Spine
Cervical Spine Anatomy Animated Tutorial
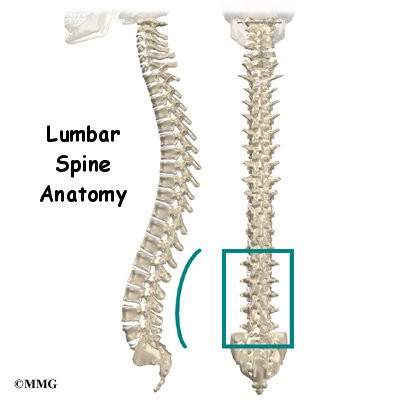
Lumbar Spine Anatomy
A Patient’s Guide to Lumbar Spine Anatomy
Introduction
Knowing the main parts of your low back and how these parts work is important as you learn to care for your back problem.
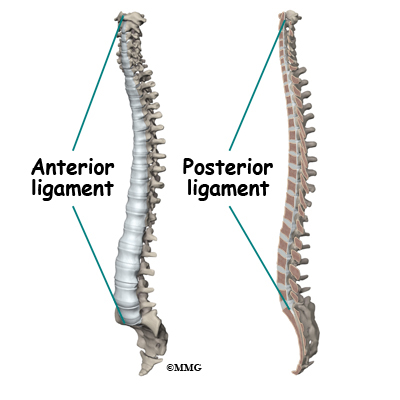
Two common anatomic terms are useful as they relate to the low back. The term anterior refers to the front of the spine. The term posterior refers to the back of the spine. The section of the spine that makes up the low back is called the lumbar spine. The front of the low back is therefore called the anterior lumbar area. The back of the lower spine is called the posterior lumbar area.
In addition to reading this article, be sure to watch our Lumbar Spine Anatomy Animated Tutorial Video.
This guide gives a general overview of the anatomy of the low back. It should help you understand
- what parts make up the low back
- how these parts work
Important Structures
The important parts of the lumbar spine include
- bones and joints
- nerves
- connective tissues
- muscles
- spinal segments
This section highlights important structures in each category.
Bones and Joints
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
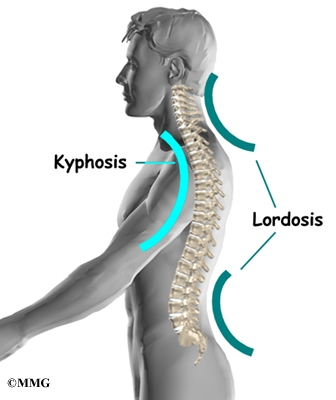
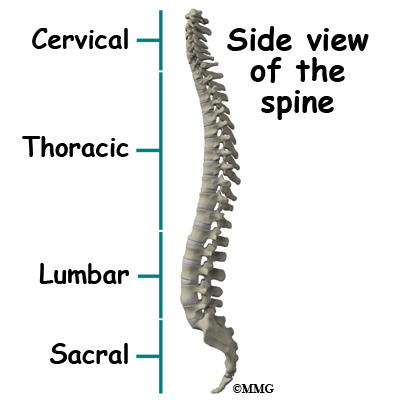
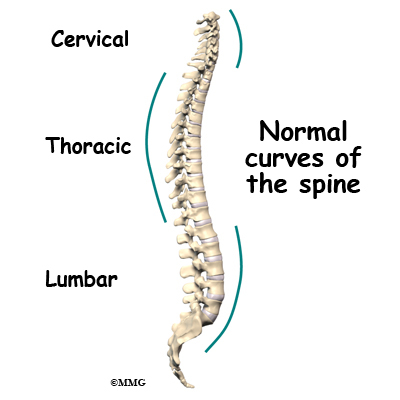
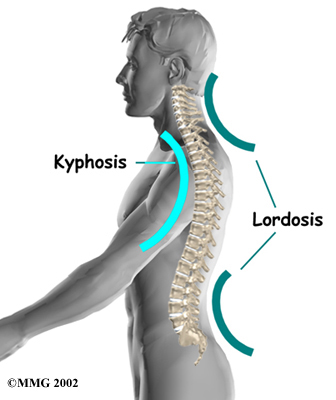
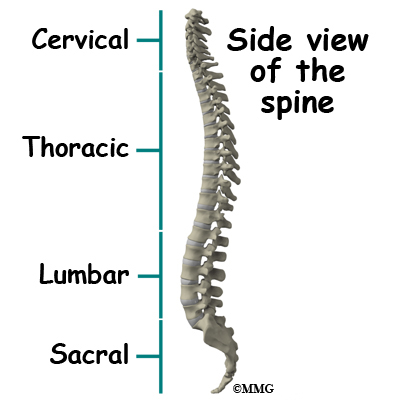
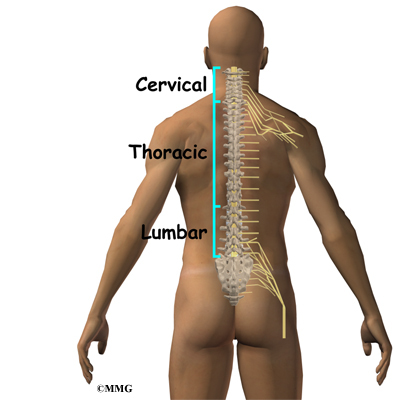
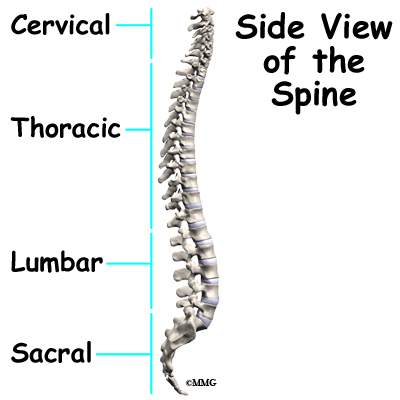
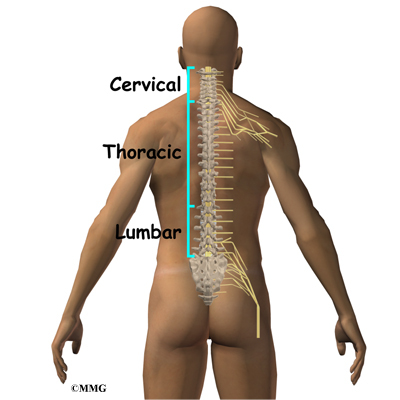
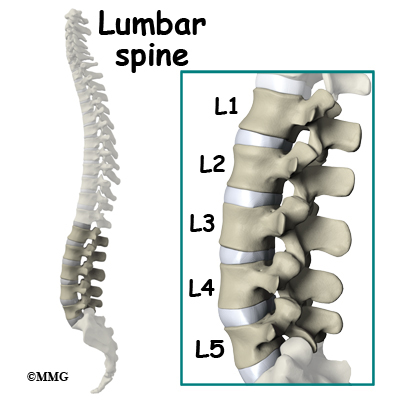
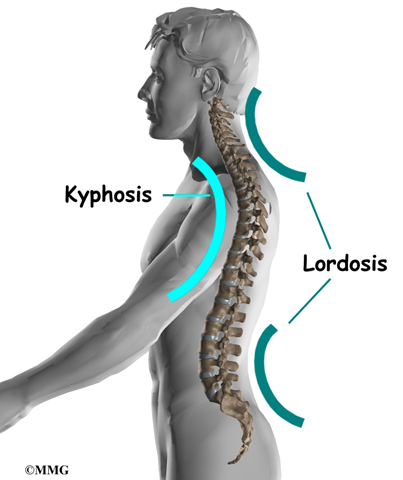
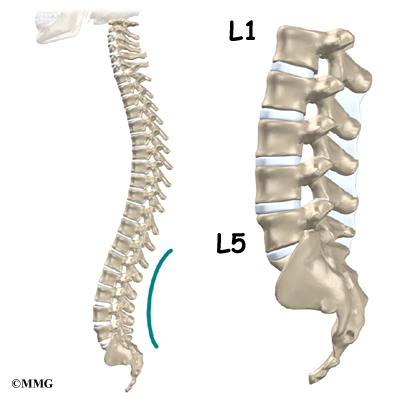
From the side, the spine forms three curves. The neck, called the cervical spine curves slightly inward.
The middle back, or thoracic spine curves outward. The outward curve of the thoracic spine is called kyphosis. The low back, also called the lumbar spine curves slightly inward. An inward curve of the spine is called lordosis.
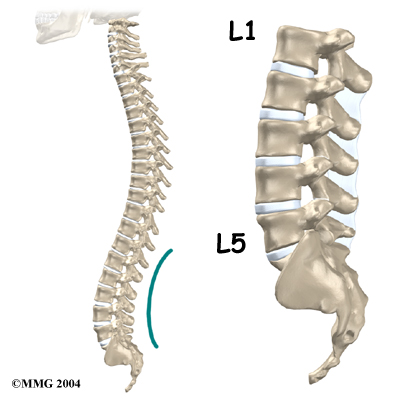
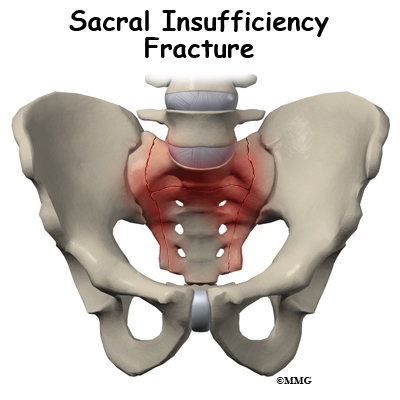
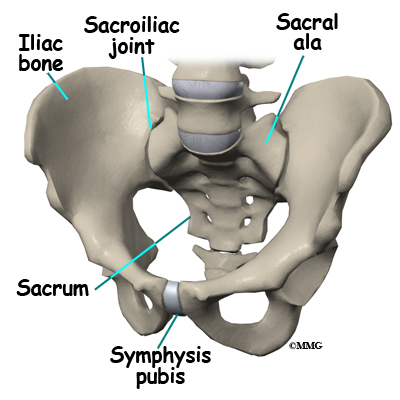
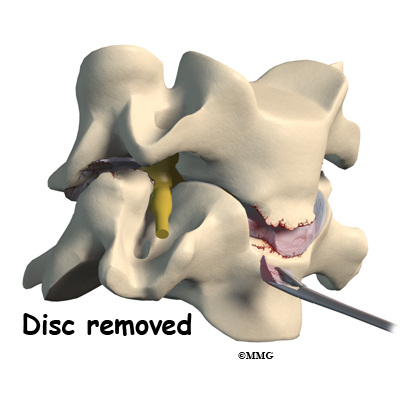
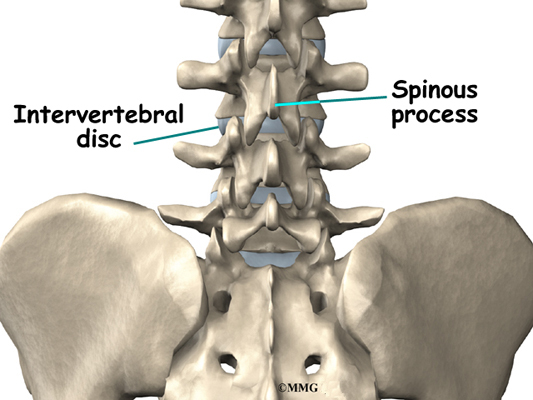
The lumbar spine is made up of the lower five vertebrae. Doctors often refer to these vertebrae as L1 to L5. The lowest vertebra of the lumbar spine, L5, connects to the top of the sacrum, a triangular bone at the base of the spine that fits between the two pelvic bones. Some people have an extra, or sixth, lumbar vertebra. This condition doesn’t usually cause any particular problems.
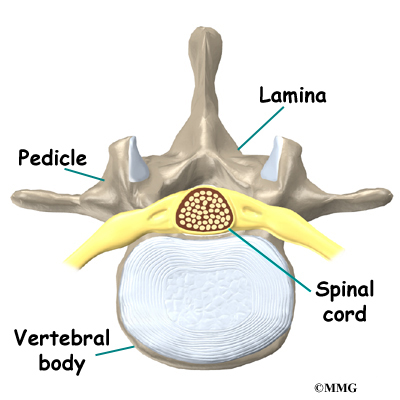
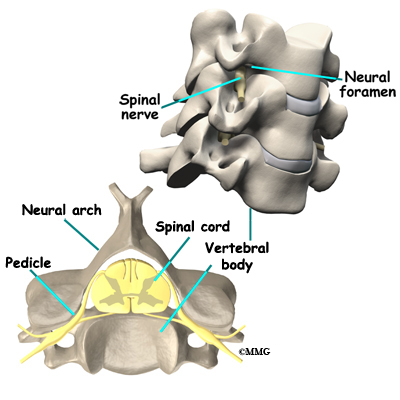
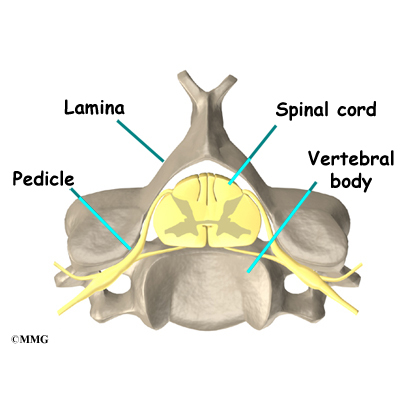
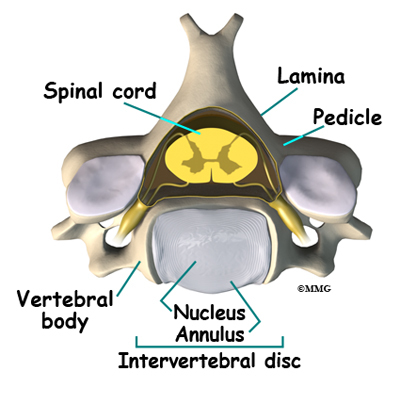
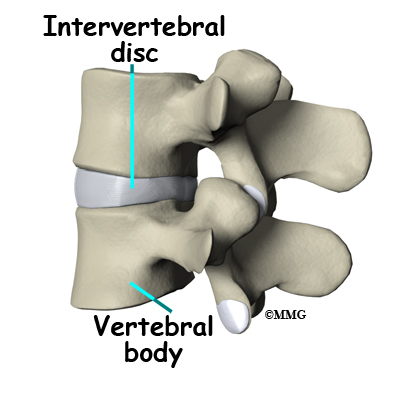
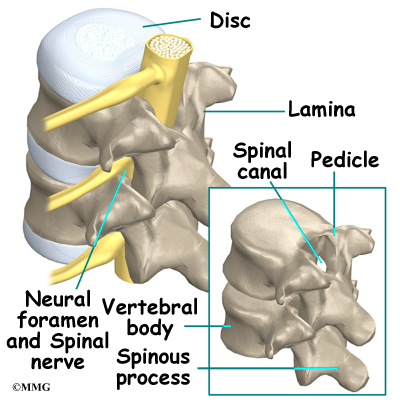
Each vertebra is formed by a round block of bone, called a vertebral body. The lumbar vertebral bodies are taller and bulkier compared to the rest of the spine. This is partly because the low back has to withstand pressure from body weight and from movements such as lifting, carrying, and twisting. Also, large and powerful muscles attaching on or near the lumbar spine place extra force on the lumbar vertebral bodies.
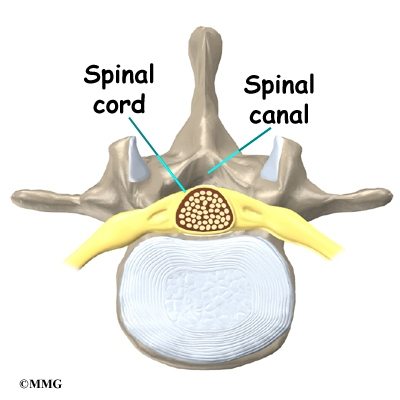
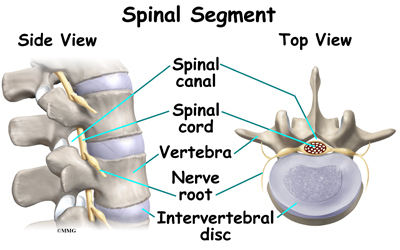
A bony ring attaches to the back of each vertebral body. This ring has two parts. Two pedicle bones connect directly to the back of the vertebral body. Two lamina bones join the pedicles to complete the ring. The lamina bones form the outer rim of the bony ring. When the vertebrae are stacked on top of each other, the bony rings form a hollow tube that surrounds the spinal cord and nerves. The laminae provide a protective roof over these nerve tissues.
A bony knob projects out at the point where the two lamina bones join together at the back of the spine. These projections, called spinous processes, can be felt as you rub your fingers up and down the back of your spine. Each vertebra also has two bony knobs that point out to the side, one on the left and one on the right. These bony projections are called transverse processes. The projections in the low back are broader than in other areas of the spine because many large back muscles attach and impart powerful forces on them.
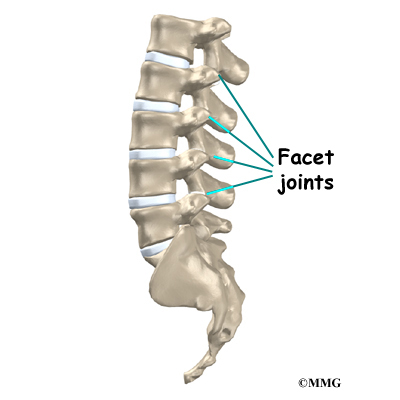
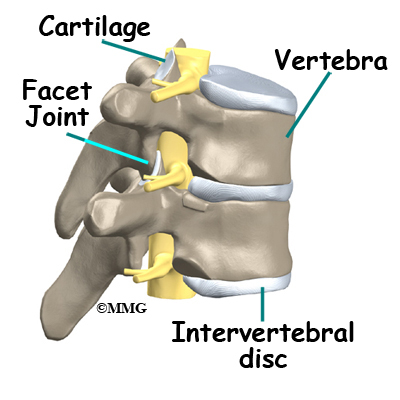
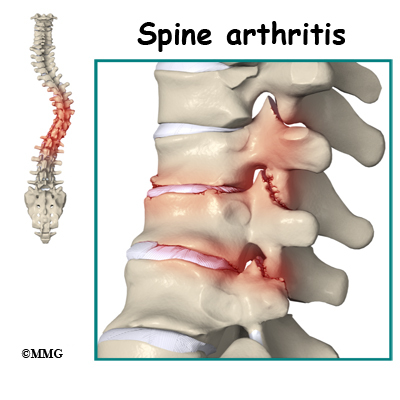
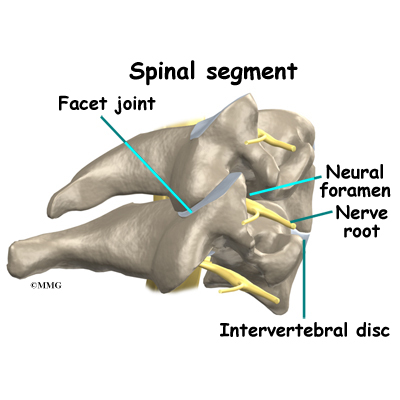
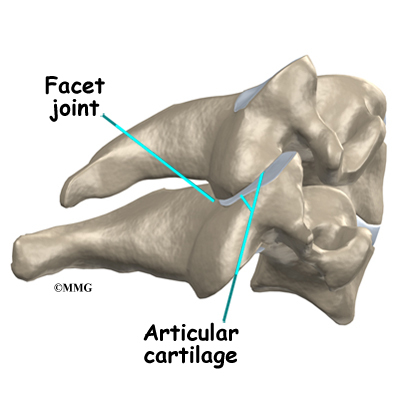
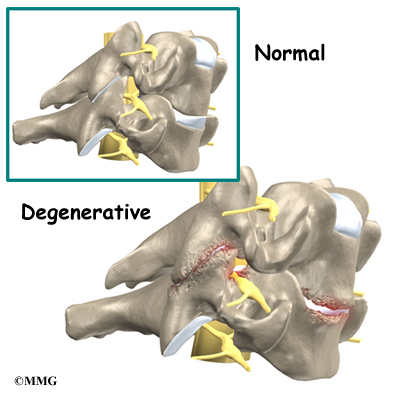
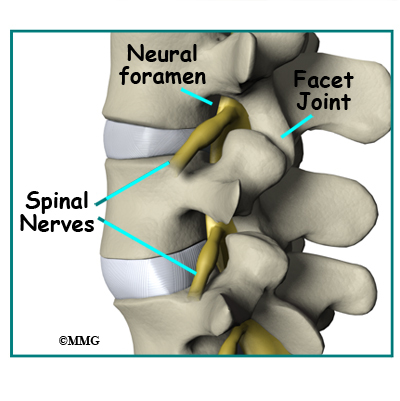
Between the vertebrae of each spinal segment are two facet joints. The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
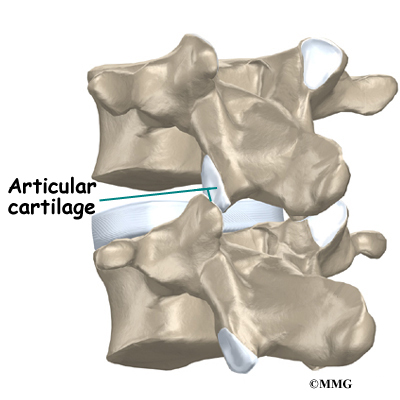
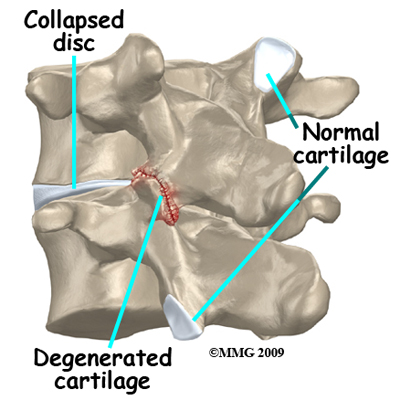
The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the ends of bones to move against each other smoothly, without friction.
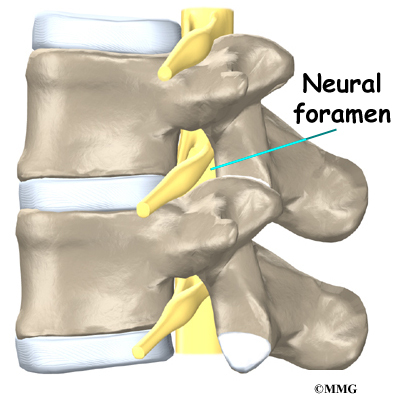
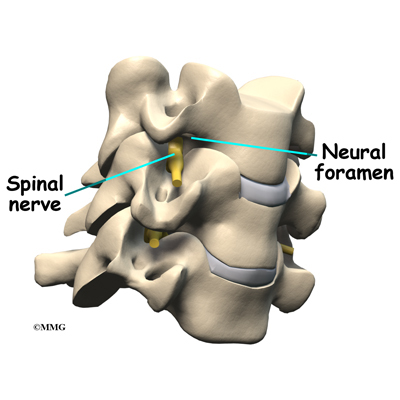
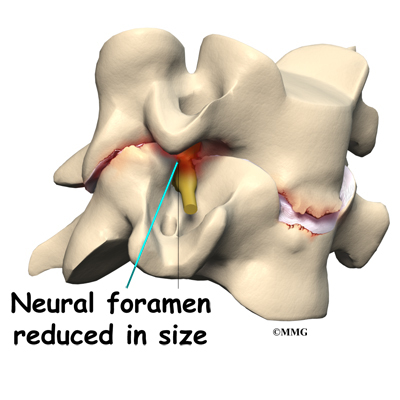
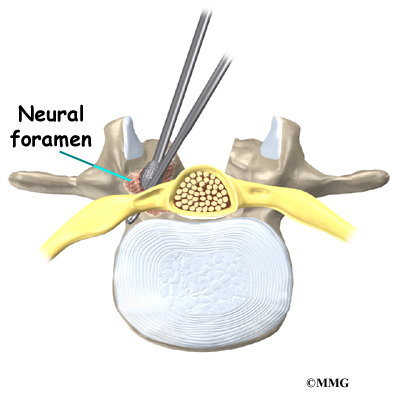
On the left and right side of each vertebra is a small tunnel called a neural foramen. (Foramina is the plural term.) The two nerves that leave the spine at each vertebra go through the foramina, one on the left and one on the right. The intervertebral disc (described later) sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits in back of the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
Nerves
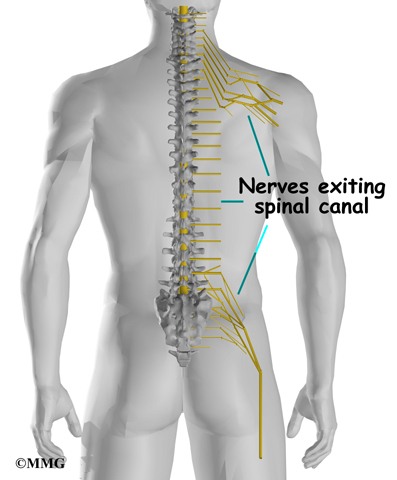
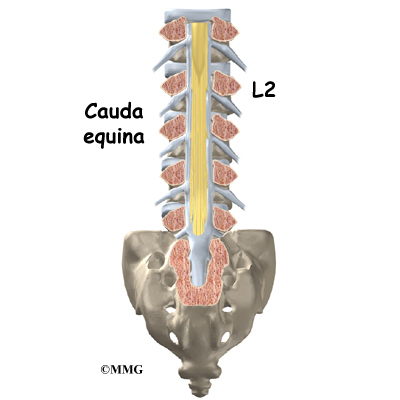
The hollow tube formed by the bony rings on the back of the spinal column surrounds the spinal cord. The spinal cord is like a long wire made up of millions of nerve fibers. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
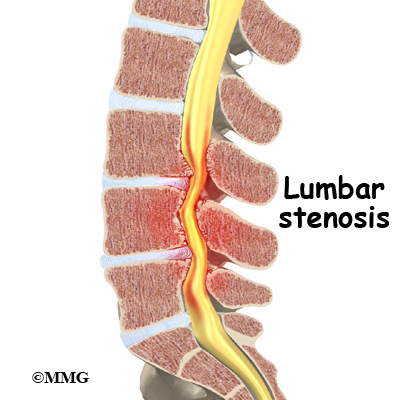
The spinal cord extends down to the L2 vertebra. Below this level, the spinal canal encloses a bundle of nerves that goes to the lower limbs and pelvic organs. The Latin term for this bundle of nerves is cauda equina meaning horse’s tail.
Between vertebrae, two large nerves branch off the spinal cord, one on the left and one on the right. The nerves pass through the neural foramina of each vertebra. These spinal nerves group together to form the main nerves that go to the organs and limbs. The nerves of the lumbar spine (cauda equina) go to the pelvic organs and lower limbs.
Connective Tissues
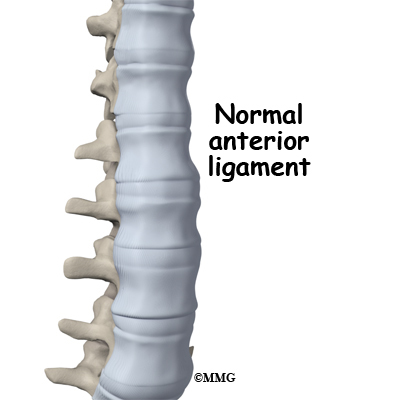
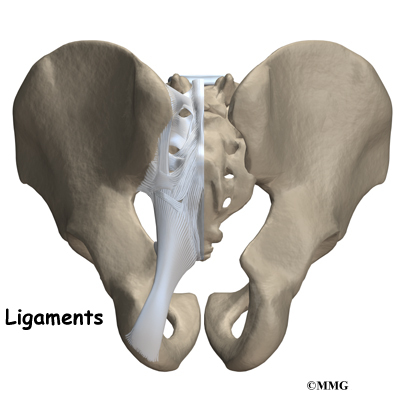
Connective tissues are networks of fiber that hold the cells of the body together. Ligaments are strong connective tissues that attach bones to other bones. Several long ligaments connect on the front and back sections of the vertebrae. The anterior longitudinal ligament runs lengthwise down the front of the vertebral bodies. Two other ligaments run full-length within the spinal canal. The posterior longitudinal ligament attaches on the back of the vertebral bodies. The ligamentum flavum is a long elastic band that connects to the front surface of the lamina bones (just behind the spinal cord). Thick ligaments also connect the bones of the lumbar spine to the sacrum (the bone below L5) and pelvis.
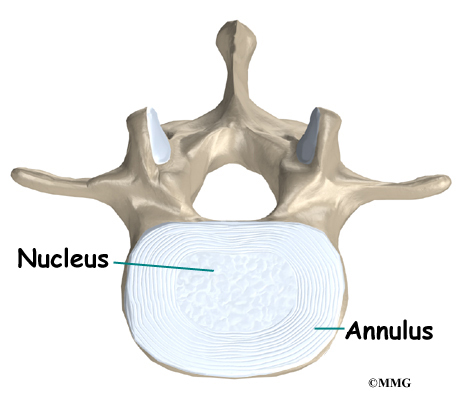
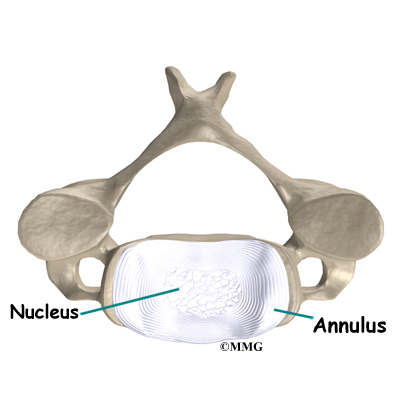
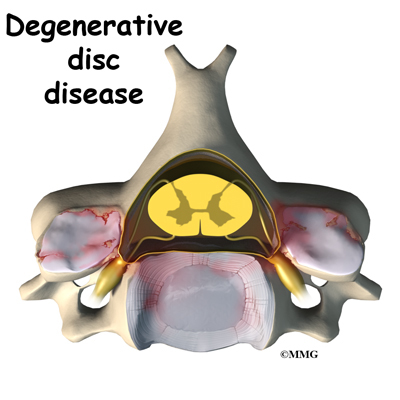
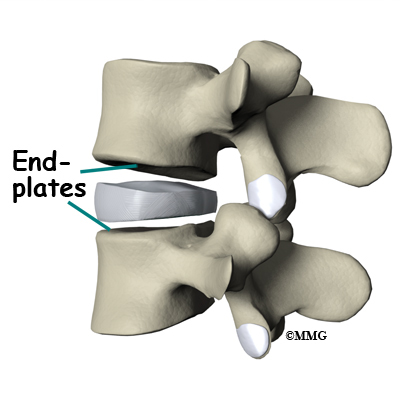
A special type of structure in the spine called an intervertebral disc is also made of connective tissue. The fibers of the disc are formed by special cells, called collagen cells. The fibers may be lined up like strands of nylon rope or crisscrossed like a net.
