Artificial Knee Replacement (Knee Arthroplasty) Animated Tutorial
Knee
Knee Anatomy Animated Tutorial
Knee Anatomy
A Patient’s Guide to Knee Anatomy
Introduction
To better understand how knee problems occur, it is important to understand some of the anatomy of the knee joint and how the parts of the knee work together to maintain normal function.
First, we will define some common anatomic terms as they relate to the knee. This will make it clearer as we talk about the structures later.
Many parts of the body have duplicates. So it is common to describe parts of the body using terms that define where the part is in relation to an imaginary line drawn through the middle of the body. For example, medial means closer to the midline. So the medial side of the knee is the side that is closest to the other knee. The lateral side of the knee is the side that is away from the other knee. Structures on the medial side usually have medial as part of their name, such as the medial meniscus. The term anterior refers to the front of the knee, while the term posterior refers to the back of the knee. So the anterior cruciate ligament is in front of the posterior cruciate ligament.
In addition to reading this article, be sure to watch our Knee Anatomy Animated Tutorial Video.
This guide will help you understand
- what parts make up the knee
- how the parts of the knee work
Important Structures
The important parts of the knee include
- bones and joints
- ligaments and tendons
- muscles
- nerves
- blood vessels
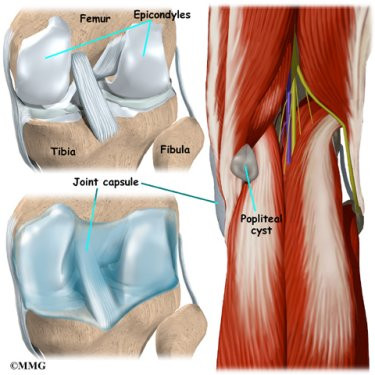
Bones and Joints
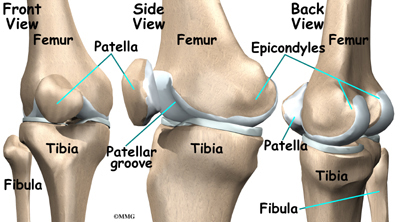
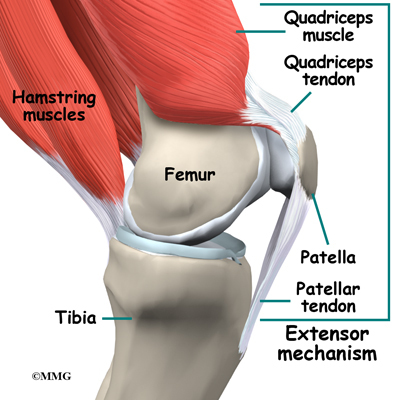
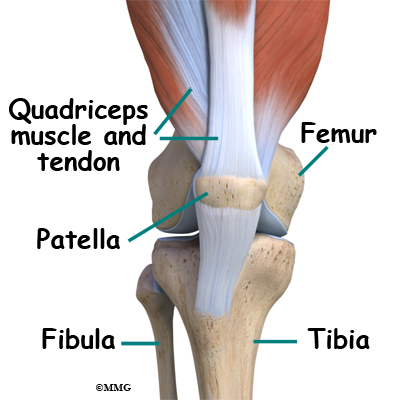
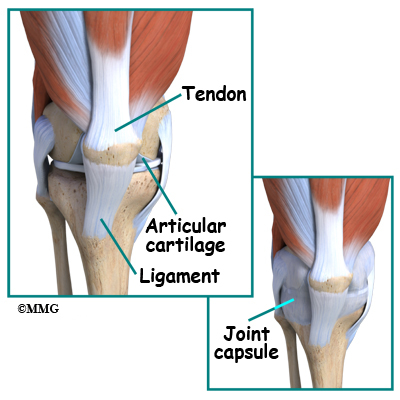
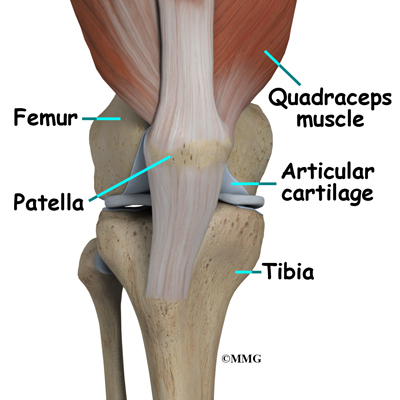
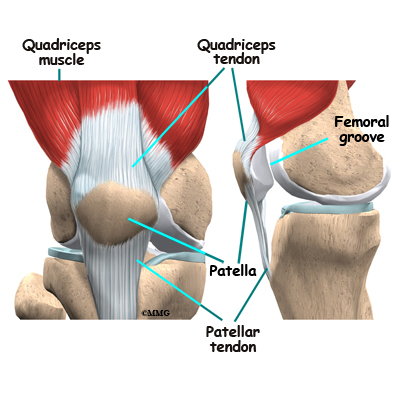
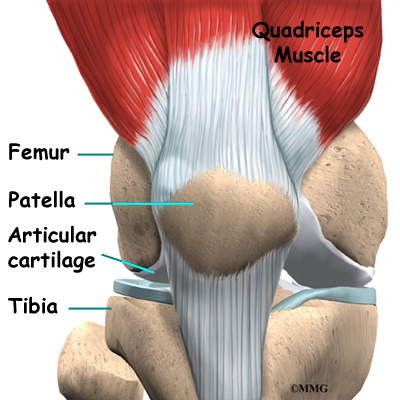
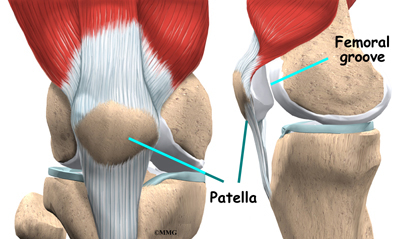
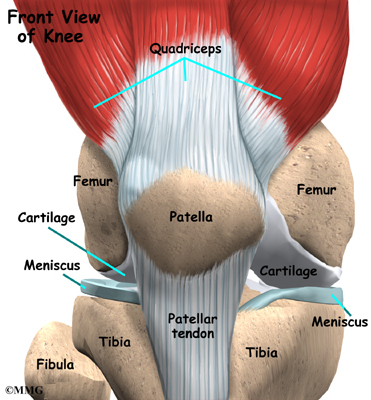
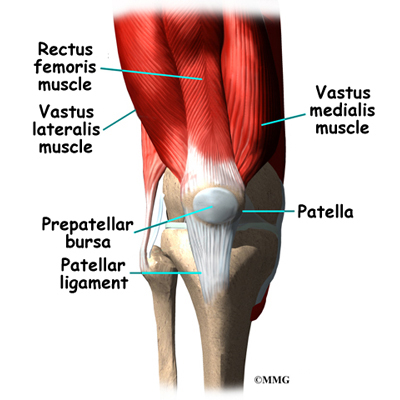
The knee is the meeting place of two important bones in the leg, the femur (the thighbone) and the tibia (the shinbone). The patella (or kneecap, as it is commonly called) is made of bone and sits in front of the knee.
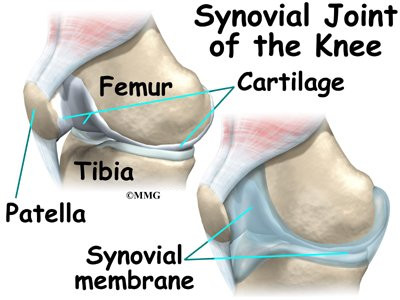
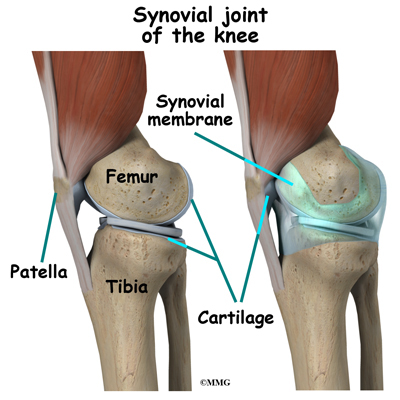
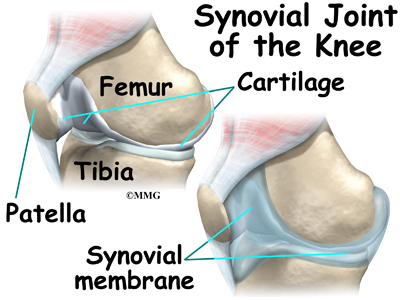
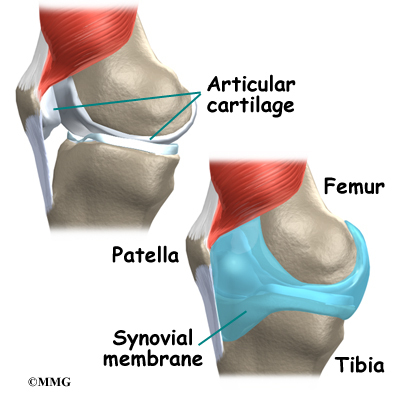
The knee joint is a synovial joint. Synovial joints are enclosed by a ligament capsule and contain a fluid, called synovial fluid, that lubricates the joint.
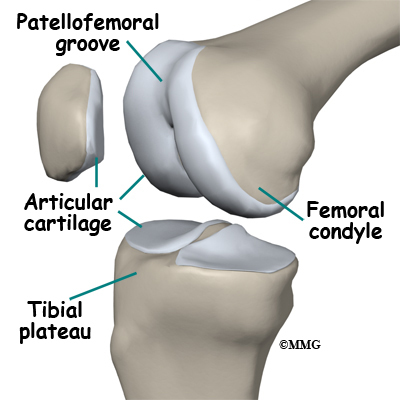
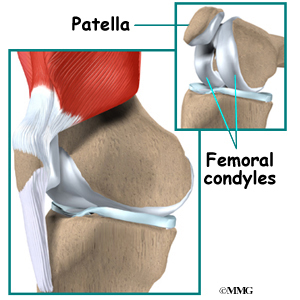
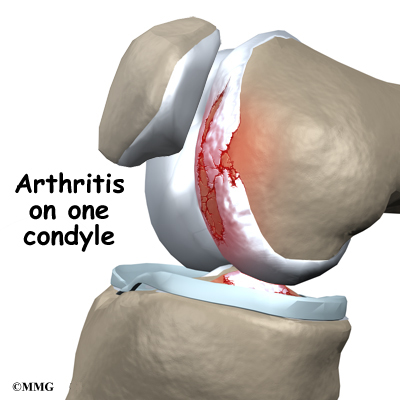
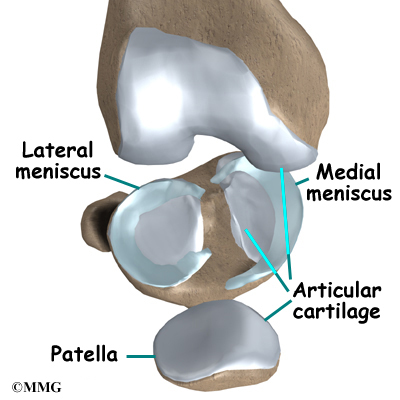
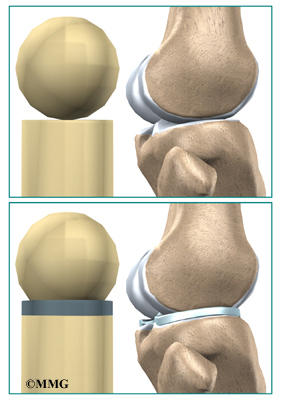
The end of the femur joins the top of the tibia to create the knee joint. Two round knobs called femoral condyles are found on the end of the femur. These condyles rest on the top surface of the tibia. This surface is called the tibial plateau. The outside half (farthest away from the other knee) is called the lateral tibial plateau, and the inside half (closest to the other knee) is called the medial tibial plateau.
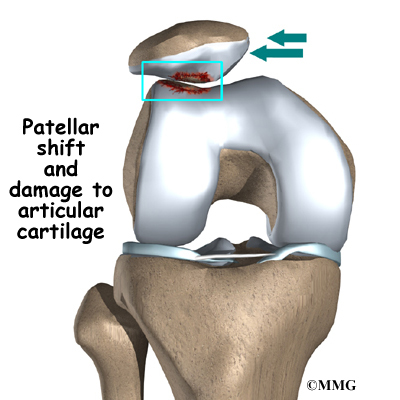
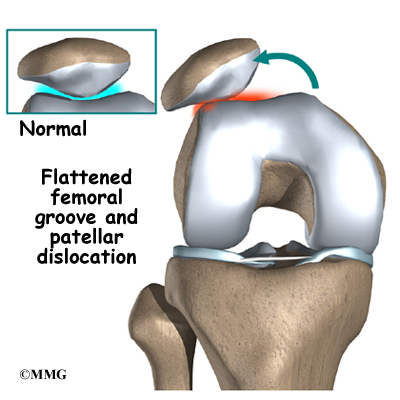
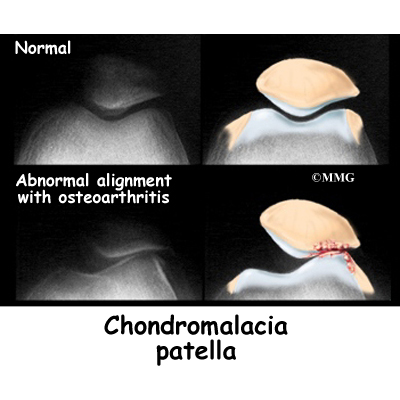
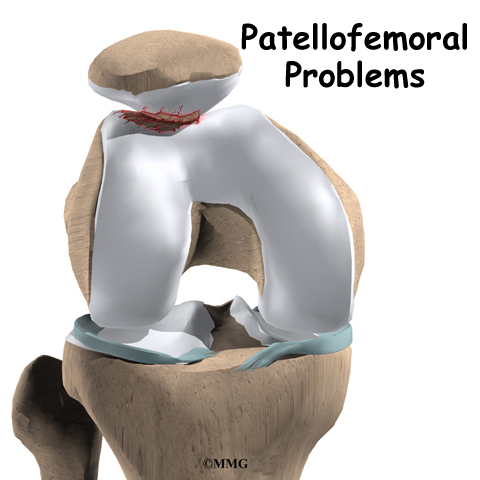
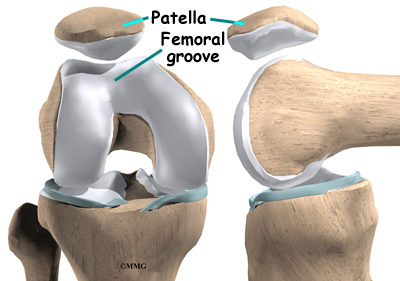
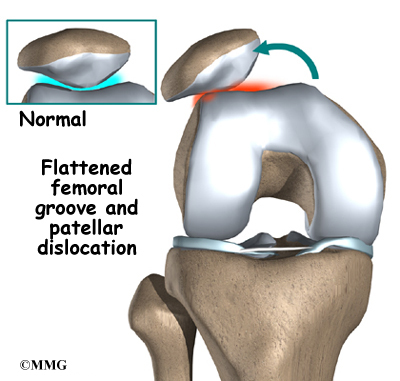
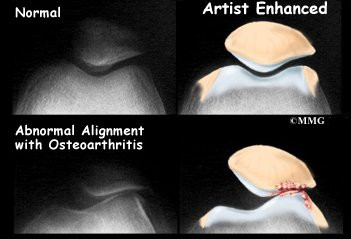
The patella glides through a special groove formed by the two femoral condyles called the patellofemoral groove.
The smaller bone of the lower leg, the fibula, never really enters the knee joint. It does have a small joint that connects it to the side of the tibia. This joint normally moves very little.
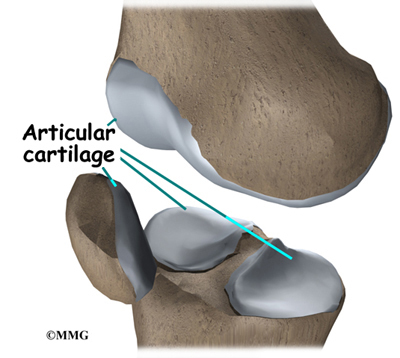
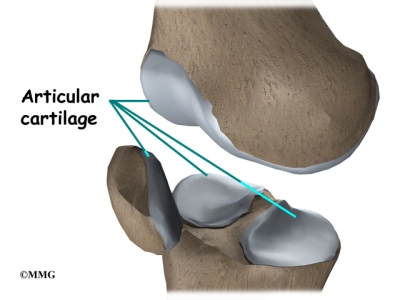
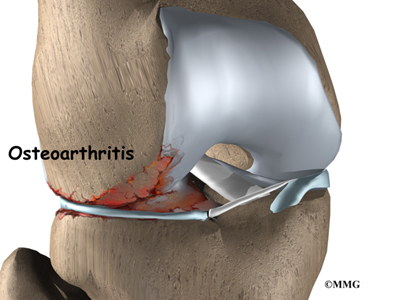
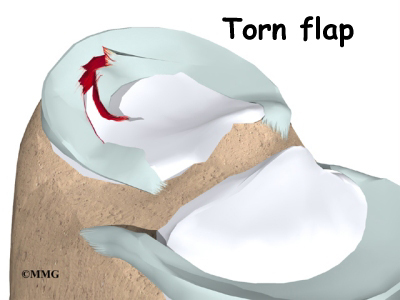
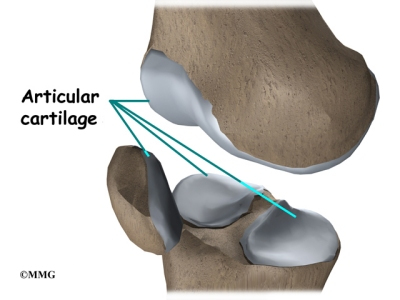
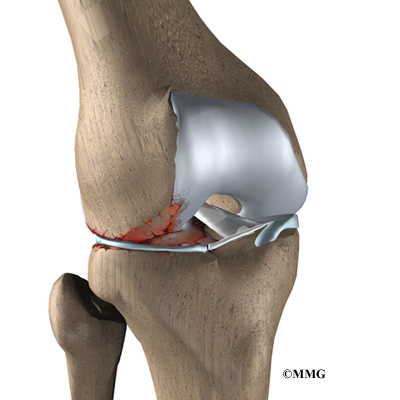
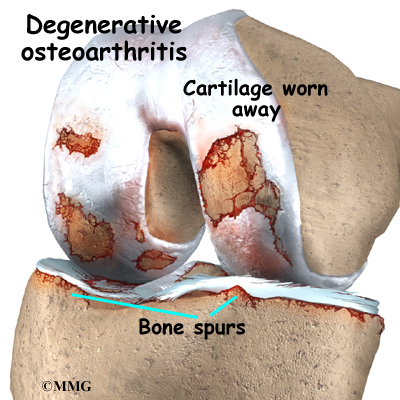
Articular cartilage is the material that covers the ends of the bones of any joint. This material is about one-quarter of an inch thick in most large joints. It is white and shiny with a rubbery consistency. Articular cartilage is a slippery substance that allows the surfaces to slide against one another without damage to either surface. The function of articular cartilage is to absorb shock and provide an extremely smooth surface to facilitate motion. We have articular cartilage essentially everywhere that two bony surfaces move against one another, or articulate. In the knee, articular cartilage covers the ends of the femur, the top of the tibia, and the back of the patella.
Ligaments and Tendons
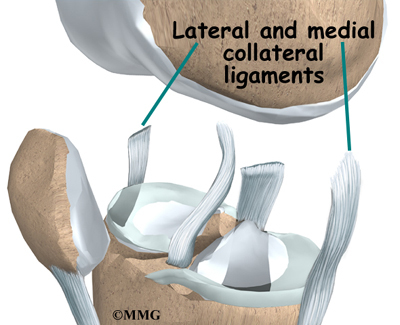
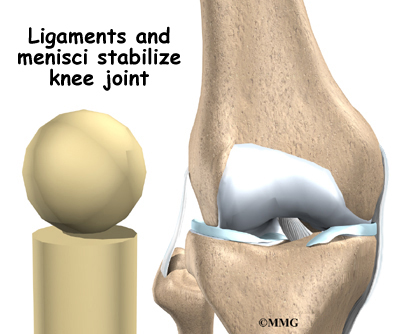
Ligaments are tough bands of tissue that connect the ends of bones together. Two important ligaments are found on either side of the knee joint. They are the medial collateral ligament (MCL) and the lateral collateral ligament (LCL).
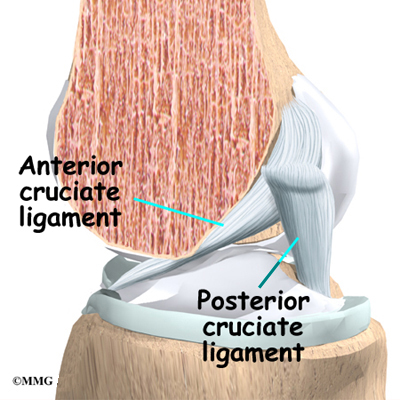
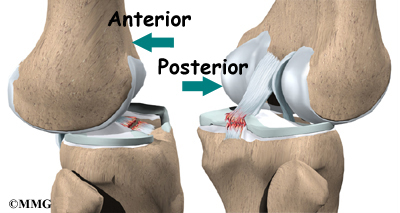
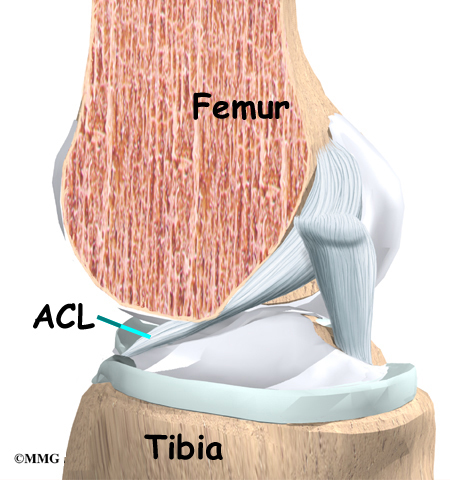
Inside the knee joint, two other important ligaments stretch between the femur and the tibia: the anterior cruciate ligament (ACL) in front, and the posterior cruciate ligament (PCL) in back. The MCL and LCL prevent the knee from moving too far in the side-to-side direction. The ACL and PCL control the front-to-back motion of the knee joint.
The ACL keeps the tibia from sliding too far forward in relation to the femur. The PCL keeps the tibia from sliding too far backward in relation to the femur. Working together, the two cruciate ligaments control the back-and-forth motion of the knee. The ligaments, all taken together, are the most important structures controlling stability of the knee.
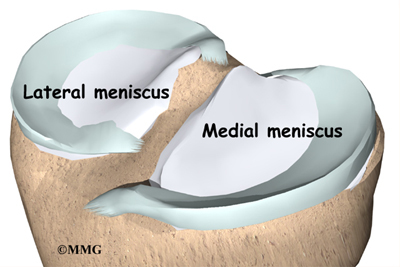
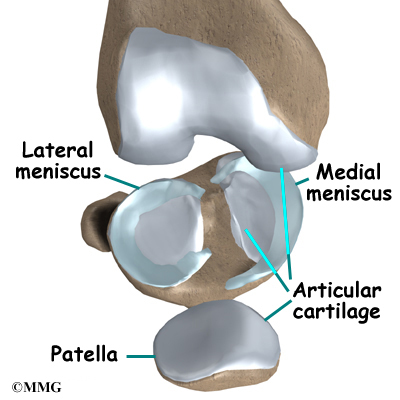
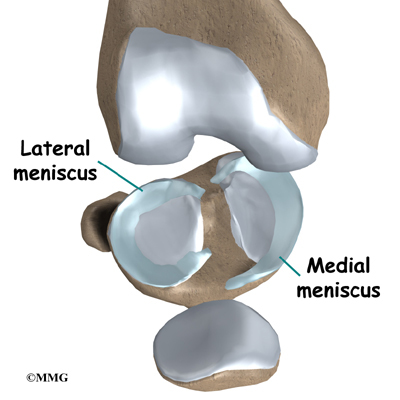
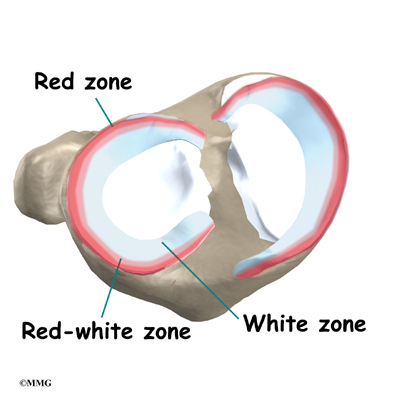
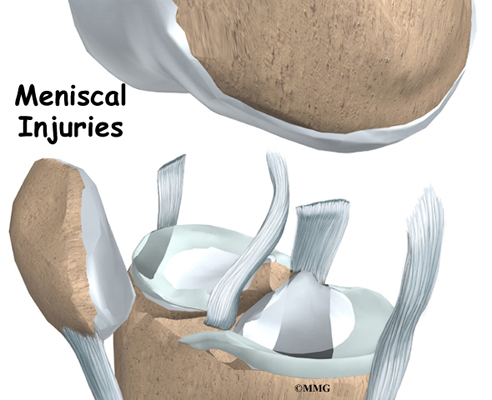
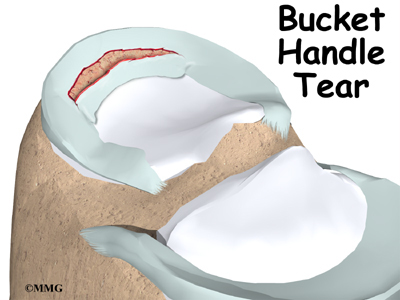
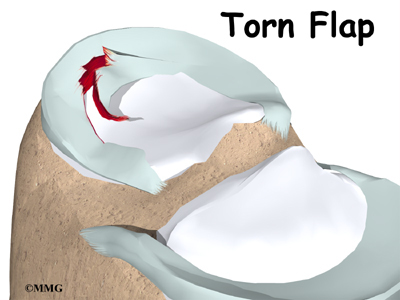
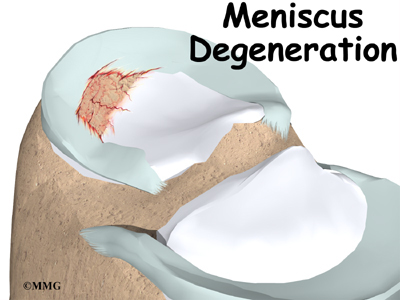
Two special types of ligaments called menisci sit between the femur and the tibia. These structures are sometimes referred to as the cartilage of the knee, but the menisci differ from the articular cartilage that covers the surface of the joint.
