the side. Forceps are used to take out the front half of the disc. Next a small rotary cutting tool (a burr) is used to carefully remove the back half of the disc. A surgical microscope is used to help the surgeon see and remove pieces of disc material and any bone spurs that are near the spinal cord.
The muscles and soft tissues are put back in place, and the skin is stitched together.
Posterior Discectomy
This method is used when the herniated disc has fragmented into small pieces near the spinal nerve.
The operation is usually done with the patient lying face down with the neck bent forward and held in a headrest. The surgeon makes a short incision down the center of the back of the neck. The skin and soft tissues are separated to expose the bones along the back of the spine.
Then the surgeon may use an X-ray to identify the injured disc. A burr is used to shave the edge off the lamina bones, the back part of the ring over the spinal cord. When the disc has jutted straight backward into the spinal cord (central herniation), surgeons may need to completely remove both lamina bones in order to see better and to be able to clear all the pieces of the disc near the spinal cord.
Related Document: A Patient’s Guide to Cervical Laminectomy
After shaving the lamina bone, the surgeon cuts a small opening in the ligamentum flavum, a ligament within the spinal canal and in front of the lamina bone. By removing part of this ligament, the surgeon exposes the spot where the disc fragments are pressed against the spinal nerve. Next, the spinal nerve is gently moved upward. Using a surgical microscope, the surgeon magnifies the area in order to carefully remove the disc fragments and any bone spurs.
The muscles and soft tissues are put back in place, and the skin is stitched together.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following discectomy include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Ongoing Pain
Many patients get nearly complete relief of symptoms from the discectomy procedure. As with any surgery, however, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are usually able to get out of bed within an hour or two after surgery. Your surgeon may have you wear a hard or soft neck collar. If not, you will be instructed to move your neck only carefully and comfortably.
Most patients leave the hospital the day after surgery and are safe to drive within a week or two. People generally get back to light work by four weeks and can do heavier work and sports within two to three months.
Outpatient physical therapy is usually prescribed only for patients who have extra pain or show significant muscle weakness and deconditioning.
Rehabilitation
What should I expect as I recover?
Patients usually don’t require formal rehabilitation after routine cervical discectomy surgery. Surgeons may prescribe a short period of physical therapy when patients have lost muscle tone in the shoulder or arm, when they have problems controlling pain, or when they need guidance about returning to heavier types of work.
If you require outpatient physical therapy, you will probably only need to attend therapy sessions for two to four weeks. You should expect full recovery to take up to three months.
At first, therapy treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are added slowly. These include exercises for improving heart and lung function. Walking, stationary cycling, and arm cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. You’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job. Your therapist can also provide ideas for alternate forms of work. You’ll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Cervical Corpectomy and Strut Graft
A Patient’s Guide to Cervical Corpectomy and Strut Graft
Introduction
A corpectomy is surgery to relieve pressure on the spinal cord due to spinal stenosis. In spinal stenosis, bone spurs press against the spinal cord, leading to a condition called myelopathy. This can produce problems with the bowels and bladder and disrupt the way you walk. Fine motor skills of the hand may also be impaired. In a corpectomy, the front part of the spinal column is removed. (Corpus means body, and ectomy means remove.) Bone grafts are used to fill in the space. This procedure is used when bone spurs have developed in more than one vertebra.
This guide will help you understand
- what part of the spinal column is affected
- why the procedure becomes necessary
- what happens before and during the operation
- what to expect as you recover
Anatomy
What parts of the neck are involved?
Surgeons perform this procedure through the front of the neck. This is known as the anterior neck region. Key structures include ligaments, bones, intervertebral discs, the spinal cord and spinal nerves.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
Spinal stenosis occurs when bone spurs project into the spinal column and press against the spinal cord. Removing the vertebral bodies along the front section of the spinal column gives surgeons a way to relieve pressure on the front surface of the spinal cord, reducing or eliminating the symptoms caused by the bone spurs.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
The surgeon starts by making an incision up the left side of the neck to the ear and then under the jaw to the bottom of the chin. The skin flap is opened to expose the structures of the neck. Retractors are used to separate and hold the muscles and soft tissues apart so the surgeon can work on the front of the spine.
Special instruments are attached either to the skull or the spinal bones to stretch the neck with mild traction. The traction pull spreads the neck joints apart to give the surgeon more room to work. It also takes additional pressure off the spinal cord. Then the surgeon inserts a needle into the disc and does an X-ray to locate the exact sections where the bones are to be removed.
The surgeon carefully cuts part of the anterior longitudinal ligament away from the front section of the spinal column. Instruments are then used to take out the front half of the discs that lie between the vertebral bodies. Next, a small rotary cutting tool (a burr) is used to carefully remove the back half of the discs (called discectomy) and a row of vertebral bodies (called corpectomy). The ring of bone that surrounds and protects the spinal column isn’t touched.
When the discs and vertebral bodies are out of the way, the posterior longitudinal ligament can be seen where it covers the front of the spinal cord. This thin ligament is shaved to remove areas that have hardened or buckled, as these areas are known to add pressure to the spinal cord.
The surgeon then prepares a bone graft that will fill in the space where the discs and vertebral bodies have been removed. A section of bone is taken from the fibula, the thin bone that runs along the outside of the lower leg. (The main bone of the lower leg is called the tibia.) Some surgeons prefer to take bone from the pelvis instead of the fibula.
Before inserting the bone graft, the surgeon increases the traction pull on the neck to help separate the space even more. The bone graft is sized to fill the full length of the removed section of bone and discs from one end to the other.
The section of bone is grafted into the space where the vertebral bones have been taken out. The graft acts like a supportive column, or strut, to support the elongated space and to prevent the neck from buckling forward. Your surgeon may attach a metal plate along the front of the spine to help lock the new graft in place.
Another X-ray is taken to check the position of the graft. Then the muscles and soft tissues are put back in place, and the skin is stitched together. Patients are often placed in a rigid neck brace for at least three months to hold the neck still while the bones grow together, or fuse.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following corpectomy surgery include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- problems with the graft or hardware
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up very early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine. Your surgeon may give you antibiotics before spine surgery when the procedure requires bone grafts or hardware (plates, rods, or screws).
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. Surgeons usually prefer to do surgery on the left side of the neck where the path of the nerve is more predictable than on the right side. During surgery, the nerve may be stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases in which the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Problems with the Graft or Hardware
Corpectomy surgery requires bone to be grafted into the spinal column. The graft is taken from either the top rim of the pelvis or, more commonly, from the fibula bone along the outside of the lower leg. There is a risk of having pain, infection, or weakness in the area where the graft is taken.
After the graft is placed, the surgeon checks the position of the graft before completing the surgery. However, the graft may shift slightly soon after surgery to the point it is no longer able to hold the spine stable. When the graft migrates out of position, it may cause injury to the nearby tissues. When the graft shifts out of place, a second surgery may be needed to align the graft and apply more hardware to hold it firmly in place.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. The surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) If the joint motion from a nonunion continues to cause pain, you may need a second operation.
