A Patient’s Guide to Chronic Pain and Sleep
Introduction
Sleep and pain problems are among the most common complaints in our society. It is not surprising then that these conditions frequently occur in the same person. Painful diseases such as backache, osteoarthritis, rheumatoid arthritis, headache, and fibromyalgia may interfere with sleep. However, poor sleep may also promote pain, headaches, and fatigue. Studies have shown that several nights of disturbed sleep in healthy people may cause not only sleepiness, but also nonspecific generalized muscle aching and fatigue.
This guide will help you understand
- the stages of sleep
- the importance of sleep to your body
- what can cause sleep disturbances
- what treatment options are available
Sleep is defined as the natural periodic suspension of consciousness during which the powers of the body are restored. Sleep is a complex process involving several stages. There are changes in the chemistry and behavior of the body during sleep.
There are many processes in the body that rely on the sleep-wake cycle. These processes are important in fighting infection, healing our body, and allowing processing of new knowledge or information. It is believed that sleep is crucial to learning and intellectual function. Proper sleep is absolutely necessary for the normal function of the body. Sleep disturbances can have significant and serious consequences. Lab rats die after two to three weeks of sleep deprivation.
Anatomy of Sleep
Circadian Rhythm
The circadian rhythm is a built-in cycle of sleep and wake times. There are other cyclic changes that occur in your body. These include changes in temperature, heart rate, blood pressure, hormone secretions, and lung function. These internal cycles are controlled by a group of nerve cells called a circadian pacemaker. This pacemaker is closely related to parts of the retina (in the back of the eye) and a small organ in the brain called the hypothalamus. Humans have a biological clock that is represented by a 24-hour cycle. Sunlight appears to be the cue that resets this clock on a daily basis.
The Human Sleep Cycle
There is a lot of difference in mammals’ need for sleep. Daily sleep time for man is approximately seven to eight hours. An owl monkey needs 17 hours a day. A bat needs 20 hours a day. Sleeping too little or too much can be harmful to a person’s health.
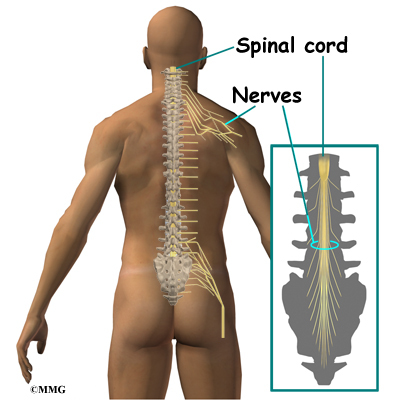
Human sleep occurs in cycles that are generally about 90 minutes long. There are five stages of sleep within each sleep cycle. These stages are further divided into two separate states, non-rapid eye movements (NREM) and rapid eye movement (REM). These stages are defined by brain wave activity using an electroencephalogram (EEG).
NREM sleep is the lighter stage of sleep. Body movements occur, but the mind is quiet. NREM is divided into four stages, with each stage of sleep getting progressively deeper.
REM sleep is deep sleep that is more refreshing. This is because there is total muscle relaxation except for bursts of rapid eye movements. The brain is active in REM sleep, dreaming occurs in this stage of sleep. Ideally, 20 to 50 percent of an adult’s sleep should be in REM sleep. During this phase of sleep, there may be irregularities of the heart and breathing. These can be recognized by monitoring the heart with an electrocardiogram (ECG). REM sleep has been described as a highly activated brain in a paralyzed body.
As sleep continues, the time spent in NREM sleep is decreased and the amount of time in REM sleep increases. The last third of the night is mostly REM sleep. It is linked to the circadian rhythm of body temperature.
There are age-related changes that are predictable. Infants usually start the sleep cycle with REM sleep. As we approach age 65 and older, less time is spent in REM sleep.
Causes
What causes this problem?
Some sleep disorders are known to have genetic causes. Others are caused by illnesses such as Parkinson’s disease, depression, lung disease, or heart failure. Other sleep disorders have an unknown cause. There are several common sleep disorders.