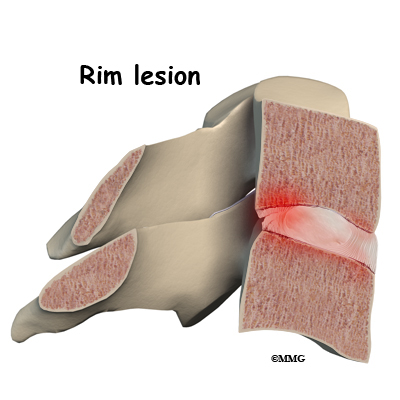
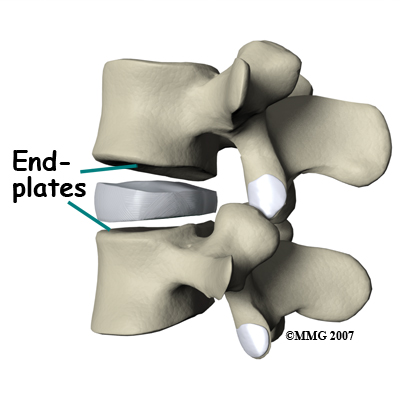
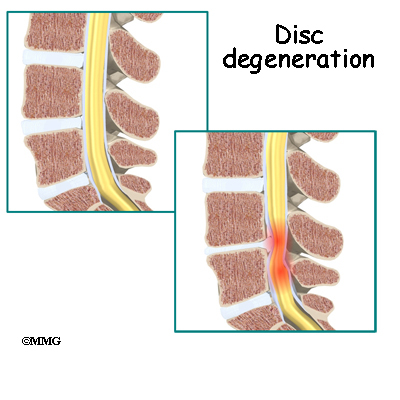
An intervertebral disc is made of two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption in the spine. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
Muscles
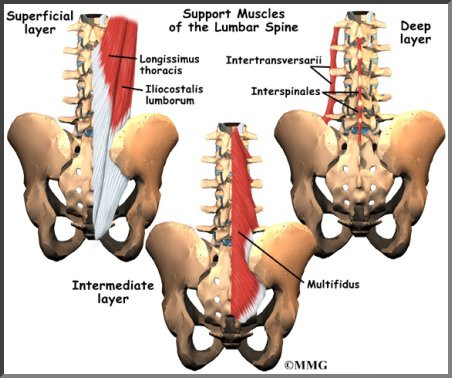
The muscles of the low back are arranged in layers. Those closest to the skin’s surface, the superficial layer, are covered by a thick tissue called fascia. The middle layer, called the erector spinae, has strap-shaped muscles that run up and down over the lower ribs, chest, and low back. They join in the lumbar spine to form a thick tendon that binds the bones of the low back, pelvis, and sacrum. The deepest layer of muscles attaches along the back surface of the spine bones, connecting the low back, pelvis, and sacrum. These deepest muscles coordinate their actions with the muscles of the abdomen to help hold the spine steady during activity.
Spinal Segment
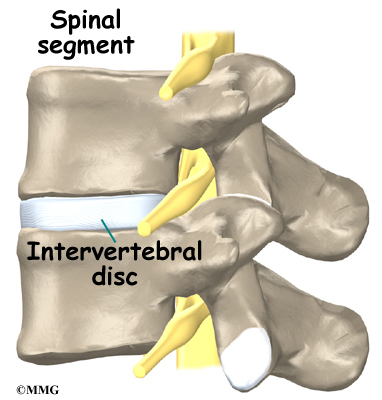
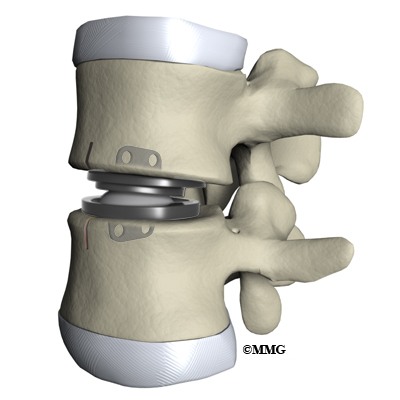
A good way to understand the anatomy of the lumbar spine is by looking at a spinal segment. Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal column at each vertebra, and the small facet joints that link each level of the spinal column.
The intervertebral disc separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during heavy activities that put strong force on the spine, such as jumping, running, and lifting.
The spinal segment is connected by two facet joints, described earlier. When the facet joints of the lumbar spine move together, they bend and turn the low back.
Summary
Many important parts make up the anatomy of the back. Understanding the regions and structures of the lumbar spine can help you be more involved in your health care and better able to care for your back problem.
Transcutaneous Electrical Stimulation (TENS) for Cervical Spine Pain
A Patient’s Guide to Transcutaneous Electrical Stimulation (TENS) for Cervical Spine Pain
Introduction
Neck (cervical spine) pain due to musculoskeletal disorders, is the second largest cause of time off work – low back pain being first. It is generally worse in the morning and evening. The most commonly prescribed intervention is rest and analgesics, and often a referral to physical therapy. Among the rehabilitation intervention treatments for neck pain is the transcutaneous electrical nerve stimulation (TENS) unit.
Electrical nerve stimulation is a treatment for pain that is used primarily for chronic pain. The electrical stimulation is delivered through electrodes or patches placed on the skin. The technique and the device used is called transcutaneous electrical stimulation or TENS for short.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
This guide will help you understand
- who may benefit from a TENS unit
- how a TENS unit works
- what to expect with a TENS unit
Who may benefit from a TENS unit
TENS can be used for relief of pain associated with a wide variety of painful conditions. This may include back pain caused by spine degeneration, disc problems, or failed back surgery. Nerve pain from conditions such as chronic regional pain syndrome (CRPS) and neuropathies caused by diabetes or as a side effect of cancer treatment may also be managed with TENS.
TENS has been used for people suffering from cancer-related pain, phantom-limb pain (a chronic pain syndrome following limb amputation), and migraine or chronic tension-type headaches.
TENS can also be used for muscle soreness from overuse, inflammatory conditions, and both rheumatoid and osteoarthritis. Athletes with painful acute soft tissue injuries (e.g., sprains and strains) may benefit from TENS treatment.
Sometimes it is used after surgery for incisional or post-operative pain from any type of surgery (e.g., joint replacement, cardiac procedures, various abdominal surgeries, cesaerean section for the delivery of a baby). Studies show that TENS can significantly reduce the use of analgesics (pain relievers, including narcotic drugs) after surgery.
TENS is usually used along with other forms of treatment and pain control such as analgesics, relaxation therapy, biofeedback, visualization or guided imagery, physical therapy and exercise, massage therapy, nerve block injections, and/or spinal manipulation.
The effectiveness of TENS remains controversial. The American Academy of Neurology (AAN) findings published in Dec. 30, 2009 issue of Neurology claims it is not effective and cannot be recommended. But, many patients find TENS effective for pain relief, easy to use, and with very low side effects. It may be worth a try for those who suffer from chronic low back pain. It can be discontinued easily if it doesn’t work. TENS cannot correct an underlying problem; it is only used for temporary relief of symptoms.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
To summarize, the benefits from TENS treatment can include:
- pain relief
- increased circulation and healing
- decreased use of pain relievers or other analgesic drugs
- increased motion and function
How does TENS work?
TENS produces an electrical impulse that can be adjusted for pulse, frequency, and intensity. The exact mechanism by which it works to reduce or even eliminate pain is still unknown. It is possible there are several different ways TENS works. For example, TENS may inhibit (block) pain pathways or increase of the secretion of the pain reducing substances (e.g., endorphins, serotonin) in the CNS.
Electrical nerve stimulation is a treatment for pain that is used primarily for chronic pain. The electrical stimulation is delivered through electrodes or patches placed on the skin. The technique and the device used is called transcutaneous electrical neurostimulation or TENS for short.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary or even long-lasting pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
Recent research has also shown that autosuggestion or the placebo effect is a powerful way many people experience pain relief or improvement in symptoms. Simply by believing the treatment (any treatment, including TENS) will work has a beneficial effect on the nervous system. Many studies have shown that people get pain relief through the placebo effect alone.
How do I use my TENS unit?
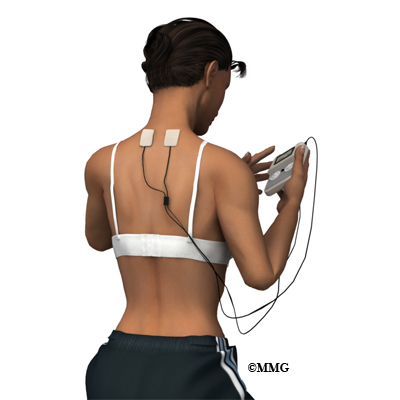
You will be shown how to use your TENS device by your healthcare provider trained in the set-up and use of this modality. Round or square rubber electrodes are applied to the skin over or around the painful area. Usually four electrodes (two pairs) are used to get maximum benefit from this treatment.
The electrodes are self-adhesive with a protective layer of gel built in to prevent skin irritation or burning. The unit is battery-operated with controls you manipulate yourself to alter the strength of the electrical signal. The unit can be slipped into a pocket or clipped to your belt. You may use two or four electrodes.
The electrodes will be placed on your body at positions selected by a physician or physical therapist. The electrode placement is determined based on the location of the involved nerves and/or the location of your pain.
The first place to try the electrodes is either directly over the painful area or on either side of the pain. You will slowly turn up the intensity of the unit until you feel a buzzing, tingling, or thumping sensation strong enough to override the pain signals.
If that doesn’t work, you may get better results putting the electrodes over the area where the spinal nerve root exits the vertebra. Sometimes it takes a bit of trial and error to find the right settings and best electrode placement for you.
Be sure and let your healthcare provider know if you experience increased pain. Electrodes placed below the level of a peripheral nerve impairment might actually block the input from the TENS unit and cause increased pain. Or placement over an area of scar tissue from surgery can cause increased skin resistance and decreased transmission of the electrical impulses.
Another way to use TENS is over spots in the muscles that trigger pain called trigger points (TrPs). Trigger points are areas of hyperirritability in the muscles that can cause chronic pain. The healthcare provider will identify any TrPs present during your exam. Usually TrPs are taken care of with a treatment designed to eliminate them. In some patients they are chronic and don’t go away or come back easily. In such cases, TENS may be helpful.
Your health care team will guide you through the trial-and-error process for finding the best electrode placement for you and make any changes needed in the program.
When you should NOT use TENS
- If you have loss of skin sensation or even decreased sensation, you should not use TENS. With altered sensation, there is a risk of turning the unit up too high and causing injury or harm.
- The use of TENS is not recommended for older adults with Alzheimer’s, dementia, or other cognitive problems.
- If you have a cardiac pacemaker, you should not use TENS as the electrical signals could interfere with your pacemaker. Cardiac patients should not use TENS without their physician’s approval.
Some guidelines when using TENS
- Before applying the electrodes, it is important to remove all lotions, oils, or other applications to the skin. You may want to shave hair from the local area where the electrode will be applied.
- Daily use of TENS for several hours at a time is recommended. You should not wear the unit for long periods of time (e.g., 24 hours) or during extended sleep time (napping is okay but TENS should not be used while sleeping at night or for more than a couple of hours).
- Never place an electrode over an open wound or area of skin irritation. Report any skin problems or burns immediately.
- Do not place electrodes near your eyes or over your throat.
- Do not use TENS in the shower or bathtub.
- Move the electrodes a bit each time you put them on to avoid skin irritation.
- You should experience a comfortable tingling sensation that is comfortable enough to allow you to complete daily tasks and activities.
- You may want to keep a daily journal of your pain levels, the settings you use, and a record of the medications you are taking for pain relief. By reviewing your notes, you may find the best combination of electrode placement and unit settings that gives you the most pain relief.
What you can expect with TENS
You should feel a mild to moderately strong tingling or buzzing sensation. Some people experience a more unpleasant sensation described as burning or prickling. Depending on the intensity and duration of your pain, you may or may not get results right away.
It can take several days to even several weeks to get the desired results. Differences in results may occur based on properties of skin resistance, type of pain, and individual differences in the mechanism of pain control. Be patient and persistent. Do not hesitate to contact your healthcare provider as often as it takes to get the desired results.
Many patients do report good-to-excellent results, first with pain control, then pain relief, and finally reduction in the use of medications. Although it doesn’t happen for everyone, some chronic pain patients are “cured” permanently from their pain.
As each of these benefits from the TENS treatment occur, you may find yourself increasing your activity level – either with the same level of TENS usage or even with reduced frequency of use, intensity of signal, or duration (length of time the unit is turned on).
If for any reason your pain starts to increase in frequency, duration, or intensity, don’t assume the treatment isn’t working for you. First, check the TENS unit for any malfunction, need to recharge, or replace the electrodes with new ones. If your unit is battery-operated, you may find it necessary to turn the intensity up to obtain the same sensation when the batteries are low. This should alert you to the need for battery replacement.
Finally, be aware that some patients experience “breakthrough pain,” referring to a situation in which you get pain relief at first but then even with the TENS unit, you start to have pain once again. Turning the intensity up high enough to cause muscle contraction is an indication of breakthrough pain.
Sometimes a different setting for the stimulator may be needed when this happens. Most units have a setting that allows for random pulse frequency, duration, and amplitude. The use of this setting helps keep the nervous system from getting used to a specific amount of stimulation and ignoring it. This phenomenon is called habituation or adaptation.
Summary
TENS is an effective method of pain control for chronic pain when you want to maintain your normal routine of daily activities that would otherwise be hampered by too high of pain levels. TENS helps many people reduce and sometimes even eliminate the use of pain medications, thus avoiding side-effects of long-term drug use.
Even without complete pain relief, TENS makes it possible to stay active and participate in work, family, and even recreational activities. There are no significant adverse effects from the use of TENS. The ability of this treatment technique to moderate pain and reduce the use of pain medications is a real benefit — especially with the potential for serious or adverse effects from long-term use of pain relievers.
Transcutaneous Electrical Stimulation (TENS) for Chronic Lumbar Spine Pain
A Patient’s Guide to Transcutaneous Electrical Stimulation (TENS) for Chronic Lumbar Spine Pain
Introduction
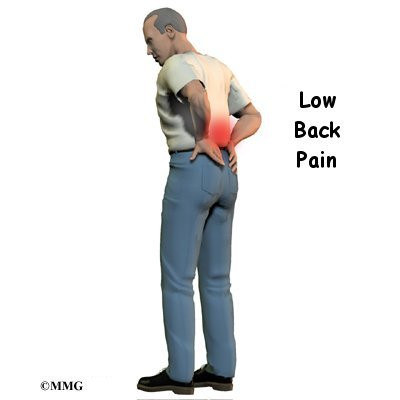
Low back pain due to musculoskeletal disorders, is the largest cause of time off work. The most commonly prescribed intervention is rest, pain medications, and a referral to physical therapy.
Physicians and physical therapists commonly recommend the use of a transcutaneous electrical nerve stimulation (TENS) unit as part of a pain management strategy for controlling low back pain. TENS is used primarily for chronic pain.
This guide will help you understand
- who may benefit from a TENS unit
- how a TENS unit works
- what to expect with a TENS unit
Who may benefit from a TENS?
TENS can be used for relief of pain associated with a wide variety of painful conditions. This may include back pain caused by spine degeneration, disc problems, or failed back surgery. Nerve pain from conditions such as chronic regional pain syndrome (CRPS) and neuropathies caused by diabetes or as a side effect of cancer treatment may also be managed with TENS.
TENS has been used for people suffering from cancer-related pain, phantom-limb pain (a chronic pain syndrome following limb amputation), and migraine or chronic tension-type headaches.
TENS can also be used for muscle soreness from overuse, inflammatory conditions, and both rheumatoid and osteoarthritis. Athletes with painful acute soft tissue injuries (e.g., sprains and strains) may benefit from TENS treatment.
Sometimes it is used after surgery for incisional or post-operative pain from any type of surgery (e.g., joint replacement, cardiac procedures, various abdominal surgeries, cesaerean section for the delivery of a baby). Studies show that TENS can significantly reduce the use of analgesics (pain relievers, including narcotic drugs) after surgery.
TENS is usually used along with other forms of treatment and pain control such as analgesics, relaxation therapy, biofeedback, visualization or guided imagery, physical therapy and exercise, massage therapy, nerve block injections, and/or spinal manipulation.
The effectiveness of TENS remains controversial. The American Academy of Neurology (AAN) findings published in Dec. 30, 2009 issue of Neurology claims it is not effective and cannot be recommended. But, many patients find TENS effective for pain relief, easy to use, and with very low side effects. It may be worth a try for those who suffer from chronic low back pain. It can be discontinued easily if it doesn’t work. TENS cannot correct an underlying problem; it is only used for temporary relief of symptoms.
TENS is a noninvasive way to override or block signals from the nerves to the spinal cord and brain. Pain messages may be altered enough to provide temporary pain relief. Besides controlling pain, this type of electrical stimulation can also improve local circulation and reduce or eliminate muscle spasm.
To summarize, the benefits from TENS treatment can include:
- pain relief
- increased circulation and healing
- improved sleep pattern
- decreased use of pain relievers or other analgesic drugs
- increased motion and function
How does a TENS work?
TENS produces an electrical impulse that can be adjusted for pulse, frequency, and intensity. The exact mechanism by which it works to reduce or even eliminate pain is still unknown. It is possible there are several different ways TENS works. For example, TENS may inhibit (block) pain pathways or increase of the secretion of the pain reducing substances (e.g., endorphins, serotonin) in the CNS.
Electrical stimulation has been shown to enhance tissue healing by improving circulation. This effect may alter pain perception.
Some integrative medicine practitioners also believe that it’s possible that the flow of energy through the meridian system modifies the sensation of pain. These practitioners believe that meridians are interconnected channels of energy throughout the body that are closely linked with the central nervous system (brain and spinal cord) as well as the peripheral nervous system (spinal nerves). These practitioners suggest that the electrical stimulation from the TENS unit is able to open up any blocked areas of energy flow bringing pain relief.
Recent research has also shown that autosuggestion or the placebo effect is a powerful way many people experience pain relief or improvement in symptoms. Simply by believing the treatment (any treatment, including TENS) will work has a beneficial effect on the nervous system. Many studies have shown that people get pain relief through the placebo effect alone.
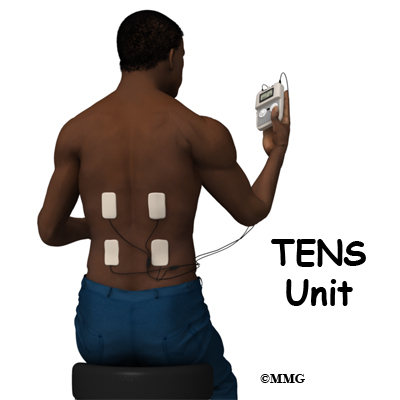
How do I use my TENS unit
You will be shown how to use your TENS device by your healthcare provider trained in the set-up and use of this modality. Round or square rubber electrodes are applied to the skin over or around the painful area. Usually four electrodes (two pairs) are used to get maximum benefit from this treatment.
The electrodes are self-adhesive with a protective layer of gel built in to prevent skin irritation or burning. The unit is battery-operated with controls you manipulate yourself to alter the strength of the electrical signal. The unit can be slipped into a pocket or clipped to your belt. You may use two or four electrodes.
The electrodes will be placed on your body at positions selected by a physician or physical therapist. The electrode placement is determined based on the location of the involved nerves and/or the location of your pain.
The first place to try the electrodes is either directly over the painful area or on either side of the pain. You will slowly turn up the intensity of the unit until you feel a buzzing, tingling, or thumping sensation strong enough to override the pain signals.
If that doesn’t work, you may get better results putting the electrodes over the area where the spinal nerve root exits the vertebra. Sometimes it takes a bit of trial and error to find the right settings and best electrode placement for you.
Be sure and let your healthcare provider know if you experience increased pain. Electrodes placed below the level of a peripheral nerve impairment might actually block the input from the TENS unit and cause increased pain. Or placement over an area of scar tissue from surgery can cause increased skin resistance and decreased transmission of the electrical impulses.
Another way to use TENS is over spots in the muscles that trigger pain called trigger points (TrPs). Trigger points are areas of hyperirritability in the muscles that can cause chronic pain. The healthcare provider will identify any TrPs present during your exam. Usually TrPs are taken care of with a treatment designed to eliminate them. In some patients they are chronic and don’t go away or come back easily. In such cases, TENS may be helpful.
Your health care team will guide you through the trial-and-error process for finding the best electrode placement for you and make any changes needed in the program.
When you should NOT use TENS
1.If you have loss of skin sensation or even decreased sensation, you should not use TENS. With altered sensation, there is a risk of turning the unit up too high and causing injury or harm.
2.The use of TENS is not recommended for older adults with Alzheimer’s, dementia, or other cognitive problems.
3.If you have a cardiac pacemaker, you should not use TENS as the electrical signals could interfere with your pacemaker. Cardiac patients should not use TENS without their physician’s approval.
Some guidelines when using TENS
- Before applying the electrodes, it is important to remove all lotions, oils, or other applications to the skin. You may want to shave hair from the local area where the electrode will be applied.
- Daily use of TENS for several hours at a time is recommended. You should not wear the unit for long periods of time (e.g., 24 hours) or during extended sleep time (napping is okay but TENS should not be used while sleeping at night or for more than a couple of hours).
- Never place an electrode over an open wound or area of skin irritation. Report any skin problems or burns immediately.
- Do not place electrodes near your eyes or over your throat.
- Do not use TENS in the shower or bathtub.
- Move the electrodes a bit each time you put them on to avoid skin irritation.
- You should experience a comfortable tingling sensation that is comfortable enough to allow you to complete daily tasks and activities.
- You may want to keep a daily journal of your pain levels, the settings you use, and a record of the medications you are taking for pain relief. By reviewing your notes, you may find the best combination of electrode placement and unit settings that gives you the most pain relief.
What can you expect with TENS
You should feel a mild to moderately strong tingling or buzzing sensation. Some people experience a more unpleasant sensation described as burning or prickling. Depending on the intensity and duration of your pain, you may or may not get results right away.
It can take several days to even several weeks to get the desired results. Differences in results may occur based on properties of skin resistance, type of pain, and individual differences in the mechanism of pain control. Be patient and persistent. Do not hesitate to contact your healthcare provider as often as it takes to get the desired results.
Many patients do report good-to-excellent results, first with pain control, then pain relief, and finally reduction in the use of medications. Although it doesn’t happen for everyone, some chronic pain patients are “cured” permanently from their pain.
As each of these benefits from the TENS treatment occur, you may find yourself increasing your activity level – either with the same level of TENS usage or even with reduced frequency of use, intensity of signal, or duration (length of time the unit is turned on).
If for any reason your pain starts to increase in frequency, duration, or intensity, don’t assume the treatment isn’t working for you. First, check the TENS unit for any malfunction, need to recharge, or replace the electrodes with new ones. If your unit is battery-operated, you may find it necessary to turn the intensity up to obtain the same sensation when the batteries are low. This should alert you to the need for battery replacement.
Finally, be aware that some patients experience “breakthrough pain,” referring to a situation in which you get pain relief at first but then even with the TENS unit, you start to have pain once again. Turning the intensity up high enough to cause muscle contraction is an indication of breakthrough pain.
Sometimes a different setting for the stimulator may be needed when this happens. Most units have a setting that allows for random pulse frequency, duration, and amplitude. The use of this setting helps keep the nervous system from getting used to a specific amount of stimulation and ignoring it. This phenomenon is called habituation or adaptation.
Summary
TENS is an effective method of pain control for chronic pain when you want to maintain your normal routine of daily activities that would otherwise be hampered by too high of pain levels. TENS helps many people reduce and sometimes even eliminate the use of pain medications, thus avoiding side-effects of long-term drug use.
Even without complete pain relief, TENS makes it possible to stay active and participate in work, family, and even recreational activities. There are no significant adverse effects from the use of TENS. The ability of this treatment technique to moderate pain and reduce the use of pain medications is a real benefit — especially with the potential for serious or adverse effects from long-term use of pain relievers.
Diffuse Idiopathic Skeletal Hyperostosis
A Patient’s Guide to Diffuse Idiopathic Skeletal Hyperostosis
Introduction
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is a phenomenon that more commonly affects older males. It is associated with stiffness and back pain, but often it causes no signs or symptoms.
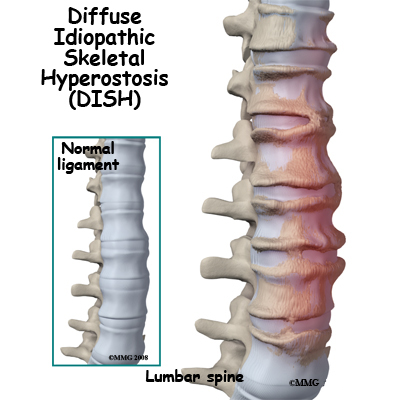
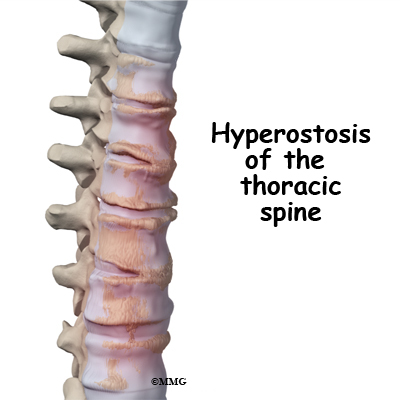
The most common finding of Diffuse Idiopathic Skeletal Hyperostosis (DISH) is ligaments that turn into bone. It is also known as Forestier’s disease, after the name of the physician who recognized it. It is most often confirmed by x-ray.
This guide will help you understand
- what parts of the spine are affected
- what causes this condition
- what does this condition feel like
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the spine are involved?
The spine, or vertebral column, is made up of bones that stack on top of one another. These bones are called vertebrae. There are five sections of the spine. At the top is the neck, or cervical spine, which connects with the skull. Below the neck is the thoracic spine or mid-back, which has the ribs attached. The ribs form your chest. Below the thoracic spine is your lumbar spine or low back. The lumbar spine attaches to the sacrum which is part of the pelvis. The last section of the spine is the coccyx, also know as the tail bone.
There are ligaments that help stabilized the spine. The ligament along the front of the spine is called the anterior longitudinal ligament. There is another ligament that attaches to the back of the spine called the posterior longitudinal ligament. These are the spinal ligaments that can turn into bone in Diffuse Idiopathic Skeletal Hyperostosis (DISH).
Causes
What causes this problem?
Diffuse Idiopathic Skeletal Hyperostosis generally occurs in people between the ages of 50 and 60. It appears more often in men than women. While the cause is unknown, there seems to be a connection with having diabetes, high blood pressure, coronary artery disease, and being over weight.
Some researchers feel that the extra bone is made because of extra blood supply near the spine. Growth factors that effect the formation of calcium likely play a role.
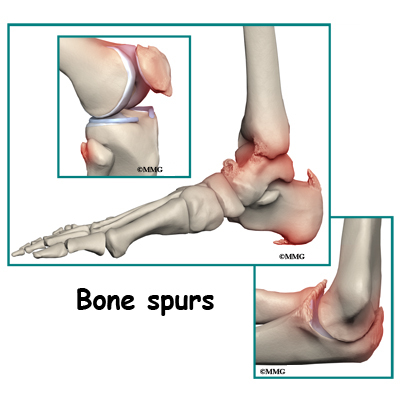
DISH generally affects the ligament in front of the spine called the anterior longitudinal ligament. This is the most common ligament that turns into bone with DISH, but it can affect other ligaments as well. Another common feature of DISH is that it can cause syndesmophytes (a bony outgrowth attached to a ligament) and tendonitis at sites other than the spine. These calcification sites can lead to bone spurs in the heels, elbows, ankles, knees, and shoulders. Bone spurs and inflammation develop where the tendon attaches to the bones.
Although DISH is considered a form of osteoarthritis, it is not considered degenerative, from wear or tear. The disc heights and facet joints do not show wear and tear as with other forms of osteoarthritis.
Medications that are used to treat acne may increase your risk of having DISH. These medications are called retinoids. They are similar to vitamin A.
Symptoms
What does the condition feel like?
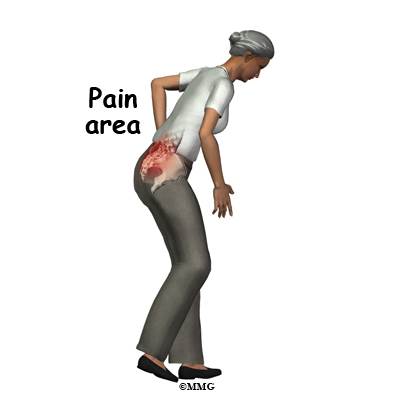
Stiffness and decreased range of motion are the most common symptoms of DISH. The stiffness usually happens in the morning upon waking. It also happens after a long period of rest. Often the decrease in motion in the spine is with side-bending. DISH most commonly affects the mid back, but can also affect the neck and low back. It also seems to affect the right side of the thoracic spine more often than the left side. Pain may be a symptom of DISH, but not always.
In addition to changes in the spine, DISH can also cause stiffness, pain, and inflammation in tendons throughout the body. When DISH affects areas other than the spine, it feels like tendonitis. Ligaments and tendons where they attach to the bone near the joints develop extra bone growth.
Difficulty swallowing (dysphagia), or a hoarse voice, can happen when people have DISH in the neck. The bone spurs can put pressure on your esophagus (tube connecting the throat with the stomach), making it difficult to swallow. The pressure can also cause a hoarse voice or difficulty in breathing. In rare cases, this can become serious. This may require surgery to remove the bone spurs.
Neurological problems are rare in DISH. In severe cases, the extra bone growth around the spine can cause problems with the spinal cord or nerves. Squeezing of the spinal cord can cause loss of feeling and paralysis.
Diagnosis
How do doctors diagnose the problem?
Your doctor will complete a history and physical examination. Your doctor will ask you questions about things such as activity, urination, bowel movements, weakness, and stiffness. Range of motion of the spine is usually evaluated, as well as tenderness of the spine or muscles next to the spine.
Neurological examination usually includes checking reflexes at the knees and ankles (elbows and wrists if your neck is involved), sensation, and muscle strength. Your doctor may ask you to walk on your heels and toes.
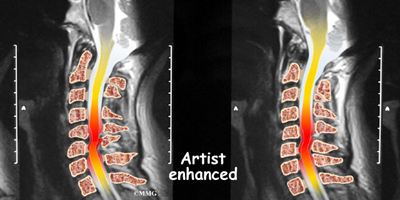
Your doctor may ask that you have x-rays of your spine, usually the mid-back. If you have signs of nerve problems, a magnetic resonance imaging (MRI) scan, or a computed tomography (CT) scan may be ordered.
The MRI allows your doctor to look at slices of the area in question. The MRI machine uses magnetic waves, not x-rays. It shows the soft tissues of the body. This includes the spinal cord, nerves, and discs. It can also show spinal bones.
Computed tomography (CT) is best for evaluating problems with the vertebral bones. It is usually tolerated well but exposes you to radiation.
Extra bone growth along the vertebral column can be identified with any of these imaging tests. The extra bone growth must involve three or more adjacent vertebrae to meet the criteria for DISH. The calcification along the spine has a very unique appearance. Some doctors call it cascading or flowing. It is also sometimes described as appearing like candle wax dripping and oozing down the spine.
Treatment
What treatment options are available?
Nonsurgical Treatment
While there is no cure for DISH, there are treatments that can help the symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) may help manage pain or tendonitis-like inflammation. Tylenol® which is also called acetaminophen may also help relieve pain. More severe pain may be treated with corticosteroid injections.