In the second procedure, the surgeon usually adds more bone graft. If hardware was used in the first surgery, the surgeon will check to make sure it is attached firmly. Hardware may also be added to secure the bones so they will fuse together.
Ongoing Pain
Corpectomy is a complex surgery. Not all patients feel complete pain relief with this procedure. The main goal of this surgery is to get pressure off the spinal cord and to try and prevent further problems. As with any surgery, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Most patients are placed in a rigid neck brace or a halo vest, for a minimum of three months after surgery. These restrictive measures may not be needed if the surgeon attached metal hardware to the spine during the surgery.
Patients usually stay in the hospital after surgery for up to one week. During this time, a physical therapist will schedule daily sessions to help patients learn safe ways to move, dress, and do activities without putting extra strain on the neck.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal. Outpatient physical therapy is usually started five weeks after the date of surgery.
Rehabilitation
What should I expect during my recovery?
Rehabilitation after corpectomy surgery can be a slow process. You will probably need to attend therapy sessions for two to three months, and you should expect full recovery to take up to one year.
Many surgeons prescribe outpatient physical therapy beginning a minimum of five weeks after surgery. At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are slowly added. These include exercises for improving heart and lung function. Walking, stationary cycling, and arm cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist also works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. At first, this may be as simple as helping you learn how to move safely and easily in and out of bed, how to get dressed and undressed, and how to do some of your routine activities. Then you’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will tailor your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job. You’ll learn new ways to do these tasks to keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Cervical Laminectomy
A Patient’s Guide to Cervical Laminectomy
Introduction
A laminectomy is a surgical procedure to relieve pressure on the spinal cord due to spinal stenosis. In spinal stenosis, bone spurs press against the spinal cord, leading to a condition called myelopathy. Myelopathy can produce problems with the bowels and bladder, disruptions in the way you walk, and impairments with fine motor skills in the hands. In a laminectomy, a small section of bone covering the back of the spinal cord is removed. Lamina refers to the roof of bone over the back of the spinal cord, and ectomy means the medical procedure for removing a section of the bony roof to take pressure off the spinal cord.
This guide will help you understand
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
Anatomy
What parts of the neck are involved?
Surgeons perform this procedure through the back of the neck. This is known as the posterior neck region. It includes the parts that make up the bony ring around the spinal cord (the pedicles and laminae.)
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
View animation of disc collapse
A laminectomy can alleviate the symptoms of spinal stenosis, a condition that causes the spinal cord to become compressed inside the spinal canal. Wear and tear on the spine from aging and from repeated stresses and strains can cause a spinal disc to begin to collapse. This is the first stage of spinal stenosis. As the space between the vertebrae narrows, the posterior longitudinal ligament that attaches behind the vertebral body may buckle and push against the spinal cord. The degenerative process can also cause bone spurs to develop. When these spurs point into the spinal canal, they squeeze the spinal cord. In a laminectomy, the surgeon removes a section of the lamina bone, the buckled parts of the posterior longitudinal ligament, and the bone spurs, taking pressure off the spinal cord.
Preparation
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
This surgery is usually done with the patient lying face down on the operating table. The surgeon makes an incision down the middle of the back of the neck. The skin and soft tissues are separated to expose the bones along the back of the spine. Some surgeons use a surgical microscope during the procedure to magnify the area they’ll be working on.
Surgeons have found that complete removal of the laminae loosens the facet joints that connect the back of the spine. This can cause the spine to tilt forward. To avoid this, a hinge can be formed by only cutting partially through the lamina on one side. A second cut is made all the way through the other lamina. This edge is then lifted away from the spinal cord, and the other edge acts like a hinge. The hinged side forms a bone union, which holds the opposite side open and keeps pressure off the spinal cord.
Small cutting instruments may be used to carefully remove soft tissues near the spinal cord. Then the surgeon takes out any small disc fragments and scrapes off nearby bone spurs. In this way, additional tension and pressure are taken off the spinal cord.
The muscles and soft tissues are put back in place, and the skin is stitched together. Patients are usually placed in a neck brace after surgery to keep the neck positioned comfortably.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following laminectomy include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- segmental instability
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Segmental Instability
Laminectomy surgery can cause the spinal segment to loosen, making it unstable. The facet joints that connect the back of the spine normally give enough stability, even when the lamina is taken off. This is why surgeons prefer to leave the facet joints in place whenever possible. But these joints may have to be removed if they are enlarged with arthritis. During total laminectomy, the facet joints are removed. This procedure creates extra space around the nerves but often leads to segmental instability. Fusion surgery is generally needed to fix the loose segment.
Related Document: A Patient’s Guide to Posterior Cervical Fusion
Ongoing Pain
Many patients get nearly complete relief of symptoms from the laminectomy procedure. As with any surgery, however, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your doctor about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are usually able to get out of bed within an hour or two after surgery. Your surgeon may have you wear a soft neck collar. If not, you will be instructed to move your neck only carefully and comfortably.
Most patients leave the hospital the day after surgery and are safe to drive within a week or two. People generally get back to light work by four weeks and can do heavier work and sports within two to three months.
Outpatient physical therapy is usually prescribed when patients have extra pain or show significant muscle weakness and deconditioning.
Rehabilitation
What should I expect as I recover?
Rehabilitation after laminectomy surgery is generally only needed for a short period of time. If you require outpatient physical therapy, you will probably need to attend therapy sessions for two to four weeks. You should expect full recovery to take up to three months.
Many surgeons prescribe outpatient physical therapy within four weeks after surgery. At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are added slowly. These include exercises for improving heart and lung function. Walking, stationary cycling, and arm cycling are ideal cardiovascular exercises. Therapists also teach specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. At first, this may be as simple as helping you learn how to move safely and easily in and out of bed, how to get dressed and undressed, and how to do some of your routine activities. Then you’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job. Your therapist can also provide ideas for alternate forms of work. You’ll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Cervical Spinal Stenosis
A Patient’s Guide to Cervical Spinal Stenosis
Introduction
The spinal cord is a column of nerve tissue protected by a bony tube in the spinal column. Conditions that narrow the space in this tube put the spinal cord at risk of getting squeezed. This narrowing in the spinal column of the neck is called cervical spinal stenosis, or cervical stenosis. Pressure against the spinal cord as a result of spinal stenosis causes myelopathy, a condition that demands medical attention. Myelopathy can cause problems with the bowels and bladder, change the way you walk, and affect your ability to use your fingers and hands.
This guide will help you understand
- what parts make up the spine and neck
- what causes cervical spinal stenosis
- how the condition is diagnosed
- what treatment options are available
Anatomy
What parts make up the spine and neck?
The spine is made of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body, forming a canal.
This bony ring is formed by two sets of bones. One set, the pedicle bones, attaches to the back of each vertebral body.