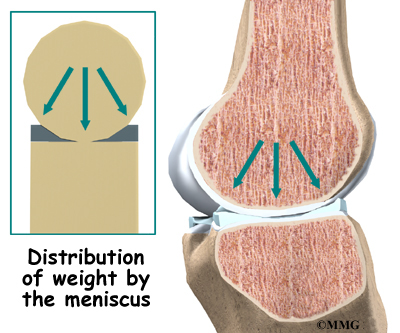
The two menisci of the knee are important for two reasons: (1) they work like a gasket to spread the force from the weight of the body over a larger area, and (2) they help the ligaments with stability of the knee.
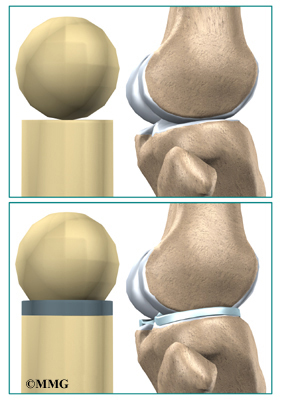
Imagine the knee as a ball resting on a flat plate. The ball is the end of the thighbone as it enters the joint, and the plate is the top of the shinbone. The menisci actually wrap around the round end of the upper bone to fill the space between it and the flat shinbone. The menisci act like a gasket, helping to distribute the weight from the femur to the tibia.
Without the menisci, any weight on the femur will be concentrated to one point on the tibia. But with the menisci, weight is spread out across the tibial surface. Weight distribution by the menisci is important because it protects the articular cartilage on the ends of the bones from excessive forces. Without the menisci, the concentration of force into a small area on the articular cartilage can damage the surface, leading to degeneration over time.
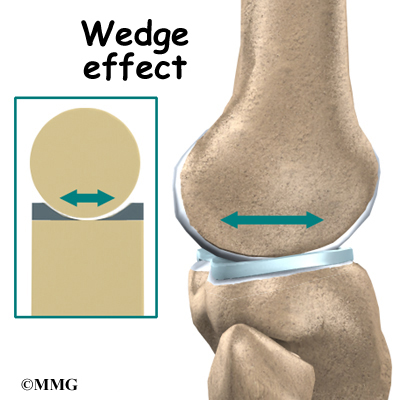
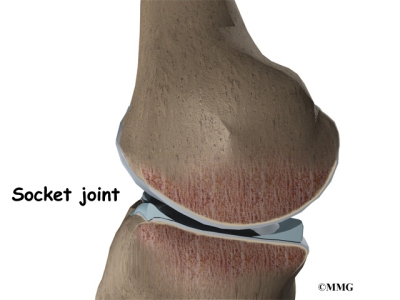
In addition to protecting the articular cartilage, the menisci help the ligaments with stability of the knee. The menisci make the knee joint more stable by acting like a wedge set against the bottom of a car tire. The menisci are thicker around the outside, and this thickness helps keep the round femur from rolling on the flat tibia. The menisci convert the tibial surface into a shallow socket. A socket is more stable and more efficient at transmitting the weight from the upper body than a round ball on a flat plate. The menisci enhance the stability of the knee and protect the articular cartilage from excessive concentration of force.
Taken all together, the ligaments of the knee are the most important structures that stabilize the joint. Remember, ligaments connect bones to bones. Without strong, tight ligaments to connect the femur to the tibia, the knee joint would be too loose. Unlike other joints in the body, the knee joint lacks a stable bony configuration. The hip joint, for example, is a ball that sits inside a deep socket. The ankle joint has a shape similar to a mortise and tenon, a way of joining wood used by craftsmen for centuries.
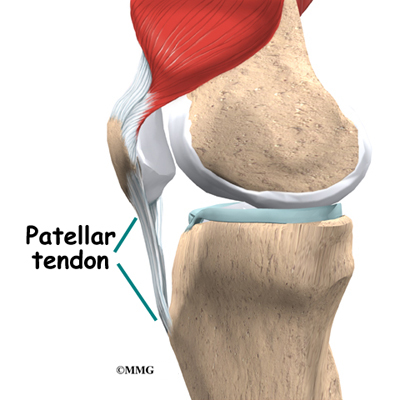
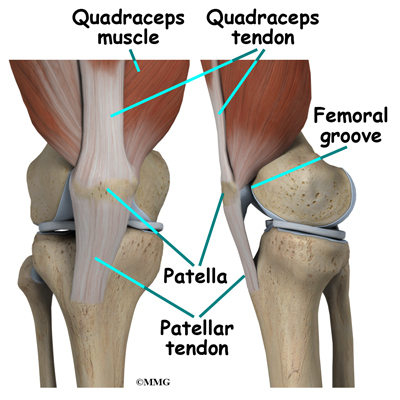
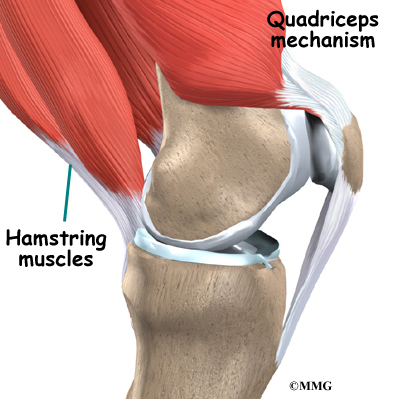
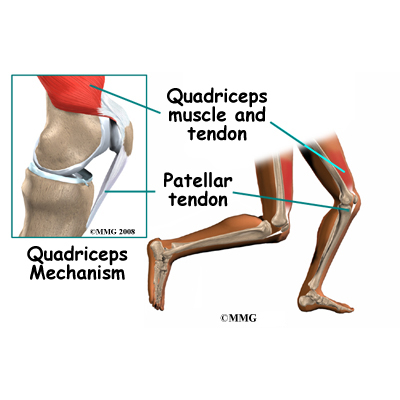
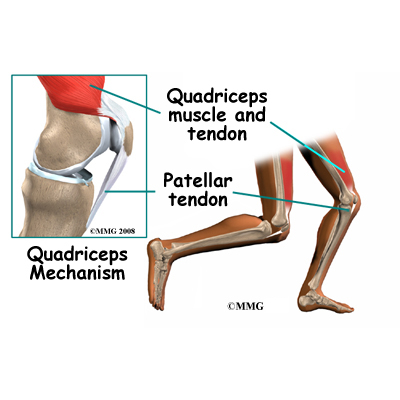
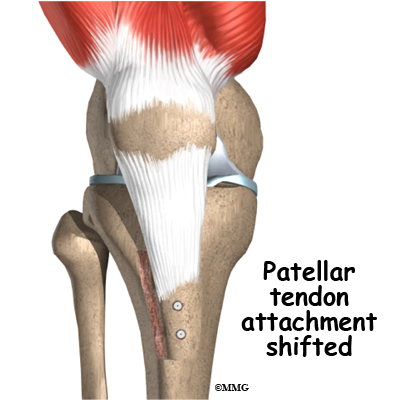
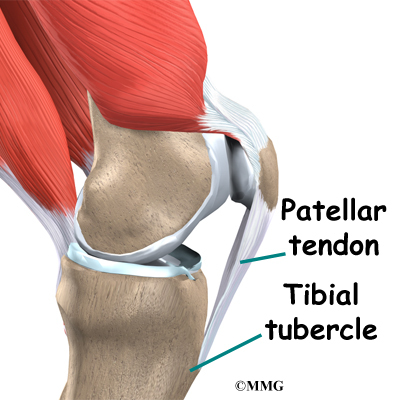
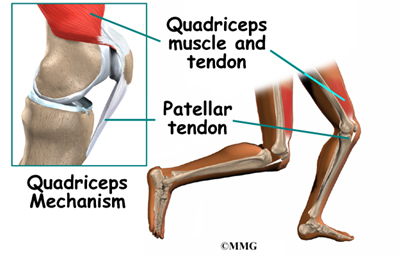
Tendons are similar to ligaments, except that tendons attach muscles to bones. The largest tendon around the knee is the patellar tendon. This tendon connects the patella (kneecap) to the tibia. This tendon covers the patella and continues up the thigh.
There it is called the quadriceps tendon since it attaches to the quadriceps muscles in the front of the thigh. The hamstring muscles on the back of the leg also have tendons that attach in different places around the knee joint. These tendons are sometimes used as tendon grafts to replace torn ligaments in the knee.
Muscles
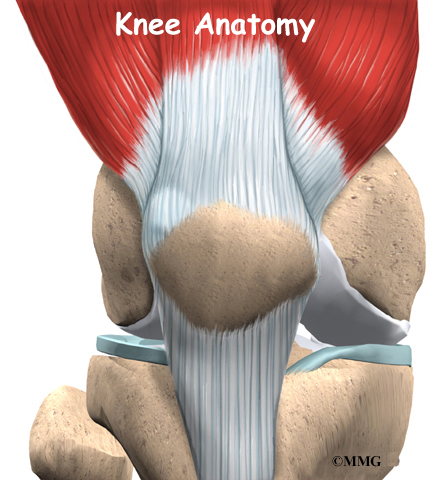
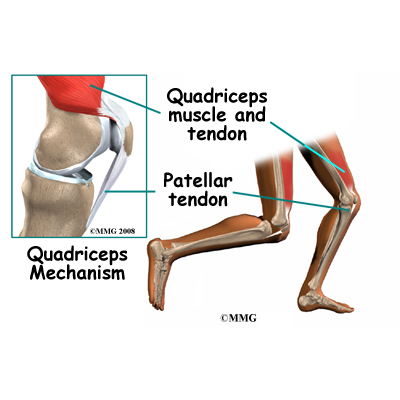
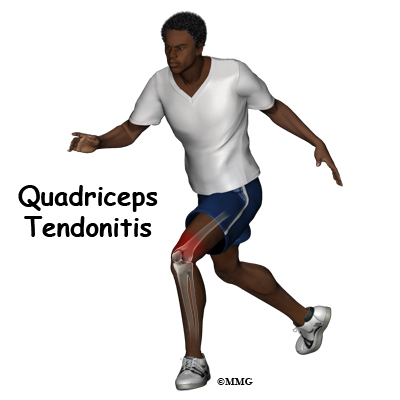
The extensor mechanism is the motor that drives the knee joint and allows us to walk. It sits in front of the knee joint and is made up of the patella, the patellar tendon, the quadriceps tendon, and the quadriceps muscles. The four quadriceps muscles in front of the thigh are the muscles that attach to the quadriceps tendon. When these muscles contract, they straighten the knee joint, such as when you get up from a squatting position.
The way in which the kneecap fits into the patellofemoral groove on the front of the femur and slides as the knee bends can affect the overall function of the knee. The patella works like a fulcrum, increasing the force exerted by the quadriceps muscles as the knee straightens. When the quadriceps muscles contract, the knee straightens.
The hamstring muscles are the muscles in the back of the knee and thigh. When these muscles contract, the knee bends.
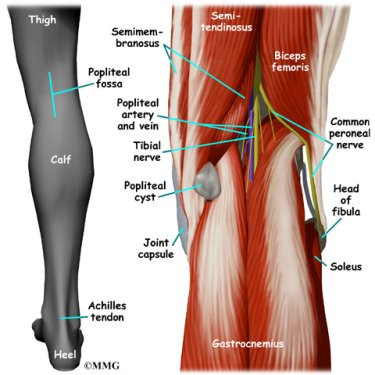
Nerves
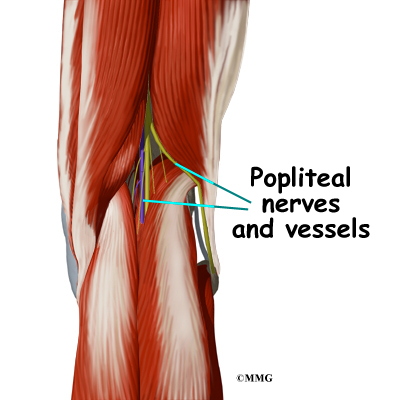
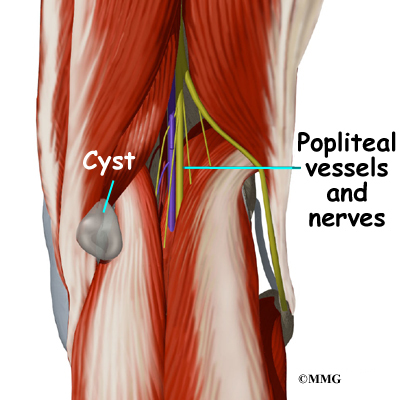
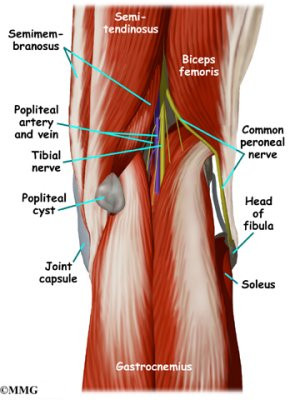
The most important nerves around the knee are the tibial nerve and the common peroneal nerve in the back of the knee. These two nerves travel to the lower leg and foot, supplying sensation and muscle control. The
large sciatic nerve splits just above the knee to form the tibial
nerve and the common peroneal nerve. The tibial nerve continues down
the back of the leg while the common peroneal nerve travels around the
outside of the knee and down the front of the leg to the foot. Both of
these nerves can be damaged by injuries around the knee.
Blood Vessels
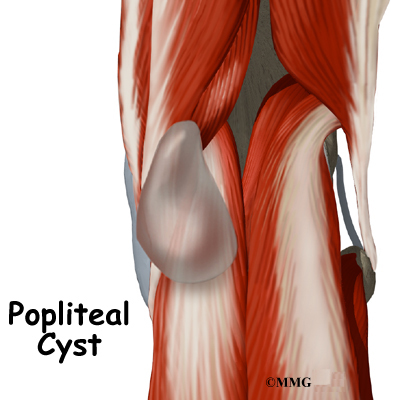
The major blood vessels around the knee travel with the tibial nerve
down the back of the leg. The popliteal artery and popliteal vein are the largest blood supply to the leg and foot. If the popliteal artery is damaged beyond repair, it is very likely the leg will not be able
to survive. The popliteal artery carries blood to the leg and foot.
The popliteal vein carries blood back to the heart.
Summary
The knee has a somewhat unstable design. Yet it must support the body’s full weight when standing, and much more than that during walking or running. So it’s not surprising that knee problems are a fairly common complaint among people of all ages. Understanding the basic parts of the knee can help you better understand what happens when knee problems occur.
ACL Hamstring Tendon Graft Reconstruction
A Patient’s Guide to Hamstring Tendon Graft Reconstruction of the ACL
Introduction
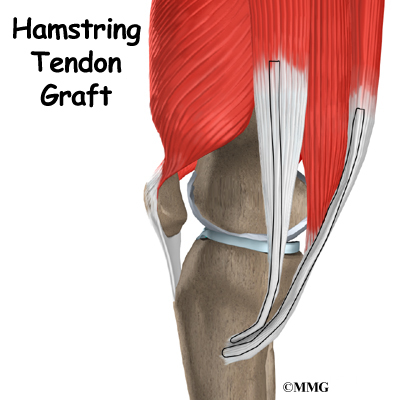
When the anterior cruciate ligament (ACL) in the knee is torn or injured, surgery may be needed to replace it. There are many different ways to do this operation. One is to take a piece of the hamstring tendon from behind the knee and use it in place of the torn ligament. When arranged into three or four strips, the hamstring graft has nearly the same strength as other available grafts used to reconstruct the ACL.
This guide will help you understand
- what parts of the knee are treated during surgery
- how surgeons perform the operation
- what to expect before and after the procedure
Anatomy
What parts of the knee are involved?
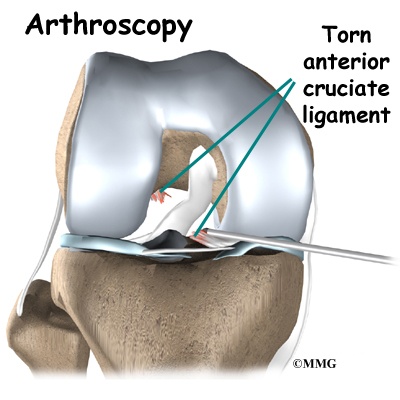
Ligaments are tough bands of tissue that connect the ends of bones together. The ACL is located in the center of the knee joint where it runs from the backside of the femur (thighbone) to the front of the tibia (shinbone).
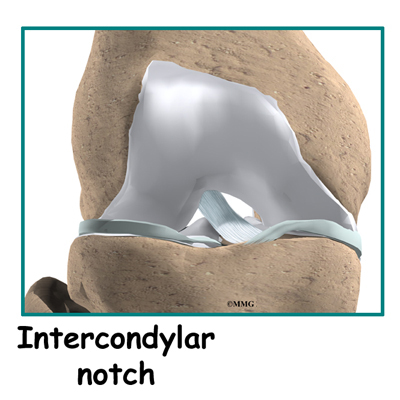
The ACL runs through a special notch in the femur called the intercondylar notch and attaches to a special area of the tibia called the tibial spine.
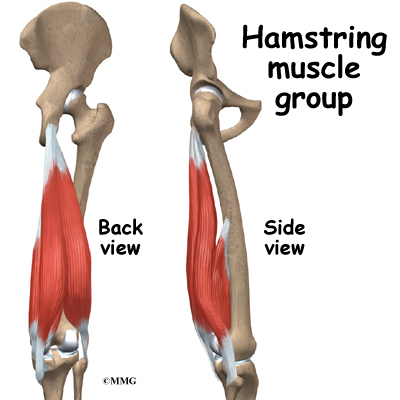
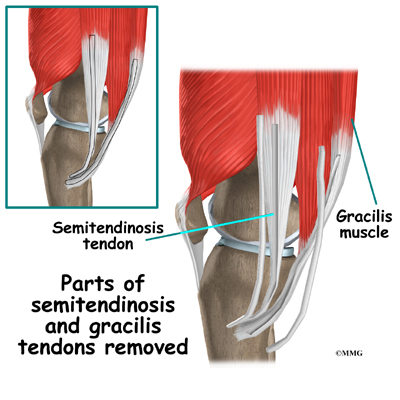
The hamstrings make up the bulk of the muscles in back of the thigh. The hamstrings are formed by three muscles and their tendons: the semitendinosus, semimembranosus, and biceps femoris. The top of the hamstrings connects to the ischial tuberosity, the small bony projection on the bottom of the pelvis, just below the buttocks. (There is one ischial tuberosity on the left and one on the right.)
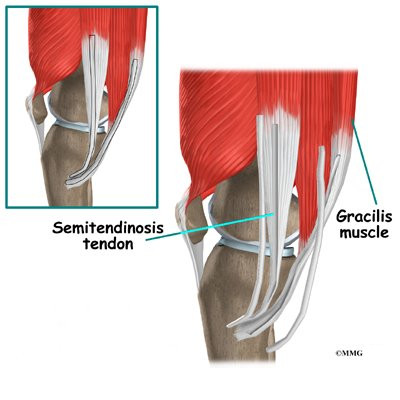
The hamstring muscles run down the back of the thigh. Their tendons cross the knee joint and connect on each side of the tibia. The graft used in ACL reconstruction is taken from the hamstring tendon (semitendinosus) along the inside part of the thigh and knee. Surgeons also commonly include a tendon just next to the semitendinousus, called the gracilis.
The hamstrings function by pulling the leg backward and by propelling the body forward while walking or running. This movement is called hip extension. The hamstrings also bend the knees, a motion called knee flexion.
Related Document: A Patient’s Guide to Knee Anatomy
Related Document: A Patient’s Guide to Anterior Cruciate Ligament Injuries
Rationale
What does the surgeon hope to accomplish?
The main goal of ACL surgery is to keep the tibia from moving too far forward under the femur bone and to get the knee functioning normally again.
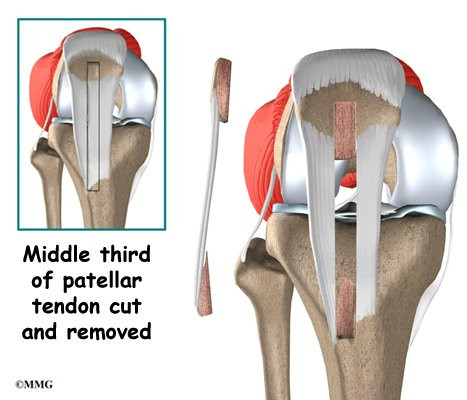
There are two grafts commonly used to repair a torn ACL. One is a strip of the patellar tendon below the kneecap. The other is the hamstring tendon graft. For a long time, the patellar tendon was the preferred choice because it is easy to get to, holds well in its new location, and heals fast. One big drawback to grafting the patellar tendon is pain at the front of the knee after surgery. This can be severe enough to prevent any pressure on the knee, such as kneeling.
For this reason, a growing number of surgeons are using grafted tissue from the hamstring tendon. There are no major differences in the final results of these two methods. When it comes to symptoms after surgery, joint strength and stability, and ability to use the knee, either method is good. However, with the hamstring tendon graft, there are generally no problems kneeling and no pain in the front of the knee.
Related Document: A Patient’s Guide to Patellar Tendon Graft Reconstruction of the ACL
Preparation
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. Your therapist will check your current pain levels, your ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. Your therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted to the surgery center early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
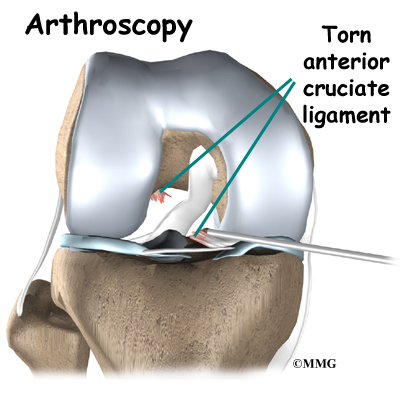
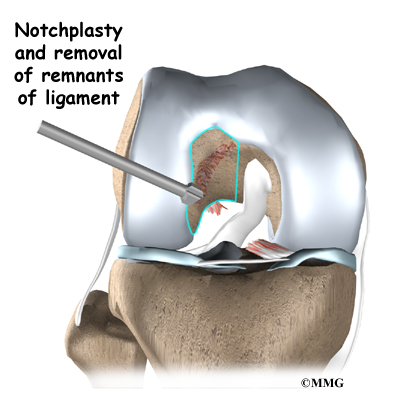
Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during arthroscopy for this procedure. The surgery doesn’t require the surgeon to open the knee joint.
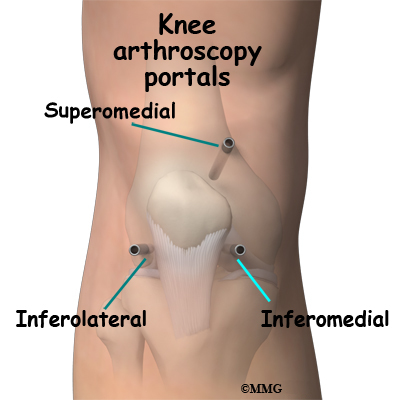
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia. The surgeon begins the operation by making two small openings into the knee, called portals. These portals are where the arthroscope and surgical tools are placed into the knee. Care is taken to protect the nearby nerves and blood vessels.
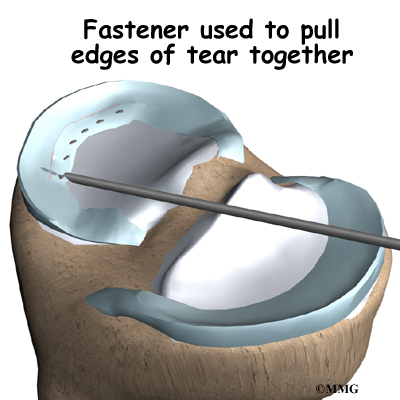
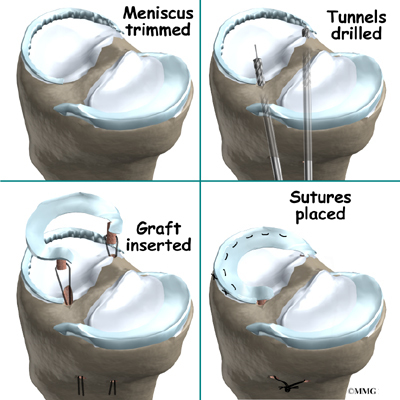
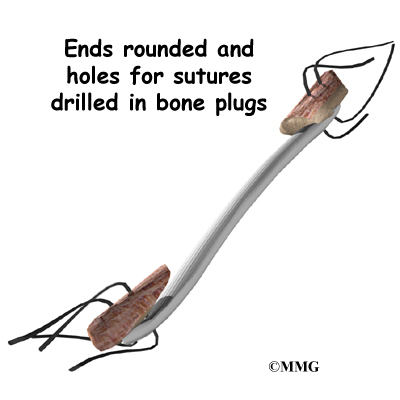
An incision is also made along the inside edge of the knee, just over where the hamstring tendons attach to the tibia. Working through this incision, the surgeon takes out the semitendinosus and gracilis tendons. Some surgeons prefer to use only the semitendinosus tendon and do not disrupt the gracilis tendon.