Sleep-Related Breathing Disorders or Sleep Apnea. Apnea means without breath. While sleeping, when a person stops breathing for a minimum of 10 seconds it is called an apneic episode. If you have more than five apnea events in an hour, you are diagnosed with sleep apnea. Oxygen level in the blood or tissues is also important when making the diagnosis of sleep apnea. Oxygen levels at 95 percent and above are normal. In sleep apnea, levels may drop to 80 percent or lower. Levels below 70 percent are considered dangerously low. When this low, the heart may beat irregularly and may even cause death.
There are two main types of sleep apnea.
Central sleep apnea is the interruption of breathing during sleep. The cause may be unknown. Or it can be caused by medications such as opioids (narcotics). Other causes can be heart failure, stroke, renal failure, lung disease, or being at high altitudes.
Obstructive sleep apnea (OSA) is caused by closing of the airway when air should be moving into the nose, mouth, and lungs. It may be as common as two to four of every 100 adults, and three out of every 100 children.
Narcolepsy is a term that is used for excessive daytime sleepiness without troubled sleep during the night. It is diagnosed when a person can fall asleep with a short delay (usually eight minutes or less) to REM sleep. Falling asleep while driving, hallucinations while sleeping, and sleep paralysis may occur. Narcolepsy appears to be genetic. A substance called hypocretin/orexin is found to be decreased in persons with narcolepsy. Narcolepsy is treated with medications.
Sleep-related movement disorders include restless legs syndrome (RLS) and periodic limb movement disorders (PLMD).
Restless legs syndrome (RLS) is described as a strong, nearly uncontrollable desire to move the legs. The sensations are worse at rest and occur more frequently in the evening or during the night. Walking or moving the legs relieves the sensation.
Periodic limb movement disorders (PLMD) is the involuntary limb movements which are often rhythmical that can fragment or interrupt sleep. Because they are rhythmical, they are thought to originate from a subcortical region of the brain. Possibly up to 40 percent of persons over 65 years of age may have PLMD.
Insomnia is difficulty falling asleep, staying asleep, or sleep that is not refreshing and restorative. It happens in as many as 30 percent of Americans. Symptoms of insomnia aside from difficulty sleeping include daytime exhaustion or fatigue, lack of energy, lack of concentration, forgetfulness, irritability, and depression. Insomnia can be caused by many different conditions. It happens more frequently as we age, particularly after 60. It may be caused by stress, depression and anxiety, or mental illness. Noise or extreme temperatures in the environment can also cause insomnia. Other causes of insomnia can be shift work, jet lag, nighttime activity schedules, and medication side effects. Use of alcohol, tobacco, and illicit drugs may interfere with sleep. A person with insomnia may also have one of the other sleep disorders such as sleep apnea, narcolepsy, or restless legs syndrome.
Unusual behaviors may occur during sleep. These behaviors include sleepwalking, sleep talking, tooth grinding, and other physical activities. These can cause arousals and get in the way of normal sleep cycles. Sleep related tooth grinding is called bruxism. Clenching of the teeth may cause tempomandibular joint pain and/or wearing down of the teeth. An appliance similar to a mouth guard or retainer may be used to treat bruxism.
Symptoms
What does the condition feel like?
Sleepiness is the most common symptom in people with a sleep disorder. Sleepiness is caused by the decrease in the amount, the quality of sleep, as well as the circadian rhythm of the body.
Fatigue and not feeling refreshed after sleeping, may be signs you have a sleep disorder.
Snoring and stopping breathing while sleeping are other symptoms of a possible sleep disorder.
Sleep disorders may be associated with many chronic illnesses such as high blood pressure, heart attacks, stroke, headache, or depression. There are many processes in the body that rely on the sleep-wake cycle. These processes are important in fighting infection, healing our body, and allowing processing of new knowledge or information. Sleep disturbances can have significant and serious consequences. Slower reaction times may decrease driving safety and cause auto accidents. Poor balance, decreased concentration, and forgetfulness are also noted in persons with sleep disorders. Mood disorders (irritability or depression), decreased motivation, and lack of energy may also be symptoms of chronic sleep problems.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history and physical examination. Your doctor will ask you several questions to determine if your symptoms call for a sleep study. You may be asked to fill out a questionnaire about snoring, sleepiness, stopping breathing during sleep, unwanted leg movements, medications you are taking and such.