On the other end, each pedicle bone connects with a lamina bone. The lamina bones form a protective roof over the back of the spinal cord. When the vertebra bones are stacked on top of each other, the bony rings forms a long bony tube that surrounds and protects the spinal cord as it passes through the spine.
An intervertebral disc fits between each vertebral body and provides a space between the spine bones. The disc works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
Why do I have this problem?
The bony spinal canal normally has more than enough room for the spinal cord. Typically, the canal is 17 to 18 millimeters around, slightly less than the size of a penny. Spinal stenosis occurs when the canal narrows to 13 millimeters or less. When the size drops to 10 millimeters, severe symptoms of myelopathy occur. Myelopathy is a term for any condition that affects the spinal cord. The symptoms of myelopathy result from pressure against the spinal cord and reduced blood supply in the spinal cord as a result of the pressure.
Spinal stenosis may develop for any number of reasons. Some of the more common causes of spinal stenosis include
- congenital stenosis
- degeneration
- spinal instability
- disc herniation
- constriction of the blood supply to the spinal cord
Congenital Stenosis
Some people are born with a spinal canal that is narrower than normal. This is called congenital stenosis. They may not feel problems early in life, but having a narrow canal to begin with places them at risk for stenosis. Even a minor neck injury can set them up to have pressure against the spinal cord. People born with a narrow spinal canal often have problems later in life, because the canal tends to become narrower due to the affects of aging. These degenerative changes often involve the formation of bone spurs (small bony projections) that point into the spinal canal and put pressure on the spinal cord.
Degeneration
Degeneration is the most common cause of spinal stenosis. Wear and tear on the spine from aging and from repeated stress and strain can cause many problems in the cervical spine. The intervertebral disc can begin to collapse, shrinking the space between vertebrae. Bone spurs may form that protrude into the spinal canal and reduce the space available to the spinal cord. The ligaments that hold the vertebrae together may become thicker and can also push into the spinal canal. All of these conditions narrow the spinal canal.
Spinal instability
Spinal instability can cause spinal stenosis. Spinal instability means there is extra movement among the bones of the spine. Instability in the cervical spine can happen if the supporting ligaments have been stretched or torn from a severe injury to the head or neck. People with diseases that loosen their connective tissues may also have spinal instability. For example, rheumatoid arthritis can cause the ligaments in the upper bones of the neck to loosen, allowing the topmost neck bones to shift and close off the spinal canal. Whatever the cause, extra movement in the bones of the spine can lead to spinal stenosis and myelopathy.
Disc herniation
Spinal stenosis can occur when a disc in the neck herniates. Normally, the shock-absorbing disc is able to handle the downward pressure of gravity and the strain from daily activities. However, if the pressure on the disc is too strong, such as from a blow to the head or neck, the nucleus inside the disc may rupture through the outer annulus and squeeze out of the disc. This is called a disc herniation. If an intervertebral disc herniates straight backward, it can press against the spinal cord and cause symptoms of spinal stenosis.
Constriction of the blood supply to the spinal cord
The changes that happen with degeneration and disc herniation can choke off the blood supply that goes to the spinal cord. The sections of the spinal cord that don’t get blood have less oxygen and don’t function normally, leading to symptoms of myelopathy.
Symptoms
What does cervical stenosis feel like?
Cervical stenosis usually develops slowly over a long period of time. This is partly because degeneration in later life is the main cause of spinal stenosis. Symptoms rarely appear all at once when degeneration is causing the problems. A severe injury or a herniated disc may cause symptoms to come on immediately.
The first sign to appear in some patients is a change in the way they walk. They don’t realize this problem is coming from their neck. But pressure on the spinal cord in the neck can affect the nerves and muscles in the legs, leading to changes in the way they walk. Eventually their walking pattern gets jerky and they lose muscle power in the legs. This is called spasticity.
Most patients also have problems in their hands. The main complaint is that their hands start to feel numb. Others feel clumsy when doing fine motor activities like writing or typing. The ability to grip and let go of items becomes difficult because the muscles along the inside edge of the palm and fingers weaken.
Shoulder weakness also develops in many patients. This happens most often when the spinal cord is compressed in the upper part of the neck. Most affected are the shoulder blade muscles and the deltoid muscle, which covers the top and outside of the shoulder. These muscles weaken and begin to show signs of wasting (atrophy) from not getting nerve input.
The area where the spinal cord is compressed in patients with stenosis is very close to the nerves that go to the arm and hand. The problem that compresses the spinal cord in the neck may also affect the nerves where they leave the spinal column. Nerve pressure can cause pain to radiate from the neck to the shoulder, upper back, or even down one or both arms. It can also cause numbness on the skin of the arm or hand and weakness in the muscles supplied by the nerve.
Pressure against the spinal cord also creates problems with the bowels and bladder. Mild spinal cord pressure makes you feel like you have to urinate more often. But it also makes it difficult to get urine to flow (urinary hesitancy). Moderate disturbances cause people to have a weak flow of urine, making them dribble urine. They also have to strain during bowel movements. In severe cases, people aren’t able to voluntarily control their bladder or bowels. This is called incontinence.
Diagnosis
How will my doctor identify the condition?
Diagnosis begins with a complete history and physical exam. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities. This will include questions about pain, feelings of numbness or weakness, changes in bowel or bladder function, and whether you’ve noticed any changes in the way you walk.
Then the doctor does a physical examination to see which neck movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are tested. Your doctor will also watch you walk to see if there are any subtle changes in your walking pattern.
X-rays are used to look for the cause of pressure against the spinal cord. The images can show if degeneration has caused the space between the vertebrae to collapse and may show if a bone spur is pressing against the spinal cord.
If more information is needed, your doctor may order a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the spinal cord and can show where it is being squeezed. This machine creates pictures that look like slices of the area your doctor is interested in. The test does not require any special dye or a needle.
A computed tomography (CT) scan may also be ordered. The CT scan is a detailed X-ray that lets doctors see slices of bone tissue. The image can show if bone spurs are protruding into the spinal column and taking up space around the spinal cord.
Your doctor may recommend electrical tests of the nerves that go to your arm and hand. An electromyography (EMG) test is used to check if the motor pathway in a nerve is working correctly. Doctors may also order a somatosensory evoked potential (SSEP) test to locate more precisely where the spinal cord is getting squeezed. The SSEP is used to measure whether a nerve is able to get and send sensory information such as pain, temperature, and touch. The function of a nerve may be recorded with an electrode placed over the skin or with a needle that is inserted into the nerve or sensory center of the brain.
Treatment
What can be done for the problem?
Nonsurgical Treatment
Spinal myelopathy is a serious condition. If your condition is causing significant problems or is rapidly getting worse, your doctor may not begin with nonsurgical treatments and instead recommend surgery immediately. If the symptoms are mild, nonsurgical treatment may be tried initially to see if the symptoms improve.
At first, doctors may suggest immobilizing the neck. Keeping the neck still for a short time can calm inflammation and pain. Patients are instructed to restrict their daily activities by avoiding heavy and repeated motions of the neck, arms, and upper body. Doctors may also prescribe a soft neck collar. The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. Patients wear the collar during waking hours for up to three months. Then they slowly begin to taper the amount of time they wear it each day.