Surgery
Rarely is surgery necessary. However, if the extra bone growth compresses the spinal cord or nerve roots, surgery may be needed. Surgery is done to relieve pressure on the spinal cord or nerve roots. Surgery to take out the extra bone growth (spurs) in the neck may help with symptoms of difficulty swallowing. You should expect to be hospitalized for a brief stay. Initially you may be asked to wear a corset or brace for support.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Physical therapy may help delay the loss of motion in affected joints. Regular exercise such as walking or stretching is recommended. This helps with the stiffness and pain. Exercises help increase your range of motion in your joints. Heat may also be helpful to areas of your body affected by DISH.
After Surgery
Physical and/or occupational therapy can help you with getting in and out of bed properly, moving, walking, dressing, etc. Initially, you will not be allowed to lift more than 10 pounds. At first, using a walker may be more comfortable and safe. Gradually you will be able to return to your normal activities.
Regular exercise such as walking or stretching is recommended. This helps with the stiffness and pain. Exercises help increase your range of motion in your joints. Heat may also be helpful to areas of your body affected by DISH.
Your surgeon will want you to follow up on a regular basis. Repeat examination will include testing of the nerves and spinal cord. Imaging studies will also be repeated.
Adult Degenerative Scoliosis
A Patient’s Guide to Adult Degenerative Scoliosis
Introduction
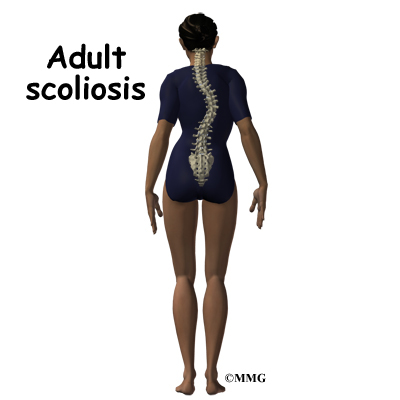
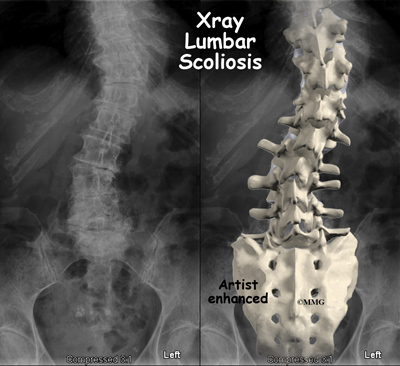
A normal healthy spine will be straight when seen from the front or the back. When seen from the side, the normal spine forms a gentle “S” curve, which is known as adult degenerative scoliosis.
Scoliosis is an abnormal or exaggerated curve of the spine from the side or from the front or back. Adult degenerative scoliosis is different from the type of scoliosis that occurs in teenagers. Adult degenerative scoliosis occurs after the spine has stopped growing and results from wear and tear of the spine. The condition most often affects the lumbar spine.
This guide will help you understand
- what parts make up the spine
- what causes adult degenerative scoliosis
- how your doctor will diagnose this condition
- what treatment options are available
Anatomy
What parts make up the spine?
The spine is made up of 24 moveable bone segments called vertebrae. The spine is divided into three distinct portions. There are seven cervical or neck vertebrae, 12 thoracic or mid-back vertebrae and five lumbar or low back vertebrae.
The spine is made up of three general parts. The top portion is the cervical spine and connects with the skull or cranium. The middle portion is the thoracic spine and is identified by the ribs that attach to each of the vertebrae. The lower portion is the lumbar spine. It connects with the pelvis at the sacrum.
The vertebra stack on top of one another and are separated by discs. The spine has normal curves. When looking at the spine from the side, the spinal column is not straight up and down, but forms an “S” curve. The cervical spine has an inward curve called a lordosis. The thoracic spine curves outward. This curve is called a kyphosis. The lumbar spine usually has an inward curve or a lordosis. The “S” curve seen in the side view allows for shock-absorption and acts as a spring when the spine is loaded with weight. This “S” curve maintains balance of the spine in a forward and backward plane.
The spinal cord travels within a canal made by the vertebra. Branching off of the spinal cord are nerve roots. These nerves then supply arm, trunk, and leg muscles for movement. They also supply muscles of organs such as the bladder.
Discs are fluid-filled cushions between the vertebrae. Facet joints are small joints in the back that allow movement. Facet joints are lined with cartilage. The cartilage is a covering of the joint surface that gives some cushion and protects the bone. It is also slippery which helps with motion.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Related Document: A Patient’s Guide to Thoracic Spine Anatomy
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
What causes adult degenerative scoliosis?
Adult degenerative scoliosis can be a result of scoliosis from childhood. The curvature may increase during adulthood and become painful. Scoliosis that happens in childhood is usually idiopathic, meaning there is no known reason for it.
Any part of the spine can be affected by scoliosis including the cervical, thoracic, or lumbar vertebrae. Most often the lumbar spine is affected. The vertebrae curve to one side and may rotate, which makes the waist, hips, or shoulders appear uneven.
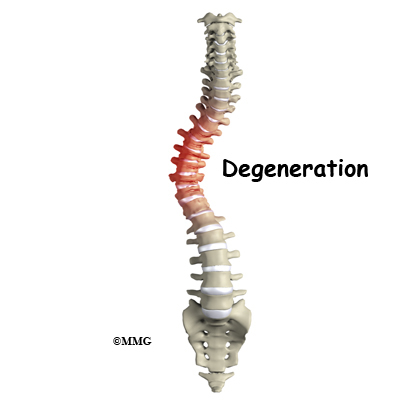
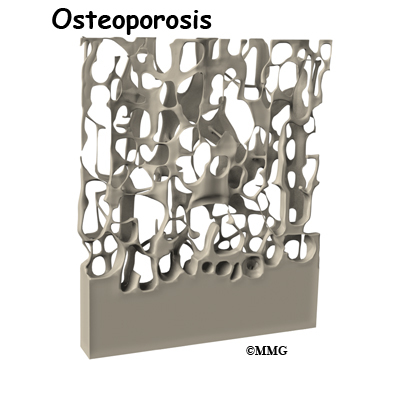
The most common cause of adult degenerative scoliosis is from degeneration, known as wear and tear. It usually occurs after the age of 40. In older women, it is often related to osteoporosis. Osteoporosis is the loss of calcium in the supporting bone. This makes the vertebrae weak.
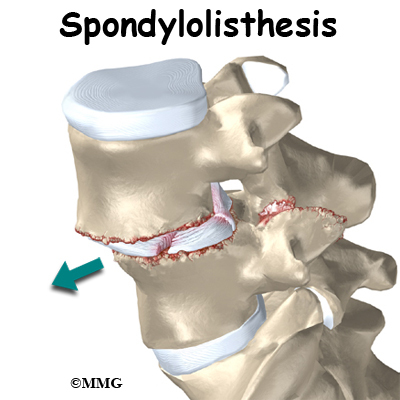
In adult degenerative scoliosis, the spine loses its structural stability and becomes unbalanced. This imbalance of the spine causes changes in the way the forces of the spine are directed. The larger the scoliotic curve becomes, the faster these changes cause degeneration of the spine. This creates a vicious cycle where increasing deformity causes more imbalance, that in turn causes more deformity. While this process occurs very slowly, it usually continues to slowly progress until something is done to restore the balance in the spine.
When there is an “S” curve when viewing the spine from the front, the condition is called scoliosis. The scoliotic deformity may also affect the normal “S” curve that the spine has when vised from the side. These curves are normal and required to maintain the proper balance of the spine. Many patients with scoliosis actually lose the normal curves of the spine.
Our body has a natural tendency to try to maintain a balance where the head is straight above the middle of the pelvis. If one leg is longer that the other, and the pelvis tilts, the spine will curve in the opposite direction to place the head above the center of the pelvis. If there is a curve in a portion of the spine, then the remainder of the spine will bend in the opposite direction to try and keep the head above the middle of the pelvis.
The scoliotic curve has a convex and concave side. The convex side is simply the outside of the curve where concave is the inside of the curve. The spine above and below the curve will tend to bend in the opposite direction in an attempt to balance the spine. Remember, the body will always try to place the head immediately above the middle of the pelvis. The concave side will tend to have more compression of the facet joints and possibly the nerve roots. This can lead to more pain from arthritis on the concave side of the curve and may lead to pain, weakness and numbness into the legs from the compressed nerve roots. These nerve changes are called radiculopathy.
In adult degenerative scoliosis, there is gradual narrowing of the discs that cushion between the vertebrae. The cartilage and joint surfaces of the facet joints in the spine can wear out, causing arthritis. This can cause back pain.
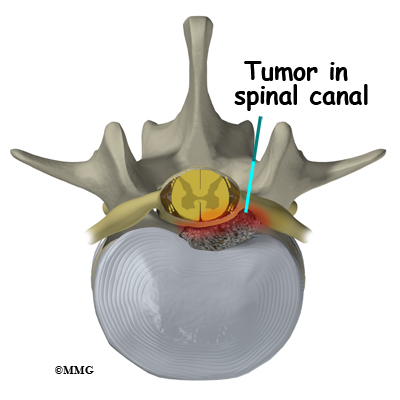
Stenosis is a term meaning narrowing. There are times when the canal for the spinal cord is narrowed. The openings for the nerve roots may also be narrowed. This will usually cause compression of the nerve structures. When the spinal cord or spinal nerves are compressed, pain, changes in feeling and/or motor function of the muscles can happen.
Sometimes spondylolisthesis occurs. This is slippage of one vertebra on the other. This can happen in adult degenerative scoliosis when the vertebrae do not stack on top of one another like they are supposed to. One vertebra may be shifted sideways, not lining up as it should. The slippage is graded from I to IV, one being mild, IV often causing neurological symptoms.
In rare and severe cases, the chest may become deformed because of scoliosis. This may affect the lungs and heart. This can lead to breathing problems, fatigue, and even heart failure.
Degenerative scoliosis is more common the older we get. As our population ages, adult scoliosis will be even more common. It will be an increasing source of deformity, pain, and disability.
Related Document: A Patient’s Guide to Scoliosis
Symptoms
What does adult degenerative scoliosis feel like?
Most people who have scoliosis will notice the deformity it can cause. There is usually a hump (rib hump) in the back. One shoulder and/or side of the pelvis may be lower than the other. You may have noticed that you have shrunk in height. You may not be able to stand up straight. For many, there is no significant pain caused by the scoliosis. Other symptoms may include:
- Decreased range of motion or stiffness in the back
- Pain involving the spine
- Stiffness and pain after prolonged sitting or standing
- Pain when lifting and carrying
- Pain may travel to areas away from the spine itself. It may cause pain in the buttocks or legs
- Spasm of the nearby muscles
- Difficulty walking
- Difficulty breathing
Diagnosis
How will my doctor know if I have adult degenerative scoliosis?
Your doctor will ask you several questions about your pain, function, what makes your pain better and worse, when it started, bowel or bladder function, motor function, and whether you have had previous surgery.
Your doctor will perform a physical examination that will include observation of your posture in standing position both sideways and from the front and back to assess for scoliosis. Mobility of your spine and hips, as well as walking ability will be evaluated.
A neurological exam that includes testing reflexes with a small rubber hammer, and testing of sensation will likely be included.
Your doctor will want to start with x-rays to measure the degree of the scoliosis. X-rays provide pictures of the alignment of the vertebra. Using a device to measure angles held up to the x-ray image, the degree of curvature of the spine can be measured. These measurements are referred to as the Cobb angles. Diagnosis of scoliosis is made when a curve measures greater than 10 degrees. X-rays can also give your doctor information about how much degeneration has occurred in the spine. They show the amount of space between the vertebrae. They can also show the degree of fusion of the spine following surgery.
If you are having pain into your leg(s), or difficulty with bowel or bladder function, your doctor will likely order a magnetic resonance imaging (MRI) scan. The MRI scan provides a better image of the soft tissues such as discs, nerves, and the spinal cord. The MRI machine uses magnetic waves rather than x-rays to show the soft tissues of the spine. The pictures show slices of the area imaged. The test does not require a needle or dye.
A computed tomography (CT) scan may be ordered. It is best for evaluating problems with the vertebral bones. It is a form of x-ray. Sometimes, it may require dye into the spinal canal fluid so that the spinal cord and nerve root anatomy is identified better. When dye is injected for this purpose, the technique is called a myelogram.
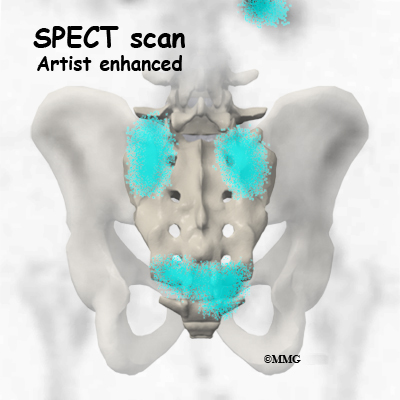
SPECT stands for Single Photon Emission Computed Tomography. It is a nuclear scan because it uses a radioactive tracer, Technetium. Technetium is injected into your vein. Where there is increase in metabolic activity, such as in the case with inflammation (arthritis), fracture, infection, or tumor the Technetium will be more concentrated.
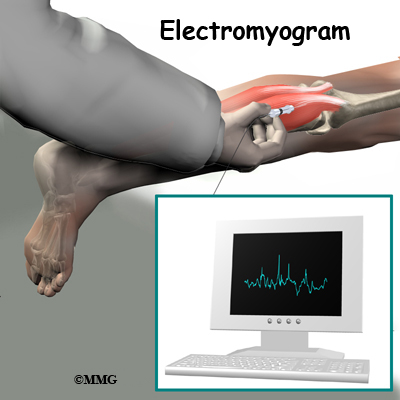
Electromyogram (EMG) and/or or nerve conduction velocity (NCV) tests are performed by the placement of small needles in extremities where there is concern about change in motor function, or sensation. By using low-level electrical current, the device measures whether or not a motor nerve is being compressed. It can also help determine the source of changes in sensation. The EMG tests the muscles to see whether they are working properly. If they aren’t, it may be because the nerve is not working well. The NCV test measures the speed of the impulses traveling along the nerve. Impulses are slowed when the nerve is compressed or constricted.
Treatment
What treatment options are available?
Most of the time treatment of adult degenerative scoliosis is conservative care, meaning non-surgical. Rarely is surgery necessary. Treatment decisions for adult degenerative scoliosis are based on how much pain you are experiencing, how much the condition is affecting your ability to function and whether or not you are having symptoms of nerve compression.
Nonsurgical Treatment
Whenever possible, doctors prefer treatment other than surgery. The first goal of nonsurgical treatment is to ease pain and other symptoms so the patient can resume and maintain normal activities as soon as possible.
Your doctor may prescribe treatment from a physical therapist. Much of the pain from adult degenerative scoliosis is the result of muscle spasm. This spams occurs when the normal muscles must work harder than normal try to restore the balance to the spine. The muscles become fatigued and begin to spasm. This causes pain.
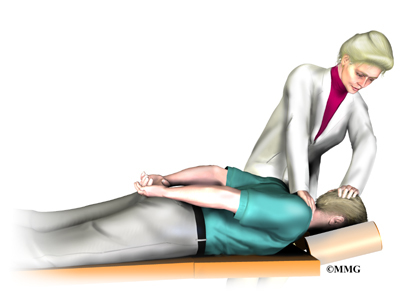
The physical therapist can help you with positions and exercises to ease these symptoms. The therapist can design an exercise program to improve flexibility of tight muscles, to strengthen the back and abdominal muscles, and to help you move safely and with less pain.
You may also be prescribed medication to help you gain better control of your symptoms so you can resume normal activity swiftly. Over-the-counter anti-inflammatory medications such as Ibuprofen or Aleve may be helpful. There are also many prescription anti-inflammatories available. Narcotic medication may be considered to make you more comfortable.
Bracing may provide some help especially when the scoliosis is painful or unstable. Braces that are made to fit may be more comfortable and effective but they are more expensive than off-the-shelf braces or supports. There are also unloading braces to help relieve pressure on the discs, nerves and joints of the spine.
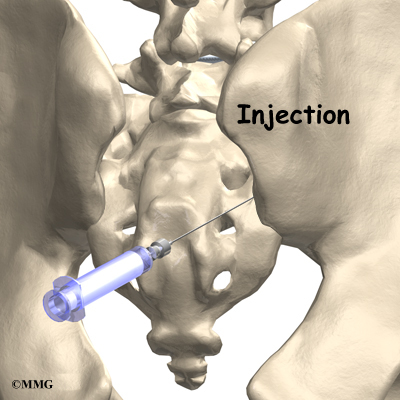
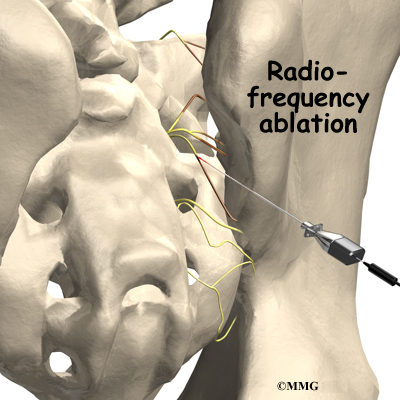
If symptoms continue to limit your ability to function normally, your doctor may suggest an injection into the spine to help with pain. Your doctor may recommend facet injections into the joints of the spine. A procedure called radiofrequency ablation may provide more lasting benefit. Epidural or transforaminal injections into the spine can also be helpful. A series of injections may be more helpful to provide temporary decrease in pain.
If you have osteoporosis, discuss with your doctor how you can optimize your treatment for this condition to slow the progression of osteoporosis. Adequately treating the osteoporosis can help reduce the progression of the scoliosis.
Related Document: A Patient’s Guide to Epidural Steroid Injections
Related Document: A Patient’s Guide to Facet Joint Injections
Related Document: A Patient’s Guide to Radiofrequency Ablation
Surgery
Surgery is usually considered when non-surgical treatments have not provided enough relief from pain – or when the nerves of the spine are being damaged. Surgery is more common when the curvature is continuing to increase and the imbalance of the spine is clearly getting worse. Surgery to correct adult degenerative scoliosis is both complex and difficult. Most surgeons would not suggest surgical intervention except as a last resort when all conservative measures have failed and the pain is intolerable.
Adult degenerative scoliosis is a disease of older people. As a result, the overall health of the individual is important when making decisions about whether or not to consider surgery. Other illnesses, such as heart disease, lung disease or diabetes, may increase the risk of medical complications either during or after the operation and make surgery too risky.
Surgeons must consider the quality of the bone of the spine as well. Older individuals are more likely to have some degree of osteoporosis. This makes the bone weaker. Weaker bone may not be able to hold the instrumentation, the rods and screws necessary to correct the spine. If the bone weakened by osteoporosis cannot hold the screws necessary to hold the spine aligned as it fuses, this can lead to failure of the entire operation.
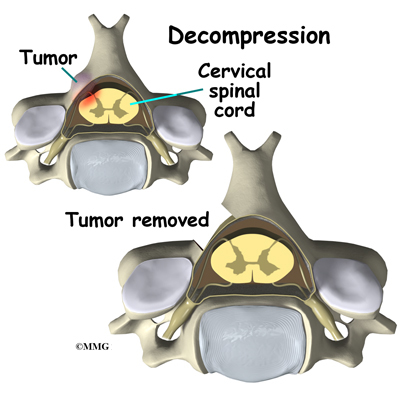
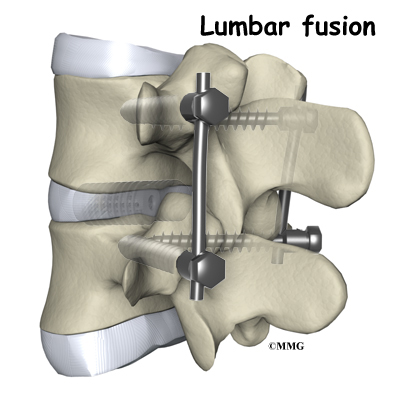
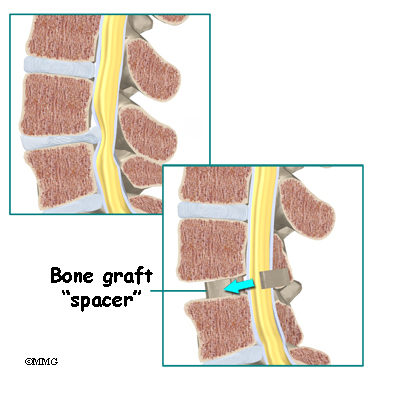
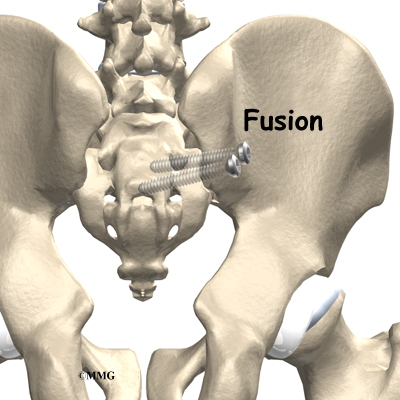
The goal of surgery is to improve the balance of the spine and remove pressure on any of the nerves of the spine. Surgery to relieve pressure on the nerves is called a decompression. Surgery to reinforce the area that is unstable is called a fusion. To accomplish the goals of the surgery requires several steps.
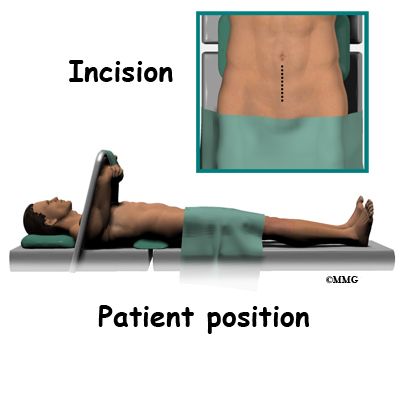
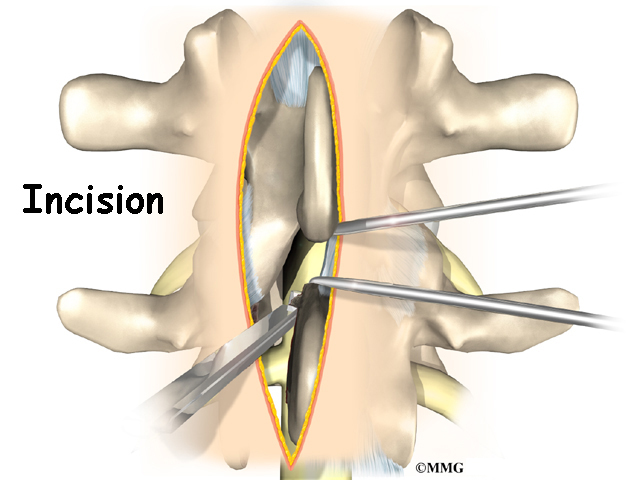
First, the surgeon must be able to adequately see the area of spine to be corrected. This is called the exposure. The surgery usually requires an incision in the back. In some cases, surgery will also need to be performed on the front of the spine. This may require an incision in the abdomen or from the side of the body to allow the surgeon to reach the front of the spine. Sometimes a combination of both is necessary.
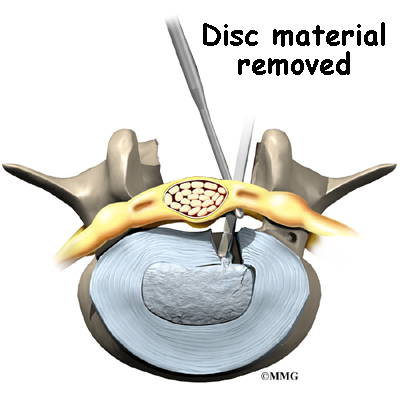
Next, the surgeon must perform a decompression so that all nerves are free of any pressure. This is accomplished by removing any bone spurs or disc material that is causing pressure on the spinal nerves.
The surgeon must then mobilize the spine. Usually after the decompression is finished, the spine is mobilized a great deal. Removing bone spurs and disc material also loosens the contracted scar tissue around the spine and allows the surgeon to straighten the spine back toward normal.
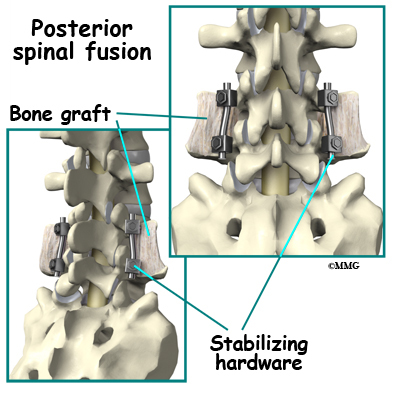
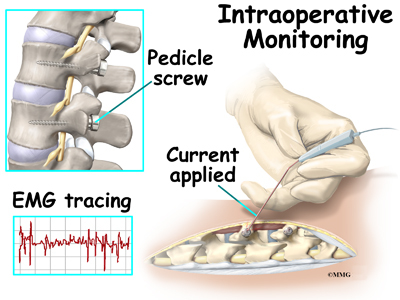
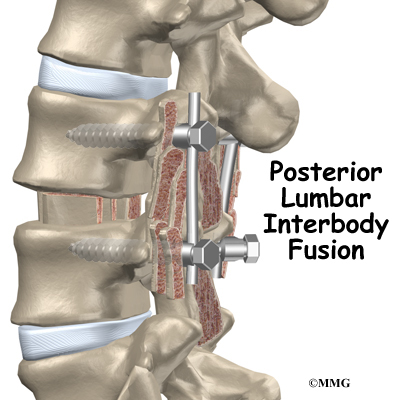
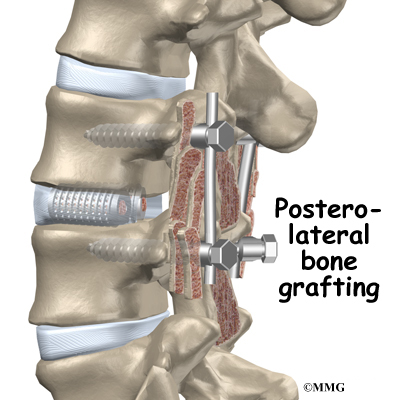
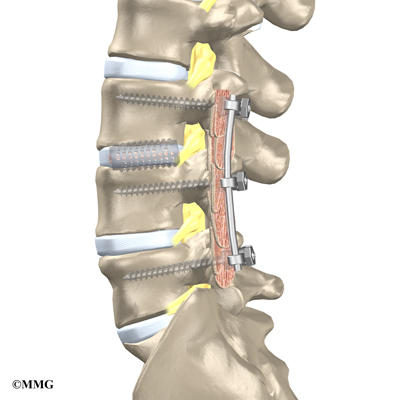
Finally, the surgeon must insert the screws and rods that will hold the spine in the new position while the fusion occurs. Two special screws called pedicle screws are inserted into each vertebra. These special screws are then attached to metal rods that hold the vertebrae in alignment.
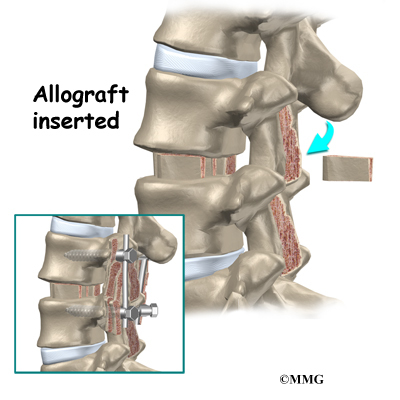
Bone graft is placed between each vertebra. This bone graft will form a solid bone bridge between each vertebra and allow the spine to grow together – or fuse. The combination of the pedicle screws and the metal rods is called the instrumentation. This instrumentation forms the strut that will hold the spine in the correct alignment until the spine fuses.
Once the spine has fused, it will remain in the balanced position. The instrumentation is no longer really necessary, as the fused bone of the spine is now what is keeping the spine from collapsing again. The instrumentation is rarely removed and only removed when it is causing a problem. Restoring balance to the spine should decrease pain and reduce the risk of future problems.
Related Document: A Patient’s Guide to Posterior Lumbar Fusion
Rehabilitation
What can I expect during recovery and treatment?
Nonsurgical Rehabilitation
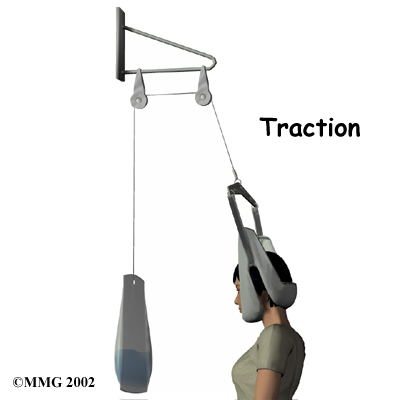
Physical therapy is important for strengthening muscles of the spine, abdomen, hip girdle, and legs. Stretching of certain muscles may also be recommended. Stretching or traction applied to the sides of the curve is sometimes used by physical therapists and chiropractors. Exercises must be done on a regular, ongoing basis. It may be possible to improve posture and motion.
Your physical therapist may be instructed by your physician to place a battery operated electrical device (TENS unit) over the area of pain. This reduces painful input to the brain from your back.
Traction devices may be tried by your physical therapist or chiropractor. These are often available for home use.
Muscle stimulators are battery-powered electrical devices that cause muscle contraction. The electrodes or patches are placed over a muscle such as along the spine. There are wires that then attach the electrodes to the device. The current is given for a limited period of time, controlled by a timer. This can help train the muscles to contract on their own.
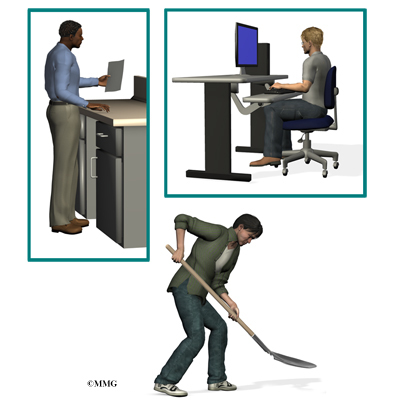
Activity modification such as limited lifting or avoidance of prolonged sitting or standing may be helpful. Occasional use of a cane or walker to improve walking tolerance may be recommended.
Use of ice or heat may prove beneficial. Your doctor or physical therapist can provide you with guidelines.
Your physical therapist may advise you to participate in weight bearing exercises to help strengthen your bones and muscles. These may include activities such as walking, toning with the use of weights or other resistance, and tai chi.
After Surgery
If surgery was necessary for your adult scoliosis you will likely be hospitalized for several days following surgery. Some patients prefer to extend their stay in a transitional care unit in the hospital, or even a skilled nursing facility (nursing home).
Your surgeon may suggest a brace following surgery, to ensure that you do not bend too far and to support your spine.
You will be allowed to get in and out of bed and walk shortly after surgery. Lifting is usually limited during the initial recovery period. You will gradually be allowed to resume your usual activities after several weeks or months.
It may be recommended that you have physical and occupational therapy after your surgery to help you regain strength and independence with daily activity. They also will help you with activity modification. They can recommend equipment for use in your home that may be helpful.
Your surgeon will want to see you periodically to monitor your progress. Repeat imaging with X-ray, MRI or CT scan is usually done to follow the progress of your spine as it heals.