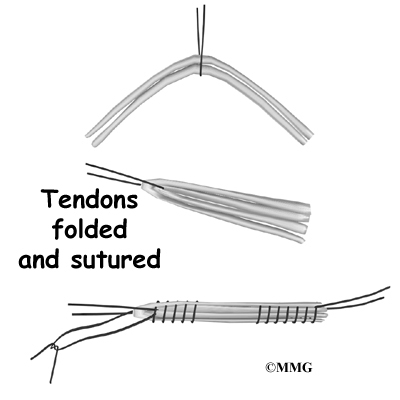
The tendons are arranged into three or four strips, which increases the strength of the graft. The surgeon stiches the strips together to hold them in place.
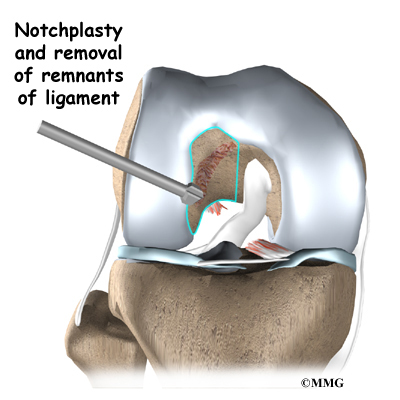
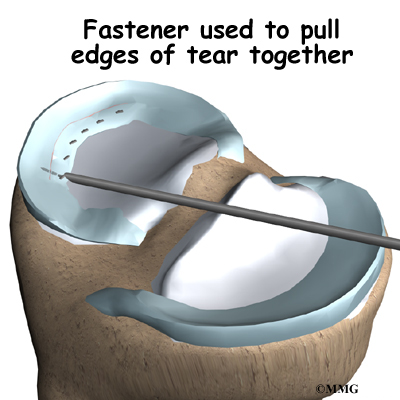
Next, the surgeon prepares the knee to place the graft. The remnants of the original ligament are removed. The intercondylar notch (mentioned earlier) is enlarged so that nothing will rub on the graft. This part of the surgery is referred to as a notchplasty.
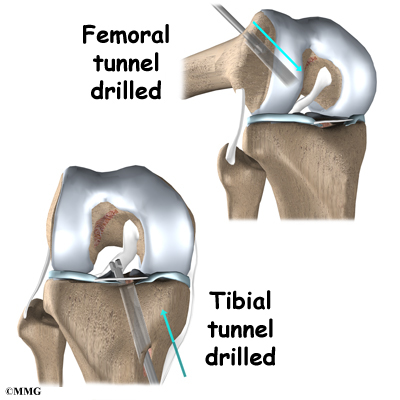
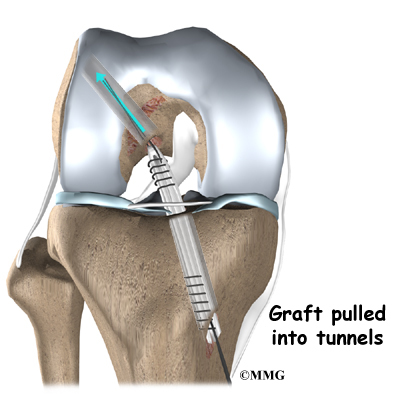
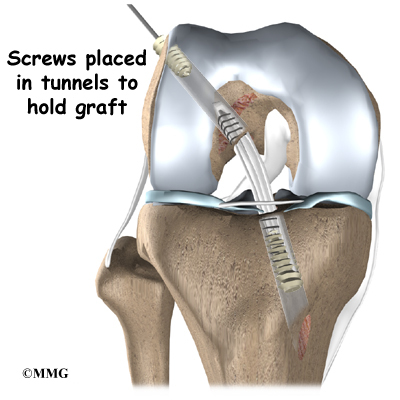
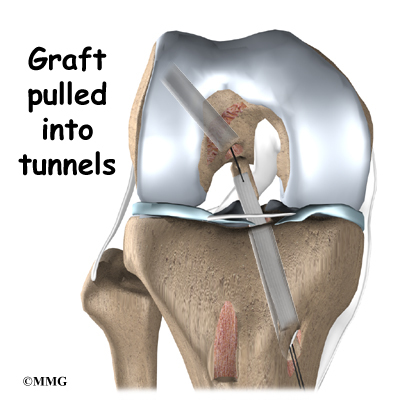
Once this is done, holes are drilled in the tibia and the femur to place the graft. These holes are placed so that the graft will run between the tibia and femur in the same direction as the original ACL. The graft is then pulled into position through the drill holes. Screws or staples are used to hold the graft inside the drill holes.
To keep fluid from building up in your knee, the surgeon may place a tube in your knee joint. The portals and skin incisions are then stitched together, completing the surgery.
Complications
What can go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hamstring tendon graft reconstruction of the ACL are
- anesthesia complications
- thrombophlebitis
- infection
- problems with the graft
- problems at the donor site
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the surgical incision can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
Problems with the Graft
After surgery, the body attempts to develop a network of blood vessels in the new graft. This process, called revascularization, takes about 12 weeks. The graft is weakest during this time, which means it has a greater chance of stretching or rupturing. A stretched or torn graft can occur if you push yourself too hard during this period of recovery. When revascularization is complete, strength in the graft gradually builds. A second surgery may be needed to replace the graft if it is stretched or torn.
Problems at the Donor Site
Problems can occur at the donor site (the area behind the leg where the hamstring graft was taken from the thigh). A potential drawback of taking out a piece of the hamstring tendon is a loss of hamstring muscle strength.
The main function of the hamstrings is to bend the knee (knee flexion). This motion may be slightly weaker in people who have had a hamstring tendon graft to reconstruct a torn ACL. Some studies, however, indicate that overall strength is not lost because the rest of the hamstring muscle takes over for the weakened area. Even the portion of muscle where the tendon was removed works harder to make up for the loss.
The hamstring muscles sometimes atrophy (shrink) near the spot where the tendon was removed. This may explain why some studies find weakness when the hamstring muscles are tested after this kind of ACL repair. However, the changes seem to mainly occur if both the semitendinosus and gracilis tendons were used. And the weakness is mostly noticed by athletes involved in sports that require deep knee bending. This may include participants in judo, wrestling, and gymnastics. These athletes may want to choose a different method of repair for ACL tears.
The body attempts to heal the donor site by forming scar tissue. This new tissue is not as strong as the original hamstring tendon. Because of this, there is a small chance of tearing the healing tendon, especially if the hamstrings are worked too hard in the early weeks of rehabilitation following surgery.
After Surgery
What should I expect after surgery?
You may use a continuous passive motion (CPM) machine immediately afterward to help the knee begin moving and to alleviate joint stiffness. The machine straps to the leg and continuously bends and straightens the joint. This continuous motion is thought to reduce stiffness, ease pain, and keep extra scar tissue from forming inside the joint. The CPM is often used with a form of cold treatment that circulates cold water through hoses and pads around your knee.
Most ACL surgeries are now done on an outpatient basis. Many patients go home the same day as the surgery. Some patients stay one to two nights in the hospital if necessary. The tube placed in your knee at the end of the surgery is usually removed after 24 hours.
Your surgeon may also have you wear a protective knee brace for a few weeks after surgery. You’ll use crutches for two to four weeks in order to keep your knee safe, but you’ll probably be allowed to put a comfortable amount of weight down while you’re up and walking.
Rehabilitation
What will my recovery be like?
Patients usually take part in formal physical therapy after ACL reconstruction. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The goal is to help you regain full knee extension as soon as possible.
The physical therapist will choose treatments to get the thigh muscles toned and active again. Patients are cautioned about overworking their hamstrings in the first six weeks after surgery. They are often shown how to do isometric exercises for the hamstrings. Isometrics work the muscles but keep the joint in one position.
As the rehabilitation program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. Specialized balance exercises are used to help the muscles respond quickly and without thinking. This part of treatment is called neuromuscular training. If you need to stop suddenly, your muscles must react with just the right amount of speed, control, and direction. After ACL surgery, this ability doesn’t come back completely without exercise.
Neuromuscular training includes exercises to improve balance, joint control, muscle strength and power, and agility. Agility makes it possible to change directions quickly, go faster or slower, and improve starting and stopping. These are important skills for walking, running, and jumping, and especially for sports performance.
When you get full knee movement, your knee isn’t swelling, and your strength and muscle control are improving, you’ll be able to gradually go back to your work and sport activities. Some surgeons prescribe a functional brace for athletes who intend to return quickly to their sports.
Ideally, you’ll be able to resume your previous lifestyle activities. However, athletes are usually advised to wait at least six months before returning to their sports. Most patients are encouraged to modify their activity choices.
You will probably be involved in a progressive rehabilitation program for four to six months after surgery to ensure the best result from your ACL reconstruction. In the first six weeks following surgery, expect to see the physical therapist two to three times a week. If your surgery and rehabilitation go as planned, you may only need to do a home program and see your therapist every few weeks over the four to six month period.
Bipartite Patella
A Patient’s Guide to Bipartite Patella
Introduction
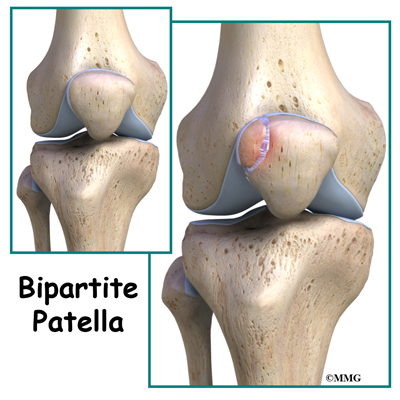
Bipartite patella is a congenital condition (present at birth) that occurs when the patella (kneecap) is made of two bones instead of a single bone. Normally, the two bones would fuse together as the you grow. But in bipartite patella, they remain as two separate bones. About one per cent of the population has this condition. Boys are affected much more often than girls. When this condition is discovered in adulthood it is oftentimes an “incidental finding”.
This guide will help you understand
- what parts of the knee are involved
- how this condition develops
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What is the patella and what does it do?
The knee is the meeting place of two important bones in the leg, the femur (the thighbone) and the tibia (the shinbone). The patella (kneecap) is the moveable bone that sits in front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this condition?
The patella starts out as a piece of fibrous cartilage. It turns into bone or ossifies as part of the growth process. Each bone has an ossification center. This is the first area of the structure to start changing into bone.
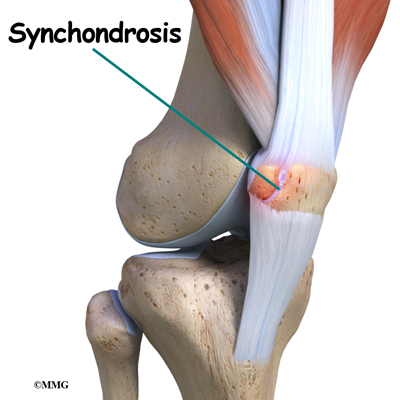
Most bones (including the patella) only have one primary ossification center. But in some cases, a second ossification center is present. Normally, these two centers of bone will fuse together during late childhood or early adolescence. If they don’t ossify together, then the two pieces of bone remain connected by fibrous or cartilage tissue. This connective tissue is called a synchondrosis.
The most common location of the second bone is the supero-lateral (upper outer) corner of the patella. But the problem can occur at the bottom of the patella or along the side of the kneecap.
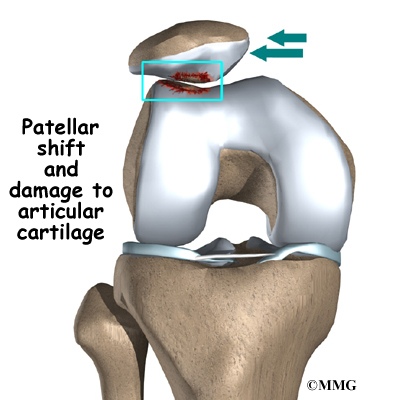
Injury or direct trauma to the synchondrosis can cause a separation of this weak union leading to inflammation. Repetitive microtrauma can have the same effect. The cartilage has a limited ability to repair itself. The increased mobility between the main bone and the second ossification center further weakens the synchondrosis resulting in painful symptoms.
Symptoms
What does bipartite patella feel like?
Most of the time, there are no symptoms. Sometimes there is a bony bump or place where the bone sticks out more on one side than the other. If inflammation of the fibrous tissue between the two bones occurs, then painful symptoms develop directly over the kneecap. The pain is usually described as dull aching. There may be some swelling.
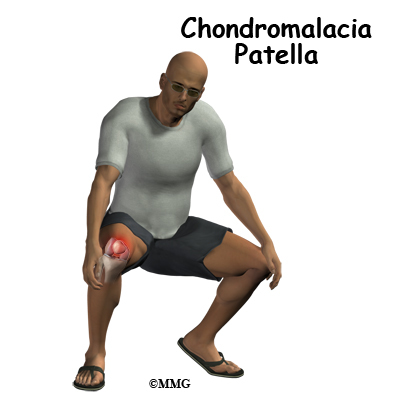
Movement of the knee can be painful, especially when bending the joint. Atrophy of the quadriceps and malalignment of the patella can lead to patellar tracking problems. Squatting, stair climbing, weight training, and strenuous activity aggravate the knee causing increased symptoms. For the runner, running down hill causes increased pain, tenderness, and swelling.
Diagnosis
How will my doctor diagnose this condition?
Most of the time, this condition is seen on X-rays of the knee that are taken for some other reason. This is referred to as an incidental finding. Sometimes, it is mistaken for a fracture of the patella. But since the problem usually affects both knees, an X-ray of the other knee showing the same condition can confirm the diagnosis.
MRIs or bone scans are useful when a fracture is suspected but doesn’t show up on the X-rays. The presence of fibrocartilaginous material between the two bones helps confirm a diagnosis of bipartite patella. An MRI can show the condition of articular cartilage at the patellar-fragment interface. The lack of bone marrow edema helps rule out a bone fracture. CT scans will show the bipartite fragment but are not as helpful as MRIs because bone marrow or soft tissue edema does not show up, so it’s still not clear from CT findings whether the symptoms are from the fragment or fracture.
Treatment
What treatment options are available?
Most of the time, no treatment is necessary. Most people who have a bipartite patella, probably don’t even know it. But if an injury occurs and/or painful symptoms develop, then treatment may be needed.
Nonsurgical Treatment
Conservative care involves rest, over-the-counter nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen, and activity modification. Avoiding deep flexion such as squatting, excess use of the stairs, and resisted weight training are advised.
Separation of the synchondrosis can be treated with immobilization for four to six weeks. The knee is placed in full extension using a cylinder cast, knee immobilizer, or dynamic patellar brace. An immobilizer is a removable splint. It’s usually only taken off to wash the leg and remains in place the rest of the time. The dynamic brace immobilizes the knee in an extended (straight-leg) position with limited flexion (up to 30 degrees). The brace reduces pain by decreasing the pull on the patella from the quadriceps muscle. Once healing occurs and the cast or brace is no longer needed, then stretching exercises of the quadriceps muscle are prescribed.
Surgery
If conservative care with immobilization is not successful in alleviating swelling and pain, then surgery may be suggested. When the bipartite fragment is small, then the surgeon can simply remove the smaller fragment of bone. When the bipartite fragment is larger and also contains part of the joint surface, the surgeon may decide to try and force the two fragments to heal together or fuse. The connective tissue between the two fragments is removed first and the two bony fragments are then held together or stabilized with a metal screw or
pin. This is called internal fixation. The two fragments of bone heal
together or fuse, creating a solid connection between the two fragments. Although successful in reuniting the patella, the procedure may require several weeks of immobilization. As a result, knee stiffness may occur. This usually requires physical therapy once the bones have healed to regain strength and motion.
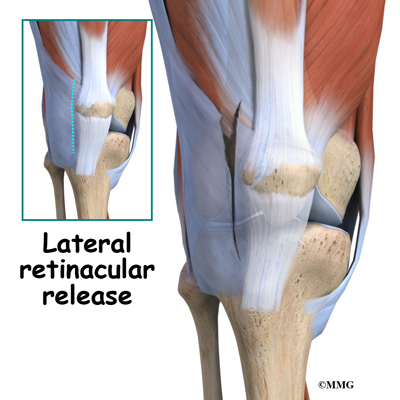
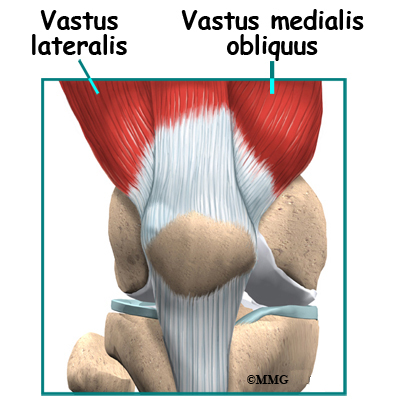
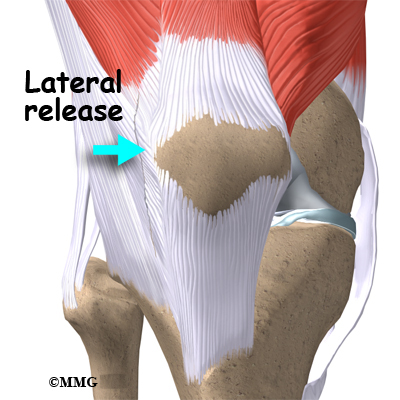
Another potential treatment option is a procedure called a lateral
retinacular release. It may be beneficial to remove the constant pull
of the vastus lateralis tendon (a part of the large quadriceps muscle
of the thigh) where it attaches to the bone of the bipartite fragment of the upper, outer patella. Simply cutting this attachment reduces the constant pull on the bony fragment. Healing of the two fragments may occur as a result.
Rehabilitation
What should I expect after Treatment?
Nonsurgical Rehabilitation
Most patients respond well to activity modification and immobilization. When the X-ray shows complete ossification of the two bone fragments, then you’ll be able to return to your regular activities. If there is no improvement after three months of conservative care, then surgery is considered.
After Surgery
Usually, the removal of a bipartite patella is a simple surgery with prompt relief of pain and quick recovery. Athletes can expect full range of motion, a stable knee, and a fairly rapid return to normal activity (one to two months). But runners and other athletes who have had an extended time of immobility, muscle weakness and atrophy, loss of normal joint motion, and patellar tracking problems may require a special rehab program. A physical therapist will prescribe and monitor a rehabilitation program starting with range of motion and quadriceps strengthening exercises.
Athletes will be progressed quickly to restore full motion and strength. An aerobic program to improve cardiovascular endurance is often needed after so many months of inactivity. Proprioception and functional activities are added in order to prepare the individual to return to full sports participation. Proprioceptive exercises help restore the joint’s sense of position. Proprioceptive activities are needed to restore normal movement and prevent further injury.
Pigmented Villonodular Synovitis of the Knee
A Patient’s Guide to Pigmented Villonodular Synovitis (PVNS) of the Knee
Introduction
Pigmented villonodular synovitis of the knee (PVNS) is a very rare disease. Pigmented villonodular synovitis is most often painless inflammation or swelling, and overgrowth of the lining of a joint. The growth can invade the nearby bone.
Eighty per cent of the time pigmented villonodular synovitis affects just one joint of the body, primarily the knee joint. The hip, shoulder, and the smaller joints in the hands and feet can also be affected.
Pigmented villonodular synovitis occurs in less than two persons per million per year. It occurs in both men and women commonly between the ages of 20 and 45 years.
This guide will help you understand
- what parts of the knee are involved
- how this condition develops
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts of the knee are affected?
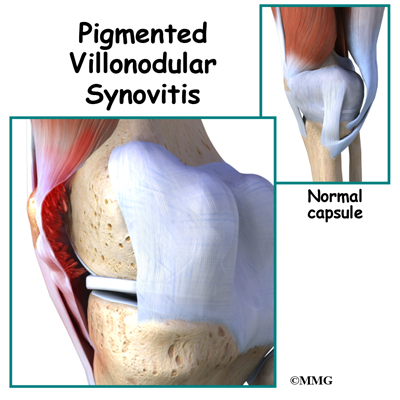
There are several types of joints in the body, but pigmented villonodular synovitis (PVNS) generally affects the synovial joints. Synovial joints are the most common joints in the body (90 percent). They are the most mobile of the joints.
The knee joint is a synovial joint. It is surrounded by synovial tissue which is tough. It is not stretchy or elastic. The synovial tissue forms a covering called a joint capsule around the joint. The joint capsule helps stabilize the joint. The soft padding on the ends of the bones is called articular cartilage. This helps the joint move smoothly. Ligaments and tendons help hold the joint together.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this condition?
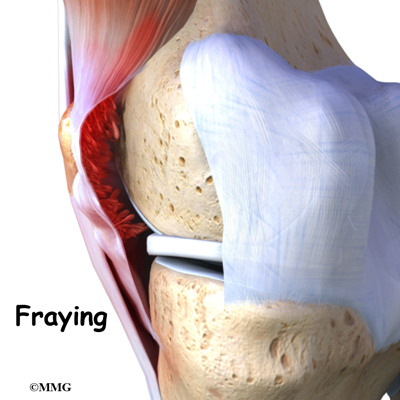
Villous means hair-like. In pigmented villonodular synovitis, the tissue that is affected may look frayed or hair-like. The synovial tissue can also appear folded. Sometimes the tissue will have round bumps or nodules. The nodular type is usually seen in tendons. Tissue affected by pigmented villonodular synovitis can contain deposits of fat. Pigmented means colored. The synovium and its fluid is often a brown color instead of clear. This is because blood, which contains iron, is deposited in the fluid.
Pigmented Villonodular Synovitis (PVNS) at one time was thought to be a form of malignant cancer. It is now considered a benign, or non-cancerous, inflammatory process.
It is not known if PVNS is due to injury. Patients have reported injury at some time to the affected joint, others do not. There does not seem to be a genetic cause. It happens in both men and women generally between the ages of 20 and 45 years. It occurs in less than two persons per million per year.
The exact cause is unknown. Some doctors believe it’s caused by abnormal metabolism of fat. Others think it may be caused by repetitive inflammation. Some feel that blood within the joint may cause the inflammatory change.
Symptoms
What are the symptoms?
Symptoms of pigmented villonodular synovitis (PVNS) of the knee include inflammation, swelling, stiffness, and tenderness around the joint. The pain can come and go.
Symptoms may feel like arthritis. The pain comes on slowly in the joint. There may be swelling, tenderness, and limited movement of the knee. The symptoms can come and go. Eighty per cent of the time PVNS affects the knee.
Sometimes a popping feeling is felt in the knee. Tenderness in the front part of the knee near the knee cap is usually noticed. The symptoms are rather “non-specific”, meaning that they can act like other problems. PVNS of the knee can easily be mistaken for a torn meniscus, or problems with the patella (knee cap).
There are two types of pigmented villonodular synovitis (PVNS). When it occurs in one large synovial joint of the body, such as the knee, it is considered diffuse. This is because the inflammation is more widespread within the joint. The synovial capsule, bursa, and tendon sheaths around the joint can all be involved. Even the bones in the knee joint can be affected.
The other type of pigmented villonodular synovitis is localized, or focal. This form is rare. It usually affects just the tendon sheaths around smaller joints in the hands and feet. This means there will be localized swelling and likely some tenderness along the tendons.
Diagnosis
How will my doctor diagnose this condition?
Your doctor will want to do a physical examination. He/she will want to measure range of motion of the knee joint. Your doctor will also want to determine if there is any swelling, nodules, tenderness, or fluid in the joint. Swelling in your knee may feel warm and be somewhat tender to palpation.
Imaging plays an important role in the diagnosis of pigmented villonodular synovitis (PVNS). Often, X-rays will be normal. Sometimes there will be cysts in the bone at the joint caused by the invasion of PVNS. There are usually no wear and tear changes like with arthritis.
MRI does not use x-rays. It uses magnetic waves. It allows the doctor to
see your tissues and bones in thin slices. You will need an MRI with
contrast. This means that you will have to have an IV inserted. The contrast
material is called gladolinium. The gladolinium will go where cells are more
active in your body. Cells tend to be more active in areas where there is
inflammation, and in tumors.
If PVNS has invaded the bone, your doctor will likely want you to have a computed tomography (CT) scan. This is a special form of xray. Like the MRI, it takes pictures in slices. This will require the injection of intravenous contrast so that tissues can be better evaluated.
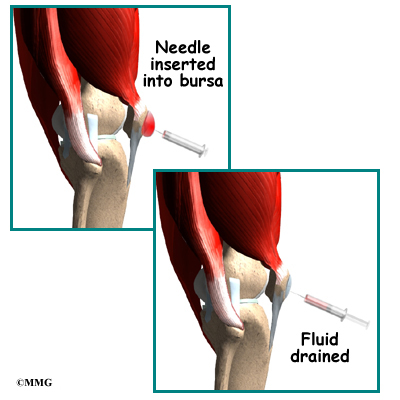
Your doctor may want to remove (aspirate) fluid from the joint that is affected. This is called arthrocentesis. The fluid is taken out with a needle. The fluid is then tested in the lab. If PVNS is the cause of the symptoms, most of the time the fluid will contain blood.
A contrast material may be injected into the joint after aspiration which will enhance the imaging studies. The contrast material will show irregular and nodular defects in imaging studies. This testing is called an arthrogram.
A biopsy of the affected tissue may be suggested. This can certainly confirm the diagnosis of PVNS. Computed tomography is used to perform the biopsy. Pictures are taken while your doctor is placing the needle in the tissue to be removed and tested. The tissue that is removed is then looked at in the lab. If pigmented villonodular synovitis (PVNS) is present, the synovium will be thickened. It will likely have both villous and nodular extra growth. Inflammation cells called giant cells are usually present. The synovium and fluid will be a brown color. This is due to deposits of iron in the blood.
Treatment
What treatment options are available?
Nonsurgical Treatment
There is no nonsurgical treatment. Because the PVNS can grow and invade bone, surgery is the recommended treatment.