Your doctor may do a physical exam. An examination of your nose, mouth, throat, and lungs is usually included. Your doctor may request that you have a chest x-ray. The x-ray is to check for abnormalities of your lungs, or to measure your heart size.
There are doctors who specialize in sleep medicine. You may be asked to be evaluated by one of them.
Examination of your nose and mouth is done to determine if there is decrease in the size of your airway, or factors that may interfere with proper airflow. Swollen sinuses from dryness or allergies, or jaw deformity are examples. The doctor may also examine your teeth to see if there are signs of wear from bruxism.
Examination of the throat is done to find out if you have enlarged tonsils or extra or swollen tissue in the back of your mouth. The piece of tissue that dangles down from the top of the back of the mouth is called the uvula. Uvula means grape cluster, and is shaped similar to one. In some people, it can be enlarged and can get in the way of proper airflow.
If lung disease is possible, the specialist may want to assess your lung function. Some of the risk factors for lung disease include smoking, heart failure, or asthma. You may be asked to blow into a device that measures the force, and how much air you can blow. There are more complex machines that may also be used to monitor airflow in and out of your lungs. The specialist may also have you do hand-held reflex testing in the office. This also monitors your ability to stay alert.
Your doctor may want to monitor the oxygen or carbon dioxide levels in your blood. This is done with a machine called an oximeter. The part that measures the oxygen or carbon dioxide levels in your blood is similar to a clothes pin. It is worn over your finger or ear lobe. It is connected by a wire to the oximeter. It then measures and records your oxygen level when sleeping. Normal oxygenation is 95 to 100 percent. In sleep apnea, levels may drop to 80 percent or lower. Levels below 70 percent are considered dangerously low.
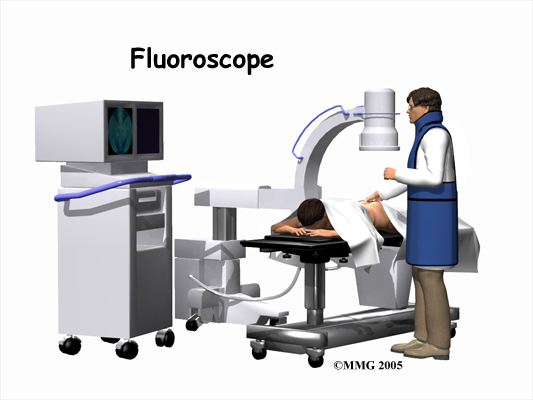
A polysomnogram is a procedure that is used to diagnose sleep disorders. It is done at a sleep laboratory or center. It is a way to record and measure what is going on during sleep. It can measure biological functions as well as body movement. Information is gathered from a set of electrodes taped to your skin. Wires from the electrodes carry signals to a monitoring device where they are recorded. The doctor then interprets the information. There are no needles. The electrodes measure electrical activity and do not cause an electrical shock.
The sleep laboratory consists of private rooms with beds. The sleep room is well insulated and temperature is kept comfortable. You may be allowed to wear your usual sleep clothes. You will be given a buzzer to alert the sleep study technician if you need to get up or get uncomfortable for any reason. Testing in the sleep study center may also involve seeing how long it takes to fall asleep while reading or resting.
Brain wave monitoring is done with several electrodes placed on the surface of the skull. These electrodes monitor and record brain wave activity. It can tell the different stages of sleep and when you are awake.
Other electrodes are placed near the outside corner of each eye in order to monitor eye movements. Electrodes on the chin or throat monitor jaw muscle tightening. Electrodes on the stomach monitor abdominal movements. Electrodes on the legs sense leg movements.
The heart rate and rhythm is monitored with an electrocardiogram (ECG). Sticky patches with electrodes are placed on the chest. There is an increase in cardiovascular events such as heart attack and stroke in persons with chronic sleep problems.
Another measuring device is called a strain gauge. It is a stretchy belt that is worn around the chest to measure chest movement.
Treatment
What treatment options are available?