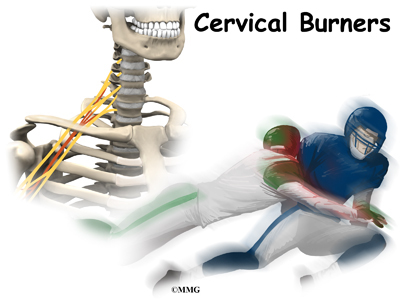
Cervical Burners and Stingers (Brachial Plexus Injuries)
A Patient’s Guide to Burners and Stingers (Brachial Plexus Injuries)
Introduction
Injury to the nerves of the neck and shoulder that cause a burning or stinging feeling are called burners or stingers. Another name for this type of nerve injury is brachial plexus injury. Football players are affected most often. Up to half of all college football players have had at least one burner or stinger. Many of these occurred during high school football. Fortunately, it’s not a serious neck injury.
This guide will help you understand
- what parts of the body are involved
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the body are involved?
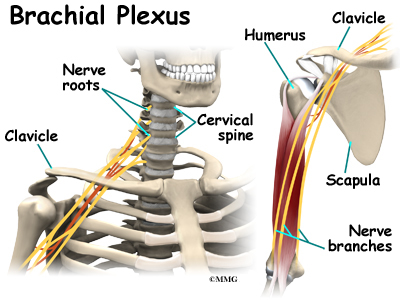
The brachial plexus is affected most often by a downward or backward force against the shoulder. A nerve plexus is an area where nerves branch and rejoin. The brachial plexus is a group of nerves in the cervical spine from C5 to C8-T1. This includes the lower half of the cervical nerve roots and the nerve root from the first thoracic vertebra.
The nerves leave the spinal cord, go through the neck, under the clavicle
(collar bone) and armpit, and then down the arm.
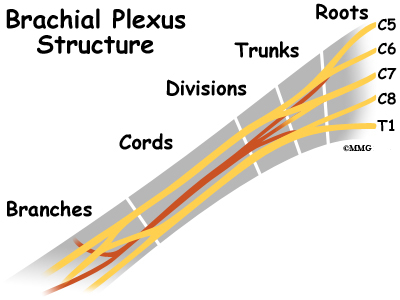
The brachial plexus begins with five roots that merge or join together to form three trunks. The three trunks are upper (C5-C6), middle (C7), and lower (C8-T1). Each trunk then splits in two, to form six divisions. These divisions then regroup to become three cords (posterior, lateral, and medial).
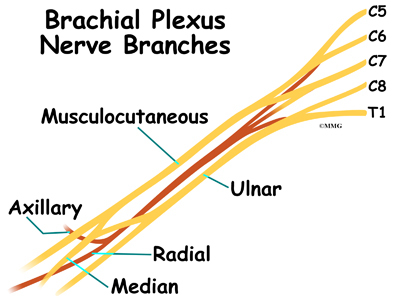
Finally, there are branches that result in three nerves to the skin and muscles of the arm and hand: the median, ulnar, and radial nerves.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
Burners or stingers are the result of traction or compressive forces on the brachial plexus or cervical nerve roots. The usual mechanism of injury occurs when a direct blow or hard hit to the top of your shoulder pushes it down at the same time your head is forced to the opposite side.
In the process, the brachial plexus between the neck and shoulder gets stretched. The same injury can happen if a downward force hits the collarbone directly. In football, burners or stingers occur most often when you tackle or block another player. This motion overstretches the nerves of the brachial plexus.
It’s not clear exactly where in the brachial plexus the damage occurs. Some experts suggest the injury is most likely to be at the level of the trunks, rather than at the nerve root level. The results of other studies show that burners or stingers from compression forces cause nerve root damage while traction injuries result in plexus injuries. A nerve root injury would be much more serious than a burner or stinger from a trunk injury of the brachial plexus.
Other athletes who participate in wrestling, gymnastics, snow skiing, and martial arts can also experience burners or stingers. Some studies suggest that athletes with a narrow cervical canal may be at increased risk for this type of injury.
Symptoms
What does this condition feel like?
A burning or stinging feeling between the neck and shoulder is the hallmark finding in this condition. True neck pain is more likely to be an injury to the neck itself. With burners or stingers, the painful symptoms start above the shoulder and go down the arm and even into the hand.
The shoulder and arm may feel numb or weak. You may feel as if this area is tingling. Weakness may be present at the time of the injury. Some patients report the arm feels and appears to be “dead”. This paralysis and other symptoms may be transient or temporary. They may only last a few seconds or minutes. But for some patients, healing takes days or weeks. In rare cases, the damage can be permanent.
Diagnosis
How do doctors diagnose this condition?
A careful history and physical exam are needed to diagnose stingers or burners. By assessing areas of weakness, the examiner may be able to tell whether a stretch injury of the brachial plexus has occurred. Nerve function and reflexes are also evaluated. If the physician suspects a cervical spine injury, further testing may be needed.
X-rays, MRI, and electrodiagnostic studies such as an electromyogram (EMG) can help make the final diagnosis. The EMG will confirm a problem, pinpoint the area of damage, and give an idea of how long recovery will take for each individual.
Treatment
What treatment options are available?
Nonsurgical Treatment
Protecting the neck with a soft collar is the first step in the acute phase of burners or stingers. If the injury occurs on the playing field, the player is placed in a protective collar before being moved off the field. This is worn until X-rays are taken to rule out fracture, dislocation, or other more serious neck injury.
Rest and gentle neck and shoulder range of motion are advised until symptoms resolve. If this does not occur within a few days, then physical therapy may be needed. Your therapist will use modalities such as biofeedback, electrical nerve stimulation, and manual therapy to help restore the natural function of the nerves.
Range of motion and strengthening exercises will be added as tolerated. Posture is very important during the healing phase. A chest-out position helps open the spinal canal, thus giving more room for the spinal cord. This posture also decreases pressure on the nerve roots. Your therapist will provide sport-specific therapy when the symptoms resolve (go away).
Surgery
Surgery is not a treatment option for burners or stingers. Management remains conservative (nonsurgical). Patients are followed through the athletic season until recovery is complete.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Burners and stingers are self-limiting. This means that with treatment, they will resolve over time. You will likely be able to return to full sports participation when you no longer have any symptoms. Full neck and shoulder motion must be present. And you should be able to participate in practice without any problems before entering a game.
It is possible to get another burner or stinger but it could be something more serious. If you experience these types of symptoms again, slowly lie down on the ground. Wait for the team trainer or physician to examine you before moving your head and neck.
Some football players choose to wear extra padding, special shoulder pads, or a neck roll to protect the neck and avoid reinjury. All equipment should be in good condition and fit properly. Daily stretching of the neck is advised. Players should avoid using spearing or head tackling, which has been prohibited since 1979.
Dropped Head Syndrome
A Patient’s Guide to Dropped Head Syndrome
Introduction
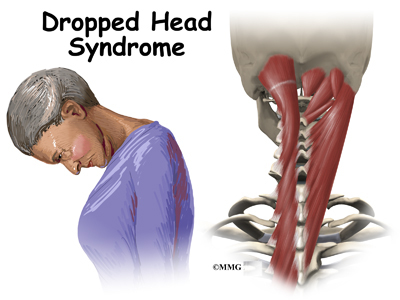
Dropped Head Syndrome is characterized by severe weakness of the muscles of the back of the neck. This causes the chin to rest on the chest in standing or sitting. Floppy Head Syndrome and Head Ptosis are other names used to describe the syndrome.
Most of the time, Dropped Head Syndrome is caused by a specific generalized neuromuscular diagnosis. When the cause is not known, it is called isolated neck extensor myopathy, or INEM.
This guide will help you understand
- what parts make up the cervical spine
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts make up the cervical spine?
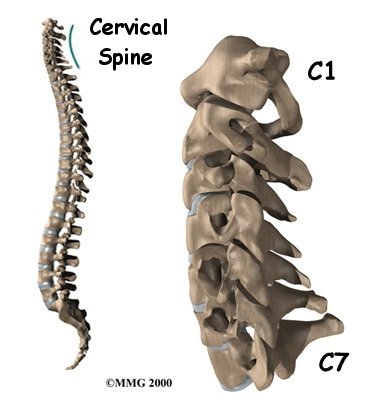
The spine is made up of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord. The spinal cord is a made up of nerve cells which grow to look like a rope or cord about one half inch in diameter. The spinal cord attaches to the base of the brain. The base of the brain is called the
brainstem.
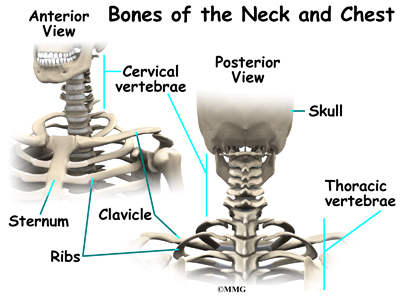
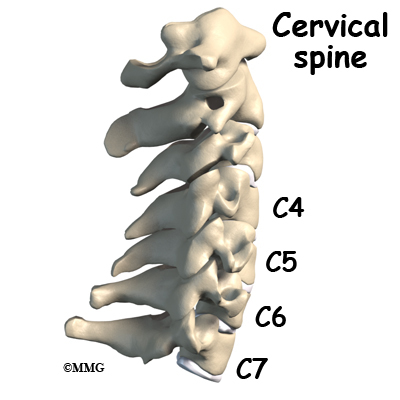
The vertebral column is divided into three distinct portions. The cervical, or neck portion attaches to the base of the skull at the upper end. The lower end of the cervical portion connects with the thoracic spine. There are seven cervical vertebrae.
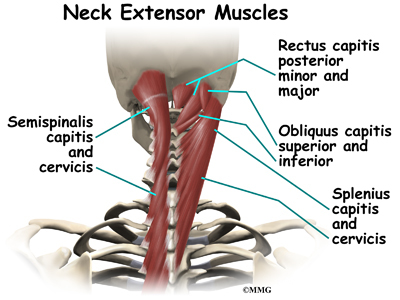
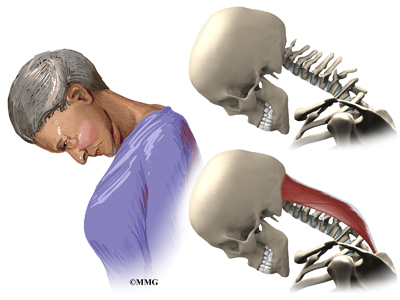
There are many muscles that lie in the neck region. Some attach from the base of the skull, others to the spine, ribs, collar bone, and shoulder blade. Extension of the neck happens when the top of the head tilts backward. This causes the face and eyes to look up. Flexion of the neck is when the top of the head tilts forward. This causes the eyes to look down. It also lowers the chin to the chest.
The vertebrae stack on top of one another. When looking at the spine from the side, or from the sagittal view, the vertebral column is not straight up and down, but forms an “S” curve. The cervical spine has an inward curve called a lordosis. The thoracic spine curves outward. This curve is called a kyphosis. The lumbar spine usually has an inward curve or a lordosis. The “S” curve seen in the sagittal or side view allows for shock-absorption and acts as a spring when the spine is loaded with weight.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
Most of the time, Dropped Head Syndrome is caused by a specific generalized neuromuscular diagnosis. These include amyotrophic lateral sclerosis (ALS) also known as Lou Gehrig’s disease, Parkinson’s disease, myasthenia gravis, polymyositis, and genetic myopathies. Other specific causes can include motor neuron disease, hypothyroidism, disorders of the spine, and cancer.
When the cause of Dropped Head Syndrome is not known, it is called isolated neck extensor myopathy, or INEM.
The INEM form of Dropped Head Syndrome usually happens in older persons. The weakness of the muscles in the back of the neck usually occurs gradually over one week to three months.
Symptoms
What does the condition feel like?
The symptoms of dropped head syndrome are usually painless. It most often occurs in the elderly. The weakness is limited to the muscles that extend the neck. Dropped Head Syndrome usually develops over a period of one week to three months. The head is then tilted downward. Because of the weakness of the extensors of the neck, the chin rests on the chest. Lifting or raising the head in sitting or standing is impossible. When lying down however, the neck is able to extend.
Gaze is down at the floor, instead of forward. The face is downward. The neck appears elongated, and the curve at the base of the neck is accentuated. This can cause over stretching or pinching of the spinal cord. When this happens, there may be weakness and numbness of the arms or entire body.
Dropped head syndrome can also cause difficulty swallowing, speaking, and breathing.
Diagnosis
How will my doctor diagnose this condition?
Diagnosis begins with a complete history and physical exam. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities.
Your doctor will do a physical examination to test your reflexes, skin sensation, muscle strength.
Most of the time, loss of of neck extension occurs as part of a more generalized neurological disorder. Neurological conditions must be considered first because some are treatable. A neurologist will usually be involved to help decide what is causing the chin-on-chest deformity.
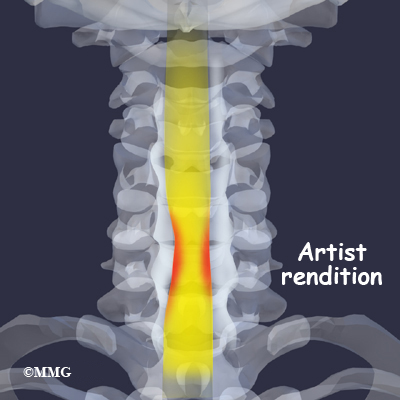
Your doctor will likely ask that you have magnetic resonance imaging (MRI) of your neck. The MRI machine uses magnetic waves rather than X-rays. It shows the anatomy of the neck. It is very good at showing the spinal cord and nerves. The test does not require a dye or a needle.
Electromygraphy (EMG) uses small diameter needles in the muscle belly being tested. It helps determine how well the nerve conducts signals to the muscles.
A muscle biopsy may be needed. A small piece of muscle is removed and examined under a microscope. A closer look at the muscle fibers can be helpful in making a diagnosis.
In isolated neck extensor myopathy (INEM), the muscle biopsy is non-specific. EMG shows some myopathic changes. Labs are normal.
If no other associated neurologic disorders are found, then the diagnosis of isolated neck extensor myopathy (INEM) is made. It is a diagnosis of exclusion, meaning that everything else that could caused it has been ruled out. It is not known what causes isolated neck extensor myopathy (INEM).
Some doctors feel that isolated neck extensor myopathy (INEM) is caused by either a non-specific non-inflammatory or inflammatory response that is restricted to the neck extensor muscles. Another possible cause is thoracic kyphosis. When the natural curve of the thoracic spine is increased, it may place the extensor muscles at a disadvantage given the weight of the head. This may cause over stretching and weakness of the extensor muscles.
Treatment
What treatment options are available?
Isolated neck extensor myopathy (INEM) is considered benign because it does not spread or get worse. Symptoms can improve in some cases. It is most often treated conservatively.
Nonsurgical Treatment
Treatment of Dropped Head Syndrome is mainly supportive. The weakness remains localized to the neck extensor muscles, physical therapy may help with this. There are some cases that improve dramatically, but most usually do not improve.
The most useful treatment is use of a neck collar. It can partially correct the chin-on-chest deformity. This improves the forward gaze and activities of daily living. It also can help prevent contractures of the neck in a fixed flexed posture. However, it can be uncomfortable and cause sores under the chin. Some use a baseball cap attached to straps around the trunk. This avoids the chin discomfort from using a collar.
Prednisone is a potent anti-inflammatory that may be prescribed. It may be beneficial when there is local myositis, or inflammation of the muscles. It can be taken in a pill form by mouth or intravenously.
Surgery
Unless fusion is necessary, surgery is usually not recommended in Dropped Head Syndrome.
When there is damage to the nerves in the neck or spinal cord, surgery to fuse the neck may be necessary. This usually requires a fusion from C2-T2. The loss of neck movement after fusion leaves patients unable to see the ground in front of their feet. This makes them at greater risk for falls. The inconvenience caused by having a rigid neck may prove to be a greater problem than the original dropped head deformity.
Osteoporosis, particularly in older females also poses a problem with surgery. The soft bone may allow the metal used to stabilize the spine to pull out.
Rehabilitation
What should I expect as I after treatment?
Nonsurgical Rehabilitation
Physical therapy is usually recommended. Neck extension strengthening exercises may provide some improvement. However, most patients will find the strengthening both tiring and frustrating. When lying down on your back you can move the neck to maintain range of motion. This helps to avoid unnecessary stiffness and shortening of the muscles in the front of the neck.
Range of motion exercises should be done on an ongoing basis to avoid contractures of the neck. Wearing a neck collar when up will likely improve activities of daily living.
Speech therapy may be recommended for swallowing, feeding, and breathing problems. Some people may need to have a feeding tube inserted through the stomach.
Your doctor may want to repeat imaging of the spine. There is the possibility of over stretching or pinching the spinal cord when the neck extensors are so weak. You will need to watch for symptoms such as weakness or numbness in the arms or other portions of the body. Bowel and bladder function could become a problem.
After Surgery
If surgery is recommended, you will probably require an overnight hospital stay or a few days stay. Initially, you will not be allowed to lift, and you will have to move carefully. Most likely your neck will be placed in a fairly rigid brace. You will eventually be able to resume your normal activities. You can expect healing of the fusion in three to nine months.
Physical therapy is usually recommended after surgery. Neck extension strengthening exercises are prescribed to prevent contracture of the neck. Occupational therapy may be recommended to help with arm strengthening. It can also help with dressing, and other activities of daily living. Equipment needs can be evaluated by the occupational therapist. Speech therapy may also be recommended after surgery.
Your surgeon will want to follow up with you on a regular basis. Imaging studies may need to be repeated on occasion. Assessment of the fusion is usually done with X-rays.
Treatment Guidelines for Low Back Pain
A Patient’s Guide to Treatment Guidelines for Low Back Pain
Introduction
In the United States low back pain is ranked number five among the most common reasons for physician office visits. Of the patients who get medical care, they usually improve rapidly in the first month. However, up to one-third of patients report chronic back pain of at least moderate severity.
Many diagnostic tests and treatments have been tried for low back pain. Many things may be suggested, but have little evidence to show their worth. Diagnostic tests and treatments for low back pain can also be costly. In 1998, it is estimated that 26.3 million dollars were spent in the U.S. On health care for low back pain.
What to do about back pain can be confusing for both you and your provider. The American College of Physicians (ACP) and the American Pain Society (APS) recently had a panel review and analyzed available research on acute and chronic low back pain in adults.
The panel’s recommendations were considered proven only when they were supported by at least fair-quality evidence. They also had to have at least moderate benefits. Some were considered proven even with small benefits if there were no significant harms, costs, or burdens.
This guide will give you a general overview of the newly recommended
guidelines for the evaluation, diagnosis, and treatment of acute and chronic low back pain in adults.
This guide will help you understand
- how your doctor will evaluate your low back pain
- what diagnostic tests are recommended
- what treatment options are recommended based on evidence
Recommendation 1:
Clinicians should conduct a focused history and physical examination to help place patients with low back pain into 1 of 3 broad categories: nonspecific low back pain, back pain potentially associated with radiculopathy or spinal stenosis, or back pain potentially associated with another specific spinal cause. The history should include assessment of psychosocial risk factors, which predict risk for chronic disabling back pain (strong recommendation, moderate-quality evidence).1
Your doctor will want to do a history and physical examination to determine if there is a specific reason for your low back pain. It is important for your doctor to determine if there is neurologic (nerve) involvement. Your back pain can then be placed into one of three categories:
- non-specific back pain
- back pain with radiculopathy (leg pain)
- back pain from another specific source (fracture, infection, tumor, etc.)
The most common category is non-specific back pain. This means that the cause of the pain is unknown. More than 85% of patients evaluated in the primary care setting with low back pain have non-specific low back pain. This means there are no findings of a specific disease or spinal abnormality.
Another category is back pain with leg pain. Leg pain is called radiculopathy or sciatica. This may be caused by a problem with a disc between the bones of the spine. Discs may be torn (annular tear), bulged (protruded), or ruptured (herniated). Leg pain can also be caused by stenosis. Stenosis happens when the hollowed out portion of the bones of the spine become narrowed. The spinal cord lies in the hollowed out portion. When it becomes narrow, the spinal cord can become pinched. Stenosis can also happen when there is narrowing of the opening for the nerve root. The nerve root branches off the spinal cord.
Other specific spinal causes of low back pain include fracture, infection, tumor, cancer, and inflammatory arthritis.
Spinal cord and nerve function can be evaluated in several ways. Straight leg raise (SLR) test is when your doctor lifts your leg up while the knee is kept straight. This can be useful in diagnosing a herniated disc. Your doctor will want to check the strength of various muscles in the legs. Reflexes at the knees and ankles should be evaluated also. Sensation of the leg also evaluates nerve function.
Other signs that there may be a neurological problem include loss of bowel or bladder function.
Your doctor will ask questions about the possibility of low back pain that comes from problems outside the back. Sometimes pain is from the pancreas, kidneys, or bulging of the large blood vessel in the abdomen called the aorta. Your doctor will also want to know about risk factors for cancer and infection.
Your doctor will ask about any problems with your mood, stress, or problems at home or on the job. Psychosocial factors are known to make your back pain worse, or interfere with your back pain getting better. These include depression, passive coping strategies, job dissatisfaction, disputed compensation claims, and being overly focused on physical symptoms. These problems can predict the course of low back pain even more so than findings on the physical exam, or the severity of your pain.
Recommendation 2:
Clinicians should not routinely obtain imaging or other diagnostic tests in patients with nonspecific low back pain (strong recommendation, moderate-quality evidence).1
There is no evidence that routine plain x-rays in patients with nonspecific low back pain improve patient outcomes. They subject you to a significant amount of radiation. The amount of radiation to reproductive (sperm and egg) cells from two views of the lumbar spine is equivalent to being exposed to a daily chest x-ray for more than one year.
Plain x-rays are recommended when there is the possibility of compression fracture of the vertebra bone. High-risk patients are those with a history of osteoporosis or steroid use.
Your doctor may want you to have imaging when nonspecific low back pain (without symptoms of radiculopathy or spinal stenosis) becomes persistent (lasting more than four to eight weeks). There is no optimal evidence to make a recommendation as to which imaging study is most useful in this case.
Recommendation 3:
Clinicians should perform diagnostic imaging and testing for patients with low back pain when severe or progressive neurologic deficits are present or when serious underlying conditions are suspected on the basis of history and physical examination (strong recommendation, moderate-quality evidence).1
Neurologic deficits or the suspicion of a serious underlying condition such as cancer or infection merit a prompt work-up with Magnetic Resonance Imaging (MRI) or Computed Tomography (CT). Delayed diagnosis is linked to worse outcomes.
MRI allows your doctor to look at slices of the area in question. The MRI machine uses magnetic waves, not x-rays to show the soft tissues of the body. This includes the spinal cord, nerves, and discs. It can also evaluate spinal bones. The test may require that a dye be injected intravenously (through a vein).
CT scans are a form of x-ray. MRIs are generally preferred over CTs since it does not use radiation.
If you have risk factors for cancer, the recommendations are for either x-rays, blood work to measure erythrocyte sedimentation rate (ESR), or an MRI.
Recommendation 4:
Clinicians should evaluate patients with persistent low back pain and signs or symptoms of radiculopathy or spinal stenosis with MRI (preferred) or CT only if they are potential candidates for surgery or epidural steroid injection (strong recommendation, moderate-quality evidence).1
Most patients with lumbar disc herniations with radiculopathy improve with noninvasive therapy (treatments other than spinal injections or surgery) within the first four weeks.
If symptoms of radiculopathy become persistent after noninvasive therapies, the panel recommends surgical removal of the disc or epidural steroid injections as possible treatment options. Surgery is also a treatment option for spinal stenosis with persistent symptoms.
Recommendation 5:
Clinicians should provide patients with evidence-based information on low back pain with regard to their expected course, advise patients to remain active, and provide information about effective self-care options (strong recommendation, moderate-quality evidence).1
Your doctor should inform you that an acute episode of low back pain with or without radiculopathy or sciatica should more than likely improve in the first month.
The evidence shows that staying active is more effective than resting in bed. Return to normal activities as soon as possible should be encouraged. Self-care education books are inexpensive and have shown to be helpful. Their benefits are similar to costlier therapies such as supervised exercise, acupuncture, massage, and spinal manipulation.
The panel authors did not find sufficient evidence to guide specific recommendations about modified work on the job. Factors to consider are your age, general health, and physical demands of your required job tasks.
Use of heating pads may provide short-term relief of acute low back pain. There is not adequate evidence to recommend lumbar supports and cold packs.
Recommendation 6:
For patients with low back pain, clinicians should consider the use of medications with proven benefits in conjunction with back care information and self-care. Clinicians should assess severity of baseline pain and functional deficits, potential benefits, risks, and relative lack of long-term efficacy and safety data before initiating therapy (strong recommendation, moderate-quality evidence). For most patients, first-line medication options are acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs).1
Medications from several classes have been shown to have moderate, mostly short-term benefits for patients with low back pain.
Acetaminophen (Tylenol®) is a slightly weaker pain medication than non-steroidal anti-inflammatories (NSAIDs). However, acetaminophen is generally safer and less costly. Acetaminophen can cause liver enzyme elevations at dosages of 4 g (4,000 mg)/day even in healthy adults. The clinical significance of the liver enzyme elevation is uncertain.
NSAIDs can be selective, or non-selective. Advil® and Motrin® (ibuprofen); and Aleve® (naproxen) are examples of over-the-counter non-selective NSAIDs. Celebrex® is the only selective NSAID available in the United States. Nonselective NSAIDs, while more effective than acetaminophen, are known to cause stomach and kidney problems. Selective NSAIDs such as Celebrex® and most non-selective NSAIDS also increase risk for heart attack. The lowest effective doses for the shortest periods necessary are recommended. If you benefit from nonselective NSAIDs, taking a medication to protect the stomach lining may be beneficial and more cost-effective than a selective NSAID. It was also recommended that doctors remain alert for new evidence about the safety of NSAIDs. There is not enough evidence to recommend for or against aspirin to treat low back pain.
When used carefully opioid analgesics (Tramadol) are an option in the management of acute or chronic severe, disabling low back pain. Potential risks such as addiction and abuse should be considered before starting them. There is not enough evidence to recommend one opioid over another.
Skeletal muscle relaxants may provide short term relief of acute low back pain. There is no convincing evidence that skeletal muscle relaxants differ in effectiveness or safety. Sedation can be a problem with any of the muscle relaxants.
Tricyclic antidepressants such as Pamelor® have demonstrated effectiveness in the management of chronic low back pain. Selective serotonin reuptake inhibitors (SSRIs) such as Prozac®, Zoloft®, Celexa® and Lexapro®, and trazodone have not shown that they are effective for low back pain. Serotonin-norepinephrine reuptake inhibitors (SNRIs) have not yet been evaluated for low back pain. Since depression is common in patients with chronic low back pain, it should be properly treated.
Small, short-term benefits for the treatment of leg pain or radiculopathy have been found with gabapentin (Neurontin®). There is not adequate evidence to recommend for or against other similar drugs for radiculopathy.
Benzodiazepines such as Valium® (diazepam) provide short-term pain relief for acute or chronic low back pain. However, they can be abused, cause addiction, and require more of them to get the same result. When benzodiazepines are used, a time-limited course is recommended.
Herbal therapies including devil’s claw, willow bark, and capsicum seem to be safe options for acute exacerbations of chronic low back pain.
Systemic corticosteroids have not been shown to be helpful in the treatment of low back pain with or without sciatica.
Overall, evidence is limited on the benefits and risks when medications are used long-term for low back pain.
Recommendation 7:
For patients who do not improve with self-care options, clinicians should consider the addition of nonpharmacologic therapy with proven benefits for acute low back pain, spinal manipulation; for chronic or subacute low back pain, intensive interdisciplinary rehabilitation, exercise therapy, acupuncture, massage therapy, spinal manipulation, yoga, cognitive-behavioral therapy, or progressive relaxation (weak recommendation, moderate-quality evidence).1
Spinal manipulation may provide small to moderate short-term benefits for acute low back pain. Supervised exercise therapy, home exercise regimens, and other non-medication treatments have not been proven to be effective for acute low back pain.
For subacute low back pain (lasting four to eight weeks), intensive interdisciplinary rehabilitation is moderately effective. This usually includes the services of a physician, psychologist, physical therapist, social worker, or vocational counselor. Active physical therapy to restore function and a form of psychological treatment called cognitive-behavioral therapy (CBT) are shown to reduce time off work due to low back pain.
For chronic low back pain there are non-medication treatments with fair to good supporting evidence and moderate benefit. These include acupuncture, massage therapy, and Viniyoga-style yoga. Exercise therapy has also shown fair to good supporting evidence. This includes individualized, supervised stretching, and strengthening therapy. Cognitive-behavioral therapy (CBT) or progressive relaxation, spinal manipulation, and intensive interdisciplinary rehabilitation have also shown moderate benefit. Short-term benefits may be obtained with back schools, but the evidence is inconsistent.
Transcutaneous electrical nerve stimulation (TENS) and intermittent or continuous traction have not been proven effective for chronic low back pain. There is insufficient evidence to recommend interferential therapy, low-level laser, shortwave diathermy, or ultrasound for chronic low back pain.
Lastly, the panel recommends that patient expectations of benefit from a treatment be considered when choosing therapies. They found that this seems to positively influence outcomes.
1. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of Internal Medicine 2007. Vol. 147, No. 7. Pp. 478–491.
Sacral Insufficiency Fractures
A Patient’s Guide to Sacral Insufficiency Fractures
Introduction
The sacrum is a wedge shaped bone that makes up part of the pelvis. It transmits the weight of the body to the pelvic girdle. As the name suggests, sacral insufficiency fractures occur when the quality of the sacral bone has become insufficient to handle the stress of weight bearing. The bone has lost some of its supporting structure and has become weak. Since this is usually because of osteoporosis, sacral insufficiency fractures occur most often in older women.
This guide will help you understand
- what parts make up the sacrum
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What makes up the sacrum?
The sacrum is the triangular bone just below the lumbar spine. The sacrum has five segments fused together into one large bone. The coccyx or tailbone attaches to the bottom of the sacrum.
The sacrum forms the base of the spine and the center of the pelvis. The sacrum transmits the weight of the body to the pelvic girdle. It is shorter and wider in the female than in the male. Its name means “sacred bone”.
At the top of the sacrum there are wings from each side called the sacral ala. At the ala, the sacrum fits between the two halves of the pelvis. These pelvic bones are called the iliac bones. This is where the sacroiliac joints are formed. Most everyone has two dimples in their low back where the sacroiliac joints form. These three bones of the pelvis, the sacrum and the two iliac bones, make a ring.
Each of the iliac bones has projections called the pubic rami. They meet together in the front of the pelvis, forming a joint called the symphysis pubis. The iliac bones also contain the cup or socket for the hip joint.
Nerves that leave the spine in the area of the sacrum help control the bowels and bladder and provide sensation to the crotch area.
There are three types of bone, woven bone, cortical bone, and cancellous bone. In adults, woven bone is found where there is a broken bone that is healing (callus formation). It can also be found with hyperparathyroidism and Paget’s disease. It is composed of randomly arranged collagen strands. It is normally remodeled by the body and replaced with cortical or cancellous bone.
Cortical bone is called compact or lamellar bone. It forms the inside and outside tables of flat bones and the outside surfaces of long bones. It is dense and makes up 80 percent of our bone mass. The radius (wrist bone), skull, and long bones are made of cortical bone.
Cancellous bone is also called trabecular bone. It lies between the cortical bone surfaces. It is the inner supporting structure and is spongy. It makes up 20 percent of our bone mass. Normal cancellous bone is always undergoing remodeling on the inside surfaces of bone. Cancellous bone is found in the hip, spine, and femur.