If the condition is very mild, some doctors have their patients work with a physical therapist. At first, treatments are used to ease pain and inflammation. Electrical stimulation treatments can help calm muscle spasm and pain. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or the therapist can apply the traction pull by hand.
Some patients are given an epidural steroid injection (ESI). The injection is given in a part of the spinal canal called the epidural space. This is the area between the dura (the material that covers the spinal cord) and the spinal column. It is thought that injecting steroid medication into this space fights inflammation around the nerves and discs. This can reduce the swelling and give the spinal cord more room.
Surgery
When there are signs that pressure is building on the spinal cord, surgery may be required, sometimes right away. Surgeries used to treat spinal stenosis include
- laminectomy
- anterior cervical discectomy and fusion
- corpectomy and strut graft
Laminectomy
The lamina is the covering layer of the bony ring of the spinal canal. It forms a roof-like structure over the back of the spinal cord. When bone spurs or disc contents have pushed into the spinal canal, a laminectomy is done to take off the lamina bone in order to release pressure on the spinal cord.
Some surgeons completely remove the entire lamina bone, called a total laminectomy. Others prefer to keep the lamina in place by forming a hinge on one edge of the bone. This hinge is formed by cutting partially through the lamina on one side.
A second cut is made all the way through the lamina on the other side. This edge is then lifted away from the spinal cord, and the other edge acts like a hinge. The hinged side eventually forms a bone union, which holds the opposite side open and keeps pressure off the spinal cord.
Related Document: A Patient’s Guide to Laminectomy
Anterior Cervical Discectomy and Fusion
A fusion surgery joins two or more bones into one solid bone. Fusion of the neck bones is most often done through the front of the neck. The surgeon takes out the intervertebral disc (discectomy) between two vertebrae. A layer of bone is shaved off the flat surfaces of the two vertebrae to be fused. This causes the surfaces to bleed and stimulates the bone to heal. (This is similar to the way two sides of a fractured bone begin to heal.) A section of bone is grafted from the top part of the pelvis bone and inserted into the space where the disc was taken out. This separates the two vertebra bones, taking pressure off the spinal cord. As the bone graft heals in place, the vertebral bones fuse together into one solid bone.
Related Document: A Patient’s Guide to Anterior Cervical Discectomy and Fusion
Corpectomy and Strut Graft
A corpectomy relieves pressure over a large part of the spinal cord. In this procedure, the surgeon takes off the front part of the spinal column and removes several vertebral bodies. The spaces are then filled with bone graft material. Metal plates and screws are generally used to hold the spine in place while it heals. A corpectomy is used in cases of severe spinal stenosis.
Related Document: A Patient’s Guide to Cervical Corpectomy And Strut Graft
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Patients with mild symptoms of cervical myelopathy may try nonsurgical treatment for three to six months. After wearing a neck brace for up to three months, patients will slowly resume routine activities. They usually visit their doctor every four to six weeks to check their progress.
After Surgery
Some patients leave the hospital shortly after surgery, but some surgeries require patients to stay in the hospital for a few days. A physical therapist may see the patient for treatment in the hospital room after surgery. Therapy sessions are designed to help patients learn to move and begin doing routine activities without putting extra strain on the neck.
During recovery from surgery, a patient may be placed in a halo vest or rigid neck brace. These braces are used to restrict the motion in the neck to allow the fusion to heal. Patients generally need to be extremely cautious about overdoing activities in the first few weeks to months after surgery.
Most patients spend time rehabilitating at home. Bone fusion may take several months. When the surgeon is absolutely certain the bones have fused together, patients are able to discontinue using the neck brace or halo vest.
After being in a rigid neck brace for four to six months, patients are often weak and deconditioned. They sometimes need the help of a physical therapist to work on neck movement, strength, and general conditioning.
As therapy sessions come to an end, the therapist may help patients with decisions about getting back to work.
Ideally, patients are able to go back to their previous activities. However, some patients may need to modify their activities to avoid future problems.
Cervical Radiculopathy
A Patient’s Guide to Cervical Radiculopathy
Introduction
Neck pain has many causes. Mechanical neck pain comes from injury or inflammation in the soft tissues of the neck. This is much different and less concerning than symptoms that come from pressure on the nerve roots as they exit the spinal column. People sometimes refer to this problem as a pinched nerve. Health care providers call it cervical radiculopathy.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the neck is involved?
The spine is made of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body. When the vertebra bones are stacked on top of each other, the bony rings forms a long bony tube that surrounds and protects the spinal cord as it passes through the spine.
Traveling from the brain down through the spinal column, the spinal cord sends out nerve branches through openings on both sides of each vertebra. These openings are called the neural foramina. (The term used to describe a single opening is foramen.)
The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits in back of the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
An intervertebral disc fits between the vertebral bodies and provides a space between the spine bones. The disc normally works like a shock absorber. An intervertebral disc is made of two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
Why do I have this problem?
Cervical radiculopathy is caused by any condition that puts pressure on the nerves where they leave the spinal column. This is much different than mechanical neck pain. Mechanical neck pain is caused by injury or inflammation in the soft tissues of the neck, such as the discs, facet joints, ligaments, or muscles.
The main causes of cervical radiculopathy include degeneration, disc herniation, and spinal instability.
Degeneration
View animation of degenerative changes
As the spine ages, several changes occur in the bones and soft tissues. The disc loses its water content and begins to collapse, causing the space between the vertebrae to narrow. The added pressure may irritate and inflame the facet joints, causing them to become enlarged. When this happens, the enlarged joints can press against the nerves going to the arm as they try to squeeze through the neural foramina. Degeneration can also cause bone spurs to develop. Bone spurs may put pressure on nerves and produce symptoms of cervical radiculopathy.
Herniated Disc
Heavy, repetitive bending, twisting, and lifting can place extra pressure on the shock-absorbing nucleus of the disc. A blow to the head and neck can also cause extra pressure on the nucleus. If great enough, this increased pressure can injure the annulus (the tough, outer ring of the disc). If the annulus ruptures, or tears, the material in the nucleus can squeeze out of the disc. This is called a herniation.
Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand these pressures. However, as the annulus ages, it tends to crack and tear. It is repaired with scar tissue. Over time, the annulus becomes weakened, and the disc can more easily herniate through the damaged annulus. If the herniated disc material presses against a nerve root it can cause pain, numbness, and weakness in the area the nerve supplies.
Spinal Instability
Spinal instability means there is extra movement among the bones of the spine. Instability in the cervical spine (the neck) can develop if the supporting ligaments have been stretched or torn from a severe injury to the head or neck. People with diseases that loosen their connective tissue may also have spinal instability. Spinal instability also includes conditions in which a vertebral body slips over the one just below it. When the vertebral body slips too far forward, the condition is called spondylolisthesis. Whatever the cause, extra movement in the bones of the spine can irritate or put pressure on the nerves of the neck, causing symptoms of cervical radiculopathy.