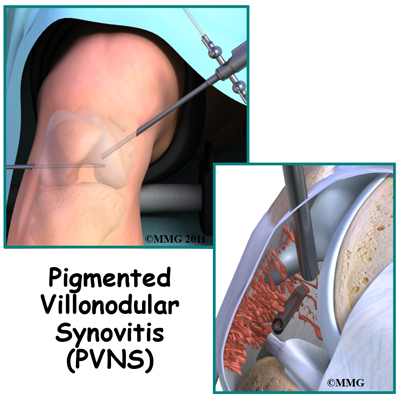
Surgery
Since PVNS can invade the joint, the most effective treatment is surgery. Removing the synovium and involved tissue is necessary. Since PVNS can grow back, sometimes radiation is recommended. Sometimes joint replacement may be needed.
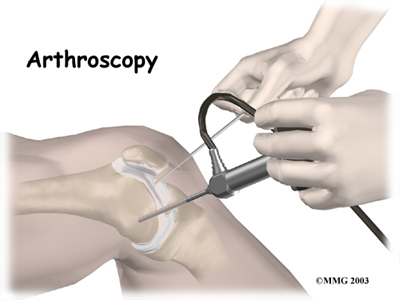
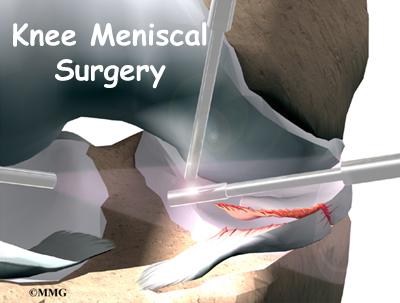
The recommended treatment for PVNS is removal of all the affected tissue. The surgery is called a synovectomy. Most of the time this surgery can be done with an arthroscope. Your surgeon makes tiny cuts in the skin over your joint. A thin tube with a tiny camera is used so your surgeon can see inside the joint. Instruments for cutting, smoothing, and removing tissue are passed through another thin tube. Arthroscopy is done as a “same day” surgery, meaning you can go home the same day.
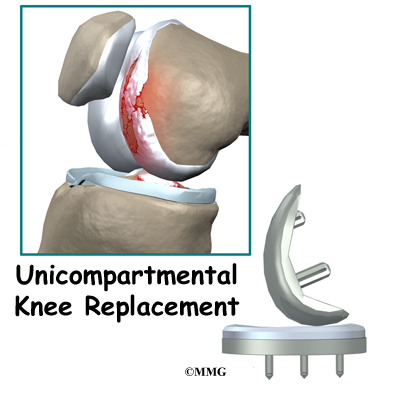
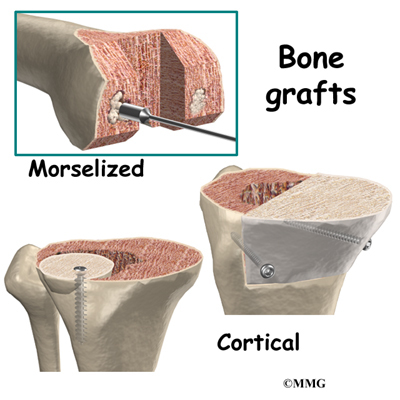
Sometimes the synovectomy is done by opening the knee joint. In diffuse pigmented villonodular synovitis (PVNS), all the tissue, including any bone that seems to be affected is removed. Grafting, or replacing the bone with transplanted bone may be necessary to maintain the joint. In some instances, a total joint replacement of the knee is necessary.
Diffuse PVNS grows back in nearly 50 percent of cases. If your surgeon is concerned that not all of the affected tissue was removed, you may have to have radiation therapy. It is also used if there is recurrence (return) of PVNS after it has been removed.
Radiation therapy is determined by a specialist called a radiation oncologist. A machine that emits radiation waves may be used to treat the affected area. Other times, radiation pellets can be inserted in the area that needs to be treated. This helps to keep the radiation contained, so that it harms as little as possible of the normal tissue.
Rehabilitation
What should I expect after Treatment?
After Surgery
Rehabilitation usually involves physical therapy. Range-of-motion exercises are important and may be started right away. Strengthening and conditioning exercises will allow you to return to your previous level of activity. When surgery involves the leg, walking with a walker or crutches may be recommended at first.
If knee joint replacement is required, you will likely be hospitalized for three to five days. A continuous passive motion (CPM) machine may be used while in the hospital or started when you return home. Your leg will rest in the machine that is plugged into a wall outlet. The machine slowly bends you knee. This allows range of motion for several minutes or hours at a time. Pain will need to be treated for several weeks. You will need to be careful about keeping your incision clean, and monitor closely for infection.
Use of cold packs will help minimize swelling from surgery for the first several days. You may need pain medication if over the counter anti-inflammatories or acetaminophen (Tylenol®) do not control your pain.
After treatment, your doctor will want you to follow up with him periodically. Repeat MRI is needed to evaluate possible return of the PVNS.
Knee Arthroscopy
A Patient’s Guide to Knee Arthroscopy
Introduction
The use of arthroscopy has revolutionized many different types of orthopedic surgery. During knee arthroscopy, a small video camera attached to a fiberoptic lens is inserted into the body to allow a physician or surgeon to see without making a large incision (arthro means joint scopy means look). The knee was the first joint in which the arthroscope was commonly used to both diagnose problems and to perform surgical procedures inside the knee joint.
This guide will help you understand
- what parts of the knee are involved
- what types of conditions can be treated
- what to expect after surgery
Anatomy
What parts of the knee are involved?
The knee joint is formed where the femur (lower end of the thighbone) connects with the tibia (upper end of the main lower leg bone). On the front of the joint is the patella (kneecap). The patella is what is called a sesamoid bone that is a part of the extensor mechanism of the knee joint. The extensor mechanism connects the large muscles of the thigh to the tibia; contracting the thigh muscles pulls on the tibia and allows us to straighten the knee. The parts of the extensor mechanism include the thigh muscles, the quadriceps tendon, the patella and the patella tendon.
The knee joint is surrounded by a water tight pocket called the joint capsule. This capsule is formed by the knee ligaments, connective tissue and synovial tissue. When the joint capsule is filled with sterile saline and is distended, the surgeon can insert the arthroscope into the pocket that is formed, turn on the lights and the camera and see inside the knee joint as if looking into an aquarium. The surgeon can see nearly everything that is inside the knee joint including: (1) the joint surfaces of the tibia, femur and patella, (2) the two menisci, (3) the two cruciate ligaments, and (4) the synovial lining of the joint.
There is one meniscus on each side of the knee joint. The C-shaped medial meniscus is on the inside part of the knee, closest to your other knee. (Medial means closer to the middle of the body.) The U-shaped lateral meniscus is on the outer half of the knee joint. (Lateral means further out from the center of the body.)
The menisci (plural for meniscus) protect the articular cartilage on the surfaces of the thighbone (femur) and the shinbone (tibia). Articular cartilage is the smooth, slippery material that covers the ends of the bones that make up the knee joint. The articular cartilage allows the joint surfaces to slide against one another without damage to either surface.
Ligaments are tough bands of tissue that connect the ends of bones together. The Anterior Cruciate Ligament (ACL) is located in the center of the knee joint where it runs from the backside of the femur (thighbone) to connect to the front of the tibia (shinbone).
The ACL runs through a special notch in the femur called the intercondylar notch and attaches to a special area of the tibia called the tibial spine.
The ACL is the main controller of how far forward the tibia moves under the femur. This is called anterior translation of the tibia. If the tibia moves too far, the ACL can rupture. The ACL is also the first ligament that becomes tight when the knee is straightened. If the knee is forced past this point, or hyperextended, the ACL can also be torn.
The Posterior Cruciate Ligament (PCL) is located near the back of the knee joint. It attaches to the back of the femur (thighbone) and the back of the tibia (shinbone) behind the ACL.
The PCL is the primary stabilizer of the knee and the main controller of how far backward the tibia moves under the femur. This motion is called posterior translation of the tibia. If the tibia moves too far back, the PCL can rupture.
Related Document: A Patient’s Guide to Knee Anatomy
Rationale
What does my surgeon hope to accomplish?
When knee arthroscopy first became widely available in the 1970’s it was used primarily to look inside the knee joint and make a diagnosis. Today, knee arthroscopy is used in performing a wide range of different types of surgical procedures on the knee joint including confirming a diagnosis, removing loose bodies, removing or repairing a torn meniscus, reconstructing torn ligaments, repairing articular cartilage and fixing fractures of the joint surface.
Your surgeon’s goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeons ability to perform that procedure. The arthroscope image is magnified and allows the surgeon to see better and clearer. The arthroscope allows the surgeon to see and perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. But remember, the arthroscope is only a tool. The results that you can expect from a knee arthroscopy depend on what is wrong with your knee, what can be done inside your knee to improve the problem and your effort at rehabilitation after the surgery.
Preparations
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. The therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted for surgery early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the procedure?
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia. In simple cases, local anesthesia may be adequate. Special braces are attached to the operating room table. These are used to safely cradle the leg and allows the surgeon to move the leg and bend the knee easily. Finally, sterile drapes are placed to create a sterile environment for the surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources and surgical instruments.
The surgeon begins the operation by making two or three small openings into the knee, called portals. These portals are where the arthroscope and surgical instruments are placed inside the knee. Care is taken to protect the nearby nerves and blood vessels. A small metal or plastic tube (or cannula) will be placed through one of the portals to inflate the knee with sterile saline.
The arthroscope is a small fiber-optic tube that is used to see and operate inside the joint. The arthroscope is a small metal tube about 1/4 inch in diameter (slightly smaller than a pencil) and about seven inches in length. The fiberoptics inside the metal tube of the arthroscope allows a bright light and TV camera to be connected to the outer end of the arthroscope. The light shines through the fiberoptic tube and into the knee joint. A TV camera is attached to the lens on the outer end of the arthroscope. The TV camera projects the image from inside the knee joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the knee joint) while moving the arthroscope to different places inside the knee joint.
Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be one with much smaller incisions. For example, simple removal of a torn meniscus or loose body can be done using two small 1/4 inch incisions. More extensive surgical procedures such as ligament reconstruction or fracture repair may require larger incisions.
Once the surgical procedure is complete, the arthroscopic portals and surgical incisions will be closed with sutures or surgical staples. A large bandage will be applied from mid thigh to the toes. Wrapping the entire leg with a compressive bandage reduces swelling and helps prevent blood clots in the leg. Once the bandage has been placed, you will be taken to the recovery room.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur during knee arthroscopy. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following knee arthroscopy are
- anesthesia complications
- thrombophlebitis
- infection
- equipment failure
- slow recovery
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following knee arthroscopy, it is possible that a postoperative infection may occur. This is very uncommon and happens in less than 1% of cases. You may experience increased pain, swelling, fever and redness or drainage from the incisions. You should alert your surgeon if you think you are developing an infection.
Infections are of two types: superficial or deep. A superficial infection may occur in the skin around the incisions or portals. A superficial infection does not extend into the joint and can usually be treated with antibiotics alone. If the knee joint itself becomes infected, this is a serious complication and will require antibiotics and possibly another surgical procedure to drain the infection.
Equipment Failure
Many of the instruments used by the surgeon to perform knee arthroscopy are small and fragile. These instruments can be broken resulting in a piece of the instrument floating inside of the knee joint. The broken piece is usually easily located and removed, but this may cause the operation to last longer than planned. There is usually no damage to the knee joint due to the breakage.
Different types of surgical devices (screws, pins, and suture anchors) are used to hold tissue in place during and after arthroscopy. These devices can cause problems. If one breaks, the free-floating piece may hurt other parts inside the knee joint, particularly the articular cartilage. The end of the tissue anchor may poke too far through tissue and the point may rub and irritate nearby tissues. A second surgery may be needed to remove the device or fix problems with these devices.
Slow Recovery
Not everyone gets quickly back to routine activities after knee arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscope allows surgeons to do a great deal of reconstructive surgery inside the knee without making large incisions. How fast you recover from knee arthroscopy depends on what type of surgery was done inside your knee. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the knee ligaments or articular cartilage tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss this with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic knee surgery.
After Surgery
What happens after surgery?
Knee arthroscopy is usually done on an outpatient basis meaning that patients go home the same day as the surgery. More complex ligament reconstructions that require larger incisions and surgery that alters bone may require a short stay in the hospital to control pain more aggressively and monitor the situation more carefully. You may also begin physical therapy while in the hospital.
The portals are covered with surgical strips, the larger incisions may have been repaired with either surgical staples or sutures and the knee may be wrapped in an elastic bandage (Ace wrap). Crutches are commonly used after knee arthroscopy. They may only be needed for one to two days after a simple procedure.
Patients who have had more complex reconstructive surgery may need to wear a knee brace for several weeks. The brace helps to protect the healing tissue inside the knee joint. You may be allowed to remove the brace at times during the day to do gentle range-of-motion exercises and bathe.
Follow your surgeon’s instructions about how much weight to place on your foot while standing or walking. Avoid doing too much, too quickly. You may be instructed to use a cold pack on the knee and to keep your leg elevated and supported.
Rehabilitation
What will my recovery be like?
Your rehabilitation will depend on the type of surgery required. You may not need formal physical therapy after simple procedures such as a partial meniscectomy. Some patients may simply do exercises as part of a home program after some simple instructions.
Many surgeons have patients take part in formal physical therapy after any type of knee arthroscopy procedure. Generally speaking, the more complex the surgery the more involved and prolonged your rehabilitation program will be. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. Physical therapists will also work with patients to make sure they are putting only a safe amount of weight on the affected leg.
Today, the arthroscope is used to perform quite complicated major reconstructive surgery using very small incisions. Remember, just because you have small incisions on the outside, there may be a great deal of healing tissue on the inside of the knee joint. If you have had major reconstructive surgery, you should expect full recovery to take several months. The physical therapist’s goal is to help you keep your pain under control and improve the range of motion and strength of your knee. When you are well under way, regular visits to your therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Pes Anserine Bursitis of the Knee
A Patient’s Guide to Pes Anserine (Goosefoot) Bursitis
Introduction
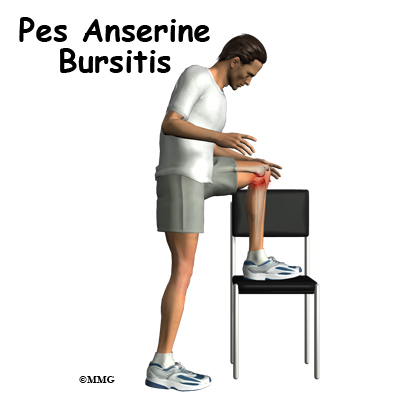
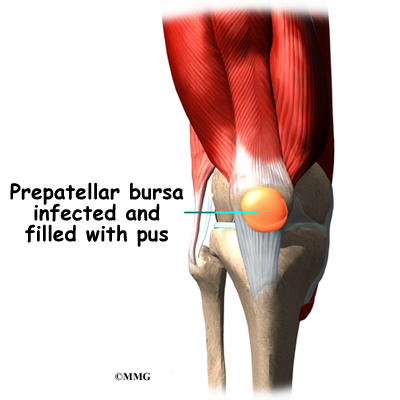
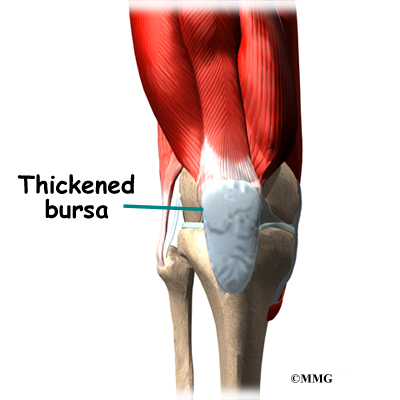
Bursitis of the knee occurs when constant friction on the bursa causes inflammation. The bursa is a small sac that cushions the bone from tendons that rub over the bone. Bursae can also protect other tendons as tissues glide over one another. Bursae can become inflamed and irritated causing pain and tenderness.
This guide will help you understand
- what part of the knee is affected
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts of the body are involved?
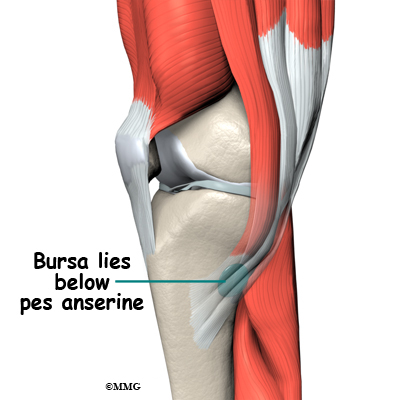
The pes anserine bursa is the main area affected by this condition. The pes anserine bursa is a small lubricating sac between the tibia (shinbone) and the hamstring muscle. The hamstring muscle is located along the back of the thigh.
There are three tendons of the hamstring: the semitendinosus, semimembranosus, and the biceps femoris. The semitendinosus wraps around from the back of the leg to the front. It inserts into the medial surface of the tibia and deep connective tissue of the lower leg. Medial refers to the inside of the knee or the side closest to the other knee.
Just above the insertion of the semitendinosus tendon is the gracilis tendon. The gracilis muscle adducts or moves the leg toward the body. The semitendinosus tendon is also just behind the attachment of the sartorius muscle. The sartorius muscle bends and externally rotates the hip. Together, these three tendons splay out on the tibia and look like a goosefoot. This area is called the pes anserine or pes anserinus.
The pes anserine bursa provides a buffer or lubricant for motion that occurs between these three tendons and the medial collateral ligament (MCL). The MCL is underneath the semitendinosus tendon.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this problem?
Overuse of the hamstrings, especially in athletes with tight hamstrings is a common cause of goosefoot. Runners are affected most often. Improper training, sudden increases in distance run, and running up hills can contribute to this condition.
It can also be caused by trauma such as a direct blow to this part of the knee. A contusion to this area results in an increased release of synovial fluid in the lining of the bursa. The bursa then becomes inflamed and tender or painful.
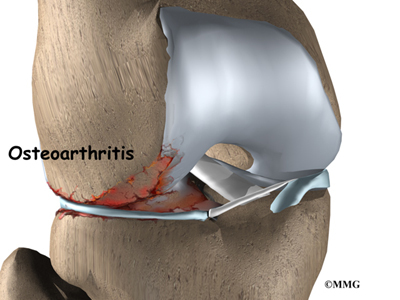
Anyone with osteoarthritis of the knee is also at increased risk for this condition. And alignment of the lower extremity can be a risk factor for some individuals. A turned out position of the knee or tibia, genu valgum (knock knees), or a flatfoot position can lead to pes anserine bursitis.
Symptoms
What does the condition feel like?
The patient often points to the pes anserine as the area of pain or tenderness. The pes anserine is located about two to three inches below the joint on the inside of the knee. This is referred to as the anterior knee or proximedia tibia. Proximedia is short for proximal and medial. This term refers to the front inside edge of the tibia.
Some patients also have pain in the center of the tibia. This occurs when other structures are also damaged such as the meniscus (cartilage). The pain is made worse by exercise, climbing stairs, or activities that cause resistance to any of these tendons.
Diagnosis
How do doctors diagnose this problem?
A history and clinical exam will help the physician differentiate pes anserine bursitis from other causes of anterior knee pain, such as patellofemoral syndrome or arthritis. An X-ray is needed to rule out a stress fracture or arthritis. An MRI may be needed to look for damage to other areas of the medial compartment of the knee. Fluid from the bursa may be removed and tested if infection is suspected.
The examiner will also assess hamstring tightness. This is done in the supine position (lying on your back). Your hip is flexed (bent) to 90 degrees. The knee is straightened as far as possible. The amount of knee flexion is an indication of how tight the hamstrings are. If you can straighten your knee all the way in this position, then you do not have tight hamstrings.
Treatment
What treatment options are available?
Nonsurgical Treatment
The goal of treatment for overuse injuries such as pes anserine bursitis is to reduce the strain on the injured tissues. Stopping the activity that brings on or aggravates the symptoms is the first step toward pain reduction.
Bedrest is not required but it may be necessary to modify some of your activities. This will give time for the bursa to quiet down and for the pain to subside. Patients are advised to avoid stairs, climbing, or other irritating activities. This type of approach is called relative rest
Ice and antiinflammatory medications can be used in the early, inflammatory phase. The ice is applied three or four times each day for 20 minutes at a time. Ice cubes wrapped in a thin layer of toweling or a bag of frozen vegetables applied to the area works well.
Athletes are often instructed by their physical therapist or athletic trainer to perform an ice massage. A cup of water is frozen in a Styrofoam container. The top edge of the container is torn away leaving a one-inch surface of ice that can be rubbed around the area. The Styrofoam protects the hand of the person holding the cup while applying the ice massage. The pes anserine area is massaged with the ice for 10 minutes or until the skin is numb. Caution is advised to avoid frostbite.
Over-the-counter nonsteroidal antiinflammatory drugs (NSAIDs) such as Ibuprofen may be advised. In some cases, the physician will prescribe stronger NSAIDs. Your physical therapist can also use a process called iontophoresis. Using an electric charge, an antiinflammatory drug can be pushed through the skin to the inflamed area. This method is called transdermal drug delivery. Iontophoresis puts a higher concentration of the drug directly in the area compared to taking medications by mouth. This process does not deliver as much drug as a local injection.
Improving flexibility is a key part of the prevention and treatment of this condition. Hamstring stretching is performed at least twice a day for a minimum of 30 seconds each time. Holding the stretch for a full minute has been proven even more effective. Some patients must perform this stretch more often, even once an hour if necessary.
Do not bounce during the stretch. Hold the position at a point of feeling the stretch but not so far that it is painful or uncomfortable. Deep breathing can help ease the discomfort. Try to stretch a little more as you breathe out.
Quadriceps strengthening is also important. This is especially true if there are other areas of the knee affected. The quadriceps muscle along the front of the thigh extends the knee and helps balance the pull of the hamstrings.
A special type of exercise program called closed kinetic chain (CKC) is performed for six to eight weeks to assist with quadriceps strengthening. The CKC may include single-knee dips, squats and leg presses. Resisted leg-pulls using elastic tubing are also included. The exercise program is prescribed by a physical therapist and gradually progressed during the eight-week session.
If these measures are not enough, your physician may inject the bursa with a solution of lidocaine (an anesthetic or numbing agent) combined with a steroid (an antiinflammatory). The steroid injection can be diagnostic as well. If the symptoms are improved, it is assumed the problem was coming from the pes anserine bursa.
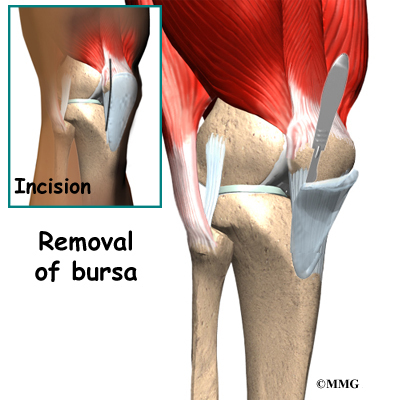
Surgery
Surgery is rarely needed for pes anserine bursitis. The bursa may be removed if chronic infection cannot be cleared up with antibiotics.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Pes anserine bursitis is considered a self-limiting condition. This means it usually responds well to treatment and will resolve without further intervention. Athletes may have to continue a program of hamstring stretching and CKC quadriceps strengthening on a regular basis.
Athletes may return to sports or play when the symptoms are gone and are no longer aggravated by certain activities. Protective gear for the knee may be needed for those individuals who participate in contact sports. During the rehab process, activity level and duration are gradually increased. If the symptoms don’t come back, the athlete can continue to progress to full participation in all activities.
After Surgery
If the bursa is removed, you follow the same steps of rehab and recovery outlined under Nonsurgical Treatment.
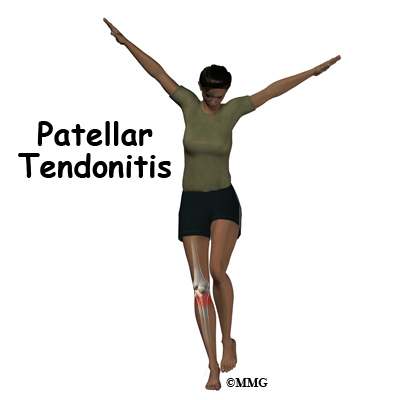
Patellar Tendonitis
A Patient’s Guide to Patellar Tendonitis
Introduction
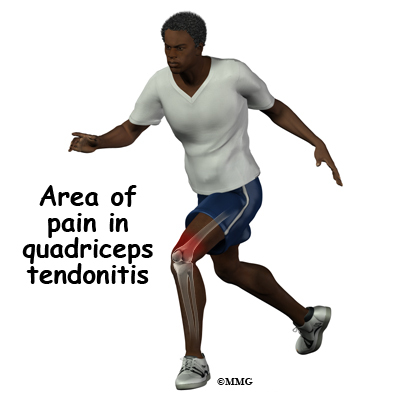
Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury. This produces pain, weakness, and swelling of the knee joint. Patellar tendonitis (also known as jumper’s knee) is a common overuse condition associated with running, repeated jumping and landing, and kicking.
This guide will help you understand
- what parts of the knee are involved
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the knee are involved?
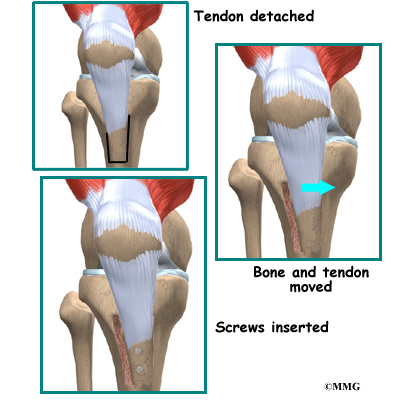
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the tibia lower leg bone.
The large quadriceps muscle ends in a tendon that inserts into the tibial tubercle, a bony bump at the top of the tibia (shin bone) just below the patella. The tendon together with the patella is called the quadriceps mechanism. Though we think of it as a single device, the quadriceps mechanism has two separate tendons, the quadriceps tendon on top of the patella and the infrapatellar tendon or patellar tendon below the patella.
Tightening up the quadriceps muscles places a pull on the tendons of the quadriceps mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
The long bones of the femur and the tibia act as level arms, placing force or load on the knee joint and surrounding soft tissues. The amount of load can be quite significant. For example, the joint reaction forces of the lower extremity (including the knee) are two to three times the body weight during walking and up to five times the body weight when running.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this problem?