The three main cells that form and shape bones are osteoblasts, osteocytes, and osteoclasts. Osteoblasts are bone-forming cells. When calcium is deposited in the cells, they make bones strong and hard. Osteocytes are mature osteoblasts trapped within the bone. Osteoclasts are bone-resorbing cells. They dissolve bone surfaces by releasing a chemical called an enzyme. Their activity is in part controlled by hormones in the body.
It is normal for bones to have mini fractures from everyday wear and tear. They are healed by ongoing bone remodeling. Bone remodeling occurs in 120 day cycles. Normal bone has a balance of clearing away old bone and formation of new bone. Osteoclasts resorb or clear away the damaged bone for the first 20 days. Bone is then formed by osteoblasts over the last 100 days.
Sacral insufficiency fractures usually are parallel to the spine. They are most often in the ala, just beside the sacroiliac joint. At times there is also a transverse fracture that connects insufficiency fractures when they occur on both sides of the sacrum. The fracture lines then create an “H” pattern. Sacral fractures are classified into three zones, zone 1, zone 2, and zone 3. If the fracture involves just the ala, there is usually not a risk for nerve damage.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
What causes sacral insufficiency fractures ?
A physician named Lourie first described sacral insufficiency fractures in 1982. These fractures can cause severe pain in the buttock, back, hip, groin, and/or pelvis. Walking is typically slow and painful. Many daily activities become painful, difficult, and in some cases impossible.
Sacral insufficiency fractures occur when the quality of the sacral bone has become insufficient to handle the stress of weight bearing. The bone has lost some of its supporting structure and has become weak.
Osteoporosis is the leading cause of sacral insufficiency fractures. Osteoporosis is defined as low bone mass (weight). There is a decrease in bone tissue and minerals such as calcium. This can make the bones fragile. This means they can break more easily. Bone mineral density is measured by a DEXA scan. DEXA involves scanning the lumbar spine, the hip, and sometimes, the wrist. Osteoporosis affects 25 million people in the United States. Of these, 80 percent are females.
Other risk factors that can weaken bone include radiation to the pelvis, steroid use, rheumatoid arthritis, hyperparathyroidism, anorexia nervosa, liver transplantation, osteopenia, Paget’s disease, hip joint replacement, and lumbosacral fusion. Sacral insufficiency fractures can also occur in pregnant or breastfeeding women due to temporary osteoporosis.
Sacral insufficiency fractures can occur spontaneously, meaning there does not need to be any trauma such as a fall. The fracture can just simply happen when the bone becomes too weak to handle the stress of weight bearing. When the sacrum is fractured, 60 percent of the time the bone in front of the pelvis will also fracture. This bone is called the pubic ramus.
Symptoms
What does a sacral insufficiency fracture feel like ?
Unfortunately, sacral insufficiency fractures are often an unsuspected and undiagnosed cause of low back pain in elderly women. It was not until 1982 that they were described by a physician named Lourie.
Symptoms can include severe pain in the buttock, back, hip, groin, and/or pelvis. If the pubic ramus has fractured, there may be pain in the front of the pelvis. Walking is typically slow and painful. It can be difficult to do other necessary activities. Your back or pelvis may be tender to touch. You may find that you have limited range of motion of your low back.
Rarely there is nerve damage with sacral insufficiency fractures. When nerve damage does occur, the symptoms are usually problems with bowel or bladder function, or decreased sensation or strength of the leg(s).
Diagnosis
How do doctors diagnose the problem?
Your doctor will want to ask questions about your general health, what your symptoms feel like, and if there was any trauma that could have caused your symptoms.
Your doctor will want to perform a physical exam. This will likely include checking your nerve and spinal cord function, checking your range of motion, and feeling or tapping your back and pelvis to check for tenderness.
Your doctor will want you to have imaging of your pelvis. Plain X-rays are often negative. However, a fracture will be seen on bone scan, Computed Tomography (CT), or Magnetic Resonance Imaging (MRI).
Your doctor may order a bone scan with technetium-99m medronate ethylene diphosphonate (MDP). The MDP is injected into your vein. This should be performed after a minimum of 48 to 72 hours after symptoms begin. Where there is a fracture, the MDP will be concentrated. Uptake patterns on the scan may include the “H”-shape, also called the Honda sign when there is a sacral insufficiency fracture.
Single Photon Emission Computed Tomography (SPECT) is a new, advanced diagnostic nuclear medicine procedure that uses the emission of a radioisotope that is carried in the blood to the tissues. SPECT imaging is often added to provide information that is not available on routine bone scan images. It provides three-dimensional (3-D) views of the area examined. Following a bone scan you will remain on the exam table and the camera will rotate around the table while it takes pictures. SPECT imaging adds 30 to 60 minutes to the time of the nuclear scan. Sedation may be needed.
CT scan may be used to confirm and complement a positive bone scan. The CT scan uses special Xrays.
MRI is the radiological examination of choice by some doctors. Bone marrow edema on an MRI suggests a fracture. The MRI machine uses magnetic waves, not X-rays to show the bone and soft tissues.
Your doctor may request that you give samples of blood for the laboratory. This is to see if there could be another cause for osteoporosis that can be treated.
Treatment
What treatment options are available?
Most of the time treatment for sacral insufficiency fractures is non-surgical.
Nonsurgical Treatment
Treatment consists of rest, pain medications, and gradual walking with a walker or crutches. Improvement of symptoms may begin after one to two weeks of treatment. Most people are pain free in six to 12 months. Complete healing may occur after nine months. Most patients should have a full recovery.
Water exercise may be recommended to allow movement.
Bracing with a corset is sometimes helpful.
Medications that are used to help the fracture heal include calcium (1200-1500mg) and Vitamin D (400-800 IU). Bisphoshonates such as Actonel, Fosamax and Boniva are used to treat osteoporosis. Calcitonin is also used to help with pain and healing of the bone when broken. Parathyroid hormone (PTH) replacement can also be beneficial. It increases both bone resorption and bone formation. Bone mineral density is increased, making the bone stronger.
For pain, narcotics or opioids can be helpful. Some doctors feel that nonsteroidal anti-inflammatories (NSAID) such as Aleve or Ibuprofen should not be used for at least three to four weeks after a new fracture. Some studies have shown that they can slow fracture healing.
Your doctor may want you to have physical therapy to help with your pain. Heat, gentle massage, and electrical stimulation, or TENS units may improve pain.
Surgery
Surgical treatment is rare with sacral insufficiency fractures. A newer treatment that shows some promise in relieving pain and allowing more normal activity sooner is called a sacroplasty.
During sacroplasty, a bone glue called polymethylmethacrylate (PMMA) is injected into the fracture. Serious complications can occur if it is not performed correctly.
Sacroplasty may be considered in those with a severe decrease in functional ability and quality of life. It may provide faster relief of pain than typical conservative care. It is usually done in a surgery suite.
The area that is to be injected is cleaned and sterilized. This helps to decrease the possibility of an infection. A needle is placed in the area over the fracture. This is monitored with an X-ray machine. Bone glue is then injected and hardens rather quickly. This stabilizes the fracture. You are usually allowed to go home the same day.
If there are neurological symptoms from the sacral fracture, The sacrum may need to be stabilized. Hardware such as screws and plates may be used.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Previously, bedrest was the recommended treatment for sacral insufficiency fractures. There are many complications of prolonged bedrest, especially in the elderly.
Medical management presently allows limited weight bearing. This can be tolerated with a wheeled walker or crutches in most cases. Limited weight bearing actually helps to stimulate new bone growth.
In six to nine months, you should be able to return to your previous activity level.
If you have a sacroplasty, the fracture will be considered healed much more quickly. This allows you to return to your previous activity level sooner also. Your doctor will likely repeat imaging studies to check the progress of the healing fracture(s).
Treating osteoporosis is crucial in an attempt to decrease the risk of another insufficiency fracture. Your doctor will likely recommend additional calcium, vitamin D. A prescription medication to help prevent mineral loss from your bones is also commonly used. Regular follow up with your doctor is important. DEXA scans are usually repeated to ensure that the treatments for your osteoporosis are working.
Weight bearing activities such as walking, and lifting light weights can be helpful. Avoiding excessive caffeine, alcohol, and smoking is important.
After Surgery
You will likely have to remain non-weight bearing for a period of time before being allowed to walk with a walker or crutches. You will need assistance for daily activities initially. This may mean that you will have to have live-in help, or stay in an extended care facility or nursing home.
Once allowed, your surgeon may want a physical therapist to help with walking and maintaining strength. Your surgeon may want an occupational therapist to help you with equipment that may be helpful, showering, dressing, and other daily activities.
Your surgeon will want you to follow up with him or her on a regular basis to check on how the fracture is healing. Imaging studies will be repeated. Healing should occur in six to 12 months. If the fracture heals properly, you should be able to return to your usual activities.
Treating osteoporosis is crucial in an attempt to decrease the risk of another insufficiency fracture. Your surgeon will likely recommend additional calcium, vitamin D. A prescription medication to help prevent mineral loss from your bones is also commonly used. Regular follow up with your doctor is important. DEXA scans are usually repeated to ensure that the treatments for your osteoporosis are working.
When allowed, weight bearing activities such as walking, and lifting light weights can help keep your bones strong. Avoiding too much caffeine, alcohol, and smoking is important.
Spinal Tumors
A Patient’s Guide to Spinal Tumors
Introduction
A tumor is an abnormal growth of tissue. There are several types of tumors that can develop in or near the spine. There are many types of spinal tumors. They can involve the spinal cord, nerve roots, and/or the vertebrae (bones of the spine) and pelvis.
There are two classifications of spine tumors. A spinal tumor can be primary, meaning it comes from cells within or near the spine. Primary tumors of the spine are rare. More commonly a spinal tumor that is found is a secondary spinal tumor. This means that the tumor traveled there from somewhere else in the body.
Tumors can be benign (non-cancerous) or malignant (cancerous).
This guide will give you a general overview of spinal tumors and help you understand
- what parts of the spine are involved
- what causes spinal tumors
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the spine are involved?
The cervical spine is formed by the first seven vertebrae. The cervical spine starts at the bottom edge of the skull. It ends where it joins the top of the thoracic spine. The thoracic spine is where the chest begins and is made up of twelve vertebrae. This region is different than the other areas of the spine because it has ribs attached to the vertebrae. It ends where it joins with the lumbar spine. The lumbar spine is made up of five vertebrae in the lower back. It joins with the sacrum or pelvis at the bottom.
Each vertebra is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body. When they are stacked on top of one another, the rings form a hollow tube called a neural arch. This forms a canal where the spinal cord is located. The spinal cord is protected by the bone. The spinal cord begins at the base of the brain, just below the medulla or brain stem. It ends in the lumbar spine at about the first or second lumbar vertebrae where it is called the conus medullaris. Here it splits into many fibers.
This is called the cauda equina because it looks like a horse’s tail.
The spinal cord is a tube of nerve cells that is hollow in the middle. It carries sensory and motor messages to and from the body and the brain. It is surrounded by layers of tissue and fluid called the cerebral spinal fluid. It is housed in the vertebral or spinal column which is made up of 24 bones, called vertebrae. Vertebrae are stacked on top on one another to form the spinal column. The spinal column is the body’s main upright support.
There are three layers of tissue that surround the spinal cord. The thin, delicate lining of the spinal cord is the pia mater. The next layer is the arachnoid membrane. It was named that because it looks like a spider web. The outermost layer that is thicker and tougher is called the dura mater. These layers are continuous with the layers covering the brain. These layers may give rise to tumors that can spread to the spinal cord.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
A primary spinal tumor means it comes from cells within or near the spine. They can involve the spinal cord, nerve roots, and/or the vertebrae (bones of the spine) and pelvis.They can be benign (non-cancerous) or malignant (cancerous). In general, benign tumors do not invade other tissues. Malignant tumors may invade other tissues and organs in the body. Although primary spinal tumors often contain a number of abnormal genes their cause remains unknown. In some cases the tumors run in families.
Tumors in the spine become a problem when they compress the spinal cord or nerves. This can lead to serious complications such as paralysis and loss of bladder and bowel control. Others can destroy the vertebral bone that supports the spinal cord making it unstable.
Nerve roots on either side of each spinal segment are made up of bundles of motor and sensory nerves that come from the spinal cord. Nerves are covered by protective cells called Scwhann cells. A form of spinal tumor involving the Schwann cells is called a Schwannoma.
A secondary spinal tumor is more common. This means that the tumor traveled there from cancer somewhere else in the body. These secondary or metastasized tumors are always cancerous. These cancer cells travel and cause tumors that usually involve the vertebrae or bony portion of the spine. They may come from melanoma (skin cancer), cancer in the lung, breast, prostate, kidney, or thyroid gland for example.
Symptoms
What does a spinal tumor feel like?
Sometimes the tumors are found before they cause any symptoms. The symptoms will vary depending on where the tumor is located and what tissues are involved.
At times, pain, bowel or bladder problems, sexual dysfunction, change in sensation, or muscle weakness of the arms or legs may alert you to the problem. This often means that the tumor is compressing the spinal cord or nerve root. Tumors that originate in the spinal cord itself may not cause pain. Pain that awakens you in the night or development of scoliosis (abnormal spine curve) may be a sign that the bone of the vertebra is being destroyed by a spinal tumor.
Symptoms may have a gradual or rapid onset. Symptoms usually worsen without treatment.
Diagnosis
How will my doctor diagnose the problem?
Diagnosis begins with a thorough history and physical exam. Your doctor will ask questions about your symptoms and how your problem is affecting your daily activities. This will include questions about pain, feelings of numbness or weakness, change in bowel or bladder function, and whether you have noticed any changes in the way you walk. Your doctor will want to know if have been diagnosed with any type of cancer in the past.
During the physical exam, sensation of the skin, muscle strength, and reflexes are tested. Your doctor may ask you to walk to see if there are any changes in your walking pattern.
In addition to having lab work done, there are several procedures that can help your doctor diagnose a spinal tumor.
Magnetic resonance imaging (MRI) allows your doctor to look at slices of the area in question. The MRI machine uses magnetic waves, not X-rays to show the soft tissues of the body. This includes the spinal cord and nerves. The test may require the use of dye that is given intravenously.
Computed tomography (CT) scan may be ordered when an MRI is unavailable. Dye will be introduced into the spinal canal fluid so that the spinal cord and nerve root anatomy are identified better. When dye is injected for this purpose, the technique is called a myelogram.
X-rays of the spine may be ordered when there is the likelihood of metastasized tumor from cancer elsewhere. It can show only changes in the bones. Many primary spinal tumors do not affect the bone when they are in the early stage.
Bone scans can be used to detect fracture, bone infection, or cancer. A radioactive tracer, technetium (Tc), is injected into your vein. Where there is an increase in metabolic activity, such as is the case with cancer, the Tc will be more concentrated. Spinal tumors may be malignant, or metastasized from cancer somewhere else in the body. It is helpful to use a scan to see if there are other areas in the body where the cancer may be.
A biopsy helps determine the type of the tumor. A biopsy may require surgery. Sometimes it can be performed using a needle while using CT for guidance. A piece of the tumor is removed and looked at under a microscope.
Types of Spinal Tumors
Malignant Spinal Tumors
Osteosarcoma occurs most often in children, adolescents, and young adults. Males are more likely to be affected than females. Treatment usually consists of removal of the tumor when possible as well as chemotherapy. Radiation therapy is not effective. Older persons with Paget’s disease or who have had radiation therapy may develop this type of tumor.
Ewing’s Sarcoma occurs in the bone of the spine or surrounding tissues. It usually affects adolescents and those in early adulthood. When it involves the spine, it may cause paralysis and loss of bladder or bowel function (incontinence), numbness or tingling. Removing the tumor is preferred if possible, in combination with chemotherapy and sometimes radiation. If the tumor has traveled to the bone marrow, stem cell transplant is a more aggressive form of treatment.
Chondrosarcoma usually occurs in adults and is most common in flat bones such as the pelvis. They usually are noticed because they cause pain and swelling. Surgery is performed to remove the tumor and any tumors that have spread, usually to the lung. In most cases, chemotherapy is not effective.
Astrocytomas are tumors that involve nerve cells within the spinal cord and brain. They most commonly occur in children and adolescents. Neurological symptoms such as weakness and/or sensory changes may be the cause for seeking treatment. They tend to spread throughout the spinal cord and brain. Astrocytomas in the spine can usually be removed surgically. However, they are difficult to completely remove. Radiation therapy may be necessary following surgery to slow the spread of the tumor.
Cancer in the bone marrow is called multiple myeloma. Bone tissue is destroyed by excessive growth of plasma cells in the bone marrow. When X-rayed it appears that holes have been taken out of the bone. These are called osteolytic lesions. Plasma cells are part of the immune system and in multiple myeloma they grow uncontrolled forming tumors in the bone marrow. Any part of the skeletal system (bones) can be affected including the spine. For multiple myeloma, treatment may include chemotherapy and other medications, radiation, and stem cell transplantation.
Benign Spinal Tumors
Osteoid osteoma is the most common of the benign tumors involving the bone of the spine. It is usually found during adolescence. It may be discovered because of scoliosis or curvature of the spine. It may cause pain that does not ease up, and is worse at night. Anti-inflammatory medications are used for treatment. Sometimes removal of the tumor by surgery is necessary. A newer, less invasive treatment is called radio-frequency ablation. These tumors rarely recur (come back).
Related Document: A Patient’s Guide to Radiofrequency Ablation
Osteoblastomas are larger versions of osteoid osteomas. They tend to be found in people under the age of 30. They may cause scoliosis or curvature of the spine. Osteoblastomas tend to be more aggressive and require surgery to remove the tumor. There is a 10% chance that the tumor may recur.
Giant cell tumors are very rare and tend to affect the vertebral body of a spinal segment. They can be aggressive and sometimes spread to other parts of the body, usually the lung. Treatment involves surgery to remove the tumor. Also, radiation therapy may be used.
Enchondromas are tumors involving cartilage. They may grow into the spinal canal or press on the spinal nerve roots. When they cause paralysis, bowel or bladder incontinence, or other neurological symptoms they are surgically removed. They rarely can become chondrosarcomas, which are malignant tumors that can spread to other parts of the body.
Hemangiomas are tumors involving blood vessels that affect the vertebral body of a spinal segment. They are most commonly found in the thoracic or lumbar portion of the spine. They occur more frequently during mid-life. They are found more often in women than men. They can be a source of pain but often do not cause pain. They may be large enough to cause collapse of the vertebral body which could affect the spinal cord or nerve roots.
Meningioma is the most common spinal cord tumor. They tend to occur in older adults and are more common in women. They are usually treated with surgical removal. Rarely, meningiomas recur or spread to other parts of the body.
Ependymoma is a tumor involving the cells lining the canal in the center of the spinal cord. These tumors have the greatest chance for surgical cure.
Schwannoma is a tumor that involves the covering or sheath of peripheral nerve fibers. It may cause weakness, paralysis or sensory changes such as numbness. It can be removed surgically.
Chordomas are tumors that are typically found at the lower end of the spine. Because they can aggressively grow, they can cause compression of the spinal cord or nerve roots causing neurological problems. Treatment involves surgery to remove the tumor. Unfortunately they come back, but do not spread to other areas of the body.
Plasmacytoma is a single tumor involving the bone of a spinal segment. It can have characteristic punched out holes in the bone on X-ray. It can cause a compression fracture of the vertebral body. This can cause neurological symptoms. Spinal surgery to decrease pain and improve function may be necessary. Plasmacytoma is felt to be an isolated form of multiple myeloma, which will then develop lesions in other bones in the body. Multiple myeloma is a malignant process and is the most common primary bone cancer.
Treatment
What treatment options are available?
The type of treatment will depend on symptoms, general health, the results of imaging studies, and a biopsy if done. Many times a combination of surgical and non-surgical treatments are required. If your treatment involves radiation or chemotherapy, you will be asked to see an oncologist (a doctor that specializes in cancer).
Early diagnosis and treatment of a spinal tumor is important. If undiagnosed, the damage caused by the tumor can become permanent.
Nonsurgical Treatment
Sometimes watching the tumor for growth is all that is necessary if significant symptoms are not present. The tumor is monitored with repeat imaging such as MRI. Not all spinal tumors can be removed by surgery due to their location.
A back brace or corset may help to stabilize the spine. This should also reduce pain. It may need to be custom made to fit you.
Medications such as corticosteroids may be prescribed. They are used to decrease the swelling in the spinal cord that can cause compression. They may be taken temporarily or long-term to relieve symptoms. Analgesics such as narcotics may also be used. Medications that diminish the blood supply to the tumor have shown some success. Bisphosphonates are medications more commonly used for osteoporosis. They may be used to treat tumors that can destroy bone in the spine.
Embolization is a term used when the blood supply to a tumor is interrupted. This is done by burning the blood vessel(s). Several types of spinal tumors are treated using this method.
Chemotherapy is used if the primary tumor is a malignant or cancerous tumor. Chemotherapy is also recommended when the tumor is a secondary tumor that has traveled from another area in the body and invaded spinal tissue.
Radiation therapy may also be used to treat tumors that cannot be removed by surgery.
Stem cell transplant may be used for aggressive cancers such as Ewing’s sarcoma.
Surgery
Surgery may be the only treatment for a primary spinal tumor that is non-cancerous. As much of the tumor is removed as possible without causing neurological problems. A decompression refers to removing bone around the spinal cord or spinal nerves in order to take pressure off these structures. Neurological damage during surgery has been improved with the use of newer techniques. These techniques include ultrasonic aspirators, and microsurgery. Ultrasonic aspirators use sound waves to destroy the tumor. It also sucks up the pieces of tumor. Microsurgery uses a microscope for a better view of the operation site. This helps to minimize any damage to surrounding healthy tissue.
If the spine needs to be stabilized or fused as a result of removing a tumor in bone, metal hardware may be required. Metal plates, cages, rods, or screws may be used. The bone may be additionally supported by bone graft or bone cement.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Your doctor will require you to have periodic follow-up. New lab tests and imaging studies may be required. You may need pain management on a regular basis.
Physical therapy can help with balance, strength, walking, and coordination. Occupational therapy helps with activities of daily living such as dressing, bathing and assistance with mobility. You may need instruction in the use of a brace. Instruction in proper ways to lift and move may be necessary.
After Surgery
The amount of time you will be hospitalized depends on the type of surgery required.
After surgery, activity such as sitting and walking will be allowed as well as activities that do not require stretching of the spine or straining. Lifting is limited during the initial recovery period. You may be required to use a brace or corset after surgery to help with stability.
Radiation is often used following surgery to kill remaining tumor cells. It usually begins one to two weeks following surgery. Radiation lasts only 15-20 minutes per day for two to six weeks.
You can expect recovery and improvement in symptoms between two weeks and several months following surgery. You may need pain management during your recovery, or possibly on a more long-term basis.
Physical and occupational therapy may be beneficial to help restore any lost strength, coordination, or other skills.
Your surgeon will require you to have periodic follow-up. New lab tests and imaging studies may be required. Sometimes the tumor will grow back and need to be removed again.
Nutrition and Your Spine
A Patient’s Guide to Nutrition and Your Spine
Introduction
You are what you eat. Is that simply a funny saying or is there some truth to that old adage? The spine is not something that usually comes to mind when one thinks about nutrition – but it should. Nutrition is important in having a healthy spine. Good nutrition also helps control pain and disability when we are suffering from many different types of spine conditions.
This guide will help you understand
- what is nutrition
- how nutrition affects the spine
- how nutrition affects injury, inflammation, and pain
- how to use good nutrition to get ready for and recover from spine surgery
How you eat and exercise (or don’t exercise) will make you more or less likely to have problems with your bones, joints, and connective tissue. This guide will help you learn how to use nutrition for healing after an injury. We will describe how you can make simple changes to your diet and other lifestyle habits. These changes can be helpful if you have a painful spine condition. You will learn how to tell if you have given the changes enough time to work for you. You’ll learn to know if it’s time to move on to other health care solutions for your problem.
Nutrition
What is nutrition?
Nutrients are the chemical elements that make up a food. Nutrients are the basics of what you eat that give your body what you need for “running the show”, that is, for metabolism. Certain nutrients such as carbohydrates, fats, and proteins provide energy. Other substances such as water, electrolytes, minerals, and vitamins are needed for metabolic processes.
Nutrition is all of the internal chemical changes that happen as a result of what we eat (or do not eat) each day. Good nutrition means that what we are swallowing is something that adds to our health. Once we have digested it, food has an important job to do in our body.
Good nutrition is needed for tissue growth and repair. We get good nutrition by eating foods and taking supplements that contain all the proper and necessary ingredients. We also get good nutrition by being able to completely digest the things we swallow. Then we must be able to absorb the nutrients into the blood and other body fluids. With the right nutrients given to the cells, metabolism, or the work of the body, can occur in the most efficient and healthy way.
By the definition above, we know that a lot of what we eat is not nutritional. When we eat a purple pill or swallow a blue-colored sports drink, what we are taking in has no job to do in our body. That purple or green coloring is not a chemical your body has any use for.
The same is true for things like the preservatives added to your cereal. These chemicals are put in so that the cereal doesn’t get moldy in the box. The same thing is true for traces of hormones and antibiotics left in our meat and dairy foods. When you eat French fries from a fast-food restaurant, the oil they have been cooked in has changed into a type of fat that can’t be used by your body. In fact, it has become something called a trans-fat. Trans-fats damage the walls of your body’s cells. This will make more work for your body.
Metabolism
What is metabolism?
Metabolism refers to all of the physical and chemical changes that are taking place in your body every moment. Making energy in the body is part of metabolism. All the physical work that occurs inside your cells is part of this process, too. It includes all the work and chemical changes that happen every day in your bones, connective tissues, body fluids, and organs.
Metabolism refers to the work of changing the chemical energy in nutrients into mechanical energy or heat in your cells.
Metabolism involves two basic processes. There is anabolism (building up) and catabolism (disintegration or breaking down). During anabolism the body works to change simple chemicals from what you have eaten into complex parts, like blood, bone, or connective tissue. During catabolism, complex parts are broken into simpler pieces. One catabolic process is the breaking down of an apple you have chewed and swallowed. It is broken down into water, fiber, vitamins, and minerals. The end of catabolism is usually something being passed out of the body. We are healthy when both anabolism and catabolism are in proper balance.
Our bodies have very good ways to know when food we eat is not useful and to get rid of it. But it takes up a lot of good nutrients to sort out what’s good and what’s not. Getting rid of damaging things you eat uses up energy in the cells, too.
Nutraceuticals
If you have aches and pains, if your joints are inflamed, or if you are overweight, your diet may not have enough good nutrition to get all the necessary work done. That is why nutraceuticals have become so important.
Nutraceutical is a new word, invented by Dr. Stephen DeFelice in 1989. It is a combination of the words nutritional and pharmaceutical. Nutraceuticals are dietary supplements that are sometimes also called functional foods. Many people take nutraceuticals to offset an inadequate or unhealthy diet.
Even with a good diet of fruits and vegetables, whole grains, and the right amount and kind of protein, the standard American diet usually does not have enough nutrition for all the work your body needs to get done. We grow our fruits and vegetables with lots of fertilizers. Chemicals from the fertilizers remain on it when it’s part of your meal. The same is true for pesticides and herbicides sprayed on the plants before harvest.
We harvest fruits and vegetables when they are not quite ripe. Then they are trucked thousands of miles to our stores. Food that is not quite ripe when picked means it doesn’t have its full nutritional value. Food harvested too early will not bruise as easily when it is loaded on and off trucks. It will look good when you buy it, but it won’t have all the nutrition you need to get from eating it.
Proper Balance
We face challenges our grandparents never knew. There are extra chemicals in our food and water. Our food supply just is not as nutrient-rich as we need it to be. A proper balance between protein and high fiber, starchy foods is important for good nutritional health.
It is important to understand that nutrients always work together. Nutraceuticals can help when you aren’t able to eat a perfectly balanced diet. The same is true when you can’t eat everything organic. Supplemental vitamins, minerals, amino acids, and fatty acids are the way to help yourself meet all the needs of your body. This includes growth and repair after injury. It’s also true for the metabolic work needed to feel good, be strong, and live well.
Healthy fats are needed to grow and repair normal connective tissue, bones, and body fluids. The fiber and carbohydrates in whole grains and fresh produce are what your body is designed to thrive on. The fats found in olive oil, deep ocean fish (like salmon and sardines), and nuts and seeds are all part of good nutrition.
Organically raised beef, poultry, and wild ocean fish give the best protein. When you can’t eat organically raised meats, you can decrease your exposure to damaging chemical residues. You can do this by removing all visible fat from the meat before you cook it.
Specific problems can be related to not enough (or too much) of a single vitamin or mineral. But the proper function of the human body requires the right amounts of ALL the nutrients. You can think of it like a recipe. Your soup will taste good when all the ingredients are there in the right balance. Having too much of some of the spices, or not enough salt, will make a pot of otherwise really good food taste terrible. The same is true for the nutrient “soup” in your body. You need to have the right amounts in the correct proportions to have all your body systems work at their best. Every vitamin, mineral, amino acid, and fatty acid has hundreds of jobs to do. None of these nutrients can work well if it is not in the right relationship with all of the other nutrients.
Nutrition and the Spine
How does nutrition affect the spine?
Nutrition will determine how strong your teeth, bones, and connective tissue are. We begin to build our skeleton and connective tissue before we are born. Our diet in childhood has a major effect on how strong we are as adults. What you eat during your whole life will decide how able you are to repair bones, cartilage, ligaments, tendons, and muscles.
Everyone has to replace body tissues due to normal every day wear and tear. Some of us also have repair work to do after injuries or surgery. The raw material for repair comes from our diet. Vitamin C, all of the B vitamins, vitamin D, vitamin K and the minerals calcium, magnesium, copper, zinc, boron and manganese are especially important for bone and connective tissue health. Drinking enough water is also essential.
Your spine is your backbone. The bony pieces of the spine are called vertebrae. There are 33 of these bones. Between each vertebra is a disc made of tough cartilage with a fluid center. These discs provide the cushion that allows your backbone to bend and twist. Discs also act like shock absorbers as we walk, run, and jump. Each vertebral segment consists of bone next to bone with a cartilage cushion between. They are tied together with connective tissue, ligaments, and tendons.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Degenerative disc disease is an example of damage to connective tissue that is affected by nutrition. Everyone is going to have a certain amount of damage to the spine. This occurs throughout a lifetime. The discs can flatten, and protrude from between the bones. In time, most people will have small tears in the outer layers of these discs. You are more likely to have injuries if you have poor nutrition. And you’re less likely to have good healing.
Poor nutrition means not getting enough vitamins C, A, B6 and E, as well as the minerals zinc and copper. Daily wear and tear plus injuries from work, sports, or accidents can damage your spinal discs. Good nutrition and adequate hydration (getting enough fluids) play a vital role in your body’s ability to repair the damage and recover from the inflammation that causes the pain of back injury.
Connective tissue, like the cartilage between your joints and the ligaments and tendons that hold them together is made mostly of collagen. Collagen is a type of protein and water. Strong collagen fibers require a steady supply of dietary protein. They also need vitamin C along with vitamins A, B6, and E, and the minerals zinc and copper.