Symptoms
What does the condition feel like?
The symptoms from cervical radiculopathy are from pressure on an irritated nerve. These symptoms are not the same as those that come from mechanical neck pain. Mechanical neck pain usually starts in the neck and may spread to include the upper back or shoulder. It rarely extends below the shoulder. Headaches are also a common complaint of both radiculopathy and mechanical neck pain.
The pain from cervical radiculopathy usually spreads further down the arm than mechanical neck pain. And unlike mechanical pain, radiculopathy also usually involves other changes in how the nerves work such as numbness, tingling, and weakness in the muscles of the shoulder, arm, or hand. With cervical radiculopathy, the reflexes in the muscles of the upper arm are usually affected. This is why doctors check reflexes when people have symptoms of cervical radiculopathy.
Diagnosis
How do doctors diagnose the problem?
Doctors gather the information about your symptoms as a way to determine which nerve is having problems. Diagnosis begins with a complete history of the problem. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities. Your answers can help your doctor determine which nerve is causing problems.
Next, the doctor examines you to see which neck movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are tested in order to tell where the nerve problem is coming from.
X-rays of the cervical spine can show the cause of pressure on the nerve. The images show whether degeneration has caused the space between the vertebrae to collapse. They may also show if a bone spur is pressing against a nerve.
If more information is needed, your doctor may order magnetic resonance imaging (MRI). The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the discs, nerves, and other soft tissues in the neck. The machine creates pictures that look like slices of the area your doctor is interested in. The test does not require any special dye or needles and is painless.
Sometimes it isn’t clear where the nerve pressure is coming from. Symptoms of numbness or weakness can also happen when the nerve is being pinched or injured at other points along its path. (An example of this is pressure on the median nerve in the wrist, known as carpal tunnel syndrome.) Electrical studies of the nerves going from the neck to the arm may be requested by your doctor to see whether the nerve problem is in the neck or further down the arm. However, most doctors take X-rays and try other forms of treatment before ordering electrical tests. These tests are usually only needed when the diagnosis is not clear.
If your doctor orders electrical studies, several tests are available to see how well the nerves are functioning, including the electromyography (EMG) test. This test measures how long it takes a muscle to work once a nerve signals it to move. The time it takes will be slower if nerve pressure from radiculopathy has affected the strength of the muscle.
Another electrical test that may be used instead of EMG is cervical root stimulation (CRS). This test involves putting a small needle through the back of the neck into the nerve where it leaves the spinal column. Readings of muscle action are then taken of the muscles on the front and back of the upper arm and along the inside of the lower arm. Doctors use the readings to determine which nerve is having problems.
Treatment
What treatment options are available?
Nonsurgical Treatment
Unless the nerve problem is getting worse rapidly, most doctors will begin with nonsurgical treatments.
At first, your doctor may prescribe immobilization of the neck. Keeping the neck still for a short time can calm inflammation and pain. This might include one to two days of bed rest and the use of a soft neck collar. This collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. Normally, a patient need only wear a collar for one to two weeks. Wearing it longer tends to weaken the neck muscles.
Doctors prescribe certain types of medication for patients with cervical radiculopathy. Severe symptoms may be treated with narcotic drugs, such as codeine or morphine. But these drugs should only be used for the first few days or weeks after problems with radiculopathy start because they are addictive when used too much or improperly. Muscle relaxants may be prescribed to calm neck muscles that are in spasm. You may be prescribed anti-inflammatory medications such as aspirin or ibuprofen.
Some doctors have their patients work with a physical therapist. At first, treatments are used to ease pain and inflammation. Electrical stimulation treatments can help calm muscle spasm and pain. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or the therapist can apply the traction pull by hand.
Some patients are given an epidural steroid injection (ESI).The spinal cord travels in a tube within the bones of the spinal canal. The cord is covered by a material called dura. The space between the dura and the spinal column is the epidural space. It is thought that injecting steroid medication into this space fights inflammation around the nerves, the discs, and the facet joints. In some cases, the steroid injection is given around one specific nerve. This is called a selective nerve block. The response to this treatment helps confirm which nerve root is causing the symptoms.
Doctors usually have their patients try nonoperative treatments for at least three months before considering surgery. But when patients simply aren’t getting better, or if the problem is becoming more severe, surgery may be suggested.
Surgery
Most people with cervical radiculopathy get better without surgery. In rare cases, people don’t get relief with nonsurgical treatments. They may require surgery. There are several types of surgery for cervical radiculopathy. These include
- foraminotomy
- discectomy
- fusion
Foraminotomy
A foraminotomy is done to open the neural foramen and relieve pressure on the spinal nerve root. A foraminotomy may be done because of bone spurs or inflammation.
Related Document: A Patient’s Guide to Cervical Foraminotomy
Discectomy
In a discectomy, the surgeon removes the disc where it is pressing against a nerve. Surgeons usually perform this surgery from the front (anterior) of the neck. This procedure is called an anterior cervical discectomy. In most patients, discectomy is done together with a procedure called cervical fusion, which is described next.
Related Document: A Patient’s Guide to Cervical Discectomy
Fusion
A fusion surgery joins two or more bones into one solid bone. The purpose for treating cervical radiculopathy with fusion is to increase the space between the vertebrae, taking pressure off the nerve. The surgery is most often done through the front of the neck. After taking out the disc (discectomy), the disc space is filled in with a small block of bone graft. The bone is allowed to heal, fusing the two vertebrae into one solid bone. The space between the vertebrae is propped and held open by the bone graft, which enlarges the neural foramina, taking pressure off the nerve roots.
Related Document: A Patient’s Guide to Anterior Cervical Discectomy and Fusion
Rehabilitation
Nonsurgical Rehabilitation
What should I expect from treatment?
Even if you don’t need surgery, your doctor may recommend that you work with a physical therapist. Patients are normally seen a few times each week for one to two months. In severe cases, patients may need a few additional weeks of care.
Your therapist creates a program to help you regain neck and arm function. Treatments for cervical radiculopathy often include neck traction, described earlier. Though neck traction is often done in the clinic, your therapist may give you a traction device to use at home.
It is very important to improve the strength and coordination in the neck and shoulder blade muscles. Your therapist can also evaluate your workstation or the way you use your body when you do your activities and suggest changes to avoid further problems.
After Surgery
Rehabilitation after surgery for cervical radiculopathy can be a slow process. You will probably need to attend physical therapy sessions for six to eight weeks, and you should expect full recovery to take up to four months.
During physical therapy after surgery, your therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. Then you begin learning how to move safely with the least strain on the healing neck.
As the rehabilitation program evolves, you will do more challenging exercises. The goal is to safely advance your strength and function. As your therapy sessions come to an end, your therapist will help you with decisions about getting you back to work. Your therapist can do a work assessment to make sure you’ll be able to do your job safely. Your therapist may suggest changes that could help you work safely, with less chance of reinjuring your neck.