Non-Surgical Treatment
Treatment of insomnia can include medication and behavioral therapy. Behavioral therapies are usually done with a psychologist or person with similar training. Talk therapy may be helpful in decreasing stress and anxiety.
Quite often, changes in habits are all that is needed to improve sleep. Poor sleep habits include spending too much time in bed or having an irregular sleep schedule. Not getting sufficient bright-light exposure during the day and poor physical functioning are known to interfere with proper sleep. Sleeping in an environment that is too bright, too noisy, or too hot or cold can cause sleep problems. Drinking alcohol or caffeinated beverages too close to bedtime can also interfere with sleep. Treatment of depression is also important to consider.
Some recommended sleep medications include some of the antidepressants. Drugs that stimulate the breathing reflex may be used for central sleep apnea. Specific medications are also used for narcolepsy. Medications that treat Parkinson’s disease can be beneficial for RLS and PLMD. Our bodies make melatonin that helps regulate the sleep cycle. It is also available as an over-the-counter medication. It is most helpful for shift work and jet lag. When soft tissue in the nose or throat is enlarged, it may be recommended that you use decongestants or other medications that help shrink soft tissue in your nose and throat.
Behavioral treatments often mean changing the way you act or think. You may need to learn how to decrease stimulation of the body’s system of alertness. This system is called fight or flight and can interfere with proper sleep. When your nervous system is on high alert, it is especially difficult to fall asleep. Reducing stress, doing relaxation exercises or other soothing activities can calm the nervous system. Changing negative attitudes about yourself and sleep can also be helpful. There are many simple ways that sleep can be improved.
he following tips may be helpful for anyone with sleep problems.
Exercise can increase the core body temperature, which promotes sleep. When vigorous enough, exercise can help the body release endorphins, which are chemicals that act like morphine, a pain medication.
Increase your body temperature. A hot bath, shower, or use of a hot tub can affect body temperature. A hot drink will also warm you. It is recommended that you try to increase your body temperature within two hours before bedtime.
Bedroom environment should be a comfortable temperature, quiet, and dark. If there are factors out of your control such as a noisy neighbor or animal, earplugs may be useful. Eyeshades may help with unwanted light.
Bedtime rituals such as a bath, reading for pleasure, or listening to soothing music may help decrease your body’s alertness.
Stress reduction and relaxation improve sleep. Relaxation can include deep breathing exercises. Progressive muscle relaxation involves slowly tensing and releasing muscles. You usually start with muscles of the face, then neck. You gradually work your way down until your toes feel fully relaxed. Meditation, prayer, imagery, and listening to soothing music are other methods to help reduce stress.
Regular sleep schedule is important. Wake and get up at the same time each morning, including weekends, even after a poor night’s sleep. This will help with the circadian rhythm.
Daytime naps should generally be avoided.
Get out of bed. If you are awake in bed for more than 20 minutes, get up and go to another room. Do not watch TV in bed. The bed should be used only for sleep and sex. Too much time in bed causes interrupted and shallow sleep.
Heavy meals late in the evening should be avoided. A warm drink or small snack may be beneficial before bedtime.
Exposure to sunlight is important for the circadian rhythm. Spend some time outdoors especially after awakening. Talk to your doctor about the use of bright light therapy to help regulate the circadian rhythm. There are also lighting devices available that imitate dawn. Light boxes and dawn stimulators may be available at medical supply stores or on the Internet. It is important to buy the appropriate light box and use only as directed.
Quit smoking. Withdrawal from nicotine begins two or three hours after smoking. This can interrupt sleep.
Avoid alcohol before bed. Although it may help you fall asleep, sleep is otherwise interrupted.
Avoid caffeine particularly after the middle of the afternoon. If at all possible, decrease or don’t drink caffeinated drinks altogether. You may have to taper off of caffeine. Most people will have symptoms of withdrawal. These could include headache and fatigue.
Avoid medications that may interfere with either falling asleep or staying asleep. Narcotics for pain may cause a decrease in the brain’s ability to keep breathing during sleep. This can cause a decrease in oxygen level in the blood.
Aromatherapy is the use of scents such as lavender, chamomile, or vanilla that help to quiet the nervous system. These may be sprayed on bedding. Oils may be placed under your nose, or on your chest, or used in the bath.