Building Bone with Good Nutrition
Joints are made and maintained, repaired, and protected with proper nutrition. Bone is made of minerals like calcium, phosphorus, magnesium, and boron. Bones also contain water and collagen. The upkeep and repair of bone and connective tissue requires the right amounts of vitamins and other nutrients working together.
Another diet and nutrition-related bone disease is called osteoporosis. Osteoporosis means the bones are weakened, brittle, and can break easily. Lifestyle and nutritional factors can lead to the bone loss of osteoporosis. This includes what you eat during bone-building stages in childhood and adolescence. Nutrition throughout the adult years is also important to maintain good bone density. Calcium intake is a major factor for building bone density. You will find yourself with weakened bones if you do not get enough calcium. The same is true if you do not absorb or properly metabolize the calcium you do eat. You can also lose too much calcium through the urine because of dietary choices. Other conditions like chronic mental or emotional stress that cause inflammation of the digestive tract can prevent calcium absorption. A lack of proper acidity in the digestive tract can also make calcium pass through unabsorbed.
Vitamin D is essential for maintaining and regulating the health of bones and teeth along with many other functions in the body. It is a compound that is more of a hormone than a nutrient or vitamin and thus has an important role in regulating immune function and cell growth.
Vitamin D is needed to absorb calcium from the gut. It prevents bone loss and helps rebuild new bone. Vitamin D is needed for the enzymes that strengthen collagen. Collagen is a major component of bone and connective tissue. Vitamin D has also been shown to aid in nerve and muscle (neuromuscular) function.
How can you get enough vitamin D to ensure good body and bone health? Sunlight will produce vitamin D in your skin. Exposure of the skin to sunlight for five to 30 minutes between 10 am and 3 pm (in most geographical locations) twice a week is usually enough to make your own Vitamin D. As you get older, your capacity to produce vitamin D from sunshine slows down.
Diet may aid you but not with natural foods. Except for cod liver oil and some types of fish (salmon, tuna, mackerel, sardines), vitamin D is not found in what we eat. Only foods that have been fortified with vitamin D (e.g., milk, cereal, yogurt, orange juice) have any significant amounts of this vitamin.
A very low fat diet will make it harder for you to absorb vitamin D from your food. Lack of sunshine and limited consumption of foods fortified with Vitamin D may mean you need to take a nutritional Vitamin D supplement. Your physician will help you decide what kind and how much to take for your age, health, and risk factors. Vitamin D supplementation may be based on current levels of vitamin D in your blood.
You may be someone who does not rebuild bone as quickly as you lose it. Nutritional deficiencies can make this problem worse. Caffeine-containing drinks like coffee and colas will cause increased loss of calcium through the urine. Cola drinks with high levels of phosphorus also disrupt calcium metabolism and healthy bones.
Magnesium is as essential as calcium for strong bones. As much as 50 per cent of your magnesium is found in your bones. Magnesium is required to move calcium into bone. Magnesium is also needed to make vitamin D active. A typical American diet contains much less than the recommended daily requirement for magnesium.
Magnesium is lost through the urine. This happens when people are stressed. Studies have shown something as common as loud noise levels will increase the loss of magnesium. Alcohol and many drugs used for heart disease and high blood pressure also cause magnesium loss. Bone repair calls for amounts of magnesium usually much higher than the recommended daily allowance.
L-lysine is an amino acid that you need to activate intestinal absorption of calcium. You will lose too much calcium through your kidneys if you do not have enough lysine. Lysine is an essential element for building the collagen framework. Minerals like calcium and magnesium weave into collagen to create bone.
You may need supplementation with these minerals, vitamins, and amino acids. This applies to you if you work indoors or don’t get out in the sun much. You are also at risk if you are elderly, or are a sedentary person who drinks a lot of coffee or cola drinks. If you do not digest well, or if you eat a very low fat diet, it may be important to use a good quality supplement to protect your bones.
Specific nutritional factors that will increase your risk of pain and inflammation are
- not enough omega 3 fatty acids from ocean fish
- not enough fruits and vegetables in the diet
- not enough vitamin D from sun exposure or fortified foods
- risk factors for vitamin D deficiency (e.g., older age, dark skin, use of sunscreen, obesity, kidney disease, liver disease, use of some medications, milk intolerant)
- not enough of the minerals potassium and magnesium
- not enough protein and high quality fat in the diet to control enzymes that produce inflammation
- too many sweets and starches in the diet, leading to weight gain and to excess insulin
- too many free radical ions from rancid and hydrogenated fats, low nutrient refined foods, chemical additives and residues
Nutrition and Inflammation
Inflammation is most often thought of as the redness, warmth, swelling, and pain that occur with an injury. The body responds this way whether it’s a surgical incision or a spider bite. Inflammation is also present in an infection like a strep throat or the achy, hot finger joints of rheumatoid arthritis.
Wound healing and fighting infection are just some of the ways inflammation is activated. Inflammation is happening all the time in more or less obvious ways in your body. Medical science has begun to understand the connection between inflammation and most of the chronic degenerative diseases. Some of these diseases – like cancer, heart disease, or diabetes – develop quietly for many years before causing problems. We aren’t even aware they are present. Pain isn’t always a part of these diseases. People can be pain free even when a lot of tissue damage has occurred. Others conditions, like osteoarthritis, gall bladder disease, or degenerative disc disease, make their presence known. Pain with these conditions can range from mild to unbearable.
These conditions all have one thing in common. The tissues of the body parts involved are inflamed. The process of inflammation depends on a number of different chemical elements. These are called inflammatory mediators. Chemical mediators are released from certain kinds of white blood cells. These white blood cells are part of our immune system. First they travel to a target area. Then they cause a series of reactions that create the tissue changes we refer to as inflammation. At first this process is actually a repair response to some sort of injury or insult to the tissue. Later, the inflammatory process can become chronic and the cause of further injury.
Inflammation and Back Pain
Healthy repair depends on good nutrition. Poor nutrition can lead to damaging inflammation in the joints of your spine. Inflammation causes the loss of the cellular framework that holds bone and connective tissues together. Studies show that some people with osteoarthritis have more rapid damage to their joints. This is because they have more inflammatory chemistry in their bodies.
Back pain may or may not be present in people with bone or cartilage changes in their spine. For instance many people have x-ray images that show they have flat and bulging discs. Or they may have brittle bones. Yet they have no pain. It is inflammation that causes the tissue changes that create the sensation of pain.
Inflammation stimulates the growth of new blood vessels in joint tissues. This growth process also causes new nerves to grow in areas around joint cartilage. Doctors think this new nerve growth may be why back pain goes along with inflammation. The increased tissue activity and the swelling that comes with inflammation can make the new nerves very sensitive. All of the steps in this inflammatory process (new blood vessel growth, new nerve growth) keep each other going in a never-ending cycle. Stopping inflammation will relieve pain and slow down joint damage.
Back Pain and Obesity
Abdominal obesity adds to spine problems in very important ways. Fat around your middle can cause strain on the muscles and ligaments that support your spine. The joints of your spine are especially vulnerable to daily wear and tear from lack of support.
Most of us get fat by eating too much of the kind of starchy, refined foods that call up more insulin. Insulin will signal enzymes in your body. These enzymes increase levels of inflammatory cells. They also increase cholesterol and constrict (close down) blood vessels. All of these actions help increase the levels of pain you feel from all over your body.
Abdominal fat is made of the type of cells most active at making the kind of chemistry that causes damaging inflammation to all of your joints. The more belly fat you have, the more inflammatory chemistry you are making. Some lean people are also at risk.
How does nutrition affect healing after injury or surgery?
Good circulation is needed to build and repair a surgical incision, injured bone, or connective tissue like cartilage and ligaments. Your blood vessels carry all the raw materials needed to maintain proper strength and function of your bone and connective tissues. Your blood vessels also carry away from these body parts all the waste material from normal wear and tear as well as from injuries. A diet that has too much starch and sweets, and not enough protein and healthy fats, will cause blood vessels to constrict. Then there is less blood flow to the areas that are injured and need repair.
All of the chemical reactions that make up the work of growth and repair require good nutrition. Herbs, fruits, and vegetables contain the dietary sources of antiinflammatory chemistry needed for tissue healing. Plant foods have antioxidants that decrease the chemistry that triggers inflammation. This type of plant is called a flavonoid. Flavonoids are plants that have biologic and metabolic properties in the body. They also strengthen the healing process. They do this by knitting collagen fibers into tightly woven connective tissue. The result is well-knitted skin and blood vessels; dense bone; and strong, elastic ligaments and tendons.
What changes can you make to your diet and supplement choices if you have a spine condition?
It can be confusing to try to sort out what supplements to take. It’s not always easy to know what foods to eat or not eat to help with a spine-related problem. Different musculoskeletal conditions will have some different nutritional requirements. The form of each supplement will also be important, in terms of how useful it is for your condition.
For example, powdered nutrients in capsules or liquid forms are much more likely to be fully digested and absorbed. Tablets are often less expensive. But they don’t break down in many people’s digestive tracts.
Osteoporosis is an example of a spine-related condition with a clear link to nutritional status. Most people with osteoporosis will be advised to take at least a calcium/magnesium supplement. The best quality mineral supplements for osteoporosis are powdered and in the citrate form (for example, calcium citrate). Vitamin D should always be included in an osteoporosis formula.
Inflammatory conditions benefit from antioxidant nutrients like vitamin E. It must be natural vitamin E, not synthetic. It should always have mixed tocopherols in order to be most effective. Any inflammatory condition can be improved with the addition of at least five fish meals a week. A good, pure fish oil supplement taken daily can also help.
Here are some changes you can make to improve your spine condition. Most people will notice results in less than two weeks by following these general rules
- Drink at least eight large glasses of water or herbal tea daily. Avoid fruit juices or other beverages with coloring and preservatives added. This includes soda pop.
- Eliminate simple sugars. Get rid of sweets and starchy, refined white flour foods from your diet.
- Avoid packaged foods with added preservatives and colorings
- Take a high quality multiple vitamin/mineral supplements three times daily with each meal
- If you have any form of arthritis or any inflammatory condition, take a pure fish oil supplement. Most people are helped by one to three grams of combined omega 3 fatty acids daily. Look for EPA and DHA on the label.
- Add vitamin D3 to your supplements; make sure you are get 800 IU to 1000 IU daily. You may need more if you have a history of malabsorption (e.g., celiac disease, inflammatory bowel disease, cystic fibrosis, gastric bypass surgery)
Long-term dietary changes can benefit your spine condition. If you are overweight, ask a health professional to help you lose weight, especially abdominal fat. Most people can do this safely by
- eating fresh, raw, or steamed vegetables every day
- eating two or three pieces of fresh fruit every day
- eating five to seven fish meals a week
- eating three to six ounces of clean, lean beef, poultry, lamb, or game meat daily – eggs are also an excellent source of protein for most people
- using olive oil on salads and for cooking daily
- eating fresh nuts and seeds. Almonds, walnuts, and pumpkin seeds give us high quality, healthy fats
If you do not have a regular habit of exercise, invest in instruction with a professional who can teach you how to strengthen your muscles and protect your joints. Certain exercises will be very good for some spine conditions, and possibly harmful for others. An exercise professional is your best choice for guidance to design a safe, effective program just for your needs.
How long does it take to see results from these changes?
Many people who change their diets see results right away. The difference in body pain levels can be noticed in a matter of days. Reducing inflammation by stopping the triggers that sweets and starches create can be felt very quickly. The effects of diet changes are even more when added to the supportive chemistry of antioxidants. Dietary supplements can encourage your healing even more dramatically.
It can take some months of steady supplementation to rebuild your tissues after illness or injury. It depends on how deficient you are in certain nutrients. It may take three to six months for to experience the benefits of a specific supplement program. This time frame may vary based on your condition. Your doctor can advise you about this.
For expert help to start a nutrition plan for your spine health, see a nutritionist or contact a licensed naturopathic physician. Specially trained nutritionists may be available in your area. Many registered dietitians and conventionally trained nutritionists are limited in their ability to give personalized attention to in-hospital patients. You may have to look for an independent practitioner with more advanced training. The ongoing support of a progressive nutritionist can help you start new, healthy habits that will become a permanent part of your daily life.
Naturopathic doctors (NDs) are also available to help patients develop healthier nutritional habits for the spine. Naturopathic physicians practice the art and science of natural health care. They are trained at accredited medical colleges. Partnerships between medical doctors and naturopathic physicians are becoming more common all over the U.S. and Canada.
Intraoperative Monitoring
A Patient’s Guide to Intraoperative Monitoring
Introduction
Spine surgery can be unpredictable and potentially dangerous because it can involve areas near nerves and the spinal cord. During spinal surgery, there is a risk that damage to the nervous system can occur. This is especially true when hardware or instrumentation is used and inserted near nerves, or when a curvature of the spine is corrected. It is important for surgeons to be able to have someone experienced to monitor nerve tissue while doing the operation.
The nervous system can be monitored during spine surgery to make it safer. The term commonly used for monitoring the nervous system during surgery is intraoperative monitoring, or intraoperative neurophysiologic monitoring (IOM). Intraoperative monitoring is not only being used for complex spinal surgeries but is widely used for other surgeries too. Some of these include brain surgery, ear surgery, and surgery involving arteries.
This guide will help you understand
- what is intraoperative monitoring
- why is intraoperative monitoring important
- when is intraoperative monitoring used
- what happens during surgery
- what are possible complications
Anatomy
What parts of the spine are involved?
The spine is divided into various parts. The upper portion is the cervical spine, or neck. The middle portion is the thoracic spine, or trunk. The lower portion is the lumbar spine, or low back. There are bony blocks called vertebrae that make up the spine. They are stacked on top of one another. There are discs that separate the vertebrae and provide cushion. The spinal cord is protected by the bony spine. It lies in a hollowed area, or arch made by the bony spine. This is called the spinal canal.
Projecting from the spinal cord are nerves that travel to limbs, the trunk, and internal organs. The spinal cord is similar to a tree trunk. The nerves are like branches. The portion of the nerve as it branches off of the spinal cord is called the nerve root. The spinal cord sends and receives messages to and from the body and the brain. The nerves that branch off of the spinal cord go to various body parts to provide sensation and motor function or movement.
Nerve tissue is delicate and can be damaged relatively easily. When damage is done to the spinal cord or nerve, it may cause sensory and/or motor changes in the affected body part. The damage may be permanent.
What is intraoperative monitoring?
Intraoperative neurophysiological monitoring (IOM) uses equipment to evaluate the function of the spinal cord and nerves during spine surgery. Its role is to provide the surgeon with immediate feedback and warning before permanent nerve injury has occurred. This has been shown to increase safety and improve outcomes in complex spine surgery.
Intraoperative neurophysiological monitoring (IOM) began with the use of somatosensory evoked potentials (SSEPs). This measures the conduction of sensation above and below the area of surgery. During spinal surgery, electrodes are placed on limbs that could be affected by the surgery. Electrodes are also placed on the surface of the skull over the area of the brain where the impulse from the limb is received. A machine is used to monitor the electrical activity in the brain just like an electroencephalogram (EEG). The electrical activity is recorded as waves. When the limb is stimulated with an electrical current by the surgeon or technician, there should be a response in the brain. This checks the function of the sensory portion of the nerves and spinal cord.
Somatosensory evoked potentials (SSEPs) are the most widely used intraoperative neurophysiological monitoring during surgery. However, SSEP monitoring may not detect injuries to individual nerve roots.
In the 1980’s surgeons began using electromyography (EMG) to monitor the motor portion of the nerves during spinal surgery. It is becoming more commonly used. During surgery, while the patient is asleep, needle electrodes are placed in the muscle groups that correspond to the area where the surgeon will be working. Electrical activity from the muscle can be monitored by a machine. The activity is recorded as waves, similar to the SSEP monitor. It is also similar to the waves that are recorded from the heart muscle during an electrocardiogram (ECG). Baseline recordings are taken before the surgery begins. Recordings are then repeated throughout the procedure. A significant change in the wave alerts the surgeon or technician that the nerve in the area could be damaged. The surgeon can then take action to prevent permanent damage.
EMG seems to be more accurate in identifying potential neurological damage than other methods of monitoring that have been used. However, it is not useful when muscle paralyzing agents are used for anesthesia. It is also not useful if a nerve root has been cut completely.
Studies show that the use of both SSEPs and EMG monitoring during spinal surgery is most ideal but not always available.
Other monitoring available includes rectal and urinary sphincter electromyography, motor-evoked potentials (MEPs), transcranial electrical stimulation (TES), brainstem auditory evoked potential (BAEP), dermatomal evoked potentials (DEP), facial nerve monitoring, and spinal cord mapping.
Why is intraoperative monitoring important?
Spine surgery can be unpredictable and dangerous because it can involve areas near nerves and the spinal cord. During spinal surgery there is a risk that damage to the nervous system can occur. Intraoperative neurophysiological monitoring allows the surgeon to know, during the surgery, if/when nerve tissue is being injured or is at risk for being injured. The problem can be corrected immediately. Intraoperative neurophysiological monitoring (IOM) allows assessment of nerve tissue function while the surgery is taking place. Many complications involving the nervous system can be avoided with careful monitoring during surgery. This makes spine surgery safer. It is also proven to improve the outcomes of spinal surgery. It is being used more commonly, especially during complicated spinal surgery.
Spine surgery often involves the use of instrumentation (hardware). This hardware may include screws, rods, plates, and cages. The complication rate from instrumentation with lumbar spine fusion varies from one to 33 per cent. Possible complications from placement of hardware include damage to the spinal cord and nerve roots. Up to 10 per cent of the time, pain and sensory changes in the portion of the limb affected can result. This is called radiculopathy. One per cent of the time, motor change or weakness in the portion of the limb affected at that surgical level can occur. This is called myelopathy. Neither of these outcomes is desirable after spine surgery.
Surgeons have relied on imaging, most usually X-rays and computed tomography (CT) scans to check the placement of hardware during surgery. However, there are times when these do not show improperly placed hardware, fracture of spinal bone, or damage to nerve tissue.
Intraoperative neurophysiological monitoring (IOM) is more effective in sensing neurological damage, and misplacement of hardware. In fact, some studies show that it is one-third more effective than imaging with X-ray or CT scan.
Until intraoperative neurophysiological monitoring, surgeons commonly relied on the wake up test and the clonus test to evaluate nerve function during surgery. However, these are more difficult to repeat during the surgery, can lengthen the time of surgery, and do not fully evaluate nerve function. The wake up test involves allowing the patient to wake up from the anesthesia. The patient is then asked to move body parts that may be affected by the surgery. The clonus test involves the surgeon quickly jerking the foot towards the shin to see if the stretch reflex still works. This assesses the function of the spinal cord.
Intraoperative neurophysiological monitoring (IOM) is quick, painless, easy, and inexpensive. Recordings can be taken several times during surgery or even throughout the entire procedure. It does not cause harm to the patient. It also provides real-time feedback to the surgeon. It is safe and effective for reducing nerve tissue damage during surgery.
When is intraoperative monitoring used for spinal surgery?
Some spine surgeons may prefer to use intraoperative monitoring during most (if not all) of their surgeries. Others prefer to use it during complex surgeries. It is commonly used for the following spinal surgeries:
- All spinal cord cases
- Spinal instrumentation with hardware
- Scoliosis
- Discectomy with a neurological deficit
- Decompression with a neurological deficit
- Total disc replacement
- Pain stimulator placement
- Corpectomy
- Vertebrectomy
- Odontoid/Dens fractures
What happens during surgery?
After you are put to sleep by the anesthesiologist, small wire electrodes are placed in the muscles of your lower leg for lumbar surgery. They may be placed in the arms for neck surgery. For EMG monitoring, the electrodes are placed in specific muscles that correspond with a specific level in the spinal cord.
Technically, EMG monitoring is relatively easy, and the setup takes practically no additional time during positioning for the surgical procedure.
Intraoperative monitoring is technically done by a technician who is in the operating room during the entire procedure. A neurophysiologist may be involved in interpreting the recordings generally at a remote location where they observe the same data as seen by the technologist. This real-time interpretation by an experienced neurophysiologist is the standard of care in many regions in the United States.
If the spinal cord or nerve roots are damaged while drilling into bone, placing hardware in the spine, or decompressing the spine, the SSEP or EMG signal will change. This alerts the technician who can then alert the surgeon. Some monitoring units are equipped with a loudspeaker that allows immediate audio feedback. The surgeon can make a change at that time to avoid damage to nerve tissue.
When pedicle screws are used, the surgeon may use a handheld probe that can give an electrical stimulation to the pedicle screw once it has been placed. If the screw is where it is supposed to be, it will take a certain amount of current to cause a muscle contraction and wave on the monitor. If it is misplaced, it will take less. This is called an evoked EMG.
The surgeon can then re-evaluate the placement of the screw in order to avoid harm to the nerve root or spinal cord.
SSEPs and EMG recordings can be taken several times during the surgery if necessary without causing harm to the patient.
What are possible complications of intraoperative monitoring?
There really are none. The surgery need not be interrupted unnecessarily during surgery when neurophysiological monitoring is used. This is safer for the patient. Because the skin is penetrated with needle electrodes, there is a small risk for infection. This is minimal as the skin is disinfected before the needles are placed. The needles are sterile. They are thrown away after a single use. Mild soreness may be experienced where the needles were inserted.
Intraoperative monitoring is usually not costly. It is well worth it to avoid neurological complications during spinal surgery when possible.
Whiplash
A Patient’s Guide to Whiplash
Introduction
Whiplash is defined as a sudden extension of the cervical spine (backward movement of the neck) and flexion (forward movement of the neck). This type of trauma is also referred to as a cervical acceleration-deceleration (CAD) injury. Rear-end or side-impact motor vehicle collisions are the number one cause of whiplash with injury to the muscles, ligaments, tendons, joints, and discs of the cervical spine.
This guide will help you understand
- what parts make up the spine and neck
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts of the spine are involved?
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body’s main upright support.
The cervical spine is formed by the first seven vertebrae referred to as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom edge of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine. This is where the chest begins.
A bony ring attaches to the back of the vertebral body. When the vertebrae are stacked on top of each other, the rings form a hollow tube. This bony tube surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
As the spinal cord travels from the brain down through the spine, it sends out nerve branches between each vertebrae called nerve roots. The nerve roots that come out of the cervical spine form the nerves that go to the arms and hands.
Two spinal nerves exit the sides of each spinal segment, one on the left and one on the right. As the nerves leave the spinal cord, they pass through a small bony tunnel on each side of the vertebra, called a neural foramen. (The term used to describe more than one opening is neural foramina.)
Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at that level, and the small facet joints that link each level of the spinal column.
An intervertebral disc is made of connective tissue. Connective tissue is the material that holds the living cells of the body together. The disc is a specialized connective tissue structure that separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
There are two facet joints between each pair of vertebrae–one on each side of the spine. The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the bone ends to move against each other smoothly, without pain. The alignment of the facet joints of the cervical spine allows freedom of movement as you bend and turn your neck.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Causes
What causes this condition?
When the head and neck are suddenly and forcefully whipped forward and back, mechanical forces place excessive stress on the cervical spine. Traumatic disc rupture and soft tissue damage can occur.
The cartilage between the disc and the vertebral bone is often cracked. This is known as a rim lesion.
Damage to the disc can put pressure on the nerves as they exit the spine. The pressure or irritation can be felt as numbness on the skin, weakness in the muscles, or pain along the path of the nerve. Most people think of these symptoms as indications of a pinched nerve. Health care providers call this condition cervical radiculopathy.
Soft tissue around the facet joint can be injured. Many of the pain-sensing nerves of the spine are in the facet joints. The normally smooth surfaces on which these joints glide can become rough, irritated, and inflamed. Studies show that neck pain often comes from the damaged facet joints.
Low back pain is a common feature after a whiplash injury. Studies show that there is significant electrical activity in the muscles of the lumbar spine when the neck is extended. This effect increases when there is neck pain, possibly as a way to help stabilize the spine when neck pain causes weakness.
More than anyplace else in the body, the muscles of the neck sense sudden changes in tension and respond quickly. Tiny spindles in the muscles signal the need for more muscle tension to hold against the sudden shift in position.
The result is often muscle spasm as a self-protective measure. The increased muscle tone prevents motion of the inflamed joint. You may experience neck stiffness as a result.
Risk Factors
Each year, about three million people experience whiplash injuries to their neck and back. Of these three million people, only about one-half, will fully recover. About 600,000 of those individuals will have long-term symptoms, and 150,000 will actually become disabled as a result of the injury.
There are many factors that come into play when a person is injured in a rear-end motor vehicle accident. Any one or more of the following factors can affect recovery:
- Head turned one way or the other at the time of the impact (increases risk of nerve
involvement with pain down the arm) - Getting hit from behind (rear-impact collision)
- Previous neck pain or headaches
- Previous similar injury
- Being unaware of the impending impact
- Poor posture at the time of impact (head, neck, or chest bent forward)
- Poor position of the headrest or no headrest
- Crash speed under 10 mph
- Being in the front seat as opposed to sitting in the back seat of the car
- Collision with a vehicle larger than yours
- Being of slight build
- Wearing a seatbelt (a seat belt should always be worn, but at lower speeds, a lap and shoulder type seat belt will increase the chances of injury)
Symptoms
What are some of the symptoms of whiplash?
- Neck pain or neck pain that travels down the arm (radiculopathy)
- Headaches
- Low back pain (LBP)
- Jaw pain
- Dizziness
Ninety percent of patients involved in whiplash type accidents complain of neck pain. This is by far the most common symptom. The pain often spreads into the upper back, between the shoulder blades, or down the arm. Neck pain that goes down the arm is called radiculopathy.
Low back pain (LBP) can occur as a result of a whiplash injury. The Insurance Research Council reports that LBP occurs in 39 per cent of whiplash patients. Some studies found LBP to be present in 57 per cent of rear-impact collisions in which injuries were reported and 71 per cent of side-impact collisions.
Jaw pain as a result of temporomandibular joint (TMJ) injury can also cause painful headaches. The TMJ is formed by the bone of the mandible (lower jaw) connecting to the temporal bone at the side of the skull. The TMJ is a hinge joint that allows the jaw to open and close and to move forward, back, and sideways. Pain in this joint in called temporomandibular joint disorder (TMD).
Dizziness is quite common with a sense of lost balance being reported. It is caused by an injury to the joints of the neck called facet or zygapophyseal joints. When dizziness is reported, it should be distinguished from vertigo (also known as benign paroxysmal positional vertigo (BPPV), which results from an injury to the inner ear.
Other symptoms often reported include, but are not limited to: shoulder pain; numbness or tingling in the arms, hands, legs or feet; facial pain, fatigue, confusion, poor concentration, irritability, difficulty sleeping, forgetfulness, visual problems, and mood disorders.
It is not uncommon to have a delay in your symptoms. It is actually more common to have a 24 to 72 hour delay as opposed to immediate symptoms or pain. This is most likely due to the fact that it takes the body 24 to 72 hours to develop inflammation. Disc injuries may take even longer to manifest themselves. It is not uncommon for a disc injury to remain pain free and unnoticed for weeks to months.
Simply because there is little or no damage to your car does not mean that you were not injured. In fact, more than half of all whiplash injuries occur where there was little or no damage to one or both of the vehicles involved.
When we see visible damage to a car, it means that the car has absorbed much of that force and less force is transmitted to the occupant. On the other hand, if there is little or no damage to the car, the force is not absorbed but transferred to the driver or passengers, potentially resulting in greater injury.
Diagnosis
How do doctors diagnose the problem?
The diagnosis of neck problems begins with a thorough history of your condition and the involved car accident. You might be asked to fill out a questionnaire describing your neck problems. Then your doctor will ask you questions to find out when you first started having problems, what makes your symptoms better or worse, and how the symptoms affect your daily activity. Your answers will help guide the physical examination.
Your doctor will then physically examine the muscles and joints of your neck. It is important that your doctor see how your neck is aligned, how it moves, and exactly where it hurts.
Your doctor may do some simple tests to check the function of the nerves. These tests measure your arm and hand strength, check your reflexes, and help determine whether you have numbness in your arms, hands, or fingers.
The information from your medical history and physical examination will help your doctor decide which tests to order. The tests give different types of information.
Radiological Imaging
Radiological imaging tests help your doctor see the anatomy of your spine. There are many kinds of imaging tests including:
- X-rays
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Digital motion x-ray (DMX)
- Myelogram
- Bone Scan
- Electromyogram
X-rays
X-rays show problems with bones, such as infection, bone tumors, or fractures. X-rays of the spine also can give your doctor information about how much degeneration has occurred in the spine, such as the amount of space in the neural foramina and between the discs.
X-rays are usually the first test ordered before any of the more specialized tests. Special x-rays called flexion/extension x-rays may help to determine if there is instability between vertebrae. These x-rays are taken from the side as you bend as far forward and then as far backward as you can. Comparing the two x-rays allows the doctor to see how much motion occurs between each spinal segment.
Magnetic resonance imaging (MRI)
If more information is needed, your doctor may order an MRI. The MRI machine uses magnetic waves rather than x-rays to create pictures of the cervical spine in slices. MRIs show the cervical spine vertebrae, as well as the soft tissue structures, such as the discs, joints, and nerves. MRI scans are painless and don’t require needles or dye. MRI scan has become the most common test to look at the cervical spine after x-rays have been taken.
Computed Tomography (CT)
CT scan is a special type of x-ray that lets doctors see slices of bone tissue. The machine uses a computer and x-rays to create these slices. It is used primarily when problems are suspected in the bones.
Digital motion x-ray (DMX)
DMX is a new fluoroscopic based x-ray system designed to objectively detect and document soft tissue/ligament injury most commonly associated with whiplash injuries of the spine. DMX evaluates biomechanical relationships and abnormal movements of the cervical spine. Specifically, DMX:
- Shows abnormal movement of vertebral bodies, facets, and other spinal elements
- Shows joint hypermobility, hypomobility, or restriction
- Shows normal or abnormal initiation of cervical motion
DMX uses digital and optic technology now available. DMX is the latest generation of videofluoroscopy (VF) that uses low doses of radiation. The images have improved clarity and resolution over VF and are recorded digitally on CD or DVD disc. DMX digital images can be replayed and studied on standard computer systems. DMX images are simply x-ray images taken at 30 frames per second to form a multiple radiographic array or series that can be run as a movie file to display real time motion of the joints of the body.
DMX radiographic series can be paused at any location and the measurements and interpretation common to radiology can be applied to the still images. These images would be identical to plain film images if plain film radiography were performed at the same location at the same moment in motion. DMX acquires approximately 2700 images for the same amount of radiation as seven regular x-rays.
For more information visit http://www.dmxofmontana.com
Myelogram
The myelogram is a special kind of x-ray test where a special dye is injected into the spinal sac. The dye shows up on an x-ray. It helps a doctor see if there is a herniated disc, pressure on the spinal cord or spinal nerves, or a spinal tumor. Before the CT scan and the MRI scan were developed, the myelogram was the only test that surgeons had to look for a herniated disc. The myelogram is still used today but not nearly as often. The myelogram is usually combined with CT scan to give more detail.
Bone Scan
A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special x-rays of your neck. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem and other tests such as the CT scan or MRI scan are then used to look at the area in detail.
Electromyogram (EMG)
An electromyogram (EMG) is a special test used to determine if there are problems with any of the nerves going to the upper limbs. EMGs are usually done to see if one or more nerve roots have been pinched by a herniated disc. During the test, small needles are placed into certain muscles that are supplied by each nerve root. If there has been a change in the function of the nerve, the muscle will send off different types of electrical signals. The EMG test reads these signals and can help determine which nerve root is involved.