When your treatment is well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource for you. But you will be in charge of doing your exercises as part of an ongoing home program.
Neck Pain
A Patient’s Guide to Neck Pain
Introduction
Neck pain is a common reason people visit their doctor. Neck pain typically doesn’t start from a single injury. Instead, the problem usually develops over time from the stress and strain of daily activities. Eventually, the parts of the spine begin to degenerate. The degeneration can become a source of neck pain.
Knowing how your neck normally works and why you feel pain are important in helping you care for your neck problem. Patients are often less anxious and more satisfied with their care when they have the information they need to make the best decisions about their condition.
This document will give you a general overview of neck pain. It should help you understand
- what parts make up the spine and neck
- what causes neck pain
- what tests your doctor may run
- how to decrease your pain and increase your mobility
Anatomy
What parts make up the cervical spine, and how do they work?
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
The cervical spine is formed by the first seven vertebrae. Doctors often refer to these vertebrae as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom edge of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine. This is where the chest begins.
Each vertebra is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body. When the vertebrae are stacked on top of each other, the rings form a hollow tube. This bony tube surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
As the spinal cord travels from the brain down through the spine, it sends out nerve branches between each vertebrae called nerve roots. These nerve roots join together to form the nerves that travel throughout the body and form the body’s electrical system. The nerve roots that come out of the cervical spine form the nerves that go to the arms and hands. The thoracic spine nerves go to the abdomen and chest. The nerves coming out of the lumbar (lower) spine go to the organs of the pelvis, the legs, and the feet.
One way to understand the anatomy of the cervical spine to look at a spinal segment. Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at that level, and the small facet joints (described later) that link each level of the spinal column.
An intervertebral disc is made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. In some cases, the collagen fibers join together to form a structure like a rope. In other cases, the fibers are arranged like a piece of cloth, or knitted materials such as you find in a sweater. The disc is a specialized connective tissue structure that separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made up of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the cervical spine allows freedom of movement as you bend and turn your neck.
The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the bone ends to move against each other smoothly, without pain.
Two spinal nerves exit the sides of each spinal segment, one on the left and one on the right. As the nerves leave the spinal cord, they pass through a small bony tunnel on each side of the vertebra, called a neural foramen. (The term used to describe more than one opening is neural foramina.)
Causes
Why do I have neck pain?
There are many causes of neck pain. Doctors are not always able to pinpoint the source of a patient’s pain. Your doctor will make every effort to ensure that your symptoms are not from a serious medical cause, such as cancer or a spinal infection. Below is a brief overview of some of the most common causes of neck pain.
Spondylosis
Most neck problems happen after years of wear and tear on the parts of the cervical spine. At first, these small injuries are not painful. But over time they can add up. Eventually they begin to cause neck pain.
Doctors sometimes call these degenerative changes in the spine spondylosis. Spondylosis can affect the bones and soft tissues of the spine. However, it is important to know that most problems with spondylosis are a normal part of aging.
Degenerative Disc Disease
The normal aging process involves changes within the intervertebral discs. Repeated stresses and strains weaken the connective tissues that make up a disc. Over time, the nucleus in the center of the disc dries out. When this happens, it loses some of its ability to absorb shock. The annulus also weakens and develops small cracks and tears.
Often these changes are not painful. But larger tears that reach to the outer edge of the annulus can cause neck pain. The body tries to heal the cracks with scar tissue. But scar tissue is not as strong as the tissue it replaces. At some point the disc may finally lose its ability to absorb shock for the spine. Then forces from gravity and daily activities can take even more of a toll on the disc and other structures of the spine.
View animation of degeneration
As the disc continues to degenerate, the space between the vertebrae becomes smaller. This compresses the facet joints along the back of the spinal column. As these joints are forced together, extra pressure builds on the articular cartilage on the surface of the facet joints. This extra pressure can damage the facet joints. Over time, this may lead to arthritis in the facet joints.
These degenerative changes in the disc, facet joints, and ligaments cause the spinal segment to become loose and unstable. The extra movement causes even more wear and tear on the spine. As a result, more and larger tears occur in the annulus.
The nucleus may push through the weakened and torn annulus and into the spinal canal. This is called a herniated or ruptured disc. The disc material that squeezes out can press against the spinal nerves. The disc also emits enzymes and chemicals that produce inflammation. The combination of pressure on the nerves and inflammation caused by the chemicals released from the disc cause pain.
As the degeneration continues, bone spurs develop around the facet joints and around the disc. No one knows exactly why these bone spurs develop. Most doctors think that bone spurs are the body’s attempt to stop the extra motion between the spinal segment. These bone spurs can cause problems by pressing on the nerves of the spine where they pass through the neural foramina. This pressure around the irritated nerve roots can cause pain, numbness, and weakness in the neck, arms, and hands.
Muscle Strain
People with minor neck pain or stiffness are often told they have a muscle strain. However, unless there was a severe injury to the neck, the muscles probably haven’t been pulled or injured. Instead, the problem may be coming from irritation or injury in other spine tissues, such as the disc or ligaments. When this happens, the neck muscles may go into spasm to help support and protect the sore area.
Mechanical Neck Pain
Mechanical neck pain is caused by wear and tear on the parts of the neck. It is similar in nature to a machine that begins to wear out. Mechanical pain usually starts from degenerative changes in the disc. As the disc starts to collapse, the space between the vertebrae narrows, and the facet joints may become inflamed. The pain is usually chronic. (Chronic pain builds over time and is long-lasting.) The pain is typically felt in the neck, but it may spread from the neck into the upper back or to the outside of the shoulder. Mechanical neck pain usually doesn’t cause weakness or numbness in the arm or hand, because the problem is not from pressure on the spinal nerves.
Radiculopathy (Pinched Nerve)
Pressure or irritation in the nerves of the cervical spine can affect the nerves’ electrical signals. The pressure or irritation can be felt as numbness on the skin, weakness in the muscles, or pain along the path of the nerve. Most people think of these symptoms as indications of a pinched nerve. Health care providers call this condition cervical radiculopathy.
Several conditions can cause radiculopathy. The most common are degeneration, disc herniation, and spinal instability.
Related Document: A Patient’s Guide to Cervical Radiculopathy
- Degeneration: As the spine ages, several changes occur in the bones and soft tissues. The disc loses its water content and begins to collapse, causing the space between the vertebrae to narrow. The added pressure may irritate and inflame the facet joints, causing them to become enlarged. When this happens, the enlarged joints can press against the nerves going to the arm as they squeeze through the neural foramina. Degeneration can also cause bone spurs to develop. Bone spurs may put pressure on nerves and produce symptoms of cervical radiculopathy.