Allergies can cause swelling and narrowing of the airway. This can cause partial blockage of your airway and contribute to obstructive sleep apnea. Ask your doctor about treatment of allergies. A mixture of water with a little bit of salt can be used to rinse the lining of your nose and sinus tissue. This helps to shrink swollen tissue. It also helps to flush pollen and other allergens. Humidifiers in dry climates may also help sooth the lining of your nose and sinuses.
Lose weight particularly if you have sleep apnea. You may be asked to see a nutritionist to help with weight loss.
Change in sleep position can also make a difference. You may have more trouble breathing properly while lying on your back. Sleeping on your sides can relieve this. There are monitors and alarms available. Some people have sewn a small ball into the back of their pajamas.
Dental appliances or retainers may be useful in bringing the jaw and tongue forward during sleep. This helps to keep the airway open. Dental appliances are also used to treat bruxism (grinding the teeth at night).
Continuous positive airway pressure (CPAP) is the most common treatment for sleep apnea. It is a breathing device. A CPAP machine is a small machine that can sit on your nightstand. It has a hose that attaches to a mask that usually covers the nose. The mask is worn during sleep. Room air is blown through the nostrils, allowing the airway to remain open during sleep. Some people may also require oxygen at night. Your insurance will pay for most if not all of the cost. Typically they are obtained from oxygen or medical equipment companies.
Getting used to the CPAP machine is not always easy. Some people may experience anxiety from having the mask placed over the face. Others may not like the way it looks. It may take encouragement to help you continue with the changes necessary to improve sleep. If you still have sleepiness or insomnia after using CPAP or after making several lifestyle changes, your doctor may need to consider more aggressive treatment.
Surgery
Other treatments for sleep apnea include surgery. There are several surgeries that may be recommended. If you have trouble breathing through your nose, the surgeon may decide to cut away some of the soft tissue in the nose. Sometimes straightening the septum (cartilage) that divides the nose into two parts is also necessary.
If your airway is small, especially when the soft palate (top of the mouth) and the tongue relax during sleep, it may be recommended that you have reconstructive surgery. The most common type of reconstructive surgery is called uvulopalatopharyngoplasty or UPPP. Excess tissue such as the tonsils, adenoids, and uvula are removed. These surgeries are usually performed by an otolaryngologist, or ear, nose, and throat (ENT) surgeon.
Sometimes surgery to change the structure of the jaw or face is considered.
Ventilators or mechanical breathing machines are needed for some extreme cases of central sleep apnea. Air is blown from the ventilator through a hole in the neck called a tracheostomy. A tracheostomy is the operation used to make a small opening in the trachea or windpipe. A small cut is made by a surgeon in the front of the neck. This bypasses the causes for decreased airflow in the nose, mouth, and throat. During waking hours the tube is plugged to allow normal breathing. At night, a tube is inserted that is then connected to a ventilator or breathing machine.
Stomach banding or bypass is recommended if being overweight contributes to a sleep disorder.
Summary
Regular follow up with your doctor or therapist is recommended to help make transition into lifestyle changes easier. Trying different methods for relaxation and other changes in behavior may take some coaching.
The staff at the sleep center or the staff at the medical supply store is helpful in answering questions about equipment. They may also be able to help with making adjustments in equipment that make sleep better. It may take several weeks or months to adjust to using machines when sleeping. You may need a repeat polysomnography or a shortened version of one after you have used your equipment for a while. Adjustments may need to be made if you continue to experience fatigue or other symptoms.
Hopefully, treatment of your underlying sleep disorder will improve some of your other medical problems such as blood pressure, weight, fatigue, and lowered mood. Your doctor will want to monitor these.
A physical therapist or personal trainer may be able to help you start an exercise program. Pain and fatigue often lead to inactivity, which leads to de-conditioning. Starting an exercise program can cause increased pain at first. The support of a professional may help you continue with an exercise program.
A registered dietitian may be recommended by your doctor for weight loss.
Some cities have support groups for people with sleep disorders. Check with your physician or through your local hospital to see what support groups are available.