Grading the Severity of Injury
The physical exam combined with the imaging studies help determine the severity or grade of the injury. There is more than one way to assign a grade to a patient’s whiplash. Here are two examples of the more commonly used models used to classify or grade whiplash injuries:
Croft Guidelines
- Grade I: Minimal – No limitation of motion, no ligamentous injury, no neurological findings
- Grade II: Slight – Slight limitation of motion, no ligamentous injury, no neurologic findings
- Grade III: Moderate – Limitation of motion, ligamentous instability, neurologic symptoms present
- Grade IV: Moderate-to-Severe – Limitation of motion, some ligamentous injury, neurological symptoms, fracture or disc derangement
Quebec Whiplash Classification
- Grade 0: No complaint or physical sign
- Grade I: Neck complaint of pain, stiffness or tenderness, no physical signs
- Grade II: Neck pain and musculoskeletal signs
- Grade III: Neck pain and neurological signs
- Grade IV: Neck pain and fracture or dislocation
Treatment
What treatment options are available?
Nonsurgical Treatment
Whenever possible, doctors prefer to use treatments other than surgery. The first goal of these nonsurgical treatments is to ease your pain and other symptoms.
Your health care providers will work with you to improve your neck movement and strength. They will also encourage healthy body alignment and posture. These steps are designed to enable you to get back to your normal activities. Conservative care may include:
- Immobilization
- Medication
- Injection
- Physical therapy
- Chiropractic care
Immobilization
At first, your doctor may prescribe immobilization of the neck. Keeping the neck still for a short time can calm inflammation and pain. This might include one to two days of bed rest and the use of a soft cervical (neck) collar.
The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. A soft cervical collar may be used for the first 24 to 48 hours to help provide support and reduce pain. There is no need for a hard or rigid cervical collar unless the neck is fractured.
Soft collars should not be worn after 48 hours without a physician’s approval. Studies show that prolonged immobilization can delay healing and promote disability. Wearing it longer tends to weaken the neck muscles and reduces the facet joints’ sense of position called proprioception.
A cervical support pillow may offer some additional support while sleeping and helps to keep the neck in a more neutral position. Cervical pillows can be used any time by anyone for improved alignment while sleeping.
Medication
Your doctor may prescribe certain types of medication if the nerves are irritated or compressed and you have neck pain that travels down your arm (radiculopathy). Severe symptoms may be treated with narcotic drugs, such as codeine or morphine. But these drugs should only be used for the first few days or weeks after problems with radiculopathy start because they are addictive when used too much or improperly. Muscle relaxants may be prescribed to calm neck muscles that are in spasm. You may be prescribed anti-inflammatory medications such as aspirin or ibuprofen.
Injection
Pain resulting from irritation of the facet joints may be alleviated with injection of an anesthetic agent similar to Novacaine such as Bipuvacaine. This numbing agent both confirms the source of pain as coming from the joint and helps reduce or eliminate the pain.
Physical Therapy
Some doctors have their patients work with a physical therapist. If you require outpatient physical therapy, you will probably only need to attend therapy sessions for two to four weeks. Your rate of recovery helps determine the length of time in physical therapy. Patients with delayed recovery may need longer time in rehab.
At first, treatment is focused on easing pain and reducing inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Electrical stimulation treatments can help calm muscle spasm and pain. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or the therapist can apply the traction pull by hand. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are added within the comfortable range of motion. The therapist will teach you specific exercises to help tone and control the muscles that stabilize the neck and upper back.
Your therapist will work with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. You’ll learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, your therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job. Your therapist can also provide ideas for alternate forms of work. You’ll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Chiropractic care
Chiropractic care also offers another opportunity for relief of pain from a whiplash injury. Chiropractors adjust misalignments of the facet joints and vertebrae to restore the nerve signals and improve spinal health, which can impact overall physical health. Many chiropractors make these adjustments using a thrust technique called manipulation.
Chiropractors also take into account how nutrition, emotion, and environment affect our health. The chiropractor will assess your posture during daily activities, work, and sleep and offer you suggestions for ways to improve your day-to-day spinal alignment. You may be given some additional advice about the use of heat, cold, and exercise to help maintain the results of your chiropractic treatment.
Surgery
Most people with lingering effects from whiplash or cervical radiculopathy from whiplash get better without surgery. In rare cases, surgery may be suggested.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
You should expect full recovery to take up to three months. Integration of rehabilitation and manipulative therapy is central in getting back to your pre-injury status.
There is a strong emphasis on keeping as active as possible, which includes incorporating manual treatments and exercise. Before your rehab program ends, your healthcare team will teach you how to maintain any improvements you’ve made and ways to avoid future problems.
Cervical Artificial Disc Replacement
A Patient’s Guide to Cervical Artificial Disc Replacement
Introduction
Artificial disc replacement (ADR) is relatively new. In June 2004, the first ADR for the lumbar spine (low back) was approved by the FDA for use in the US. Replacing a damaged disc in the cervical spine (neck) is a bit trickier. The disc is part of a complex joint in the spine. Making a replacement disc that works and that will last is not an easy task. There are now several Cervical artificial disc replacement devices that have been approved by the FDA for use in the United States.
The artificial disc is inserted in the space between two vertebrae. The goal is to replace the diseased or damaged disc while keeping your normal neck motion. The hope is that your spine will be protected from similar problems above and below the affected spinal level.
This guide will help you understand:
- what parts of the spine are involved
- what your surgeon hopes to achieve
- who can benefit from this procedure
- how do I prepare for surgery
- what happens during the procedure
- what to expect as you recover
Anatomy
What parts of the spine are involved?
Disc replacement typically occurs at cervical spine levels C4-5, C5-6, or C6-7. The first seven vertebrae make up the cervical spine. Doctors often refer to the cervical vertebrae as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine (the chest area) at the first thoracic vertebra, T1.
Each vertebra is made of the same parts. The main section of each cervical vertebrae, from C2 to C7,
is formed by a round block of bone, called the vertebral body. A bony ring attaches to the back of the vertebral body. This ring has two parts. Two pedicles connect directly to the back of the vertebral body. Two lamina bones join the pedicles to complete the ring. The lamina bones form the outer rim of the bony ring. When the vertebrae are stacked on top of each other, the bony rings form a hollow tube that surrounds the spinal cord. The laminae provide a protective wall around the spinal cord.
On the left and right side of each vertebra is a small tunnel called a neural foramen. (Foramina is the plural term.) The two nerves that leave the spine at each vertebra go through the foramina, one on the left and one on the right. The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits behind the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
A special type of structure in the spine called an intervertebral disc has two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption in the spine. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
Related Document: A Patient’s Guide to Cervical Spine Anatomy
Rationale
What does the surgeon hope to achieve?
Disc replacement surgery is done to stop the symptoms of degenerative disc disease. Discs wear out or degenerate as a natural part of aging and from stress and strain on the neck. Eventually, the problem disc collapses. This causes the vertebra above to sink toward the one below. This loss of disc height affects the nearby structures – especially the facet joints.
When the disc collapses, it no longer supports its share of the load in the cervical spine. The facet joints of the spine begin to support more of the force that is transmitted between each vertebra. This increases the wear and tear on the articular cartilage that covers the surface of the joints. The articular cartilage is the smooth, slippery surface that covers the surface of the bone in any joint in the body. Articular cartilage is tough, but it does not tolerate abnormal pressure well for long. When damaged, articular cartilage does not have the ability to heal. This wear and tear is what is commonly referred to as arthritis.
Shrinking disc height also reduces the size of the neural foramina, the openings between each vertebral pair where the nerve roots leave the spinal column. The arthritis also results in the development of bone spurs that may protrude into these openings, further narrowing the space that the nerves have to exit the spinal canal. The nerve roots can end up getting squeezed where they pass through the neural foramina.
The traditional way of treating severe neck pain caused by disc degeneration is a procedure called an anterior cervical discectomy and fusion. In this procedure, the surgeon makes an incision in the anterior (front) of the neck, performs a discectomy (removes the disc) and fuses the two vertebrae together. A fusion simply means that two bones grow together. Usually, when two vertebrae are fused together, a small piece of bone called a bone graft is inserted between the two vertebrae where the disc has been removed. This bone graft serves to both separate the vertebrae and to stimulate the two bones to grow together – or fuse.
The fusion procedure usually involves the use of hardware, such as screws, plates, or cages to keep the bones from moving. Fusion restricts movement in the problem area, but it creates greater strain on the healthy spinal segments above and below. The added strain may eventually cause these segments to wear out. This is called adjacent-segment degeneration.
Replacing the damaged disc with an artificial disc, or implant, called a prosthesis can restore the normal distance between the two vertebrae. The artificial disc sits between the two vertebrae and “jacks up” the upper vertebra. Enlarging the disc space relieves pressure on the facet joints. It also opens up the space around the spinal nerve roots where they pass through the neural foramina.
Another benefit of the artificial disc replacement is that it mimics a healthy disc. Natural motion is preserved in the spine where the new disc is implanted. And it helps maintain stability in the spinal joints above and below it.
Who can benefit from this procedure
The indications for a cervical disc replacement are generally the same as for a cervical discectomy and fusion. A person must have symptoms from a cervical disc problem. Symptoms include neck and/or arm pain, arm weakness, or arm and hand numbness. These symptoms may be due to a herniated disc and/or bone spurs called osteophytes pressing on adjacent nerves or the spinal cord. This condition typically occurs at cervical spine levels C4-5, C5-6, or C6-7.
Artificial disc replacement is still somewhat new in the United States. In the United States, surgeons are currently only replacing one cervical disc in a patient’s cervical spine at this time. In Europe, surgeons are replacing more than one disc. More surgeons in the United States will probably start replacing more than one cervical disc in the near future.
Cervical artificial disc replacement is indicated for the treatment of radiculopathy (pressure on the spinal nerve) and myelopathy (pressure on the spinal cord) at one or two levels. In the future, it may be used for the treatment of three or more symptomatic levels or levels adjacent to a cervical spine fusion. This use is still under investigation.
More data is needed before the uses of cervical artificial disc replacements are expanded to other problems in the cervical spine. Cervical artificial disc replacement is not advised when there is cervical spine instability, significant facet joint damage, or infection.
Preparation
How should I prepare for surgery?
Your spine surgeon will gather a variety of information before recommending disc replacement surgery. In addition to taking a history and doing a physical exam, your surgeon may order various diagnostic studies, such as x-rays, magnetic resonance imaging (MRI) scans, CT scans, or discograms.
Once you and your surgeon have agreed that disc replacement surgery is indicated, certain preparations for the surgery are important. Your doctor may tell you to be NPO for a certain amount of time before the procedure. This means that you should not eat or drink anything for a certain amount of time before your procedure. This means no water, no coffee, no tea – not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You should tell your doctor if you are taking any medications that thin your blood or interfere with blood clotting. The most common blood thinner is Coumadin. Other medications also slow down blood clotting. Aspirin, ibuprofen, and nearly all of the anti-inflammatory medications affect blood clotting. So do medications used to prevent strokes such as Plavix. These medications usually need to be stopped seven days prior to the procedure. Be sure to let your doctor know if you are on any of these medications.
You should stop smoking or using tobacco in any form as soon as possible before surgery. This is very important to reduce complications from heart and lung problems. Tobacco use, especially smoking, also decreases the success rate of spine surgery. Stopping smoking will increase your chances of a successful result.
Discussions will be held with your family and people who may be assisting you once you return from the hospital. You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition possible prior to the surgery.
Hospitals often have preoperative teaching for patients undergoing major spinal operations. These teaching sessions can help you understand what to expect both while you are in the hospital and after you return home. A doctor who will be performing your anesthesia (an anesthesiologist) will evaluate and counsel you regarding anesthesia.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the artificial disc itself.
The cervical artificial disc has several different designs. Some look like a sandwich with two endplates separated by a plastic spacer. The two endplates are made of cobalt chromium alloy, a safe material that has been used for many years in replacement joints for the hip and knee.
A plastic (polyethylene) core fits in between the two metal endplates. The core acts as a spacer and is shaped so that the endplates pivot in a way that imitates normal motion of the two vertebrae. There are small prongs on one side of each endplate. The prongs help anchor the endplate to the surface of the vertebral body.
Another artificial disc replacement design is a ball and socket articulation to allow for normal translation of motion at that segment. The implant may be made of titanium and polyurethane in a metal-on-plastic design. Some are made of stainless steel and are all metal-on-metal.
Inserted between two vertebrae, the prosthesis reestablishes the height between two vertebrae. As a result of enlarging the disc space, the nearby spinal ligaments are pulled tight, which helps hold the prosthesis in place. The prosthesis is further held in place by the normal pressure through the spine.
The Operation
The operation is done from the anterior (front) of the body. This surgical approach is the same as that presently used for a discectomy and fusion operation. To do this, the patient is placed on his or her back. An incision is made through the skin and the thin muscles of the front of the neck. The blood vessels, the trachea (windpipe), and the esophagus are moved to the side so that the surgeon can see the front of the cervical spine. The disc that is to be replaced is identified using the fluoroscope. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure.
Working from the front of the spine, the spine surgeon removes a large section from the middle of the damaged disc. Next, the bones of the spine are spread apart to make more room to see and work inside the disc space. Using a surgical microscope, any remaining disc material toward the back of the disc is removed. The surgeon will also remove any disc fragments pressing against the nerve and shave off any osteophytes (bone spurs).
The disc space is distracted (jacked up) to its normal disc height. This step helps decompress or take pressure off the nerves. At this point, x-rays or a fluoroscope, is used to insert the artificial disc device into the prepared disc space. This allows the doctor to watch where the implant goes as it is inserted. This makes the procedure much safer and much more accurate.
Finally, the prosthesis is tested by moving the spine in various positions. An X-ray may be taken to double check the location and fit of the new disc.
View animation of artificial disc replacement
Complications
What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Weigh these as you gather advice and information. Be sure to discuss the possible risks of disc replacement with your spine surgeon.
Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
However, information from the disc replacement operations shows a low rate of complications. There have been no reports of death, significant infection, or major neurological problems.
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are
- anesthesia complications
- thrombophlebitis
- infection
- blood loss
- nerve injury or paralysis
- spontaneous ankylosis (fusion)
- subsidence (sinking)
- implant failure (need for further surgery)
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Blood Loss
Cervical disc replacement surgery carries risks associated with operating from the front of the spine. Blood vessels that travel near the front of the spine may be injured during anterior cervical surgery.
Nerve Injury
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Spontaneous Ankylosis (fusion)
Some things can go wrong with any implant. In the case of artificial disc replacements for the cervical spine, sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of neck motion is the main side effect of this problem.
Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may not affect the implant or your final results in terms of motion or function.
Some patients are left with pain, numbness, and weakness. This can occur when there’s been incomplete neurologic decompression. In other words, there is still pressure on the spinal cord or spinal nerves.
Subsidence (sinking)
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Implant Failure (need for further surgery)
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal artificial disc replacements. In rare cases, the artificial disc replacement can dislocate.
After Surgery
What happens after surgery
Most people spend one or two days in the hospital. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty. Patients generally recover quickly after the artificial disc procedure.
You should be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your neck (bending backward). You may need to wear a brace or soft collar for a short while after the operation to support your neck muscles.
As you recover in the hospital, a physical therapist may see you one or two times each day until you go home. You’ll be shown ways to move, dress, and do activities without putting extra strain on your neck. Your therapist will help you begin a walking program in the hospital. You are encouraged to continue the walking program when you return home.
When you leave the hospital, there are very few activity restrictions. You should be safe to sit, walk, and drive. However, you should avoid lifting items for at least four weeks. Your surgeon will probably release you to return to work in two to four weeks. If your job requires moving and lifting heavy items, you may require a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery.
If you spend large amounts of time in front of a computer or other machine, you may need to change the height and angle of your work surface and/or the computer. Finding a position that puts minimal stress on your neck is important. You should avoid spending hours in one position reading, sewing, or doing other handwork. The therapist can help you find optimal positions and advise you about ways to stretch your neck muscles.
Rehabilitation
What should my recovery be like?
Your surgeon may prescribe outpatient physical therapy within one to two weeks after surgery. Plan on attending therapy two to three times each week for four to six weeks.
The first few visits include treatments to calm soreness and pain from the operation. Your therapist may apply gentle soft-tissue treatments such as massage. Ice and electrical stimulation are also commonly used to calm muscle spasm and to help take away any lasting pain.
Your therapist will teach you how to protect your neck. You’ll learn ways to position your neck when you sleep, sit, and drive. And you’ll be shown ways to keep your neck safe during routine activities, such as getting in or out of bed, getting dressed, and washing your hair.
Many patients are afraid to move the head and neck for fear of damaging or dislodging the disc. Using normal motion for everyday activities will not harm your new disc in any way. Your therapist will help you learn how to move your neck and show you any limits necessary.
Active treatments are used to improve flexibility, strength, and endurance. Gentle stretching exercises for the neck are commonly prescribed. You’ll begin a series of strengthening exercises to help tone and control the muscles that stabilize the neck and upper back. It is also important to build strength in your arms. Endurance exercises may include treadmill walking, swimming, or stationary biking.
When your symptoms are under control and you’re comfortable doing your exercises, your formal therapy sessions will end. You’ll continue your exercises as part of a home program.
Summary
Artificial disc replacement offers an alternative to cervical fusion for some patients who have chronic neck pain from degenerative disc disease. While fusion stops pain by eliminating movement in the problem spinal segment, ADR allows natural motion in the part of the spine where the disc is implanted. This is because the prosthesis is designed to imitate normal movement between adjacent vertebrae.
A successful result means that your painful symptoms are better but not necessarily perfect. You can expect to have significantly less neck pain and greatly improved function with the operation. You can expect to discontinue the use of strong medications.
But remember, no one can guarantee that you’ll be free of pain or that your spine will be totally flexible after this type of surgery. The idea that preserving motion will decrease adjacent segment degeneration hasn’t been proven yet. Long-term results (10 or more years) are unavailable.
Lumbar Artificial Disc Replacement
A Patient’s Guide to Lumbar Artificial Disc Replacement
Introduction
Artificial disc replacement (ADR) is a device or implant used to replace a diseased or damaged intervertebral disc. After removing what’s left of the worn out disc, the ADR is inserted in the space between two lumbar vertebrae. The goal is to replace the diseased or damaged disc while keeping your normal spinal motion. Artificial disc surgery is relatively new in the United States but has been used in Europe for many years. In the U.S., the first lumbar artificial disc surgery was done in clinical trials in October 2001. The Federal Drug Administration (FDA) approved the use of the lumbar ADRs in October 2004.
This guide will help you understand:
- what parts of the spine are involved
- what your surgeon hopes to achieve
- who can benefit from this procedure
- what happens during the procedure
- what to expect as you recover
Anatomy
What parts of the spine are involved?
The human spine is made up of 24 spinal bones called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column gives the body its form. It is the body’s main upright support. The section of the spine in the lower back is known as the lumbar spine. Lumbar disc replacement typically occurs in the lumbar spine (from L4-S1).
An intervertebral disc sits between each pair of vertebrae. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
An intervertebral disc is made of two parts. The center, called the nucleus is spongy. It provides most of the disc’s ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are connective tissues that attach bones to other bones.
Between the vertebrae of each spinal segment are two facet joints. The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
From the side, the spine forms three curves. The neck, called the cervical spine, curves slightly inward. The middle back, or thoracic spine, curves outward. The outward curve of the thoracic spine is called kyphosis. The low back, also called the lumbar spine, curves slightly inward. An inward curve of the spine is called lordosis.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Rationale
What does the surgeon hope to achieve?
Disc replacement surgery is done to stop the symptoms of degenerative disc disease. Discs wear out or degenerate as a natural part of aging and from stress and strain on the spine. Eventually, the problem disc collapses, which causes the vertebra above to sink toward the one below. This loss of disc height affects nearby structures – especially the facet joints.
When the disc collapses it no longer supports its share of the load in the spine. The facet joints of the spine begin to support more of the force that is transmitted between each vertebra. This increases the wear and tear on the articular cartilage that covers the surface of the joints. The articular cartilage is the smooth, slippery surface that covers the surface of the bone in any joint in the body. Articular cartilage is tough, but it does not tolerate abnormal pressure well for long. When damaged, articular cartilage does not have the ability to heal. This wear and tear is what is commonly referred to as arthritis.
Shrinking disc height also reduces the size of the neural foramina, the openings between each vertebral pair where the nerve roots leave the spinal column. The arthritis also results in the development of bone spurs that may protrude into these openings further narrowing the space that the nerves have to exit the spinal canal. The nerve roots can end up getting squeezed where they pass through the neural foramina.
Replacing the damaged disc with an artificial disc, or implant, called a prosthesis can restore the normal distance between the two vertebrae. The artificial disc sits between the two vertebrae and distracts or “jacks up” the upper vertebra. Enlarging the disc space relieves pressure on the facet joints. It also opens up the space around the spinal nerve roots where they pass through the neural foramina.
Another benefit of the artificial disc replacement is that it mimics a healthy disc. Natural motion is preserved in the spine where the new disc is implanted. And it helps maintain stability in the spinal joints above and below it.
Who can benefit from this procedure?
For many years, the standard of care for chronic pain from a degenerated disc has been spinal fusion surgery. Bone graft donated by a bone bank or taken from your pelvic bone is used to fuse two or more vertebral bones together. The spine is stabilized but you will lose motion at that level. The increased stress on the next lumbar vertebra can cause problems later.
The artificial disc replacement is used to reduce or eliminate the pain while still allowing motion. One advantage of the artificial disc is that it may also prevent premature breakdown of adjacent levels of the lumbar spine.
You may be a good candidate for a lumbar artificial disc replacement if you have chronic pain and disability from lumbar disc degeneration despite nonoperative treatment for at least six months. The artificial disc replacement provides an alternative to spinal fusion. The device helps restore the normal space between two vertebrae. You will still have movement at the level where the ADR is implanted.
Preparation
How should I prepare for surgery?
Knowing what to expect before and after surgery can help you plan for recovery at home. Once you and your surgeon have agreed that disc replacement surgery is indicated, certain preparations for the surgery are important.
You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition prior to the surgery. A doctor who will be performing your anesthesia (an anesthesiologist) will evaluate and counsel you regarding anesthesia.
Certain factors put you at increased risk for problems during or after the operation. It’s best to reduce or eliminate as many of these risk factors as possible. For example, the use of alcohol or other drugs (including tobacco) can be major factors in how your body copes with anesthesia and the stress of surgery.
You should stop any anti-inflammatory medications 10 days before surgery. If you aren’t sure which medications this includes, ask your doctor. You should stop smoking or using tobacco as soon as possible but at least two weeks before surgery. This is very important to reduce complications from heart and lung problems. Smoking also decreases the success rate of spine surgery. Stopping smoking will increase your chance of a successful result.
You may need to donate one or two units of your own blood. This blood will be stored in the blood bank until surgery. If you need a transfusion either during or after your surgery you will receive your own blood back.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. Let your surgeon know if you have diabetes and how you manage it (insulin pump, insulin injections, diet, exercise). Your need for insulin can change as a result of the stress of hospitalization and surgery. Even if you are tightly controlled now, you should monitor your glucose levels closely for at least a week before surgery and continue to do so for several weeks after surgery.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the artificial disc itself. The lumbar artificial disc has several different designs. They are made of metal, ceramic, and plastic. Some look like a sandwich with two endplates separated by a plastic spacer. The two endplates are made of cobalt chromium alloy, a safe material that has been used for many years in replacement joints for the hip and knee.
A plastic (polyethylene) core fits in between the two metal endplates. The core acts as a spacer and is shaped so that the endplates pivot in a way that imitates normal motion of the two vertebrae. There are small prongs or teeth on one side of each endplate. The teeth help anchor the endplate to the surface of the vertebral body.
Another way of anchoring the artificial disc replacement is the central keel or fin design. The implant is secured to the vertebral end plates by a thin, upright piece of metal that looks like the rudder on a boat or a shark’s fin.
Another artificial disc replacement design is a ball and socket articulation to allow for normal translation of motion at that segment. The implant may be made of titanium and polyurethane in a metal-on-plastic design. Some are made of stainless steel and are all metal-on-metal.
Inserted between two vertebrae, the prosthesis reestablishes the height between two vertebrae. As a result of enlarging the disc space, the nearby spinal ligaments are pulled tight, which helps hold the prosthesis in place. The prosthesis is further held in place by the normal pressure through the spine.
The lumbar artificial disc replacement comes in a variety of sizes and angles. There are constrained and unconstrained designs. The constrained devices provide a fixed center of rotation that doesn’t change. The unconstrained design allows the center of the implant to move forward and back slightly during lumbar motion. The surgeon can also choose an implant with the correct angle for each patient in order to build in the right amount of lordosis (spinal curvature).
The Operation
Lumbar ADR is done through the anterior ( front) of the spine. For your safety there are usually two surgeons present; your spine surgeon and a general or vascular surgeon.
The new system is placed in the spine through an incision though the abdomen or belly. Working from the front of the spine through the abdomen, the organs are carefully moved to one side. This makes it easier to see the front of the spine. The spine surgeon removes a large section from the middle of the damaged disc.
Next, the bones of the spine are spread apart to make more room to see and work inside the disc space. Using a surgical microscope, any remaining disc material toward the back of the disc is removed. The surgeon will also remove any disc fragments pressing against the nerve and shave off any osteophytes (bone spurs).
The disc space is distracted (jacked up) to its normal disc height. This step helps decompress or take pressure off the nerves. At this point, x-rays or a fluoroscope, is used to insert the artificial disc device into the prepared disc space. The fluoroscope is an x-ray machine that allows the surgeon to actually see an x-ray image while doing the procedure. Using a fluoroscope, the surgeon is able to see where the implant goes as it is inserted. This makes the procedure much safer and much more accurate.
Finally, moving the spine in various positions tests the prosthesis. An X-ray may
be taken to double check the location and fit of the new disc.
Complications
What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Complications from any kind of surgery can also occur from anesthesia, infection, and development of blood clots (thrombophlebitis). Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
Your spine surgeon will discuss the most common complications with you. This document will help you prepare any questions you may have. It doesn’t provide a complete list of all the possible complications. Complications from the artificial disc replacement procedure are rare and are lower than for spinal fusion. Results continue to improve with advances in technology and better surgical techniques. The more common problems may include but are not limited to:
- problems with anesthesia
- thrombophlebitis (blood clots)
- infection
- nerve damage or paralysis
- spontaneous ankylosis (fusion)
- problems with the implant
- retrograde ejaculation (men only)
- ongoing pain
Anesthesia Complications
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs you may be taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can happen after any operation. It occurs when blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
Nerve Damage or Paralysis
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping, stretching, or cutting the nerve tissue with a surgical instrument. Nerve involvement can cause nerve pain, muscle weakness, and a loss of sensation to the areas supplied by the nerve.
These symptoms are usually temporary and will gradually go away in one to three months’ time. Swelling around the nerve or the formation of scar tissue can also result in pressure or traction on the nerve. Scar tissue called fibrosis does not always resolve resulting in chronic pain and long-term weakness and sensory changes.
Spontaneous Ankylosis
Scientists aren’t sure why but sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of spinal motion is the main side effect of this problem. Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may or may not affect the implant or your final results in terms of motion or function.
Problems with the Implant
The prosthesis itself can sometimes be a source of complications. Although rare, the prosthesis can shift out of its normal position and even dislocate. If the implant migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align or replace the implant.
And similar to other types of joint replacements, the artificial disc may fail over time if the parts wear out. Your ADR is estimated to last 15 to 20 years. If the disc moves out of position or wears out, it can be removed. When surgery is done to take out the original prosthesis, a fusion surgery will most likely be recommended.
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal ADRs.
Retrograde Ejaculation
Lumbar disc replacement surgery carries risks associated with operating from the front of the spine. In men, the anterior approach can also sometimes result in a complication called retrograde ejaculation.
Tiny nerves in front of the lower spine may be damaged during the anterior approach. If so, semen enters the bladder instead of going out through the urethra during ejaculation. Male patients planning a family might wish to consider donating sperm before surgery. Studies have not reported cases of sexual dysfunction but it is a potential risk.
Ongoing Pain
Not all patients get complete pain relief with this procedure. As with any surgery, patients should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
You may have immediate relief from your painful symptoms, but many people notice a gradual improvement over the next weeks to months. Many patients are able to reduce or eliminate the use of pain medication as well.
Your hospital stay will depend on how quickly you recover but most people are able to go home by the third day after surgery. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty.
Most people recover quickly after the artificial disc procedure. You will be getting up out of bed and walking the same day as your surgery. You may even be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your back (bending backward). You probably won’t need a back brace or other support while the tissues are healing.
When you go home, you should be safe to sit, walk, drive, and ride a bike. Lifting anything more than eight to 10 pounds should be avoided for at least four weeks. To help you gauge what you can and can’t lift, keep in mind that a gallon of milk weighs about eight pounds.
Your surgeon will continue to follow-up with you. X-rays will be done from time to time to make sure the implant is still in its proper place. Your surgeon will let you know when you can return to work. Depending on the type of work you do, this should be in about two to four weeks. If your job requires moving and lifting heavy items, you may need a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery. You can expect to return to previous recreational activity by the end of three months.
Rehabilitation
What should I expect as I recover?
While you are in the hospital, a physical therapist will see you each day and advise you about ways to move. You’ll be shown how to do your daily activities without putting extra strain on your back.
Before you leave the hospital, you will have a home program of exercises and activities to help you regain motion and function. It’s important to continue with your walking program on a daily basis when you go home. Your goal should be to walk at least 30 minutes at a moderately brisk pace at least five days each week.
Your surgeon may prescribe outpatient physical therapy within one to two weeks after surgery. Plan on attending therapy two to three times each week for about four to six weeks. Active treatments are used to improve flexibility, strength, and endurance. Gentle stretching exercises for the back are commonly prescribed. You’ll begin a series of strengthening exercises to help tone and control the muscles that stabilize the trunk and back. It is also important to build strength in your legs. Endurance exercises may include treadmill walking, swimming, or stationary biking.
When your symptoms are under control and you’re comfortable doing your exercises, your formal therapy sessions will end. You’ll continue your exercises as part of a home program.
Summary
Artificial disc replacement may offer an alternative to spinal fusion for some patients who have chronic back pain from degenerative disc disease. While fusion stops pain by eliminating movement in the problem spinal segment, artificial disc replacement allows natural motion in the part of the spine where the disc is implanted. This is because the prosthesis is designed to restore normal motion and height between adjacent vertebrae. Artificial disc replacement allows for an early return to function.
The implant is designed to withstand bending, twisting, compression and repeated loads during movement. For active adults, successful disc replacement should endure years of high loads without mechanical failure.
Long-term studies to assess the safety and effectiveness of artificial disc replacements are ongoing. Researchers are looking at the impact of the ADR on other discs and on the bony structures of the spine. So far results show a low rate of complications. There have been no reports of death, significant infection, or major neurological problems. Patient satisfaction is good to excellent in most, but not all, cases.