- Herniated Disc: Heavy, repetitive bending, twisting, and lifting can place extra pressure on the shock-absorbing nucleus of the disc. If great enough, this increased pressure can injure the annulus (the tough, outer ring of the disc). If the annulus ruptures or tears, the material in the nucleus can squeeze out of the disc. This is called a herniation. Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand these pressures. However, as the annulus ages, it tends to crack and tear. It is repaired with scar tissue. Over time, the annulus becomes weakened, and the disc can more easily herniate through the damaged annulus.
If the herniated disc material presses against a nerve root it can cause pain, numbness, and weakness in the area the nerve supplies. This condition is called cervical radiculopathy (mentioned earlier). And any time the herniated nucleus contacts tissues outside the damaged annulus, it releases chemicals that cause inflammation and pain. If the nucleus herniates completely through the annulus, it may squeeze against the spinal cord. This causes a condition that is even more serious because it affects all the nerves of the spinal cord. This condition is called cervical myelopathy.
- Spinal Instability: Spinal instability means there is extra movement among the bones of the spine. Instability in the cervical spine can develop if the supporting ligaments have been stretched or torn from a severe injury to the head or neck. People with diseases that loosen their connective tissue may also have spinal instability. Spinal instability also includes conditions in which a vertebral body slips over the one just below it. When the vertebral body slips too far forward, the condition is called spondylolisthesis. Whatever the cause, extra movement in the bones of the spine can irritate or put pressure on the nerves of the neck, causing symptoms.
Spinal Stenosis (Cervical Myelopathy)
Stenosis means closed in. Spinal stenosis refers to a condition in which the spinal cord is closed in, or compressed, inside the tube of the spinal canal. Spinal stenosis may be caused by degenerative changes, such as bone spurs pushing against the spinal cord within the spinal canal.
However, stenosis can also develop when a person of any age has a disc herniation that pushes against the spinal canal. When the spinal cord is squeezed in the neck, doctors call the condition cervical myelopathy.
This is an alarming condition that demands medical attention. Cervical myelopathy can cause problems with the bowels and bladder, change the way you walk, and affect your ability to use your fingers and hand.
Symptoms
What are some of the symptoms of neck problems?
Symptoms from neck problems vary. They depend on your condition and which neck structures are affected. Some of the more common symptoms of neck problems are
- neck pain
- headaches
- pain spreading into the upper back or down the arm
- neck stiffness and reduced range of motion
- muscle weakness in the shoulder, arm, or hand
- sensory changes (numbness, prickling, or tingling) in the forearm, hand, or fingers
Diagnosis
How will my doctor find out what is causing my problem?
The diagnosis of neck problems begins with a thorough history of your condition. You might be asked to fill out a questionnaire describing your neck problems. Then your doctor will ask you questions to find out when you first started having problems, what makes your symptoms worse or better, and how the symptoms affect your daily activity. Your answers will help guide the physical examination.
Your doctor will then physically examine the muscles and joints of your neck. It is important that your doctor see how your neck is aligned, how it moves, and exactly where it hurts.
Your doctor may do some simple tests to check the function of the nerves. These tests measure your arm and hand strength, check your reflexes, and help determine whether you have numbness in your arms, hands, or fingers.
The information from your medical history and physical examination will help your doctor decide which tests to run. The tests give different types of information.
Radiological Imaging
Radiological imaging tests help your doctor see the anatomy of your spine. There are several kinds of imaging tests.
X-rays
X-rays show problems with bones, such as infection, bone tumors, or fractures. X-rays of the spine also can give your doctor information about how much degeneration has occurred in the spine, by showing the amount of space in the neural foramina and between the discs. X-rays are usually the first test ordered before any of the more specialized tests. Special X-rays called flexion and extension X-rays may help to determine if there is instability between vertebrae. These X-rays are taken from the side as you lean as far forward and then as far backward as you can. Comparing the two X-rays allows the doctor to see how much motion occurs between each spinal segment.
MRI
The magnetic resonance imaging (MRI) scan uses magnetic waves to create pictures of the cervical spine in slices. The MRI scan shows the cervical spine bones, as well as the soft tissue structures such as the discs, joints, and nerves.
MRI scans are painless and don’t require needles or dye. The MRI scan has become the most common test to look at the cervical spine after X-rays have been taken.
CT scan
The computed tomography (CT) scan is a special type of X-ray that lets doctors see slices of bone tissue. The machine uses a computer and X-rays to create these slices. It is used primarily when problems are suspected in the bones.
Myelogram
The myelogram is a special kind of X-ray test where a special dye is injected into the spinal sac. The dye shows up on an X-ray. It helps a doctor see if there is a herniated disc, pressure on the spinal cord or spinal nerves, or a spinal tumor. Before the CT scan and the MRI scan were developed, the myelogram was the only test that doctors had to look for a herniated disc. The myelogram is still used today but not nearly as often. The myelogram is usually combined with CT scan to give more detail.
Bone Scan
A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special X-rays of your neck. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem, and other tests such as the CT scan or MRI scan are then used to look at the area in detail.
Other Tests
Your doctor may also ask you to have other tests done.
Electromyogram
An electromyogram (EMG) is a special test used to determine if there are problems with any of the nerves going to the upper limbs. EMGs are usually done to determine whether the nerve roots have been pinched by a herniated disc. During the test, small needles are placed into certain muscles that are supplied by each nerve root. If there has been a change in the function of the nerve, the muscle will send off different types of electrical signals. The EMG test reads these signals and can help determine which nerve root is involved.
Laboratory Tests
Not all causes of neck pain are from degenerative conditions. Doctors use blood tests to identify other conditions, such as arthritis or infection. Other tests may be needed to rule out problems that do not involve the spine.
Treatment
What can be done to relieve my symptoms?
Nonsurgical Treatment
Whenever possible, doctors prefer to use treatments other than surgery. The first goal of these nonsurgical treatments is to ease your pain and other symptoms.
Your health care providers will work with you to improve your neck movement and strength. They will also encourage healthy body alignment and posture. These steps are designed to slow the degeneration process and enable you to get back to your normal activities.
Medications
Many different types of medications are typically prescribed to help gain control of the symptoms of neck pain. There is no medication that will cure neck pain. Your doctor may prescribe medications to ease pain, fight inflammation, and to help you get a better night’s sleep.
Soft Neck Collar
If your pain is severe, your doctor may recommend a soft neck collar to keep your neck still for short periods of time. Resting the muscles and joints can help calm pain, inflammation, and muscle spasm.
Ice and Heat Applications
You might also be advised to place a cold pack on your neck for 10 to 15 minutes at a time, or you may be shown how to do a contrast treatment. Contrast treatments involve switching between a cold pack and a hot pack.
Physical Therapy
Some doctors ask their patients to work with a physical therapist. Therapy treatments focus on relieving pain, improving neck movement, and fostering healthy posture. A therapist can design a rehabilitation program to address your particular condition and to help you prevent future problems.
Injections
Spinal injections are used for both treatment and diagnostic purposes. There are several different types of spinal injections that your doctor may suggest. These injections usually use a mixture of an anesthetic and some type of cortisone preparation. The anesthetic is a medication that numbs the area where it is injected. If the injection takes away your pain immediately, this gives your doctor important information suggesting that the injected area is indeed the source of your pain. The cortisone decreases inflammation and can reduce the pain from an inflamed nerve or joint for a prolonged period of time.