Patellar tendonitis occurs most often as a result of stresses placed on the supporting structures of the knee. Running, jumping, and repetitive knee flexion into extension (e.g., rising from a deep squat) contribute to this condition. Overuse injuries from sports activities is the most common cause but anyone can be affected, even those who do not participate in sports or recreational activities.
There are extrinsic (outside) factors that are linked with overuse tendon injuries of the knee. These include inappropriate footwear, training errors (frequency, intensity, duration), and surface or ground (hard surface, cement) being used for the sport or event (such as running). Training errors are summed up by the rule of “toos”. This refers to training too much, too far, too fast, or too long. Advancing the training schedule forward too quickly is a major cause of patellar tendonitis.
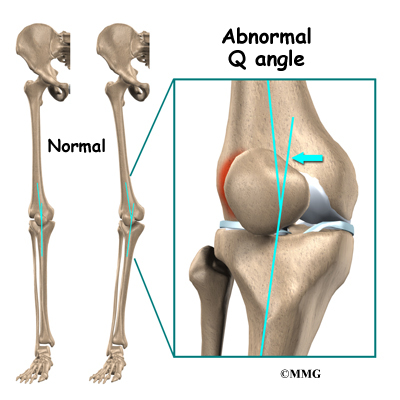
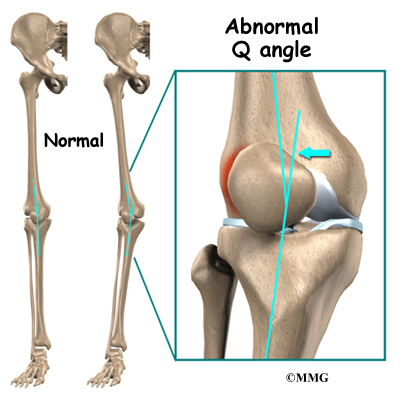
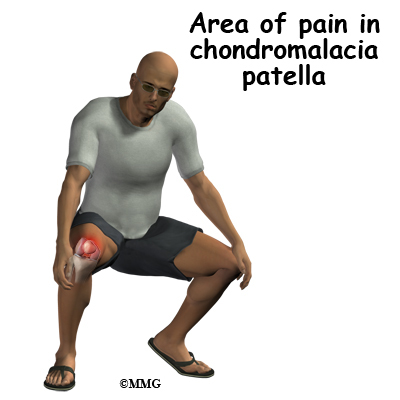
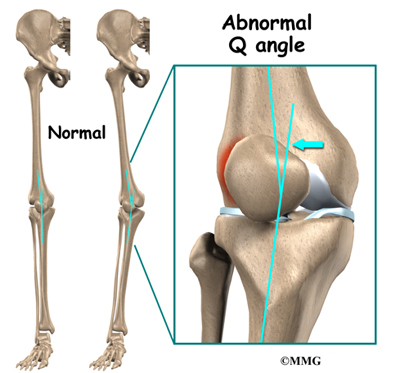
Intrinsic (internal) factors such as age, flexibility, and joint laxity are also important. Malalignment of the foot, ankle, and leg can play a key role in tendonitis. Flat foot position, tracking abnormalities of the patella, rotation of the tibia called tibial torsion, and a leg length difference can create increased and often uneven load on the quadriceps mechanism.
An increased Q-angle or femoral anteversion are two common types of malalignment that contribute to patellar tendonitis. The Q-angle is the angle formed by the patellar tendon and the axis of pull of the quadriceps muscle. This angle varies between the sexes. It is larger in women compared to men. The normal angle is usually less than 15 degrees. Angles more than 15 degrees create more of a pull on the tendon, creating painful inflammation.
Any muscle imbalance of the lower extremity (from the hip down to the toes) can impact the quadriceps muscle and affect the joint. Individuals who are overweight may have added issues with load and muscle imbalance leading to patellar tendonitis.
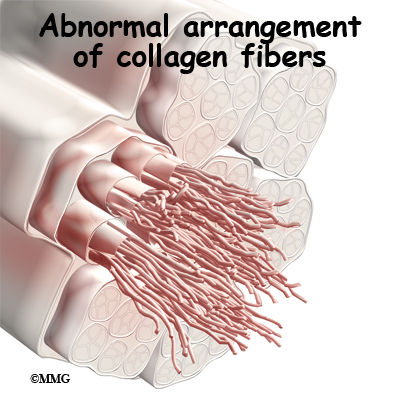
Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the muscle tendon junction may overcome the tendon’s ability to heal itself. Tissue breakdown occurs triggering an inflammatory response that leads to tendonitis.
Chronic tendonitis is really a problem called tendonosis. Inflammation is not present. Instead, degeneration and/or scarring of the tendon has developed. Chronic tendon injuries are much more common in older athletes (30 to 50 years old).
Symptoms
What does the condition feel like?
Pain from patellar tendonitis is felt just below the patella. The pain is most noticeable when you move your knee or try to kneel. The more you move your knee, the more tenderness develops in the area of the tendon attachment below the kneecap.
There may be swelling in and around the patellar tendon. It may be tender or very sensitive to touch. You may feel a sense of warmth or burning pain. The pain can be mild or in some cases the pain can be severe enough to keep the runner from running or other athletes from participating in their sport. The pain is worse when rising from a deep squat position. Resisted quadriceps contraction with the knee straight also aggravates the condition.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history of your knee problem followed by an examination of the knee, including the patella. There is usually tenderness with palpation of the inflamed tissues at the insertion of the tendon into the bone. The knee will be assessed for range of motion, strength, flexibility and joint stability.
The physician will look for intrinsic and extrinsic factors affecting the knee (especially sudden changes in training habits). Potential problems with lower extremity alignment are identified. The doctor will also check the hamstrings for telltale weakness and tightness.
X-rays may be ordered on the initial visit to your doctor. An X-ray can show fractures of the tibia or patella but X-rays do not show soft tissue injuries. In these cases, other tests, such as ultrasonography or magnetic resonance imaging (MRI), may be suggested. Ultrasound uses sound waves to detect tendon tears. MRIs use magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the knee. Usually, this test is done to look for injuries, such as tears in the quadriceps. This test does not require any needles or special dye and is painless.
Treatment
What treatment options are available?
Nonsurgical Treatment
The initial treatment for acute patellar tendonitis begins by decreasing the inflammation in the knee. Your physician may suggest relative rest and anti-inflammatory medications, such as aspirin or ibuprofen, especially when the problem is coming from overuse. Acetaminophen (Tylenol®) may be used for pain control if you can’t take anti-inflammatory medications for any reason.
Relative rest is a term used to describe a process of rest-to-recovery based on the severity of symptoms. Pain at rest means strict rest and a short time of immobilization in a splint or brace is required. When pain is no longer present at rest, then a gradual increase in activity is allowed so long as the resting pain doesn’t come back.
Physical therapy can help in the early stages by decreasing pain and inflammation. Your physical therapist may use ice massage, electrical stimulation, and ultrasound to limit pain and control (but not completely prevent) swelling. Some amount of inflammatory response is needed for a good healing response.
The therapist will prescribe stretching and strengthening exercises to correct any muscle imbalances. Eccentric muscle strength training helps prevent and treat injuries that occur when high stresses are placed on the tendon during closed kinetic chain activities. Eccentric contractions occur as the contracted muscle lengthens. Closed kinetic chain activities means the foot is planted on the floor as the knee bends or straightens.
A specific protocol of exercises may be needed when rehabilitating this injury. After a five-minute warm up period, stretches are performed. Next, in a standing position, the patient bends the knees and drops quickly into a squatting position, and then stands up again quickly. The goal is to do this exercise as quickly as possible. Eventually sandbags are added to the shoulders to increase the load on the tendon. All exercises must be done without pain.
Researchers have also discovered that patellar tendonitis responds to a concentric-eccentric program of exercises for the anterior tibialis muscle. The anterior tibialis muscle is located along the front of the lower leg. It is the muscle that helps you dorsiflex the ankle (pull your toes and ankle up toward the face).
You start with your foot in a position of full plantar flexion by rising up on your toes. Now drop down into a position of dorsiflexion. This is a concentric muscle contraction. Resistance of the foot and ankle from full dorsiflexion back into plantar flexion is the eccentric contraction. This exercise is repeated until the anterior tibialis fatigues. As your pain subsides, the program progresses so that eventually, you will just be doing the eccentric activities.
Flexibility exercises are often designed for the thigh and calf muscles. Specific exercises are used to maximize control and strength of the quadriceps muscles. You will be shown how to ease back into jumping or running sports using good training techniques. Off-season strength training of the legs, particularly the quadriceps muscles is advised.
Bracing or taping the patella can help you do exercises and activities with less pain. Most braces for patellofemoral problems are made of soft fabric, such as cloth or neoprene. You slide them onto your knee like a sleeve. A small buttress pads the side of the patella to keep it lined up within the groove of the femur. An alternative to bracing is to tape the patella in place. The therapist applies and adjusts the tape over the knee to help realign the patella. The idea is that by bracing or taping the knee, the patella stays in better alignment within the femoral groove. This in turn is thought to improve the pull of the quadriceps muscle so that the patella stays lined up in the groove. Patients report less pain and improved function with these forms of treatment.
Therapists also design special shoe inserts, called orthotics, to improve knee alignment and function of the patella. Proper footwear for your sport is important. The therapist will advise you in this area.
Prevention of future injuries through patient education is a key component of the treatment program. This is true whether conservative care or surgical intervention is required. Modification of intrinsic and extrinsic risk factors is essential.
Coaches, trainers, and therapists can work together to design a training program that allows you to continue training without irritating the tendon and surrounding tissues. Remember to warm up and stretch before exercise. Some experts recommend a cool down and stretching after exercise as well. Know your limits and don’t overdo it.
Use ice after activity if indicated by pain or swelling. Icing should be limited to no more than 20 minutes to avoid reflex vasodilation (increased circulation to the area to rewarm it causing further swelling). Heat may be used in cases of chronic tendinosis to stimulate blood circulation and promote tissue healing.
Whenever you have to miss exercising for any reason or when training for a specific event, adjust your training schedule accordingly. Avoid the “too” training errors mentioned earlier.
Surgery
Surgery is rarely needed when a wide range of protective measures, relative rest, ice, support, and rehab are used. If nonsurgical treatment fails to improve your condition, then surgery may be suggested. Surgery is designed to stimulate healing through revascularization (restoring blood supply). Weak, damaged tissue is removed and the injured tendon is repaired. Tissue remodeling through surgery can restore function.
Arthroscopic procedures can usually be done on an outpatient basis. This means you can leave the hospital the same day. If your problem requires a more involved surgical procedure where bone must be cut to allow moving the Patellar tendon attachment, you may need to spend one or two nights in the hospital.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Patellar tendonitis is usually self-limiting. That means the condition will resolve with rest, activity modification, and physical therapy. Recurrence of the problem is common for patients who fail to let the patellar tendon recover fully before resuming training or other aggravating activities.
Physical therapy for about four to six weeks is usually recommended. The aim of treatment is to calm pain and inflammation, to correct muscle imbalances, and to improve the function of the quadriceps mechanism.
With a well-planned rehabilitation program, most patients are able to return to their previous level of activity without recurring symptoms.
After Surgery
Many surgeons will have their patients take part in formal physical therapy after knee surgery. More involved surgeries for patellar realignment or restorative procedures for tendon tissue require a delay before going to therapy. And rehabilitation may be slower to allow the tendon to heal before too much strain can be put on the knee.
The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The physical therapist will choose exercises to help improve knee motion and to get the quadriceps muscles toned and active again. Muscle stimulation, using electrodes over the quadriceps muscle, may be needed at first to get the muscle moving again.
As the program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. The key is to get the soft tissues in balance through safe stretching and gradual strengthening.
The physical therapist’s goal is to help you keep your pain under control, ensure you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When you are well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Quadriceps Tendonitis
A Patient’s Guide to Quadriceps Tendonitis of the Knee
Introduction
Alignment or overuse problems of the knee structures can lead to strain, irritation, and/or injury of the quadriceps muscle and tendon. Quadriceps tendonitis produces pain, weakness, and swelling of the knee joint.
These problems can affect people of all ages but the majority of patients with overuse injuries of the knee (and specifically quadriceps tendonitis) are involved in soccer, volleyball, or running activities.
This guide will help you understand
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What is the quadriceps muscle/tendon, and what does it do?
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
The large quadriceps muscle ends in a tendon that inserts into the tibial tubercle, a bony bump at the top of the tibia (shin bone) just below the patella. The tendon together with the patella is called the quadriceps mechanism. Though we think of it as a single device, the quadriceps mechanism has two separate tendons, the quadriceps tendon on top of the patella and the patellar tendon below the patella.
Tightening up the quadriceps muscles places a pull on the tendons of the quadriceps mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
The long bones of the femur and the tibia act as level arms, placing force or load on the knee joint and surrounding soft tissues. The amount of load can be quite significant. For example, the joint reaction forces of the lower extremity (including the knee) are two to three times the body weight during walking and up to five times the body weight when running.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
How does this problem develop
Quadriceps tendonitis occurs most often as a result of stresses placed on the supporting structures of the knee. Running, jumping, and quick starts and stops contribute to this condition. Overuse injuries from sports activities is the most common cause but anyone can be affected, even those who do not participate in sports or recreational activities.
There are extrinsic (outside) factors that are linked with overuse tendon injuries of the knee. These include inappropriate footwear, training errors (frequency, intensity, duration), and surface or ground (hard surface, cement) being used for the sport or event (such as running). Training errors are summed up by the rule of toos. This refers to training too much, too far, too fast, or too long. Advancing the training schedule forward too quickly is a major cause of quadriceps tendonitis.
Intrinsic (internal) factors such as age, flexibility, and joint laxity are also important. Malalignment of the foot, ankle, and leg can play a key role in tendonitis. Flat foot position, tracking abnormalities of the patella, rotation of the tibia, and a leg length difference can create increased and often uneven load on the quadriceps mechanism. Any muscle imbalance of the lower extremity (from the hip down to the toes) can impact the quadriceps muscle and affect the joint. Individuals who are overweight may have added issues with load and muscle imbalance leading to quadriceps tendonitis.
Strength of the patellar tendon is in direct proportion to the number, size, and orientation of the collagen fibers that make up the tendon. Overuse is simply a mismatch between load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury can occur. Repeated microtrauma at the muscle tendon junction may overcome the tendon’s ability to heal itself. Tissue breakdown occurs triggering an inflammatory response that leads to tendonitis and even partial tears.
Chronic quadriceps tendonitis is really a problem called tendonosis. Inflammation is not present. Instead, degeneration and/or scarring of the tendon has developed. Chronic tendon injuries are much more common in older athletes (30 to 50 years old).
Symptoms
What does the condition feel like?
Pain from quadriceps tendonitis is felt in the area at the bottom of the thigh, just above the patella. The pain is most noticeable when you move your knee. The more you move your knee, the more tenderness develops in the area of the tendon attachment above the kneecap.
There may be swelling in and around the quadriceps tendon. It may be tender or very sensitive to touch. You may feel a sense of warmth or burning pain. The pain can be mild or in some cases the pain can be severe enough to keep the runner from running or other athletes from participating in their sport. Stiffness of the knee is common when you first get up in the morning (or after a long period of rest or inactivity), and during and after exercise
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history of your knee problem followed by an examination of the knee, including the patella. There is usually tenderness with palpation of the inflamed tissues at the insertion of the tendon into the bone. The knee will be assessed for range of motion, strength, flexibility and joint stability.
The physician will look for intrinsic and extrinsic factors affecting the knee (especially sudden changes in training habits). Potential problems with lower extremity alignment are identified. The doctor will also check to see if the quadriceps tendon is partially torn or ruptured. Weakness of the extensor mechanism is a sign of such an injury.
X-rays may be ordered on the initial visit to your doctor. An X-ray can show fractures or the presence of calcium deposits in the quadriceps muscle but X-rays do not show soft tissue injuries. In these cases, other tests, such as ultrasonography or magnetic resonance imaging (MRI), may be suggested. Ultrasound uses sound waves to detect tendon tears. MRIs use magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the knee. Usually, this test is done to look for injuries, such as tears in the quadriceps. This test does not require any needles or special dye and is painless.
Treatment
What treatment options are available?
Nonsurgical Treatment
The initial treatment for acute quadriceps tendonitis begins by decreasing the inflammation in the knee. Your physician may suggest relative rest and anti-inflammatory medications, such as aspirin or ibuprofen, especially when the problem is coming from overuse. Acetaminophen (Tylenol®) may be used for pain control if you can’t take anti-inflammatory medications for any reason.
Relative rest is a term used to describe a process of rest-to-recovery based on the severity of symptoms. Pain at rest means strict rest and a short time of immobilization in a splint or brace is required. When pain is no longer present at rest, then a gradual increase in activity is allowed so long as the resting pain doesn’t come back.
Physical therapy can help in the early stages by decreasing pain and inflammation. Your physical therapist may use ice massage, electrical stimulation, and ultrasound to limit pain and control (but not completely prevent) swelling. Some amount of inflammatory response is needed for a good healing response.
The therapist will prescribe stretching and strengthening exercises to correct any muscle imbalances. Eccentric muscle strength training helps prevent and treat injuries that occur when high stresses are placed on the tendon during closed kinetic chain activities. Eccentric contractions occur as the contracted muscle lengthens. Closed kinetic chain activities means the foot is planted on the floor as the knee bends or straightens.
Flexibility exercises are often designed for the thigh and calf muscles. Specific exercises are used to maximize control and strength of the quadriceps muscles. You will be shown how to ease back into jumping or running sports using good training techniques. Off-season strength training of the legs, particularly the quadriceps muscles is advised.
Bracing or taping the patella can help you do exercises and activities with less pain. Most braces for patellofemoral problems are made of soft fabric, such as cloth or neoprene. You slide them onto your knee like a sleeve. A small buttress pads the side of the patella to keep it lined up within the groove of the femur. An alternative to bracing is to tape the patella in place. The therapist applies and adjusts the tape over the knee to help realign the patella. The idea is that by bracing or taping the knee, the patella stays in better alignment within the femoral groove. This in turn is thought to improve the pull of the quadriceps muscle so that the patella stays lined up in the groove. Patients report less pain and improved function with these forms of treatment.
Therapists also design special shoe inserts, called orthotics, to improve knee alignment and function of the patella. Proper footwear for your sport is important. The therapist will advise you in this area.
Prevention of future injuries through patient education is a key component of the treatment program. This is true whether conservative care or surgical intervention is required. Modification of intrinsic and extrinsic risk factors is essential.
Coaches, trainers, and therapists can work together to design a training program that allows you to continue training without irritating the tendon and surrounding tissues. Remember to warm up and stretch before exercise. Some experts recommend a cool down and stretching after exercise as well. Know your limits and don’t overdo it.
Use ice after activity if indicated by pain or swelling. Icing should be limited to no more than 20 minutes to avoid reflex vasodilation (increased circulation to the area to rewarm it causing further swelling). Heat may be used in cases of chronic tendinosis to stimulate blood circulation and promote tissue healing.
Whenever you have to miss exercising for any reason or when training for a specific event, adjust your training schedule accordingly. Avoid the too training errors mentioned earlier.
Surgery
Surgery is rarely needed when a wide range of protective measures, relative rest, ice, support, and rehab are used. If nonsurgical treatment fails to improve your condition, then surgery may be suggested. Surgery is designed to stimulate healing through revascularization (restoring blood supply). Weak, damaged tissue is removed and the injured tendon is repaired. Tissue remodeling through surgery can restore function.
Arthroscopic procedures can usually be done on an outpatient basis. This means you can leave the hospital the same day. If your problem requires a more involved surgical procedure where bone must be cut to allow moving the quadriceps tendon attachment, you may need to spend one or two nights in the hospital.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Quadriceps tendonitis is usually self-limiting. That means the condition will resolve with rest, activity modification, and physical therapy. Recurrence of the problem is common for patients who fail to let the quadriceps tendon recover fully before resuming training or other aggravating activities.
Physical therapy for about four to six weeks is usually recommended. The aim of treatment is to calm pain and inflammation, to correct muscle imbalances, and to improve the function of the quadriceps mechanism.
With a well-planned rehabilitation program, most patients are able to return to their previous level of activity without recurring symptoms.
After Surgery
Many surgeons will have their patients take part in formal physical therapy after knee surgery for patellofemoral problems. More involved surgeries for patellar realignment or restorative procedures for tendon tissue require a delay before going to therapy. And rehabilitation may be slower to allow the tendon to heal before too much strain can be put on the knee.
The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The physical therapist will choose exercises to help improve knee motion and to get the quadriceps muscles toned and active again. Muscle stimulation, using electrodes over the quadriceps muscle, may be needed at first to get the muscle moving again.
As the program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. The key is to get the soft tissues in balance through safe stretching and gradual strengthening.
The physical therapist’s goal is to help you keep your pain under control, ensure you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When you are well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Chondromalacia Patella
A Patient’s Guide to Chondromalacia Patella
Introduction
The patella, or kneecap, can be a source of knee pain when it fails to function properly. Alignment or overuse problems of the patella can lead to wear and tear of the cartilage behind the patella. Chondromalacia patella is a common knee problem that affects the patella and the groove it slides in over the femur (thigh bone). This action takes place at the patellofemoral joint.
Chondromalacia is the term used to describe a patellofemoral joint that has been structurally damaged, while the term patellofemoral pain syndrome (PFPS) refers to the earlier stages of the condition. Symptoms are more likely to be reversible with PFPS.
This guide will help you understand
- what parts of the knee are affected
- how this condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What is the patella, and what does it do?
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The large quadriceps tendon together with the patella is called the quadriceps mechanism. Though we think of it as a single device, the quadriceps mechanism has two separate tendons, the quadriceps tendon on top of the patella and the patellar tendon below the patella.
Tightening up the quadriceps muscles places a pull on the tendons of the quadriceps mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
The underside of the patella is covered with articular cartilage, the smooth, slippery covering found on joint surfaces. This covering helps the patella glide (or track) in a special groove made by the thighbone, or femur. This groove is called the femoral groove.
Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These muscles are the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The vastus medialis obliquus (VMO) runs along the inside of the thigh, and the vastus lateralis (VL) lies along the outside of the thigh. If the timing between these two muscles is off, the patella may be pulled off track.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this problem?
Problems commonly develop when the patella suffers wear and tear. The underlying cartilage begins to degenerate, a condition most common in young athletes. Soccer players, snowboarders, cyclists, rowers, tennis players, ballet dancers, and runners are affected most often. But anyone whose knees are under great stress is at increased risk of developing chondromalacia patella.
Wear and tear can develop for several reasons. Acute injury to the patella or chronic friction between the patella and the femur can result in the start of patellofemoral pain syndrome. Degeneration leading to chondromalacia may also develop as part of the aging process, like putting a lot of miles on a car.
The main cause of knee pain associated with patellofemoral pain syndrome is a problem in the way the patella tracks within the femoral groove as the knee moves. Physical and biomechanical changes alter the stress and load on the patellofemoral joint.
The quadriceps muscle helps control the patella so it stays within this groove. If part of the quadriceps is weak for any reason, a muscle imbalance can occur. When this happens, the pull of the quadriceps muscle may cause the patella to pull more to one side than the other. This in turn causes more pressure on the articular cartilage on one side than the other. In time, this pressure can damage the articular cartilage leading to chondromalacia patella.
Weakness of the muscles around the hip can also indirectly affect the patella and can lead to patellofemoral joint pain. Weakness of the muscles that pull the hip out and away from the other leg, the hip abductor muscles, can lead to imbalances to the alignment of the entire leg – including the knee joint and the muscle balance of the muscles around the knee. This causes abnormal tracking of the patella within the femoral groove and eventually pain around the patella. Many patients are confused when their physical therapist begins exercises to strengthen and balance the hip muscles, but there is a very good reason that the therapist is focusing on this area.
A similar problem can happen when the timing of the quadriceps muscles is off. There are four muscles that form the quadriceps muscle group. As mentioned earlier, the vastus medialis obliquus (the muscle on the inside of the front of the thigh) and the vastus lateralis ( the muscle that runs down the outside part of the thigh) are two of these four muscles. People with patellofemoral problems sometimes have problems in the timing between the VMO and the VL. The VL contracts first, before the VMO. This tends to pull the patella toward the outside edge of the knee. The result is abnormal pressure on the articular surface of the patella.
Another type of imbalance may exist due to differences in how the bones of the knee are shaped. These differences, or anatomic variations, are something people are born with. Doctors refer to this the “Q angle”. Some people are born with a greater than normal angle where the femur and the tibia (shinbone) come together at the knee joint. Women tend to have a greater angle here than men. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the angle in the knee straightens, pushing the patella to the outside of the knee. In cases where this angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar problem as that described above. As the patella slides through the groove, it shifts to the outside. This places more pressure on one side than the other, leading to damage to the underlying articular cartilage.
Finally, anatomic variations in the bones of the knee can occur such that one side of the femoral groove is smaller than normal. This creates a situation where the groove is too shallow, usually on the outside part of the knee. People who have a shallow groove sometimes have their patella slip sideways out of the groove, causing a patellar dislocation. This is not only painful when it occurs, but it can damage the articular cartilage underneath the patella. If this occurs repeatedly, degeneration of the patellofemoral joint occurs fairly rapidly.
Symptoms
What does chondromalacia patella feel like?
The most common symptom is pain underneath or around the edges of the patella. The pain is made worse by any activities that load the patellofemoral joint, such as running, squatting, or going up and down stairs. Kneeling is often too painful to even try. Keeping the knee bent for long periods, as in sitting in a car or movie theater, may cause pain.
There may be a sensation like the patella is slipping. This is thought to be a reflex response to pain and not because there is any instability in the knee. Others experience vague pain in the knee that isn’t centered in any one spot.