Posterior Lumbar Interbody Fusion
Patient’s Guide to Posterior Lumbar Interbody Fusion
Introduction
Posterior lumbar interbody fusion (PLIF) is a procedure used to treat problems such as disc degeneration, disc herniation, and spine instability. In this procedure, the surgeon works on the spine from the back (the posterior) and removes a spinal disc in the lower (lumbar) spine. The surgeon inserts bone graft material into the space between the two vertebrae where the disc was removed (the interbody space). The graft may be held in place with a special fusion cage. The goal of the procedure is to stimulate the vertebrae to grow together into one solid bone (known as a fusion). A fusion creates a rigid and immovable column of bone in the problem section of the spine.
This guide will help you understand
- what surgeons hope to achieve
- what happens during surgery
- what to expect as you recover
Anatomy
What parts of the spine and low back are involved?
This surgery is done through an incision in the low back. The incision reaches to the spinous processes, the bony projections off the back of the vertebrae. A large block of bone, called the vertebral body makes up the front section of each vertebra. The vertebral bodies are separated by a soft cushion
called an intervertebral disc.
On the back of the vertebral body, the lamina and pedicle bones form a protective ring around the spinal canal. The spinal nerves are enclosed in the spinal canal and exit through small openings on the sides of each vertebral pair, one on the left and one on the right. These passageways are called the neural foramina. (The term neural foramen describes a
single passageway).
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Rationale
What do surgeons hope to achieve?
This procedure is often used to stop symptoms from lumbar disc disease. Discs degenerate, or wear out, as a natural part of aging and also from stress and strain on the back. Over time, the disc begins to collapse, and the space decreases between the vertebrae.
Related Document: A Patient’s Guide to Lumbar Degenerative Disc Disease
When this happens, the openings around the spinal nerves (the neural foramina) narrow and may put pressure on the nerves. The long ligaments in the spine slacken due to the collapse in vertebral height. These ligaments may even buckle and put pressure on the spinal nerves.
View animation of degeneration
Pain from disc degeneration can come from a tear in the outer portion of the disc, from chemical inflammation inside the disc, or from a herniated disc that pushes on a nearby spinal nerve. Mechanical pain can also occur from excess movement within the problem part of the spine.
Discectomy is the removal of the disc and any fragments between the vertebrae that are to be fused. Taking out the painful disc is intended to relieve symptoms. It also provides room for placing a graft that will allow the two vertebrae to fuse together.
Once the disc is removed, the surgeon spreads the bones of the spine apart slightly to make room to implant bone graft material. Bone graft is commonly taken from the rim of the pelvis and packed in a special case, called a fusion cage. Bone taken from your own body is called autograft. Bone substitutes are also being used and avoid the need for taking bone from your pelvis.
Another option is to use a wedge of hard, cortical bone taken from preserved human bone. This source of bone graft is called allograft. During the PLIF procedure, the cage or bone wedge is implanted into the interbody space. The PLIF method provides a large surface area for fusion to occur.
The graft creates a solid spacer to separate and hold the vertebrae apart. Enlarging the space between the vertebrae widens the opening of the neural foramina, taking pressure off the spinal nerves that pass through these openings. Also, the long ligaments that run up and down inside the spinal canal are pulled taut so they don’t buckle into the spinal canal.
View animation of creating a spacer
The surgeon also fixes the bones in place using pedicle screws. This instrumentation (or hardware, as it is sometimes called) holds the vertebrae together and prevents them from moving. The less motion there is between two bones trying to heal, the higher the chance they will successfully fuse. The use of instrumentation has increased the success rate of spinal fusions considerably.
During the PLIF procedure, surgeons also commonly add bone graft material along the back sides of the spine. This step is called posterolateral bone grafting. When combined with instrumentation, this approach helps fuse a large surface area on the back (posterior column) of the spine.
In a successful fusion, the vertebrae that are fused together no longer move against one another. The fusion creates one solid bone. No movement happens within the bones that are fused. Instead, they move as one unit. This helps stop the mechanical pain that was coming from the moving parts of the back. Fusion also prevents additional wear and tear on the spinal segment that was fused. By fusing the bones together, surgeons hope to reduce future problems at the spinal segment.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
During surgery the patient usually kneels face down on a special operating table. The special table supports the patient so the abdomen is relaxed and free of pressure. This position reduces blood loss during surgery. It also gives the surgeon more room to work.
Two measurements are made before surgery begins. The first measurement ensures that the surgeon chooses a fusion cage or bone wedge that will fit inside the disc space. To correctly size the fusion cage or bone wedge, the surgeon uses an X-ray image to measure the disc space in a healthy disc, above or below the problem segment.
Second, to size the length of the pedicle screws, a CT scan is used to measure the length of the pedicle bone on the back of the vertebrae to be fused. The CT scan is a special type of X-ray that lets doctors see slices of bone tissue. The machine uses a computer and X-rays to create these slices.
To begin the procedure, an incision is made down the middle of the low back. The tissues just under the skin are separated. Then the small muscles along the sides of the low back are moved aside, exposing the back of the spinal column. Next, the surgeon takes an X-ray to make sure that the procedure is being performed on the correct vertebrae.
The bone graft is prepared. When autograft (bone taken from your body) is used, the same incision made at the beginning of the surgery can be used. The surgeon reaches through the first incision and opens the tissues that cover the back of the pelvis. An osteotome is used to cut the surface of the pelvis bone. An instrument is used to gather a small amount of the pelvis bone. The graft material is prepared and will later be packed into the fusion cages. The tissues covering the pelvis bone are sutured.
Then the surgeon prepares to implant bone graft into the space between the vertebral bodies. The surgeon removes the lamina bones that cover the back of the spinal canal. Next, the surgeon cuts a small opening in the ligamentum flavum, an elastic ligament separating the lamina bones and the spinal nerves. Removing the ligamentum flavum allows the surgeon to see inside the spinal canal. The nerves are checked for tension where they exit the spinal canal. If a nerve root is under tension, the surgeon enlarges the neural foramen, the opening where the nerve travels out of the spinal canal.
The surgeon locates the spot where the pedicle screws are to be placed. A fluoroscope is used to visualize the pedicle bones. A fluoroscope is a special type of X-ray that allows the surgeon to see an X-ray picture continuously on a TV screen. The surgeon uses the fluoroscope to guide one screw through the back of each pedicle, one on the left and one on the right.
The nerve roots inside the spinal canal are then pulled aside with a retractor so the problem disc can be examined. With the nerves held to the side, the surgeon is able to see the disc where it sits just in front of the spinal canal.
A hole is cut into the rim of the back of the disc. Forceps are placed inside the hole in order to clean out disc material within the disc. Reamers and scrapers are used to open up and remove additional disc material.
The surgeon prepares the disc space where the fusion cages or bone wedges are to be inserted. Special spreaders hold the two vertebral bodies apart. A layer of bone is shaved off the flat surfaces of the two vertebrae, causing the surfaces to bleed. Bleeding stimulates the bone graft to heal the bones together.
Adequate room is needed to get the bone graft implants through the spinal column and into the disc space. The nerve roots must be pulled as far to the side as possible to open up enough space.
With the disc space held apart by the spreaders, the surgeon has enough room to place the bone graft between the two vertebral bodies. For the fusion cage method, the surgeon packs two cages with bone taken from the pelvis bone or with a suitable bone substitute. Two cages are inserted, one on the left and one on the right. When allograft bone wedges are used, the surgeon inserts the wedges and aligns them within the disc space.
The surgeon uses a fluoroscope to check the position and fit of the graft.
The spreaders used to hold the disc space apart are released. Then the doctor tests the graft by bending and turning the spine to make sure the graft is in the right spot and is locked in place.
Some surgeons add strips of bone graft along the back of the vertebrae to be fused. This is called posterolateral fusion. The bones that project out from each side of the back of the spine are called transverse processes. The back surface of the transverse processes are shaved, causing the surfaces to bleed. Small strips of bone, usually taken from the pelvis bone at the beginning of the surgery, are placed over the transverse processes. The combination of this graft material with the pedicle screws helps hold the spine steady as the interbody fusion heals.
A drainage tube may be placed in the wound. The muscles and soft tissues are then put back in place. The skin is stitched together. The surgeon may place you in a rigid brace that straps across the chest, pelvis, and low back to support the spine while it heals.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following PLIF include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- problems with the implant or hardware
- nonunion
- ongoing pain
This is not intended to be a complete list of possible complications.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can happen after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the
blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional
surgery to treat the infected portion of the spine.
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar
tissue.
The nerve roots inside the spinal canal are especially at risk during the PLIF procedure. Retractors are used to hold the nerves aside and may cause muscle weakness and a loss of sensation to the areas supplied by an injured nerve. Pressure on the nerves that supply the bowels and bladder can cause incontinence. However, these types of nerve problems after PLIF usually go away soon after surgery.
Problems with the Implant or Hardware
Fusion surgery with cages requires bone grafting. The graft is commonly taken from the top rim of the pelvis (autograft). There is a risk of pain, infection, or weakness in the area where the graft is taken. These risks are avoided when a bone graft substitute is used in place of an autograft.
After the interbody implant is placed, the surgeon checks the position of the fusion cage or bone wedge before completing the surgery. However, the implant may shift slightly soon after surgery to the point that it is no longer able to hold the spine stable. If the implant migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align or replace the implant.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) When more than one level of the spine is fused at one time, there is a greater chance that nonunion will occur. (Fusion of more than one level means two or more consecutive discs are removed and replaced with bone graft.) If the joint motion from a nonunion continues to cause pain, the patient may need a second operation.
In the second procedure, the surgeon usually adds more bone graft. Additional instrumentation may also be needed to rigidly secure the bones so they will fuse together.
Ongoing Pain
PLIF is a complex surgery. Not all patients get complete pain relief with this procedure. As with any surgery, patients should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
Afterward
What happens after surgery?
Patients are sometimes placed in a rigid body brace after surgery. The surgical drain is removed within one to two days.
Patients usually stay in the hospital after surgery for three to five days. During this time, patients work daily with a physical therapist. The therapist demonstrates safe ways to move, dress, and do activities without putting extra strain on the back. The therapist
may recommend that the patient use a walker for the first day or two. Before going home, patients are shown ways to help control pain and avoid problems.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the fusion time to begin healing. Patients are cautioned against bending, lifting, twisting, driving, and prolonged sitting for up to six weeks. Outpatient physical therapy is
usually started a minimum of six weeks after the date of surgery.
Rehabilitation
What should I expect as I recover?
Rehabilitation after PLIF can be a slow process. Many surgeons prescribe outpatient physical therapy beginning a minimum of six weeks after surgery. This delay is needed to make sure the graft has time to begin to fuse. You will probably need to attend therapy sessions for two to three months. You should expect full recovery to take up to eight months.
At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are slowly added. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with. Swimming and use of a stairclimbing machine are helpful in the later phases of treatment. Therapists also teach
specific exercises to help tone and control the muscles that stabilize the low back.
Your therapist also works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your back in safe positions as you go about your work and daily activities. Training includes positions you use when sitting, lying, standing, and walking. You’ll also work on safe body mechanics with lifting, carrying, pushing, and pulling.
As your condition improves, the therapist tailors your program to prepare you to go back to work. Some patients are not able to go back to a job that requires strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job or to do alternate forms of work. You’ll learn to do these tasks in new ways that keep your back safe and free of strain.
Before your therapy sessions end, your therapist will teach you ways to avoid future problems.
Sacroiliac Joint Dysfunction
A Patient’s Guide to Sacroiliac Joint Dysfunction
Introduction
A painful sacroiliac joint is one of the more common causes of mechanical low back pain. Sacroiliac (SI) joint dysfunction is a term that is used to describe the condition – because it is still unclear why this joint becomes painful and leads to low back pain. Sacroiliac joint dysfunction can be a nuisance but it is seldom dangerous and rarely leads to the need for surgery. Most people who suffer from this problem can reduce the pain and manage the problem with simple methods.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the back is involved?
At the lower end of the spine, just below the lumbar spine lies the sacrum. The sacrum is a triangular shaped bone that is actually formed by the fusion of several vertebrae during development. The sacroiliac (SI) joint sits between the sacrum and the iliac bone (thus the name “sacroiliac” joint). You can see these joints from the outside as two small dimples on each side of the lower back at the belt line.
The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way Legos® fit together. Very little motion occurs in the SI joint. The motion that does occur is a combination of sliding, tilting and rotation. The most the joint moves in sliding is probably only a couple of millimeters, and may tilt and rotate two or three degrees.
The SI joint is held together by several large, very strong ligaments. The strongest ligaments are in the back of the joint outside of the pelvis. Because the pelvis is a ring, these ligaments work somewhat like the hoops that hold a barrel together. If these ligaments are torn, the pelvis can become unstable. This sometimes happens when a fracture of the pelvis occurs and the ligaments are damaged. Generally, these ligaments are so strong that they are not completely torn with the usual injury to the SI joint.
The SI joint hardly moves in adults. During the end of pregnancy as delivery nears, the hormones that are produced causes the joint to relax. This allows the pelvis to be more flexible so that birth can occur more easily. Multiple pregnancies seem to increase the amount of arthritis that forms in the joint later in life. Other than the role the joint plays in pregnancy, it does not appear that motion is important to the function of the joint. The older one gets, the more likely that the joint is completely ankylosed, a term that means the joint has become completely stiffened with no movement at all. It appears that the primary function of the joint is to be a shock absorber and to provide just enough motion and flexibility to lessen the stress on the pelvis and spine.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
There are many different causes of SI joint pain. Pregnancy may be a factor in the the development of SI joint problems later in life. Also, if a person has one leg is shorter that the other, the abnormal alignment may end up causing SI joint pain and problems. Often, an exact cause leading to a painful SI joint condition can’t be found. The joint simply gets painful, and the patient and provider don’t have an answer as to why the joint has become painful.
The SI joint is a synovial joint, similar to all joints such as the knee, hip and shoulder. Because of this, different types of arthritis that affect all the joints of the body will also affect the sacroiliac joint. This includes conditions such as rheumatoid arthritis, gout and psoriasis. The joint can be infected when bacteria that travel in the blood settle in the joint causing a condition called septic arthritis. This is perhaps the most worrisome cause of SI joint pain and may well require surgery to drain the infection.
Injury to the SI joint is thought to be a common cause of pain. Injury can occur during an automobile accident. One common pattern of injury occurs when the driver of a vehicle places one foot on the brake before a collision. The impact through the foot on the brake is transmitted to the pelvis causing a twisting motion to this side of the pelvis. This can injure the SI joint on that side resulting in pain. A similar mechanism occurs with a fall on one buttock. The force again causes a twisting motion to the pelvis and may injure the ligaments around the joint.
Symptoms
What does the condition feel like?
The most common symptoms from SI joint dysfunction are low back and buttock pain. The pain may affect one side or both SI joints. The pain can radiate down the leg all the way to the foot and may be confused with a herniated disc in the lumbar spine. The pain may radiate into the groin area. People often feel muscle spasm in one or both of their buttocks muscles.
Problems with the SI joint may make sitting difficult. Pain in one SI joint may cause a person to sit with that buttock tilted up. It is usually uncomfortable to sit flat in a chair.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history and physical exam. Your doctor will ask questions about your symptoms and how the pain is affecting your daily activities. Your doctor will also want to know what positions or activities make your symptoms worse or better. You will be asked about any injuries in the past and about any other medical problems you might have such as any arthritis that runs in the family.
Your doctor then examines you by checking your posture, how you walk and where your pain is located. Your doctor checks to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested because it is difficult to distinguish pain coming from the SI joint from pain coming from other spine conditions.
Laboratory tests may be ordered if there is any question whether you might have an infection or some type of arthritis affecting multiple joints. You may also need to have blood drawn and give a urine sample to send to the laboratory for special tests.
X-rays are commonly ordered of both the low back and pelvis. X-rays can give your doctor an idea about how much wear and tear has occurred in the SI joint. X-rays of the lumbar spine and hips are also helpful to rule out problems in these areas that may act and look like SI joint dysfunction.
Other radiological tests may be useful as well. The magnetic resonance imaging (MRI) scan can be used to look at the lumbar spine and pelvis in much more detail and to rule out other conditions in the area. The MRI scan uses magnetic waves rather than x-rays and shows a very detailed picture of the soft tissues of the body.
A computed tomography (CAT) scan may also be used to show a much more detailed look at the bone of the pelvis and the sacroiliac joint.
A bone scan is useful to see how the skeleton is reacting to any type of “stress,” such as an injury, an infection, or inflammation from arthritis. This test involves injecting chemical “tracers” into your blood stream. The tracers then show up on special spine X-rays. The tracers collect in areas where the bone tissue is reacting strongly to some type of stress to the skeleton, such as arthritis and infection of the SI joint.
The most accurate way of determining whether the SI joint is causing pain is to perform a diagnostic injection of the joint. Because the joint is so deep, this must be done using X-ray guidance with a fluoroscope (a type of realtime X-ray). Once the doctor places a needle in the joint, an anesthetic is injected into the joint to numb the joint. If your pain goes away while the anesthetic is in the joint, then your doctor can be reasonably sure that the pain you are experiencing is coming from the SI joint.
Treatment
What treatment options are available?
Nonsurgical Treatment
Doctors often begin by prescribing nonsurgical treatment for SI joint dysfunction. In some cases, doctors simply monitor the patient’s condition to see if symptoms improve. Anti-inflammatory medications, such as ibuprofen and naproxen, are commonly used to treat the pain and inflammation in the joint. Acetominiphen (for example, Tylenol) can be used to treat the pain, but it will not control the inflammation.
Your doctor may ask that you rest your back by limiting your activities. The purpose of this is to help decrease inflammation and calm the muscle spasm. Some patients benefit from wearing a special brace called a sacroiliac belt. This belt wraps around the hips to hold the sacroiliac joint tightly together, which may ease your pain.
Patients often work with a physical therapist. After evaluating your condition, a therapist can assign positions and exercises to ease your symptoms. The therapist may design an exercise program to improve the strength and control of your back and abdominal muscles. Some therapists are trained in manipulative techniques that attempt to treat the pain in this manner. You may be able to learn how to adjust your SI joint yourself and ease the symptoms. If your physical therapist is not trained in manipulation, he/she may be able to suggest a chiropractic physician or osteopathic physician in your area who can provide this treatment.
If conservative treatment is unsuccessful, injections may be suggested by your doctor. As described above, injections are used primarily to confirm that the pain is coming from the SI joint. A series of cortisone injections may be recommended to try to reduce the inflammation in and around the SI joint. Cortisone is a powerful anti-inflammatory medication that is commonly used to control pain from arthritis and inflammation. Other medications have been injected into the joint as well. A chemical called hyaluronic acid has been used for years to treat osteoarthritis of the knee. This chemical is thought to reduce pain due to its lubricating qualities and the fact that it nourishes the articular cartilage in the synovial joints. The true mechanism of action remains unknown, but it has been used with some success in the SI joint. All of these injections are temporary and are expected to last several months at the most.
Related Document: A Patient’s Guide to Sacroiliac Joint Injections
Another procedure that has been somewhat successful is called radiofrequency ablation. After a diagnostic injection has confirmed that the pain is coming from the SI joint, the small nerves that provide sensation to the joint can be “burned” with a special needle called a radiofrequency probe. In theory, this destroys any sensation coming from the joint, making the joint essentially numb. This procedure is not always successful. It is temporary but can last for up to two years. It can be repeated if needed.
Surgery
Surgery may be considered if other treatments don’t work. Surgery consists of fusing the painful SI joint. A fusion is an operation where the articular cartilage is removed from both ends of the bones forming the joint. The two bones are held together with plates and screws until the two bones grow together, or fuse, into one bone. This stops the motion between the two bones and theoretically eliminates the pain from the joint.
This is a big operation and is not always successful at relieving the pain. The operation is not commonly performed unless the pain is debilitating. SI joint pain is seldom this severe.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Doctors often recommend physical therapy for patients with SI joint dysfunction. Patients are normally seen a few times each week for four to six weeks. In severe and chronic cases, patients may need a few additional weeks of care.
When movement of a joint is limited, the pain and symptoms of SI joint dysfunction may worsen. Getting more motion can give you the relief you need for daily activities. If you don’t have full range of motion, your therapist has several ways to help you get more movement including joint manipulation, stretching, and exercises. Active movement and stretching as part of a home program can also help restore movement and get you better faster.
Therapists commonly prescribe a set of stretches to improve flexibility in the muscles of the trunk, buttocks, and thighs. In addition to the treatment you receive by your therapist, you may be given ways to help your own SI joint if your pain returns. These
exercises usually require that you position your hip and pelvis in a certain way and either stretch or contract and relax specific muscles. Follow the instructions of your therapist when doing these exercises.
If the SI joint has too much mobility and problems keep coming back, you may need extra help to stabilize the SI joint. You may be issued a SI belt to stabilize the joint. A belt like this can often ease pain enough to let you exercise comfortably.
You’ll learn some exercises to help you build strength, muscle control, and endurance in the muscles that attach around the SI joint. Unfortunately, few muscles actually connect to both the sacrum and the pelvis. Key muscles to work are the gluteus maximus, as well as the abdominal and low back muscles.
After Surgery
You will normally need to wait at least six weeks before beginning a rehabilitation program after having SI joint fusion surgery. You should plan on attending therapy sessions for six to eight weeks. Expect full recovery to take up to six months.
During therapy after SI joint surgery, your therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm your pain and muscle spasm. Then you’ll begin learning how to move safely with the least strain on the healing area.
As your rehabilitation program evolves, you’ll begin doing more challenging exercises. The goal is to safely advance your strength and function.
As your therapy sessions come to an end, your therapist helps you get back to the activities you enjoy. Ideally, you’ll be able to resume your normal activities. You may need guidance on which activities are safe or how to change the way you go about your
activities.
When treatment is well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource. But you’ll be in charge of doing your exercises as part of an ongoing home program.
Piriformis Syndrome
A Patient’s Guide to Piriformis Syndrome
Introduction
Pain in the buttock that radiates down the leg is commonly called sciatica. The most common cause for sciatica is irritation of the spinal nerves in or near the lumbar spine. Sometimes the nerve irritation is not in the spine but further down the leg. One possible cause of sciatica is piriformis syndrome. Piriformis syndrome can be painful, but it is seldom dangerous and rarely leads to the need for surgery. Most people with this condition can reduce the pain and manage the problem with simple methods, such as physical therapy.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the body are involved?
The lower lumbar spinal nerves leave the spine and join to form the sciatic nerve. The sciatic nerve leaves the pelvis through an opening called the sciatic notch.
The piriformis muscle begins inside the pelvis. It connects to the sacrum, the triangular shaped bone that sits between the pelvic bones at the base of the spine. The connection of the sacrum to the pelvis bones forms the sacroiliac joint. There is one sacroiliac joint on the left and one on the right of the low back. The other end of the piriformis muscle connects by a tendon to the greater trochanter, the bump of bone on the top side of your hip.
The piriformis muscle is one of the external rotators of the hip and leg. This means that as the muscle works, it helps to turn the foot and leg outward. Problems in the piriformis muscle can cause problems with the sciatic nerve. This is because the sciatic nerve runs under (and sometimes through) the piriformis muscle on its way out of the pelvis. The piriformis muscle can squeeze and irritate the sciatic nerve in this area, leading to the symptoms of sciatica.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
The symptoms of sciatica come from irritation of the sciatic nerve. It’s still a mystery why the piriformis muscle sometimes starts to irritate the sciatic nerve. Many doctors think that the condition begins when the piriformis muscle goes into spasm and tightens
against the sciatic nerve, squeezing the nerve against the bone of the pelvis.
In some cases, the muscle may be injured due to a fall onto the buttock. Bleeding in and around the piriformis muscle forms a hematoma. A hematoma describes the blood that has pooled in that area.
The piriformis muscle begins to swell and put pressure on the sciatic nerve. Soon the hematoma dissolves, but the muscle goes into spasm.
The sciatic nerve stays irritated and continues to be a problem. Eventually the muscle heals, but some of the muscle fibers inside the piriformis muscle are replaced by scar tissue. Scar tissue is not nearly as flexible and elastic as normal muscle tissue. The
piriformis muscle can tighten up and put constant pressure against the sciatic nerve.
Symptoms
What does the condition feel like?
Piriformis syndrome commonly causes pain that radiates down the back of the leg. The pain may be felt only on one side, though it is sometimes felt on both sides. The pain can radiate down the leg all the way to the foot and may be confused for a herniated disc in the lumbar spine. Changes in sensation and weakness in the leg or foot are rare. Some people say they feel a sensation of vague tingling down the leg.
Sitting may be difficult. Usually people with piriformis syndrome do not like to sit. When they do sit down, they tend to sit with the sore side buttock tilted up rather than sitting flat in the chair.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history and physical exam. Your doctor will ask questions about your symptoms and how the pain is affecting your daily activities. Your doctor will also want to know what positions or activities make your symptoms worse or better. You will be asked about any injuries in the past and about any other medical problems you might have such as any arthritis that runs in the family.
Next the doctor examines you by checking your posture, how you walk, and where your pain is located. Your doctor checks to see which back movements cause pain or other symptoms.
Your skin sensation, muscle strength, and reflexes are also tested because it is difficult to distinguish pain coming from the sacroiliac joint from pain coming from other spine conditions.
If there is any question whether you might have an infection or some type of arthritis affecting multiple joints, laboratory tests may be ordered. You may need to have blood drawn and give a urine sample to send to the laboratory for special tests.
X-rays are commonly ordered of both the low back and pelvis. X-rays can give your doctor an idea about how much wear and tear has developed in the sacroiliac joint. X- rays of the lumbar spine and hips are also helpful to rule out problems in these areas that may look and act like sacroiliac joint problems.
Other radiological tests may also be useful. A magnetic resonance imaging (MRI) scan can be used to look at the lumbar spine and pelvis in much more detail and rule out other conditions in the area conditions. The MRI scan uses magnetic waves rather than X-rays and shows a very detailed picture of the soft tissues of the body.
A special type of MRI scan called neurography is being used more frequently to look at nerves. This uses a regular MRI scanner, but the computer settings are set to look for areas of irritation along a nerve. This may change the way doctors use the MRI to diagnose nerve problems such as piriformis syndrome, thoracic outlet syndrome, and carpal tunnel syndrome.
A bone scan is useful to see how the skeleton is reacting to any type of “stress,” such as an injury, an infection, or inflammation from arthritis. Chemical “tracers” are injected into your blood stream. The tracers then show up on special spine X- rays. The tracers collect in areas where the bone tissue is reacting strongly to some type of stress to the skeleton, such as arthritis and infection of the sacroiliac joint.
The most accurate way to tell if the piriformis muscle is the cause of pain is with a diagnostic injection into the muscle. The muscle is deep inside the buttock, so the injection requires X-ray guidance with a fluoroscope, a CT scanner, or an open MRI machine. Once the needle is placed in the muscle, an anesthetic can be injected into the muscle to paralyze the piriformis muscle. If the pain goes away after the injection, your doctor can be reasonably sure that the pain you are feel is from piriformis syndrome.
Treatment
What treatment options are available?
Nonsurgical Treatment
Doctors often begin by prescribing nonsurgical treatment for piriformis syndrome. In some cases, doctors simply monitor their patients’ condition to see if symptoms improve. Anti-inflammatory medications, such as ibuprofen and naproxen, are commonly used to treat the pain and inflammation caused by the irritation on the nerve. Acetaminophen (for example Tylenol®) can be used to treat the pain but will not control the inflammation.
You’ll probably work with a physical therapist. After evaluating your condition, the therapist uses treatments to ease spasm and pain in the piriformis muscle. Exercises, particularly stretching exercises, are given to try and relieve irritation on the sciatic nerve.
If you still have pain after trying these treatments, your doctor may suggest injections.The main use of injections is to see if your pain is from piriformis syndrome. An injection of local anesthetic such as lidocaine can be injected into the muscle to temporarily relax it. This loosens up the muscle and reduces the irritation on the sciatic nerve. Other medications have also been injected into the piriformis muscle. Cortisone, for example, may be mixed with the anesthetic medication to reduce the inflammation on the sciatic nerve. Cortisone is a potent anti-inflammatory medication that is commonly used both in pill form and in injections to treat inflammation.
Related Document: A Patient’s Guide to Piriformis Muscle Injections
Botulism injection therapy (also known as Botox® injections) can be used to actually paralyze the piriformis muscle. This makes the muscle relax, which helps take pressure off the sciatic nerve. The effect of the Botox® injection isn’t permanent; it generally only lasts a few months. In the meantime, however, it is hoped that a stretching program can be used to fix the problem. In other words, when the injection wears off, the muscle may have been stretched enough so that the symptoms do not return.
Surgery
Surgery may be considered but usually only as a last resort. There are two procedures in use. The first is to cut the piriformis tendon where it attaches on the greater trochanter (the bump on the side of your hip). The other method is to cut through the piriformis muscle to take pressure off the sciatic nerve.
These procedures are usually done on an outpatient basis, meaning that you will be able to go home the same day as the surgery. In some cases, you may need to stay in the hospital for one night. Both procedures can be done under general anesthesia or under a spinal type of anesthetic.
The surgeon begins by making a small incision, usually about three inches long, in the buttock. The fibers of the gluteus maximus, the largest buttock muscle, are split. This gives the surgeon a way to see deep into the buttock and locate the piriformis muscle. When the piriformis muscle and tendon can be seen, the surgeon then cuts (releases) the tendon where it connects to the greater trochanter.
If more room is needed to release the pressure on the nerve, a portion of the piriformis muscle may be removed.
This usually doesn’t cause problems with strength because there are several much stronger muscles that help turn the leg outward.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Most patients with piriformis syndrome work with a physical therapist. Plan to attend physical therapy sessions two to three times each week for six to eight weeks.
Your therapist begins by evaluating your condition. This includes attention to the low back, as well as the sacroiliac and hip joints.
Physical therapy treatments for piriformis syndrome often begin with heat applications. Heat is used to help the piriformis muscle relax, easing spasm and pain. Your physical therapist may place a hot pack over your buttocks muscle.
Ultrasound is another treatment choice that can be set for deep heating in the buttock area. Ultrasound uses high frequency sound waves that are directed through the skin. The deep heating effect of ultrasound is ideal for preparing the piriformis muscle for hands-
on forms of treatment and for getting the muscle to stretch out.
Hands-on treatments such as deep massage and specialized forms of soft-tissue mobilization may be used initially. Your therapist may also position your hip and leg in a way that helps to relax nerve signals to the piriformis.
The keystone treatment for piriformis treatment is stretching. Stretching is especially effective following heat and hands on treatments. Your therapist will position you in ways that help you get a good stretch on the piriformis muscle. Along with the stretches
you’ll do in the clinic, you’ll be shown several ways to stretch the muscle on your own. You need to do your stretches every few hours. Be gentle and cautious as you stretch to avoid overdoing it.
As your symptoms ease, your therapist will gradually advance your program to include posture training, muscle strengthening, and general conditioning.
After Surgery
Your surgeon may prescribe physical therapy after surgery for piriformis syndrome. You’ll probably only need to attend sessions for four to six weeks. Expect full recovery to take up to three months.
During therapy after surgery, your therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. Then you’ll begin learning how to move safely with the least strain on the healing area.
As the rehabilitation program evolves, you’ll begin doing more challenging exercises. The goal is to safely advance strength and function.
As the therapy sessions come to an end, your therapist helps you get back to the activities you enjoy. Ideally, you’ll be able to resume normal activities. You may need guidance on which activities are safe or how to change the way they go about their activities.
When treatment is well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource. But you’ll be in charge of doing your exercises as part of an ongoing home program.