Some injections are more difficult to perform and require the use of a fluoroscope. A fluoroscope is a special type of X-ray that allows the doctor to see an X-ray picture continuously on a TV screen. The fluoroscope is used to guide the needle into the correct place before the injection is given.
- Epidural Steroid Injection: Neck pain or pain that spreads down the arm may require treatment with an epidural steroid injection (ESI). In an ESI, the medication mixture is injected into the epidural space around the nerve roots. Generally, an ESI is given only when other nonoperative treatments aren’t working. ESIs are not always successful in relieving pain. If they do work, they may only provide temporary relief.
- Selective Nerve Root Injection: Another type of injection to place steroid medication around a specific inflamed nerve root is called a selective nerve root injection. The fluoroscope is used to guide a needle directly to the painful spinal nerve. The nerve root is then bathed with the medication. Some doctors believe this procedure gets more medication to the painful spot. In difficult cases, the selective nerve root injection can also help surgeons decide which nerve root is causing the problem before surgery is planned.
- Facet Joint Injection: When the problem is thought to be in the facet joints, an injection into one or more facet joints can help determine which joints are causing the problem and ease the pain as well. The fluoroscope is used to guide a needle directly into the facet joint. The facet joint is then filled with medication mixture. If the injection immediately eases the pain, it helps confirm that the facet joint is a source of pain. The steroid medication will reduce the inflammation in the joint over a period of days and may reduce or eliminate your neck pain.
- Trigger Point Injections: Injections of anesthetic medications mixed with a cortisone medication are sometimes given in the muscles, ligaments, or other soft tissues near the spine. These injections are called trigger point injections. These injections can help relieve neck pain and ease muscle spasm and tender points in the neck muscles.
Surgery
Only rarely is cervical spine surgery scheduled immediately. Your doctor may suggest immediate surgery if there are signs of pressure developing on the spinal cord or if your muscles are becoming weaker very rapidly.
For other conditions, doctors prefer to try nonsurgical treatments for a minimum of three months before considering surgical options. Most people with neck pain tend to get better, not worse. Even people who have degenerative spine changes tend to gradually improve with time.
Surgery may be suggested when severe pain is not improving.
There are many different operations for neck pain. The goal of nearly all spine operations is to remove pressure from the nerves of the spine, to stop excessive motion between two or more vertebrae, or both.
The type of surgery that is best depends on the patient’s conditions and symptoms.
Foraminotomy
A foraminotomy is done to open up the neural foramen and relieve pressure on a spinal nerve root. A foraminotomy may be done because of bone spurs or inflammation.
Related Document: A Patient’s Guide to Cervical Foraminotomy
Laminectomy
The lamina is the covering layer of the bony ring of the spinal canal. It forms a roof-like structure over the back of the spinal cord. When the nerves in the spinal canal are being squeezed by a herniated disc or from bone spurs pushing into the canal, a laminectomy removes part or all of the lamina to release pressure on the spinal cord.
Related Document: A Patient’s Guide to Laminectomy
Discectomy
In a discectomy, the surgeon removes a problem disc. Surgeons usually do this surgery from the front of the neck. This procedure is called anterior cervical discectomy. In most patients, discectomy is done together with a procedure called cervical fusion (described next).
Related Document: A Patient’s Guide to Cervical Discectomy
Cervical Fusion
A fusion surgery joins two or more bones into one solid bone. The purpose for doing spinal fusion is to increase the space between the vertebrae and to keep the sore joint from moving. This is usually done by placing a small block of bone graft in the space where a disc was removed. Opening up more space enlarges the neural foramen, takes pressure off the nerve roots, and eases tension on the facet joints. Cervical fusion is used to treat neck problems such as cervical radiculopathy, disc herniations, fractures, and spinal instability. There are two main types of fusion for neck problems.
- Anterior Discectomy and Fusion:
 Anterior discectomy and fusion is done through the front of the neck. After taking out the disc (discectomy), the disc space is filled with a small graft of bone. The bone is allowed to heal, fusing the two vertebrae into one solid bone.
Anterior discectomy and fusion is done through the front of the neck. After taking out the disc (discectomy), the disc space is filled with a small graft of bone. The bone is allowed to heal, fusing the two vertebrae into one solid bone.Related Document: A Patient’s Guide to Anterior Cervical Discectomy and Fusion
- Posterior Fusion:
 In posterior fusion, the surgeon lays small grafts of bone over the back of the spine. When these bones heal together, they fuse the two vertebrae into one solid bone. Posterior fusions in the cervical spine are primarily used to treat fractures of the neck.
In posterior fusion, the surgeon lays small grafts of bone over the back of the spine. When these bones heal together, they fuse the two vertebrae into one solid bone. Posterior fusions in the cervical spine are primarily used to treat fractures of the neck.Related Document: A Patient’s Guide to Posterior Cervical Fusion
The bone graft needs time to heal in order for the fusion to succeed. This requires the neck to be held still. After cervical fusion surgery, patients usually have to wear a special neck brace for several months. These neck braces are often bulky and restrictive. Recently, surgeons have begun using metal plates and screws (often referred to as instrumentation) to lock the bones in place. The instrumentation is fastened to the vertebrae, where it holds the bones still while the graft heals.
Corpectomy and Strut Graft
A corpectomy relieves pressure over a large part of the spinal cord. In this procedure, the surgeon takes off the front part of the spinal column and removes several vertebral bodies. The spaces are then filled with bone graft material. Metal plates and screws are generally used to hold the spine in place while it heals. A corpectomy is used in cases of severe spinal stenosis and myelopathy.
Related Document: A Patient’s Guide to Cervical Corpectomy and Strut Graft
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Nonsurgical treatments can maximize the health of your neck and prolong the time before some type of surgery is needed. Physical therapy treatment is often prescribed for two to four weeks for patients with neck pain. Treatments are designed to help ease pain and to improve mobility, strength, posture, and function. Therapy treatments will teach you how to control your symptoms and protect your neck in the years ahead. You may be given exercises to do on a regular basis.
After Surgery
Rehabilitation after surgery is much more complex. Some patients leave the hospital shortly after surgery, but some surgeries require patients to stay in the hospital for a few days. Patients who stay in the hospital may visit with a physical therapist in the hospital room soon after surgery. The treatment sessions help patients learn to move and do routine activities without putting extra strain on the neck.
Many surgical patients need physical therapy outside of the hospital as well. They often see a therapist for one to three months, depending on the type of surgery. Therapy treatments are designed to calm pain and muscle spasm, teach patients to move safely, and help patients develop strength and mobility.
As the therapy sessions come to an end, the therapist may help the patient get back to work. The therapist can do a work assessment to ensure the patient can do his or her job safely. Some patients may need to modify their work or other activities to avoid future problems.