The knee may grind, or you may hear a crunching sound when you squat or go up and down stairs. If there is a considerable amount of wear and tear, you may feel popping or clicking as you bend your knee. This can happen when the uneven surface of the underside of the patella rubs against the femoral groove. The knee may swell with heavy use and become stiff and tight. This is usually because of fluid accumulating inside the knee joint, sometimes called ‘water on the knee’. This is not unique to problems of the patella but sometimes occurs when the knee becomes inflamed.
Diagnosis
How do doctors diagnose the problem?
Diagnosis begins with a complete history of your knee problem followed by an examination of the knee, including the patella. X-rays may be ordered on the initial visit to your doctor. An X-ray can help determine if the patella is properly aligned in the femoral groove. Several X-rays taken with the knee bent at several different angles can help determine if the patella seems to be moving through the femoral groove in the correct alignment. The X-ray may show arthritis between the patella and thighbone, especially when the problems have been there for awhile.
Diagnosing problems with the patella can be confusing. The symptoms can be easily confused with other knee problems, because the symptoms are often similar. In these cases, other tests, such as magnetic resonance imaging (MRI), may be suggested. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the knee. Usually, this test is done to look for injuries, such as tears in the menisci or ligaments of the knee. Recent advances in the quality of MRI scans have enabled doctors to see the articular cartilage on the scan and determine if it is damaged. This test does not require any needles or special dye and is painless.
In some cases, arthroscopy may be used to make the definitive diagnosis when there is still a question about what is causing your knee problem. Arthroscopy is an operation that involves placing a small fiber-optic TV camera into the knee joint, allowing the surgeon to look at the structures inside the joint directly. The arthroscope allows your doctor to see the condition of the articular cartilage on the back of your patella. The vast majority of patellofemoral problems are diagnosed without resorting to surgery, and arthroscopy is usually reserved to treat the problems identified by other means.
There is no clear link between the severity of symptoms and X-ray or arthroscopic findings. Most often, the doctor relies upon the history, symptoms, and results of the examination.
Treatment
What treatment options are available?
Nonsurgical Treatment
Nonoperative treatment is usually recommended for this problem. Getting the pain and inflammation under control is the first step. The overall goals for a rehab plan are to improve muscle function and flexibility while providing pain relief or pain control.
Your physician may suggest rest and anti-inflammatory medications, such as aspirin or ibuprofen, especially when the problem is coming from overuse. Acetaminophen (Tylenol®) may be used for pain control if you can’t take anti-inflammatory medications for any reason. Activity modification, flexibility, and strengthening are key parts of the rehab program. Physical therapy can help in the early stages by decreasing pain and inflammation. Your physical therapist may use ice massage and ultrasound to limit pain and swelling.
Bracing or taping the patella can help you do exercises and activities with less pain. Most braces for patellofemoral problems are made of soft fabric, such as cloth or neoprene. You slide them onto your knee like a sleeve. A small buttress pads the side of the patella to keep it lined up within the groove of the femur.
An alternative to bracing is to tape the patella in place. The therapist applies and adjusts the tape over the knee to help realign the patella. The idea is that by bracing or taping the knee, the patella stays in better alignment within the femoral groove. This in turn is thought to improve the pull of the quadriceps muscle so that the patella stays lined up in the groove. Patients report less pain and improved function with these forms of treatment.
As the pain and inflammation become controlled, your physical therapist will work with you to improve flexibility, strength, and muscle balance in the knee. Quadriceps strengthening exercises to address deficits in knee extension strength include non-weight-bearing single-joint (e.g., knee extension) and weight-bearing multiple-joint exercises (e.g., seated leg press).
Non-weight bearing exercises are also known as open kinetic chain exercise. Weight-bearing exercises are referred as closed-chain exercise. Closed-chain exercises place less stress on the patellofemoral joint and may be used first to achieve improved function before progressing to open kinetic chain exercises. Studies also show greater VMO activity with closed kinetic chain exercise. And a closed-chain exercise program also addresses hip muscle weakness at the same time as knee muscle deficits.
The therapist will adjust your rehab program to provide you with the most pain free and effective method of treatment. The overall rehab program will include a home exercise program of stretching, agility exercises, balance activities, and strengthening designed to return you to your former level of pain free participation in sports and other activities.
Surgery
If nonsurgical treatment fails to improve your condition, surgery may be suggested. The procedure used for patellofemoral problems varies. In severe cases a combination of one or more of the following procedures may be necessary.
Arthroscopic Method
Arthroscopy is sometimes useful in the treatment of patellofemoral problems of the knee. Looking directly at the articular cartilage surfaces of the patella and the femoral groove is the most accurate way of determining how much wear and tear there is in these areas. Your surgeon can also watch as the patella moves through the groove, and may be able to decide whether or not the patella is moving normally. If there are areas of articular cartilage damage behind the patella that are creating a rough surface, special tools can be used by the surgeon to smooth the surface and reduce your pain. This procedure is sometimes referred to as shaving the patella.
Cartilage Procedure
In more advanced cases of patellar arthritis, surgeons may operate to repair or restore the damaged cartilage. The type of surgery needed for articular cartilage is based on the size, type, and location of the damage. Along with surgical treatment to fix the cartilage, other procedures may also be done to help align the patella so less pressure is placed on the healing cartilage.
Related Document: A Patient’s Guide to Articular Cartilage Problems of the Knee
Lateral Release
If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage.
In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as before the surgery. This helps to balance the quadriceps mechanism and equalize the pressure on the articular cartilage behind the patella.
Ligament Tightening Procedure
In some cases of severe patellar misalignment, a lateral release alone may not be enough. For problems of repeated patellar dislocations, the surgeon may also need to realign the quadriceps mechanism. In addition to the lateral release, the tendons on the inside edge of the knee (the medial side) may have to be tightened as well.
Bony Realignment
If the misalignment is severe, the bony attachment of the patellar tendon may also have to be shifted to a new spot on the tibia bone. Remember that the patellar tendon attaches the patella to the lower leg bone (tibia) just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove.
The surgeon removes a section of bone where the patellar tendon attaches on the tibia. This section of bone is then reattached on the tibia closer to the other knee.
Usually, the bone is reattached onto the tibia using screws. This procedure shifts the patella to the medial side. Once the surgery heals, the patella should track better within the center of the groove, spreading the pressure equally on the articular cartilage behind the patella.
Arthroscopic procedures to shave the patella or a simple lateral release can usually be done on an outpatient basis, meaning you can leave the hospital the same day. If your problem requires the more involved surgical procedure where bone must be cut to allow moving the patellar tendon attachment, you may need to spend one or two nights in the hospital.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Patients with chondromalacia may benefit from four to six weeks of physical therapy. The aim of treatment is to calm pain and inflammation, to correct muscle imbalances, and to improve function of the patella.
It is important to understand the need to keep your activity level below what will trigger more pain and tissue damage. You may need to ice your knee during the day and limit certain activities such as stairs, squatting, or running.
Good results can be expected when working slowly but steadily on flexibility and strengthening exercises. The moto of no pain, no gain does not apply to this problem. The most successful program is one of common sense. If an activity causes pain, then reduce the frequency, intensity, or duration of that activity until you are once again pain free. Gradually build up what you can do while maintaining your pain free status.
Muscle imbalances are commonly treated with stretching and strengthening exercises but improvement usually takes at least six to eight weeks. You may need to continue a modified program of flexibility and strengthening exercises to maximize control and strength of the quadriceps muscles. This type of program done two to three times each week may be needed for several more months (or longer if you continue to experience pain during progressive sports participation).
After Surgery
Many surgeons will have their patients take part in formal physical therapy after knee surgery for patellofemoral problems. Patients undergoing a patellar shaving usually begin rehabilitation right away. More involved surgeries for patellar realignment or restorative procedures for the articular cartilage require a delay before going to therapy. And rehabilitation may be slower to allow the bone or cartilage to heal before too much strain can be put on the knee.
The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The physical therapist will choose exercises to help improve knee motion and to get the quadriceps muscles toned and active again. Muscle stimulation, using electrodes over the quadriceps muscle, may be needed at first to get the muscle moving again.
As the program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. The key is to get the soft tissues in balance through safe stretching and gradual strengthening.
The physical therapist’s goal is to help you keep your pain under control, ensure you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When you are well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Unicompartmental Knee Replacement
A Patient’s Guide to Unicompartmental Knee Replacement
Introduction
A painful knee can severely affect your ability to lead a full, active life. Over the last 25 years, major advancements in artificial knee replacement have improved the outcome of the surgery greatly. One of the more recent advances in knee replacement surgery is the unicompartmental knee replacement (also known as a unicondylar knee replacement). This type of knee replacement is less invasive than a full knee replacement. The operation is designed to replace only the portions of the joint that are most damaged by arthritis. This can have significant advantages, especially in younger patients who may need to have a second artificial knee replacement as the first one begins to wear out. Removing less bone during the initial operation makes it much easier to perform a revision artificial knee replacement later in life.
This guide will help you understand:
- what your surgeon hopes to achieve
- what happens during the procedure
- what to expect after your operation
Anatomy
What is the normal anatomy of the knee?
The knee joint is formed where the femur (thighbone) meets the tibia (shinbone). A smooth cushion of articular cartilage covers the end surfaces of both of these bones so that they slide against one another smoothly. The articular cartilage is kept slippery by joint fluid made by the synovial membrane (joint lining). The fluid is contained in a soft tissue enclosure around the knee joint called the joint capsule.
View animation of smooth movement
The patella, or kneecap, is the movable bone on the front of the knee. It is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The surface on the back of the patella is covered with articular cartilage. It glides within a groove on the front of the femur.
There are two femoral condyles in each knee. The medial femoral
condyle (the one closest to the other knee) and the lateral femoral condyle (on the outside half of the knee joint).
Related Document: A Patient’s Guide to Knee Anatomy
Rationale
What does the surgeon hope to achieve?
The main reason for replacing any arthritic joint with an artificial joint is to stop the bones from rubbing against each other. This rubbing causes pain. Replacing the painful and arthritic joint with an artificial joint gives the joint a new surface, which moves smoothly and without causing pain. The goal is to help people return to many of their activities with less pain and with greater freedom of movement.
View animation of smooth movement
Preparation
How should I prepare for surgery?
The decision to proceed with surgery should be made jointly by you and your surgeon. The decision should only be made after you feel that you understand as much as possible about the procedure.
Once you decide to proceed with surgery, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your regular doctor. This is to ensure that you are in the best possible condition to undergo the operation. You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery. Your therapist will begin the teaching process before surgery to make sure you are ready for rehabilitation afterwards.
One purpose of the preoperative visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, the presence of swelling, and the available movement and strength of each knee.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will practice some of the exercises used just after surgery. You will also be trained in the use of either a walker or crutches. Whether the surgeon uses a cemented or uncemented artificial knee will determine how much weight you will initially apply through your foot while walking. Finally, an assessment will be made of any needs you will have at home once you’re released from the hospital.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the unicompartmental artificial knee itself.
There are two major types of artificial knee replacements:
- cemented prosthesis
- uncemented prosthesis
Both are still widely used. In many cases a combination of the two types is used. The decision to use a cemented or uncemented artificial knee is usually made by the surgeon based on your age, your lifestyle, and the surgeon’s experience.
Each prosthesis is made up of two main parts.
The tibial component (bottom portion) replaces the top surface of the lower bone, the tibia. The femoral component (top portion) replaces the bottom surface of the upper bone (the femoral condyle).
The femoral component is made of metal. The tibial component is usually made of two parts: a metal tray that is attached directly to the bone, and a plastic spacer that provides the slick surface. The plastic used is so tough and slick that you could ice skate on a sheet of it without much damage to the material.
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis has a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
The Operation
To begin the procedure, the surgeon makes an incision on the front of the knee to allow access to the joint. Several different approaches can be used to make the incision depending on whether the outer half (the lateral compartment) or the inner half (the medial compartment) is being replaced. The incisions used to perform the unicompartmental knee replacement are much smaller than those used to perform a traditional artificial knee replacement. For this reason, this surgery is sometimes referred to as minimally invasive.
Once the knee joint is opened, a special positioning device (a cutting guide) is placed on the end of the femur. This cutting guide is used to ensure that the bone is cut in the proper alignment to the leg’s original angles, even if the arthritis has made you bowlegged or knock-kneed. With the help of the cutting guide, the surgeon cuts several pieces of bone from the end of the femur. The artificial knee will replace these worn surfaces with a metal surface.
View animation of removing the femoral joint surfaces
View animation of preparing the femoral joint surfaces
Next, the surface of the tibia is prepared. Another type of cutting guide is used to cut the tibia in the correct alignment.
View animation of preparing the tibial joint surfaces
The metal femoral component is then placed on the femur. In the uncemented prosthesis, the metal piece is held snugly onto the femur because the femur is tapered to accurately match the shape of the prosthesis. The metal component is pushed onto the end of the femur and held in place by friction. In the cemented variety, epoxy cement is used to attach the metal prosthesis to the bone.
The metal tray that holds the plastic spacer is then attached to the top of the tibia. This metal tray is either cemented into place or held with screws if the component is of the uncemented variety. The screws are primarily used to hold the tibial tray in place until bone grows into the porous coating. The screws remain in place and are not removed.
The plastic spacer is then attached to the metal tray of the tibial component. If this component should wear out while the rest of the artificial knee is sound, it can be replaced. The replacement procedure is sometimes called a retread.
View animation of component placement
View animation of completed unicompartmental knee replacement
Finally, the soft tissues are sewn back together, and staples are used to hold the skin incision together.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following artificial knee replacement are
- anesthesia complications
- thrombophlebitis
- infection
- stiffness
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following an artificial joint surgery. The chance of getting an infection following artificial knee replacement is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want you to take antibiotics when you have dental work or surgical procedures on your bladder and colon to reduce the risk of spreading germs to the joint.
Stiffness
In some cases, the ability to bend the knee does not return to normal after knee replacement surgery. To be able to use the leg effectively to rise from a chair, the knee must bend at least to 90 degrees. A desirable range of motion is greater than 110 degrees.
The most important factor in determining range of motion after surgery is whether the ligaments and soft tissues were balanced during surgery. The surgeon tries to get the knee in the best alignment so there is equal tension on all the ligaments and soft tissues.
Sometimes extra scar tissue develops after surgery and can lead to an increasingly stiff knee. If this occurs, your surgeon may recommend taking you back to the operating room, placing you under anesthesia once again, and manipulating the knee to regain motion. Basically, this allows the surgeon to break up and stretch the scar tissue without you feeling it. The goal is to increase the motion in the knee without injuring the joint.
Loosening
The major reason that artificial joints eventually fail continues to be a process of loosening where the metal or cement meets the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from an artificial knee, but in some cases the knee will loosen earlier than that. A loose prosthesis is a problem because it usually causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the knee replacement.
Related Document: A Patient’s Guide to Revision Arthroplasty of the Knee
After Surgery
What happens after surgery
Some orthopedic surgeons recommend a device known as a continuous passive motion (CPM) machine immediately after surgery. The unit is thought to help prevent blood clots and speed healing of the wound. It may help patients get by with less need for medication. The unit may help improve knee mobility after knee replacement surgery. However, patients seem to do equally well in regaining knee motion by doing their exercises.
You may also have physical therapy treatments once or twice each day as long as you are in the hospital. Therapy treatments will address the range of motion in the knee. Gentle movement will be used to help you bend and straighten the knee. If you are using a CPM device, it will be checked for alignment and settings. Your leg may be elevated to help drain extra fluid in the leg.
Your therapist will also go over exercises to help improve knee mobility and to start exercising the thigh and hip muscles. Ankle movements are used to help pump swelling out of the leg and to prevent the possibility of a blood clot.
When you are stabilized, your therapist will help you get up for a short outing using your crutches or your walker.
Most patients are able to go home after spending one to two days in the hospital. In some cases, minimally invasive unicompartmental surgery can be done as an outpatient – meaning you can go home the same day.
You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and access the bathroom. It is also important that you regain a good muscle contraction of the quadriceps muscle and that you gain improved knee range of motion. Patients who still need extra care may be sent to a different unit until they are safe and ready to go home.
Most orthopedic surgeons recommend regular checkups after your artificial joint replacement. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends. You should always consult your orthopedic surgeon if you begin to have pain in your artificial joint, or if you begin to suspect something is not working correctly.
Most patients who have an artificial joint will have episodes of pain, but when you have pain that lasts longer than a couple of weeks you should consult your surgeon. The surgeon will examine your knee in search of reasons for the pain. X-rays may be taken of your knee to compare with x-rays taken earlier to see whether the artificial joint shows any evidence of loosening.
Rehabilitation
What should I expect during my rehabilitation?
Once discharged from the hospital, you may see your therapist for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on knee range of motion. In some cases you may require additional visits at home before beginning outpatient physical therapy. Home therapy visits end when you can safely leave the house.
Visits to the physical therapist’s office come next. Your therapist may use heat, ice, or electrical stimulation to reduce any remaining swelling or pain.
You should continue to use your walker or crutches as instructed. If you had a cemented procedure, you’ll advance the weight you place through your sore leg as much as you feel comfortable. If yours was a noncemented procedure, place only the toes down until you’ve had a follow-up x-ray and your surgeon or therapist directs you to put more weight through your leg (usually by the fifth or sixth week postoperatively).
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, thigh, and calf muscles. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the knee joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the knee.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, rising on your toes, and bending down. Specific exercises may then be chosen to simulate work or hobby demands.
Many patients have less pain and better mobility after having knee replacement surgery. Your therapist will work with you to help keep your knee joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new knee joint. Heavy sports that require running, jumping, quick stopping or starting, and cutting are discouraged. Cycling, swimming, and level walking are encouraged, as are low impact sports like golfing or bowling.
Your therapist’s goal is to help you improve knee range of motion, maximize strength, and improve your ability to do your activities. When you are well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Meniscal Surgery
A Patient’s Guide to Meniscal Surgery
Introduction
The meniscus is very important to the long-term health of the knee. In the past, surgeons would simply take out part or all of an injured meniscus. But today’s surgeons know that removing the meniscus can lead to early knee arthritis. Whenever possible, they try to repair the tear. If the damaged area must be removed, care is taken during surgery to protect the surrounding healthy tissue.
This guide will help you understand
- what parts of the knee are treated during meniscal surgery
- what operations are used to treat a damaged meniscus
- what to expect before and after meniscal surgery
Anatomy
What parts of the knee are involved?
There is one meniscus on each side of the knee joint. The C-shaped medial meniscus is on the inside part of the knee, closest to your other knee. (Medial means closer to the middle of the body.) The U-shaped lateral meniscus is on the outer half of the knee joint. (Lateral means further out from the center of the body.)
The menisci (plural for meniscus) protect the articular cartilage on the surfaces of the thighbone (femur) and the shinbone (tibia). Articular cartilage is the smooth, slippery material that covers the ends of the bones that make up the knee joint. The articular cartilage allows the joint surfaces to slide against one another without damage to either surface.
Most of the meniscus is avascular, meaning no blood vessels go to it. Only its outer rim gets a small supply of blood. Doctors call this area the red zone. The ends of a few vessels in the red zone may actually travel inward to the middle section, the red-white zone. The inner portion of the meniscus, closest to the center of the knee, is called the white zone. It has no blood vessels at all. Although a tear in the outer rim has a good chance of healing, damage further in toward the center of the meniscus will not heal on its own.
Related Document: A Patient’s Guide to Knee Anatomy
Related Document: A Patient’s Guide to Meniscal Injuries
Rationale
What does my surgeon hope to accomplish?
The meniscus is a pad of cartilage that acts like a shock absorber to protect the knee. The meniscus is also vital for knee stability. When the meniscus is damaged or is surgically removed, the knee joint can become loose, or unstable. Without the protection and stability of a healthy meniscus, the surfaces of the knee can suffer wear and tear, leading to a condition called osteoarthritis.
Related Document: A Patient’s Guide to Knee Osteoarthritis
Most tears of the meniscus do not heal on their own. A small tear in the outer rim (the red zone) has a good chance of healing. However, tears in the inner part of the meniscus often require surgery. When tears in this area are causing symptoms, they tend to get bigger. This puts the articular cartilage on the surfaces of the knee joint at risk of injury.
Surgeons aim to save the meniscus. If an injured part must be removed, only the smallest amount of the meniscus is taken out. Preserving the nearby areas of the meniscus is vital for keeping the knee healthy. If a tear can possibly be repaired, surgeons will recommend a meniscal repair.
A torn meniscus may cause symptoms of pain and swelling and sometimes catching and locking. The goal of surgery is to take these symptoms away. When the knee locks and you have to tug on it to get it moving, a small flap from a meniscal tear may have developed. The flap may be getting caught in the knee joint as you bend it. Or a small piece of the meniscus could actually be floating around inside the joint. This fragment, called a loose body, can get lodged between the moving parts of the knee, causing the knee to lock. In these cases, surgery may be needed, sometimes right away, to fix the flap or to remove the loose body.
Only when the majority of the meniscus is damaged beyond repair is the entire meniscus removed. Surgeons are experimenting with solutions to replace the meniscus.
Preparations
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. The therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted for surgery early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during meniscal surgery?
Meniscal surgery is done using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during arthroscopy. The surgeon does not need to open the knee joint.
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia. The surgeon begins the operation by making two or three small openings into the knee, called portals. These portals are where the arthroscope and surgical instruments are placed inside the knee. Care is taken to protect the nearby nerves and blood vessels.
Partial Meniscectomy
The procedure to carefully remove a damaged portion of the meniscus is called partial meniscectomy. The surgeon starts by inserting the arthroscope into one of the portals. A probe is placed into another portal. The surgeon watches on a screen while probing the meniscus. All parts of the inside of the knee joint are examined. When a meniscal tear is found, the surgeon determines the type and location of the tear. Surgical instruments are placed into another portal and are used to remove the torn portion of meniscus.
When the problem part of the meniscus has been removed, the surgeon checks the knee again with the probe to be sure no other tears are present. A small motorized cutter is used to trim and shape the cut edge of the meniscus. The joint is flushed with sterile saline to wash away debris from the injury or from the surgery. The portals are closed with sutures.
Meniscal Repair
Suture Repair
View animation of sewing the edges of a torn meniscus
Using the arthroscope and a probe, the surgeon locates the tear. The probe is used to push the torn edges of the meniscus together. A small rasp or shaver is used to roughen the edges of the tear. Then a hollow tube called a cannula is inserted through one of the portals. The surgeon threads a suture through the cannula and into the knee joint. The suture is sewn into the two edges of the tear. The surgeon tugs on the thread to bring the torn edges close together. The suture is secured by tying two to three knots. Additional sutures are placed side by side until the entire tear is fixed.
An alternate method is to pierce the knee joint with one or two curved needles. The needle goes from the outer edge of the meniscus completely through the tear. The surgeon may feed a suture from another portal into the end of the needle. Or the suture can be threaded into the needle from the outside of the knee. Both ways get the suture through the tear and allow the surgeon to sew the torn edges of the meniscus together.
Suture Anchor Repair
View animation of anchoring the edges of a torn meniscus
Special fasteners, called suture anchors, are sometimes used to anchor the torn edges of the meniscus together. These implants are biodegradable, meaning they eventually break down and are absorbed by the body. Suture anchors have barbed shafts and are pointed like an arrow. They work like a staple or straight pin to hold the healing tissues together.
Repairs using suture anchors work best for younger patients who have a single tear near the outer rim (red zone) of the meniscus. (As described earlier, this part of the meniscus has the richest blood supply.) A probe is often used to line up the torn edges of the meniscus. Then the surgeon uses a small surgical tool to punch an arrow through the damaged part of the meniscus. Usually only two or three arrows are needed. Larger tears may require up to six arrows. The arrows anchor the two torn edges together while the tear heals. It takes about six months before the arrows begin to be absorbed by the body.
Meniscal Transplantation
If the meniscus cannot be repaired or has been previously removed, a new form of treatment may offer a way to slow the onset of knee arthritis. Meniscal transplantation uses borrowed tissue to take the place of the original meniscus.
Experiments have been tried using various replacement materials. One material that is showing promise is an allograft. An allograft is tissue that is from a donor, usually preserved human meniscus tissue. Because it is so new, this surgery is currently only available for select patients in a limited number of locations.
View animation of removing the meniscus
View animation of preparing the surgical site
View animation of placing the allograft
View animation of suturing the allograft in place
Using the arthroscope, the surgeon removes remnants of the old meniscus. Next, the allograft is prepared. Small sutures are placed around the edges of the allograft. The surgeon slides the allograft with the sutures into the knee through a small incision. The allograft is sewn in place onto the tibia bone. Surgical instruments, including a cannula or needle (described earlier), may be used to secure additional sutures. Some surgeons also use special anchors to firmly fix the allograft in place. A probe is used to make sure the transplanted meniscus holds securely. The arthroscope is removed, and the portals are sewn shut.
Complications
What can go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following meniscal surgery are
- anesthesia complications
- thrombophlebitis
- infection
- suture anchor problems
- graft failure
- slow recovery
- ongoing pain
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the skin portals can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
Suture Anchor Problems
Suture anchors can cause problems. If one breaks, the free-floating piece may hurt other parts inside the knee joint, particularly the articular cartilage. Also, the end of the anchor may poke too far through the meniscus. If so, the point may rub and irritate nearby tissues. A second surgery may be needed to fix problems with suture anchors.
Graft Failure
Surgeries where tissue is grafted into the body, like bone marrow or kidney transplants, have a high risk that the body will reject the graft. This is not so in meniscal transplant surgery. The preserved graft contains no live cells, so it doesn’t have to be matched up with the person getting the graft. Also, the properties of meniscal tissue makes rejection of a transplanted graft rare. The main reason for graft failure in meniscal transplant surgery occurs when patients try to do too much, too soon after surgery. Doing sports where there are quick starts and stops, sharp pivoting, and jumping can cause the graft to fail. If the graft tears, another transplant surgery will be needed.
Slow Recovery
Not everyone after meniscal surgery gets quickly back to routine activities. Some people feel better and have less swelling, but they still find it hard to do normal activities even several months after surgery. Others with damage in their knee ligaments or in the articular cartilage also tend to have a slower recovery.
Ongoing Pain
Pain relief does not always occur with meniscal surgery. If you have pain that continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after meniscal surgery?
Meniscal surgery is done on an outpatient basis. Patients usually go home the same day as the surgery. The portals are covered with surgical strips, and the knee may be wrapped in an elastic bandage.
Crutches are used after meniscal surgery. They may only be needed for one to two days after a simple meniscectomy. Surgeons specify how much weight can be borne after meniscal repair or allograft transplant. Patients having meniscal repair are usually told not to place any weight on the foot for four to six weeks after surgery. After a transplant procedure, most patients are instructed to touch only the toes of the operated leg on the ground for four to six weeks. Some sugeons allow their patients to place a comfortable amount of weight on the foot four weeks after repair or transplant surgery.
Patients who have had a meniscal repair or transplant usually wear a knee brace for at least four weeks. The brace keeps the knee straight. It is removed often during the day to do easy range-of-motion exercises for the knee.
Follow your surgeon’s instructions about how much weight to place on your foot while standing or walking. Avoid doing too much, too quickly. You may be told to use a cold pack on the knee and to keep your leg elevated and supported.
Rehabilitation
What will my recovery be like?
Your rehabilitation will depend on the type of surgery you had. You probably won’t need formal physical therapy after partial meniscectomy. Most patients can do their exercises as part of a home program. If you require outpatient physical therapy, you will probably need to attend therapy sessions for two to four weeks. You should expect full recovery to take up to three months.
Many surgeons have their patients take part in formal physical therapy after meniscal repair and transplant procedures. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. Physical therapists will also work with patients to make sure they are putting only a safe amount of weight on the affected leg.
For the first six weeks after a meniscal repair, you should avoid bending the knee more than 90 degrees. Then it is safe to gradually bend the knee fully. However, you should avoid squatting for at least three to four months while the repair fully heals. It is not advisable to run, jump, or twist the knee for at least four to six months. Patients sometimes resume sport activities within four to six months after surgery to repair the meniscus.
Range-of-motion exercises start right away after a transplant. The goal is to get the knee to bend to 90 degrees within four weeks after surgery. As time goes on, more challenging exercises are chosen to safely advance the knee’s range of motion, strength, and function.
Ideally, patients will be able to resume their previous activities. Some patients may be encouraged to modify their activity choices, especially if an allograft was used.
The physical therapist’s goal is to help you keep your pain under control and improve your knee’s range of motion and strength. When you are well under way, regular visits to your therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Patellar Tendon Graft Reconstruction of the ACL
A Patient’s Guide to Patellar Tendon Graft Reconstruction of the ACL
Introduction
The anterior cruciate ligament (ACL) is a major stabilizer of the knee joint. This key knee ligament is commonly torn during sports activities. The standard operation to fix a torn ACL is with a patellar tendon graft. The surgeon takes out the middle section of the patellar tendon below the kneecap (patella). This new graft includes the strip of tendon, along with attached plugs of bone on each end. For this reason, it is sometimes referred to as a bone-patellar-tendon-bone graft. The surgeon removes the torn ACL and puts the new graft into the knee, making sure to line it up just like the original ligament.
Many types of tissue grafts have been tried. The patellar tendon graft has proven to be one of the strongest for ACL reconstruction. Patients who have this operation generally get back to their usual activities and sports. They often do so faster than people who have their ACL reconstructed with other types of tissue grafts.
This guide will help you understand
- what parts of the knee are treated during surgery
- how surgeons perform the operation
- what to expect before and after the procedure
Anatomy
What parts of the knee are involved?
Ligaments are tough bands of tissue that connect the ends of bones together. The ACL is located in the center of the knee joint where it runs from the backside of the femur (thighbone) to the front of the tibia (shinbone).
The ACL runs through a special notch in the femur called the intercondylar notch and attaches to a special area of the tibia called the tibial spine.
The patellar tendon is a thick and strong band of connective tissue on the front of the knee. It starts at the bottom of the patella and fastens just below the knee to a bony bump on the front of the tibia, called the tibial tubercle. When using the patellar tendon as an ACL graft, surgeons remove a strip from the middle of it. The graft includes the bony attachments from
the bottom of the patella and from the tibial tubercle.
Related Document: A Patient’s Guide to Knee Anatomy
Related Document: A Patient’s Guide to Anterior Cruciate Ligament Injuries
Rationale
What does the surgeon hope to accomplish?
The main goal of ACL surgery is to keep the tibia from moving too far forward under the femur bone and to get the knee functioning normally again.
Many surgeons prefer to use the patellar tendon when reconstructing the ACL. The graft is often chosen because it is one of the strongest ACL grafts. It’s easy to get to, holds well in its location, and generally heals fast.
The anatomy of the graft helps to speed healing and to create a solid connection. When the surgeon implants the new graft, the bony plugs on each end of the graft fit inside a tunnel of bone. This means there is bone-to-bone contact. The body treats the contact of these two bony surfaces as it would a broken bone. It responds by healing the two surfaces together. Healing at the bone-to-bone surface fixes the patellar tendon graft in place.
Preparation
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. Your therapist will check your current pain levels, your ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. Your therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted to the surgery center early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Most surgeons perform this surgery using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during arthroscopy for this procedure. The operation doesn’t require the surgeon to open the knee joint.
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia. The surgeon begins the operation by making two small openings into the knee, called portals. These portals are where the arthroscope and surgical tools are placed into the knee.
Care is taken to protect the nearby nerves and blood vessels.
A small incision is also made below the patella. Working through this incision, the surgeon takes out the middle section of the patellar tendon, along with the bone attachments on each end. The bone plugs are rounded and smoothed. Holes are drilled in each bone plug to place sutures (strong stitches) that will pull the graft into place.
Next, the surgeon prepares the knee to place the graft. The remnants of the original ligament are removed. The intercondylar notch (mentioned earlier) is enlarged so that nothing will rub on the graft. This part of the surgery is referred to as a notchplasty.
Once this is done, holes are drilled in the tibia and the femur to place the graft. These holes are placed so that the graft will run between the tibia and femur in the same direction as the original ACL.
The graft is then pulled into position using sutures placed through the drill holes. Screws are used to hold the bone plugs in the drill holes.
To keep fluid from building up in your knee, the surgeon may place a tube in your knee joint. The portals and skin incision are then stitched together, completing the surgery.
Complications
What problems can happen with this surgery?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following patellar tendon graft reconstruction of the ACL are
- anesthesia complications
- thrombophlebitis
- infection
- problems with the graft
- problems at the donor site
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the surgical incision can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
Problems with the Graft
After surgery, the body attempts to develop a network of blood vessels in the new graft. This process, called revascularization, takes about 12 weeks. The graft is weakest during this time, which means it has a greater chance of stretching or rupturing. A stretched or torn graft can occur if you push yourself too hard during this period of recovery. When revascularization is complete, strength in the graft gradually builds. A second surgery may be needed to replace the graft if it is stretched or torn.
Problems at the Donor Site
Problems can occur at the donor site (the area below the patella where the graft was taken from the knee). A major drawback of taking out a piece of the patellar tendon to reconstruct the ACL is that most patients end up having difficulty kneeling down long after surgery. Lingering pain in the front of the knee is also common.
A portion of bone is taken from the bottom of the patella during the graft procedure. This can weaken the patella. In rare cases, heavy use of the quadriceps muscle (on the front of the thigh) can cause the patella to fracture. This often requires a second surgery to repair the broken patella.
Taking tissue from the center of the patellar tendon can also cause problems. The body attempts to heal the area but sometimes produces too much scar tissue. The extra scar tissue that forms around the donor site may prevent normal motion in the knee. The patellar tendon is not as strong as it was before surgery. In rare cases, this has been linked to a tear in the patellar tendon. Also, the patellar tendon may become easily inflamed. And problems in this area can keep the quadriceps from regaining normal control and strength.
After Surgery
What should I expect after surgery?
You may use a continuous passive motion (CPM) machine immediately afterward to help the knee begin moving and to alleviate joint stiffness. The machine straps to the leg and continuously bends and straightens the joint. This continuous motion is thought to reduce stiffness, ease pain, and keep extra scar tissue from forming inside the joint. The CPM is often used with a form of cold treatment that circulates cold water through hoses and pads around your knee.
Most ACL surgeries are now done on an outpatient basis. Many patients go home the same day as the surgery. Some patients stay one to two nights in the hospital if necessary. The tube placed in your knee at the end of the surgery is usually removed after 24 hours.
Your surgeon may also have you wear a protective knee brace for a few weeks after surgery. You’ll use crutches for two to four weeks in order to keep your knee safe, but you’ll probably be allowed to put a comfortable amount of weight down while you’re up and walking.
Rehabilitation
What will my recovery be like?
Patients usually take part in formal physical therapy after ACL reconstruction. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The goal is to help you regain full knee extension as soon as possible.
The physical therapist will choose treatments to get the quadriceps muscles toned and active again. Muscle stimulation and biofeedback, which involve placing electrodes over the quadriceps muscle, may be needed at first to get the muscle going again and to help retrain it.
As the rehabilitation program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. Specialized balance exercises are used to help the muscles respond quickly and without thinking. This part of treatment is called neuromuscular training. If you need to stop suddenly, your muscles must react with just the right amount of speed, control, and direction. After ACL surgery, this ability doesn’t come back completely without exercise.
Neuromuscular training includes exercises to improve balance, joint control, muscle strength and power, and agility. Agility makes it possible to change directions quickly, go faster or slower, and improve starting and stopping. These are important skills for walking, running, and jumping, and especially for sports performance.
When you get full knee movement, your knee isn’t swelling, and your strength and muscle control are improving, you’ll be able to gradually go back to your work and sport activities. Some surgeons prescribe a functional brace for athletes who intend to return quickly to their sports.
Ideally, you’ll be able to resume your previous lifestyle activities. However, athletes are usually advised to wait at least six months before returning to their sports. Most patients are encouraged to modify their activity choices.
You will probably be involved in a progressive rehabilitation program for four to six months after surgery to ensure the best result from your ACL reconstruction. In the first six weeks following surgery, expect to see the physical therapist two to three times a week. If your surgery and rehabilitation go as planned, you may only need to do a home program and see your therapist every few weeks over the four to six month period.
Patellofemoral Problems
A Patient’s Guide to Patellofemoral Problems
Introduction
The patella, or kneecap, can be a source of knee pain when it fails to function properly. Alignment or overuse problems of the patella can lead to wear and tear of the cartilage behind the patella. This produces pain, weakness, and swelling of the knee joint. Several different problems can affect the patella and the groove it slides through in the knee joint. These problems can affect people of all ages.
This guide will help you understand
- how the kneecap works
- why kneecap problems develop
- what can be done to treat these problems
Anatomy
What is the patella, and what does it do?
The patella (kneecap) is the moveable bone on the front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone. The large quadriceps tendon together with the patella is called the quadriceps mechanism. Though we think of it as a single device, the quadriceps mechanism has two separate tendons, the quadriceps tendon on top of the patella and the patellar tendon below the patella.
Tightening up the quadriceps muscles places a pull on the tendons of the quadriceps mechanism. This action causes the knee to straighten. The patella acts like a fulcrum to increase the force of the quadriceps muscles.
The underside of the patella is covered with articular cartilage, the smooth, slippery covering found on joint surfaces. This covering helps the patella glide (or track) in a special groove made by the thighbone, or femur. This groove is called the femoral groove.
Two muscles of the thigh attach to the patella and help control its position in the femoral groove as the leg straightens. These muscles are the vastus medialis obliquus (VMO) and the vastus lateralis (VL). The VMO runs along the inside of the thigh, and the VL lies along the outside of the thigh. If the timing between these two muscles is off, the patella may be pulled off track.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
How do these problems develop?
Problems commonly develop when the patella suffers wear and tear. The underlying cartilage begins to degenerate, a condition sometimes referred to as chondromalacia patella. Wear and tear can develop for several reasons. Degeneration may develop as part of the aging process, like putting a lot of miles on a car. The patellofemoral joint is usually affected as part of osteoarthritis of the knee.
Related Document: A Patient’s Guide to Osteoarthritis of the Knee
One of the more common causes of knee pain is a problem in the way the
patella tracks within the femoral groove as the knee moves. The quadriceps muscle helps control the patella so it stays within this groove. If part of the quadriceps is weak for any reason, a muscle imbalance can occur. When this happens, the pull of the quadriceps muscle may cause the patella to pull more to one side than the other. This in turn causes more pressure on the articular cartilage on one side than the other. In time, this pressure can damage the articular cartilage.
Weakness of the muscles around the hip can also indirectly affect the patella and can lead to patellofemoral joint pain. Weakness of the muscles that pull the hip out and away from the other leg, the hip abductor muscles, can lead to imbalances to the alignment of the entire leg – including the knee joint and the muscle balance of the muscles around the knee. This causes abnormal tracking of the patella within the femoral groove and eventually pain around the patella. Many patients are confused when their physical therapist begins exercises to strengthen and balance the hip muscles, but there is a very good reason that the therapist is focusing on this area.
A similar problem can happen when the timing of the quadriceps muscles is off. There are four muscles that form the quadriceps muscle group. As mentioned earlier, the VMO is one of these four muscles. The VMO is the section of muscle on the inside of the front of the thigh. The VL runs down the outside part of the thigh. People with patellofemoral problems sometimes have problems in the timing between the VMO and the VL. The VL contracts first, before the VMO. This tends to pull the patella toward the outside of edge of the knee. The result is abnormal pressure on the articular surface of the patella.
Another type of imbalance may exist due to differences in how the bones of the knee are shaped. These differences, or anatomic variations, are something people are born with. Some people are born with a greater than normal angle where the femur and the tibia (shinbone) come together at the knee joint. Women tend to have a greater angle here than men. The patella normally sits at the center of this angle within the femoral groove. When the quadriceps muscle contracts, the angle in the knee straightens, pushing the patella to the outside of the knee. In cases where this angle is increased, the patella tends to shift outward with greater pressure. This leads to a similar problem as that described above. As the patella slides through the groove, it shifts to the outside. This places more pressure on one side than the other, leading to damage to the underlying articular cartilage.
Finally, anatomic variations in the bones of the knee can occur such that one side of the femoral groove is smaller than normal. This creates a situation where the groove is too shallow, usually on the outside part of the knee. People who have a shallow groove sometimes have their patella slip sideways out of the groove, causing a patellar dislocation. This is not only painful when it occurs, but it can damage the articular cartilage underneath the patella. If this occurs repeatedly, degeneration of the patellofemoral joint occurs fairly rapidly.
People who have a high-riding patella are also at risk of having their patella dislocate. In this condition, called patella alta, the patella sits high on the femur where the groove is very shallow. Here the sides of the femoral groove provide only a small barrier to keep the high-riding patella in place. A strong contraction of the quadriceps muscle can easily pull the patella over the edge and out of the groove, leading to a patellar dislocation. Patella alta is most common in girls, especially those who have generalized laxity (looseness) in their joints.
Symptoms
What do patellar problems feel like?
When people have patellofemoral problems, they sometimes report a sensation like the patella is slipping. This is thought to be a reflex response to pain and not because there is any instability in the knee.
Others report having pain around the front part of the knee or along the edges of the kneecap. These symptoms may be due to problems with the way the patella lines up in the femoral groove. But symptoms of patellar pain can happen even when the patella appears to be lined up properly.
Patellofemoral problems exist when there is damage to the articular cartilage underneath the patella. This does not necessarily mean that the knee will be painful. Some people never have problems. Others experience vague pain in the knee that isn’t centered in any one spot. Sometimes pain is felt along the inside edge of the patella, though it may be felt anywhere around or behind the patella. Typically, people who have patellofemoral problems experience pain when walking down stairs or hills. Keeping the knee bent for long periods, as in sitting in a car or movie theater, may cause pain.
The knee may grind, or you may hear a crunching sound when you squat or go up and down stairs. If there is a considerable amount of wear and tear, you may feel popping or clicking as you bend your knee. This can happen when the uneven surface of the underside of the patella rubs against the femoral groove. The knee may swell with heavy use and become stiff and tight. This is usually because of fluid accumulating inside the knee joint, sometimes called water on the knee. This is not unique to problems of the patella but sometimes occurs when the knee becomes inflamed.
Diagnosis
How do doctors identify these problems?
Diagnosis begins with a complete history of your knee problem followed by an examination of the knee, including the patella. X-rays may be ordered on the initial visit to your doctor. An X-ray can help determine if the patella is properly aligned in the femoral groove. Several X-rays taken with the knee bent at several different angles can help determine if the patella seems to be moving through the femoral groove in the correct alignment. The X-ray may show arthritis between the patella and thighbone, especially when the problems have been there for awhile. This is often refered to as chondromalacia patella.
Related Document: A Patient’s Guide to Chondromalacia Patella
Diagnosing problems with the patella can be confusing. The symptoms can
be easily confused with other knee problems, because the symptoms are often similar. In these cases, other tests, such as magnetic resonance imaging (MRI), may be suggested. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the knee. Usually, this test is done to look for injuries, such as tears in the menisci or ligaments of the knee. Recent advances in the quality of MRI scans have enabled doctors to see the articular cartilage on the scan and determine if it is damaged. This test does not require any needles or special dye and is painless.
In some cases, arthroscopy may be used to make the definitive diagnosis when there is still a question about what is causing your knee problem. Arthroscopy is an operation that involves placing a small fiber-optic TV camera into the knee joint, allowing the surgeon to look at the structures inside the joint directly. The arthroscope allows your doctor to see the condition of the articular cartilage on the back of your patella. The vast majority of patellofemoral problems are diagnosed without resorting to surgery, and arthroscopy is usually reserved to treat the problems identified by other means.
Treatment
What treatment options are available?
Nonsurgical Treatment
The initial treatment for a patellar problem begins by decreasing the inflammation in the knee. Your physician may suggest rest and anti-inflammatory medications, such as aspirin or ibuprofen, especially when the problem is coming from overuse. Physical therapy can help in the early stages by decreasing pain and inflammation. Your physical therapist may use ice massage and ultrasound to limit pain and swelling.
Bracing or taping the patella can help you do exercises and activities with less pain. Most braces for patellofemoral problems are made of soft fabric, such as cloth or neoprene. You slide them onto your knee like a sleeve. A small buttress pads the side of the patella to keep it lined up within the groove of the femur. An alternative to bracing is to tape the patella in place. The therapist applies and adjusts the tape over the knee to help realign the patella. The idea is that by bracing or taping the knee, the patella stays in better alignment within the femoral groove. This in turn is thought to improve the pull of the quadriceps muscle so that the patella stays lined up in the groove. Patients report less pain and improved function with these forms of treatment.
As the pain and inflammation become controlled, your physical therapist will work with you to improve flexibility, strength, and muscle balance in the knee.
Surgery
If nonsurgical treatment fails to improve your condition, surgery may be suggested. The procedure used for patellofemoral problems varies. In severe cases a combination of one or more
of the following procedures may be necessary.
Arthroscopic Method
Arthroscopy is sometimes useful in the treatment of patellofemoral problems of the knee. Looking directly at the articular cartilage surfaces of the patella and the femoral groove is the most accurate way of determining how much wear and tear there is in these areas. Your surgeon can also watch as the patella moves through the groove, and may be able to decide whether or not the patella is moving normally. If there are areas of articular cartilage damage behind the patella that are creating a rough surface, special tools can be used by the surgeon to smooth the surface and reduce your pain. This procedure is sometimes referred to as shaving the patella.
Related Document: A Patient’s Guide to Patellar Tendonitis
Cartilage Procedure
In more advanced cases of patellar arthritis, surgeons may operate to repair or restore the damaged cartilage. The type of surgery needed for articular cartilage is based on the size, type, and location of the damage. Along with surgical treatment to fix the cartilage, other procedures may also be done to help align the patella so less pressure is placed on the healing cartilage.
Related Document: A Patient’s Guide to Articular Cartilage Problems of the Knee
Lateral Release
If your patella problems appear to be caused by a misalignment problem, a procedure called a lateral release may be suggested. This procedure is done to allow the patella to shift back to a more normal position and relieve pressure on the articular cartilage. In this operation, the tight ligaments on the outside (lateral side) of the patella are cut, or released, to allow the patella to slide more towards the center of the femoral groove. These ligaments eventually heal with scar tissue that fills in the gap created by the surgery, but they no longer pull the patella to the outside as strongly as before the surgery. This helps to balance the quadriceps mechanism and equalize the pressure on the articular cartilage behind the patella.
Ligament Tightening Procedure
In some cases of severe patellar misalignment, a lateral release alone may not be enough. For problems of repeated patellar dislocations, the surgeon may also need to realign the quadriceps mechanism. In addition to the lateral release, the tendons on the inside edge of the knee (the medial side) may have to be tightened as well.
Bony Realignment
If the misalignment is severe, the bony attachment of the patellar tendon
may also have to be shifted to a new spot on the tibia bone. Remember that the patellar tendon attaches the patella to the lower leg bone (tibia) just below the knee. By moving a section of bone where the patellar tendon attaches to the tibia, surgeons can change the way the tendon pulls the patella through the femoral groove. This is done surgically by removing a section of bone where the patellar tendon attaches on the tibia. This section of bone is then reattached on the tibia closer to the other knee.
Usually, the bone is reattached onto the tibia using screws. This procedure shifts the patella to the medial side. Once the surgery heals, the patella should track better within the center of the groove, spreading the pressure equally on the articular cartilage behind the patella.
View animation of the bony realignment procedure
Arthroscopic procedures to shave the patella or a simple lateral release can usually be done on an outpatient basis, meaning you can leave the hospital the same day. If your problem requires the more involved surgical procedure where bone must be cut to allow moving the patellar tendon attachment, you may need to spend one or two nights in the hospital.
Rehabilitation
What should I expect from treatment?
Nonsurgical Rehabilitation
Patients with patellofemoral problems may benefit from four to six weeks of physical therapy. The aim of treatment is to calm pain and inflammation, to correct muscle imbalances, and to improve function of the patella.
Treatments such as ultrasound, electrical stimulation, and ice may be used to help control pain and swelling.
Muscle imbalances are commonly treated with stretching and strengthening exercises. Flexibility exercises are often designed for the thigh and calf muscles. Guided exercises are used to maximize control and strength of the quadriceps muscles.
Your therapist may issue a knee brace or instruct you how to apply tape to your knee. Therapists also design special shoe inserts, called orthotics, to improve knee alignment and function of the patella.
After Surgery
Many surgeons will have their patients take part in formal physical therapy after knee surgery for patellofemoral problems. Patients undergoing a patellar shaving usually begin rehabilitation right away. More involved surgeries for patellar realignment or restorative procedures for the articular cartilage require a delay before going to therapy. And rehabilitation may be slower to allow the bone or cartilage to heal before too much strain can be put on the knee.
The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. The physical therapist will choose exercises to help improve knee motion and to get the quadriceps muscles toned and active again. Muscle stimulation, using electrodes over the quadriceps muscle, may be needed at first to get the muscle moving again.
As the program evolves, more challenging exercises are chosen to safely advance the knee’s strength and function. The key is to get the soft tissues in balance through safe stretching and gradual strengthening.
The physical therapist’s goal is to help you keep your pain under control, ensure you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When you are well under way, regular visits to the therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Popliteal Cysts
A Patient’s Guide to Popliteal Cysts
Introduction
A popliteal cyst, also called a Baker’s cyst, is a soft, often painless bump that develops on the back of the knee. A cyst is usually nothing more than a bag of fluid. These cysts occur most often when the knee is damaged due to arthritis, gout, injury, or inflammation in the lining of the knee joint. Surgical treatment may be successful when the actual cause of the cyst is addressed. Otherwise, the cyst can come back again.
This guide will help you understand
- how a popliteal cyst develops
- why a cyst can cause problems
- what can be done for the condition
Anatomy
What is a popliteal cyst?
The knee joint is formed where the thighbone (femur) meets the shinbone (tibia). A slick cushion of articular cartilage covers the surface ends of both of these bones so that they slide against one another smoothly. The articular cartilage is kept slippery by joint fluid made by the joint lining (the synovial membrane). The fluid is contained in a soft tissue enclosure around the knee joint called the joint capsule.
A popliteal cyst is a small, bag-like structure that forms when the joint lining produces too much fluid in the knee. The extra fluid builds up and pushes through the back part of the joint capsule, forming a cyst. The cyst squeezes out toward the back part of the knee in the area called the popliteal fossa, the indentation felt in the back part of the knee between the two hamstring tendons and the top part of the calf muscle. Most people will be able to feel the cyst in the hollow area right behind the knee joint.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
Why does a popliteal cyst develop?
A popliteal cyst may form after damage to the joint capsule of the knee. The weakening of the joint capsule in the damaged area can cause the small sac of fluid to form. This can lead to a bulging of the joint capsule, much like what occurs when an inner tube bulges through a weak spot in a tire. The cyst may become larger over time.
A popliteal cyst can actually be a response to other conditions that cause swelling in the knee joint. This swelling is most often from problems of osteoarthritis or rheumatoid arthritis in the knee joint. It can also be caused by trauma, either from a direct blow to the knee or from repetitive activities that lead to overuse in the knee joint. A popliteal cyst is not from a blood clot in the leg, although sometimes it can be mistaken for a blood clot.
Symptoms
What does a popliteal cyst feel like?
The symptoms caused by a popliteal cyst are usually mild. You may have aching or tenderness with exercise or your knee may feel unsteady, as though it’s going to give out. You may feel pain from the underlying cause of the cyst, such as arthritis, an injury, or a mechanical problem with the knee, for instance a tear in the meniscus. Along with these symptoms, you may also see or feel a bulge on the back of your knee. Anything that causes the knee to swell and more fluid to fill the joint can make the cyst larger. It is common for a popliteal cyst to swell and shrink over time.
Sometimes a cyst will suddenly burst underneath the skin, causing pain and swelling in the calf. A ruptured popliteal cyst gives symptoms just like those of a blood clot in the leg, called thrombophlebitis. For this reason, it is important to determine right away the cause of the pain and swelling in the calf. Once the cyst ruptures, the fluid inside the cyst simply leaks into the calf and is absorbed by the body. In this case, you will no longer be able to see or feel the cyst. However, the cyst will probably return in a short time.
Diagnosis
How do doctors identify a popliteal cyst?
Your doctor will ask you to describe the history of your problem. Then the doctor will examine your knee and leg. A physical exam is usually all that is needed to diagnose a popliteal cyst. Unless the cyst has ruptured, further testing is typically not needed.
If the cyst has ruptured, additional tests will be required. Regular X-rays will not show the cyst since it is a soft tissue, and X-rays show mostly bones. A cyst can be seen with a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to create pictures that look like slices of the area your doctor is interested in. This test requires no needles or special dye and is painless. Your doctor may order an ultrasound test. This test uses sound waves to allow the doctor to see the outline of the cyst and determine whether it is filled with fluid or solid tissue. This is useful in determining whether the lump could actually be a tumor instead of a fluid-filled cyst.
Treatment
What can be done for the condition?
There are two types of treatment for popliteal cysts: surgical and nonsurgical. Whether or not the cyst has ruptured, how painful the cyst has become, or how much it interferes with the normal use of your knee will determine which is the best course of treatment for you. In adults the treatment is most often nonsurgical. If surgery is needed, it is usually done on an outpatient basis, meaning you can leave the hospital the same day. Unless there is a lot of discomfort from the cyst, surgery is rarely required.
Nonsurgical Treatment
Drawing the fluid out with a needle and syringe can reduce the size of the cyst. Then cortisone can be injected into the affected area to reduce inflammation. These are usually temporary solutions, however. Nonsurgical treatment also includes rest and keeping your leg propped up for several days.
In some cases doctors have their patients work with a physical therapist who uses massage treatments, compression wraps, and electrical stimulation to reduce knee swelling. Flexibility and strengthening exercises for the lower limb may be used to help improve muscle balance in the knee.
Nonsurgical treatments are usually most effective when the underlying cause of the cyst is addressed. In other words, the effects of arthritis, gout, or injury to the knee need to be controlled.
If nonsurgical methods fail, complete removal of the cyst may be needed. Once they are reassured that the cyst is not dangerous, many people simply ignore the problem unless it becomes very painful.
Surgery
The goal of surgery is to remove the cyst and repair the hole in the joint
lining where the cyst pushed through. Unfortunately, about half of the time the cyst comes back, or recurs, after being removed. Surgeons are cautious when suggesting surgery to remove a popliteal cyst because they are prone to recur. The cure is often permanent, but preventing further cysts depends a great deal on the success of treating the underlying cause. You should be aware that there is a very real chance that your cyst may return after being removed and there is no guarantee that the surgery will be successful.
Surgery can take more than an hour to complete. It is performed either under a general anesthetic, which causes you to sleep during the surgery, or using spinal anesthesia, which numbs the lower half of your body only. With spinal anesthesia, you may be awake during the surgery, but you won’t be able to watch what’s happening.
An incision will be made in the skin over the cyst. The cyst is then located and separated from the surrounding tissues. The area of the joint capsule where the cyst appears to be coming from is identified. A synthetic patch may be sewn in place to cover the hole in the joint capsule left by the removal of the cyst.
Your knee will be bandaged with a well-padded dressing and a splint for support. Your surgeon will want to check your knee within five to seven days. Stitches will be removed after 10 to 14 days. You may have some discomfort after surgery, and you will be given pain medicine to control the discomfort.
A popliteal cyst forms very near the major nerve and blood vessels of the leg. It is possible that these structures can be injured during surgery. If an injury happens, it can be a serious complication. Injury to the nerves can cause numbness or weakness in the foot and lower leg. Injury to the blood vessels may require surgery to repair them. In addition, it is uncommon but possible that another cyst can occur.
Rehabilitation
What should I expect with treatment?
Nonsurgical Rehabilitation
With nonsurgical rehabilitation, a popliteal cyst may improve in two to four weeks. Improvement, however, depends a great deal on improvement in the underlying condition (the problems that are causing the knee to swell). As long as the joint continues to swell, the size of the cyst will ebb and flow. If the knee is kept from swelling, the cyst won’t swell.
Your doctor may have you work with a physical therapist. Treatments such as ultrasound, electrical stimulation, and soft-tissue massage may be used to ease pain and swelling from the cyst.
Therapy sessions sometimes include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine to the sore area. This treatment is especially helpful for patients who can’t tolerate injections.
After Surgery
If you have surgery to remove the cyst, you can resume your daily activities and work as soon as you are able. You should keep your knee propped up for several days to avoid swelling and throbbing. Take all medicines exactly as prescribed by your surgeon. Be sure to keep all follow-up appointments.
Your surgeon may want you to use crutches or a cane for awhile. Avoid vigorous exercise for six weeks after surgery. You should be able to resume driving two weeks after surgery. Your surgeon may have you attend physical therapy sessions to regain the strength in your leg.
Prepatellar Bursitis
A Patient’s Guide to Prepatellar Bursitis
Introduction
Prepatellar bursitis is the inflammation of a small sac of fluid located in front of the kneecap. This inflammation can cause many problems in the knee.
This guide will help you understand
- how prepatellar bursitis develops
- why the condition causes problems
- what can be done for your pain
Anatomy
Where is the prepatellar bursa, and what does it do?
A bursa is a sac made of thin, slippery tissue. Bursae occur in the body wherever skin, muscles, or tendons need to slide over bone. Bursae are lubricated with a small amount of fluid inside that helps reduce friction from the sliding parts.
The prepatellar bursa is located between the front of the kneecap (called the patella) and the overlying skin. This bursa allows the kneecap to slide freely underneath the skin as we bend and straighten our knees.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
How does prepatellar bursitis develop?
Bursitis is the inflammation of a bursa. The prepatellar bursa can become irritated and inflamed in a number of ways.
In some cases, a direct blow or a fall onto the knee can damage the bursa. This usually causes bleeding into the bursa sac, because the blood vessels in the tissues that make up the bursa are damaged and torn. In the skin, this would simply form a bruise, but in a bursa blood may actually fill the bursa sac. This causes the bursa to swell up like a rubber balloon filled with water.
The blood in the bursa is thought to cause an inflammatory reaction. The walls of the bursa may thicken and remain thickened and tender even after the blood has been absorbed by the body. This thickening and swelling of the bursa is referred to as prepatellar bursitis.
Prepatellar bursitis can also occur over a longer period of time. People who work on their knees, such as carpet layers and plumbers, can repeatedly injure the bursa. This repeated injury can lead to irritation and thickening of the bursa over time. The chronic irritation leads to prepatellar bursitis in the end.
The prepatellar bursa can also become infected. This may occur without any warning, or it may be caused by a small injury and infection of the skin over the bursa that spreads down into the bursa. In this case, instead of blood or inflammatory fluid in the bursa, pus fills it. The area around the bursa becomes hot, red, and very tender.
Symptoms
What does prepatellar bursitis feel like?
Prepatellar bursitis causes pain and swelling in the area in front of the kneecap and just below. It may be very difficult to kneel down and put the knee on the floor due to the tenderness and swelling. If the condition has been present for some time, small lumps may be felt underneath the skin over the kneecap. Sometimes these lumps feel as though something is floating around in front of the kneecap, and they can be very tender. These lumps are usually the thickened folds of bursa tissue that have formed in response to chronic inflammation.
The bursa sac may swell and fill with fluid at times. This is usually related to your activity level, and more activity usually causes more swelling. In people who rest on their knees a lot, such as carpet layers, the bursa can grow very thick, almost like a kneepad in front of the knee.
Finally, if the bursa becomes infected, the front of the knee becomes swollen and very tender and warm to the touch around the bursa. You may run a fever and feel chills. An abscess, or area of pus, may form on the front of the knee. If the infection is not treated quickly, the abscess may even begin to drain, meaning the pus begins to seep out.
Diagnosis
How do doctors identify the condition?
The diagnosis of prepatellar bursitis is usually obvious from the physical examination. In cases where the knee swells immediately after a fall or other injury to the kneecap, X-rays may be necessary to make sure that the kneecap isn’t fractured. Chronic bursitis is usually easy to diagnose without any special tests.
If your doctor is uncertain whether or not the bursa is infected, a needle may be inserted into the bursa and the fluid removed. This fluid will be sent to a lab for tests to determine whether infection is present, and if so, what type of bacteria is causing the infection and what antibiotic will work best to cure the infection.
Treatment
What can be done for prepatellar bursitis?
Nonsurgical Treatment
Prepatellar bursitis that is caused by an injury will usually go away on its own. The body will absorb the blood in the bursa over several weeks, and the bursa should return to normal. If swelling in the bursa is causing a slow recovery, a needle may be inserted to drain the blood and speed up the process. There is a slight risk of infection in putting a needle into the bursa.
View animation of draining the prepatellar bursa
Chronic prepatellar bursitis is sometimes a real nuisance. The swelling and tenderness gets in the way of kneeling and causes pain. For people who need to kneel, this creates a hardship both in their occupation and recreational activities. Treatment usually starts by trying to control the inflammation. This may include a short period of rest or possibly a brace to immobilize the knee. Medications such as ibuprofen and aspirin may be suggested by your doctor to control the inflammation and swelling. A knee pad may be useful in making it easier to kneel on the affected knee.
If the bursa remains filled with fluid, a needle may be inserted and the fluid drained. During the drainage procedure, if there is no evidence of infection, a small amount of cortisone may be injected into the bursa to control the inflammation. Again, there is a small risk of infection if the bursa is drained with a needle.
Your doctor may also prescribe professional rehabilitation where the problems that are causing your symptoms will be evaluated and treated. Your physical therapist may suggest the use of heat, ice, and ultrasound to help calm pain and swelling. The therapist may also suggest specialized stretching and strengthening exercises used in combination with a knee brace, taping of the patella, or shoe inserts. These exercises and aids are used to improve muscle balance and joint alignment of the hip and lower limb, easing pressure and problems in the bursa.
If an infection is found to be causing the prepatellar bursitis, the bursa will need to be drained with a needle, perhaps several times over the first few days. You will be placed on antibiotics for several days. If the infection is slow to heal, the bursa may have to be drained surgically. To drain the bursa surgically, a small incision is made in the skin, and the bursa is opened. The skin and bursa are kept open by inserting a drain tube into the bursa for several days. This allows the pus to drain and helps the antibiotics clear up the infection.
Surgery
Surgery is sometimes necessary to remove a thickened bursa that has not improved with any other treatment. Surgical removal is usually done because the swollen bursa is restricting your activity.
To remove the prepatellar bursa, an incision is made over the top of the knee (either straight up and down or across the knee). Since the bursa is in front of the patella, the knee joint is never entered. The thickened bursa sac is removed, and the skin is repaired with stitches. You may need to stay off your feet for several days to allow the wound to begin to heal and to prevent bleeding into the area where the bursa was removed.
Some types of bursae will probably grow back after surgery, because the skin needs to slide over the kneecap smoothly. The body will form another bursa as a response to the movement of the patella against the skin during the healing phase. If all goes well, the bursa that returns after surgery will not be thick and painful, but more like a normal bursa.
Rehabilitation
What should I expect with treatment?
Nonsurgical Rehabilitation
Chronic prepatellar bursitis will usually improve over a period of time from weeks to months. The fluid-filled sac is not necessarily a problem, and if it does not cause pain, it is not always a cause for alarm or treatment. The sac of fluid may come and go with variation in activity. This is normal.
Patients with prepatellar bursitis may benefit from two to four weeks of physical therapy. Treatments such as ultrasound, electrical stimulation, and ice may be used to help control pain and swelling.
Therapy sessions sometimes include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine to the sore area. This treatment is especially helpful for patients who can’t tolerate injections.
After Surgery
If surgery is required, you and your surgeon will come up with a plan for your rehabilitation. You will have a period of rest, which may involve using crutches. You will also need to start a careful and gradual exercise program. Patients often work with a physical therapist to direct the exercises for their rehabilitation program.
Revision Arthroplasty of the Knee
A Patient’s Guide to Revision Arthroplasty of the Knee
Introduction
Over the past 30 years, artificial knee replacement surgery has become increasingly common. Millions of people have gotten a new knee joint. The first time a joint is replaced with an artificial joint the operation is called a primary joint replacement. As people live longer and more people receive artificial joints, some of those joints begin to wear out and fail. When an artificial knee joint fails, a second operation is required to replace the failing joint. This procedure is called a revision arthroplasty.
This guide will help you understand
- why revision surgery becomes necessary
- what happens during the operation
- what to expect during your recovery
Anatomy
What part of the knee is affected?
The knee joint is formed where the thighbone (femur) meets the shinbone (tibia). A slick cushion of articular cartilage covers the ends of both of these bones so that they slide against one another smoothly. The articular cartilage is kept slippery by joint fluid made by the joint lining (synovial membrane). The fluid is contained in a soft tissue enclosure around the knee joint called the joint capsule.
The kneecap (patella) is the moveable bone on the front of the knee. It is wrapped inside a tendon that connects the large muscles on the front of the thigh (the quadriceps muscles) to the tibia. The back of the patella is covered
with articular cartilage. The patella glides within a groove on the front of the femur.
Related Document: A Patient’s Guide to Knee Anatomy
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Knee
Rationale
Why does a knee revision become necessary?
The most common reasons for knee revision arthroplasty are
- mechanical loosening
- infection in the joint
- fracture of the bone around the joint
- instability of the implant
- wear of one or more parts of the implant
- breakage of the implant
Mechanical Loosening
Mechanical loosening means that for some reason (other than infection) the attachment between the artificial joint and the bone has become loose. There are many reasons why this can occur. It may be that, given enough time, all artificial joints will eventually loosen. This is one reason that surgeons like to wait until absolutely necessary to put in an artificial joint. The younger you are when an artificial joint is put in, the more likely it is that the joint will loosen and require a revision. Mechanical loosening can occur in both cemented and uncemented artificial joints. (The different types of joints are described later.)
Infection
If an artificial joint is infected, it may become stiff and painful. It may also begin to lose its attachment to the bone. An infected artificial joint will probably have to be revised to try to cure the infection.
In the knee joint, operations to exchange the original implant (prosthesis) with a new one have a good chance of success. The decision to do a revision surgery depends in part on the type of bacteria that has infected the joint. In some uncommon cases, the type of bacteria is so harmful that a revision is not possible. In these unfortunate cases, the surgeon may suggest placing a cement spacer filled with antibiotics in the knee and having the patient wear a knee brace for support. In rare cases, the knee may need to be fused together, or possibly even amputated. In less aggressive infections, the infected artificial joint is removed at one operation. Antibiotics are given for up to three months until the infection is gone. Then a second operation is done to insert a new artificial knee.
Fracture
A fracture may occur near an artificial joint. It is sometimes necessary to
use a new artificial joint to fix the fracture. For example, if the femur (thighbone) breaks where the prosthesis attaches, it may be easier to replace the femoral part of the artificial joint with a new piece that has a longer stem that can hold the fracture together while it heals. This is similar to fixing the fracture with a metal rod.
Instability
Instability means that the artificial joint dislocates. This is very painful when it happens. It is unlikely that the knee joint will completely dislocate. However, it can happen. It is more common for the knee joint to be either too tight or too loose. If the knee joint is too loose, it can cause unsteadiness and pain. If the joint is too tight, the knee is usually painful and doesn’t have a good range of motion.
Wear
With the rise in knee joint replacements, surgeons have begun to see wear in the plastic parts of the artificial joints. In some cases, if the wear is discovered in time, the revision may only require changing the plastic part of the artificial joint. If the wear continues until the metal is rubbing on metal, the whole joint may need to be replaced.
Breakage
Finally, the metal of the artificial joint can break due to the constant stress that the artificial joint undergoes everyday. In weight-bearing joints like the knee, this is greatly affected by how much you weigh and how active you are.
Preparations
What happens before surgery?
Your surgeon will carefully plan the revision operation. Before the operation, many possible options and complications will have to be taken into account. Your surgeon will discuss these with you. Be sure to ask if there are parts of the procedure, your recovery, or the risks associated with a revision joint replacement that you have questions about.
Once the decision to proceed with surgery is made, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation.
You may be scheduled for a bone scan so the surgeon can check for loosening of the artificial joint. When an artificial joint is loose, the bone around the joint reacts by trying to form new bone, a process called remodeling. The bone scan is done by injecting you with a weak radioactive chemical. Several hours later, a large camera is used to take a picture of the bone around the artificial joint. If the artificial joint is loose and there is remodeling going on, the picture will show a hot spot where the chemical has been added to the newly forming bone. The brighter the hot spot, the more likely it is that the artificial joint is loose.
If your surgeon suspects that the artificial knee is loose, other tests may be necessary to find out why the joint is loose. Before any plans are made to revise the artificial joint, most orthopedic surgeons will want to make sure that the knee is not loose because of infection. To check for infection, blood tests may be ordered. Your surgeon may also need to aspirate your knee. This involves inserting a needle into your knee joint, removing fluid, and sending the contents to the laboratory. Replacing any artificial joint that is infected is much more involved than replacing a noninfected, loose artificial joint. In some cases, infection will make a revision impossible.
Skin problems are common for people having knee revision arthroplasty. People who have low levels of lymphocytes (white blood cells that form antibodies to fight off infection) have an even greater risk of incision problems. Your surgeon may request a blood count before surgery to make sure you have adequate numbers of lymphocytes.
Past incisions in the knee can further complicate the planned revision procedure. People needing a knee revision will have at least one previous knee incision. Most surgeons who do knee revision surgery prefer to make an incision that runs down the center of the knee. This may not be possible due to previous knee incisions. The second choice is usually toward the outer (lateral) side of the knee. (Lateral is the side furthest from your other knee.) If the skin appears to be too tight for a planned incision to close, the risk of wound complications is high after the revision procedure. The orthopedic surgeon may need to consult with a plastic surgeon to ensure the best approach and result.
Another option is to use soft-tissue expanders. These are placed just under the skin next to where the revision incision will eventually go. The expanders stay in for up to eight weeks and are removed when you go in for the revision surgery. The idea is that the skin will have stretched enough so that, when the revision procedure is done, the edges of the skin can be closed and sutured together.
Before surgery, you may also need to spend time with the physical therapist who will manage your rehabilitation after the surgery. The therapist begins the teaching process before surgery to ensure that you are ready for rehabilitation afterwards. One purpose of the preoperative therapy visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the available movement and strength of each knee. Any swelling in the artificial knee is noted.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will begin to practice some of the exercises you will use just after surgery. You will also be trained in the use of either a walker or crutches. Finally, an assessment will be made of any needs you will have at home once you’re released from the hospital.
You may be asked to donate some of your own blood before the operation. This blood can be donated three to five weeks earlier. Your body will make new blood cells to replace the loss. If you need a blood transfusion during the operation, you will receive your own blood back from the blood bank.
Surgical Procedure
What happens during the operation?
Before describing the revision procedure, let’s look at the revision prosthesis itself.
The Revision Prosthesis
There are two major types of revision implants:
- cemented prosthesis
- uncemented prosthesis
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis has a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
Both are still widely used. In many cases a combination of the two types is used. The patellar (kneecap) portion of the prosthesis is commonly cemented into place. The decision to use a cemented or uncemented artificial knee is usually made by the surgeon based on your age, your lifestyle, and the surgeon’s experience.
Each prosthesis is made up of three main parts. The tibial component (bottom portion) replaces the top surface of the lower bone, the tibia. The stem of the tibial component used in revision surgery is usually much longer than the type used for primary knee replacements. This is because the bone of the tibia is usually not the same as when the initial replacement was done. The bone may be weaker, or there may be areas inside the tibia where bone is missing. A longer stem can reach further down the tibial canal and distribute your body weight better. It also gives the body a greater surface area for healing, which can improve fixation of the implant to the bone inside the tibia.
The femoral component (top portion) replaces the bottom surface of the upper bone (the femur) and the groove where the patella fits. Like the tibial component used in revision, the femoral component often has a long stem.
The patellar component (kneecap portion) replaces the surface of the patella where it glides in the groove on the femur.
The tibial component is usually made of two parts: a metal tray that is attached directly to the bone, and a plastic spacer that provides the slick surface. The femoral component is made of metal. In some types of knee implants, the patellar component is made of a combination of metal and plastic.
The Operation
To begin the procedure, the surgeon makes an incision down the front of the knee to allow access to the joint. The surgeon attempts to open the knee joint with the least amount of damage to the muscles and ligaments around the joint.
Next, the original artifical joint is removed. When the primary artificial joint was put in with cement, the cement has to be removed from inside the canal of the femur and the tibia. Because the bone is often fragile and the cement is hard, removing the cement can cause the femur or tibia to fracture during the operation. This is not unusual, and in most cases the surgeon will simply continue with the operation and fix the fracture as well.
Samples of bone and marrow tissue are usually removed during the surgery and sent to a laboratory to see if any infection is present. If an infection is present, a new artificial joint will probably not be put in (see below).
Revision joint replacements are much different from primary joint replacements. One reason that revision procedures are not routine is that there is almost always bone loss around the primary prosthesis. The surgeon deals with this problem by placing a bone graft or some other material around the artificial joint to reinforce the bone. This bone graft may come from your own body, such as bone taken from the pelvis during the same operation. This type of graft is called an autograft.
If the amount of bone needed is too large to take from your body, your surgeon may choose to use bone graft from the bone bank. This type of bone graft has been taken from someone else and placed in the bone bank. This type of transplant is called an allograft.
After application of bone and other materials to rebuild the tibia and/or femur, a new prosthesis is implanted. It is challenging to imitate the natural shape of the bones after rebuilding the bone, so a specially designed prosthesis is usually needed. All of this is carefully planned by the surgeon before the operation.
To get the best and sturdiest fit between the tibial and femoral components, the surgeon adjusts and balances the soft tissues that surround the knee joint. This may require cutting or tightening the ligaments on each side of the knee. Afterward, the surgeon checks the fit of the new knee components with the knee bent and then with the knee straightened. Further adjustment is made by changing out a thicker plastic portion of the tibial component. In the end, the surgeon tries to get the best fit so that the knee is stable through a full range of movement.
When the tibial and femoral components are in place and the soft tissues have been balanced, the surgeon will address the patella. In some cases, the patella may not need to be revised, especially when the surgeon sees good fixation of the original patellar implant. Sometimes the old patella component is simply removed, allowing the bone on the back of the patella to glide against the smooth surface on the front of the revision femoral component. In either case, the surgeon checks to see that the patella is lined up correctly and that it rides normally within the groove in the front of the femur.
Finally, the soft tissues of the knee are sewn back together, and metal staples or stitches are used to hold the skin incision together.
A revision joint replacement of the knee is more complex and unpredictable than a primary joint replacement. Since many factors can influence its longevity, your surgeon will not be able to say exactly how long your revision will last. Also, keep in mind that because revision surgery is more complicated than primary joint replacement, it may take up to a year to be able to perform your routine daily activities. Often people continue to need a walking aid because knee pain increases when they are on their feet for prolonged periods. There is also a greater chance that the knee will be tight and unable to bend all the way after knee revision surgery.
In some cases, if an artificial joint fails, it may not be possible to put another artificial joint back in. This can occur if the primary joint has failed because of an infection that cannot be controlled, if the bone has been destroyed so much that it will not support an artificial joint, or if your medical condition will not tolerate a major operation.
Sometimes a choice other than knee revision is best because a big operation might result in a failure, or even death. Removing the prosthesis and not replacing it doesn’t mean the patient can’t walk anymore. The surgeon may suggest fusing the joints of the knee, placing a spacer in the joint, or in some cases amputating the leg.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following revision arthroplasty of the knee include
- anesthesia complications
- thrombophlebitis
- infection
- myositis ossificans
- loosening
- incision complications
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following an artificial joint revision. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder and colon to reduce the risk of spreading germs to the joint.
The risk of infection is higher in revision arthroplasty than in primary joint replacement. In a primary knee replacement, the risk of infection is less than one percent. It goes up to two percent or more in revision cases. These figures are only an estimate and vary between different scientific studies.
Myositis Ossificans
Myositis ossificans is a curious problem that can affect the knee after both a primary knee replacement and a revision knee replacement. The condition occurs when the soft tissue around the knee joint begins to develop calcium deposits. Myositis means inflammation of muscle, and ossificans refers to the formation of bone. This can lead to a situation where new bone actually forms along the sides and top of the knee. This leads to stiffness and a loss of motion in the knee joint. It also causes pain.
Myositis ossificans is more common in people who have a long history of osteoarthritis with multiple bones spurs. Something about the genetic makeup in these people makes them more likely to produce bone tissue. Major reconstruction operations such as a knee revision seem to do more damage to the surrounding tissues than primary knee replacements. The operation is simply longer and harder to do. Calcium deposits are also more likely to form.
The treatment of myositis ossificans may actually begin before you get it. In cases where you are at high risk for developing this condition, your surgeon may recommend that you take medications such as indomethacin after surgery. This medication reduces the tendency for bone to form and may protect you from developing myositis ossificans.
A much more effective method that has been used a great deal to prevent the development of myositis ossificans involves radiation treatments immediately after surgery. These are the same type of radiation treatments used to treat cancer. Several short radiation treatments begun the day after surgery and continued for three to five days seem to drastically reduce the risk of developing myositis ossificans.
If myositis ossificans forms despite these precautions, treatment will depend on how much it affects your knee. Your surgeon will note how much pain it causes and how much it restricts motion. In some severe cases, you may choose to have a second operation to remove the calcified tissue that has formed. This is usually followed by radiation treatments to prevent the calcium deposits from returning.
Loosening
The major reason that artificial joints eventually fail continues to be from loosening where the metal or cement meets the bone. A loose revised prosthesis is a problem because it causes pain. Once the pain becomes unbearable, another revision surgery may be needed. The rate of loosening is higher after revision surgery than in primary arthroplasties.
Incision Complications
Poor healing of the incision is a fairly common complication of knee revision arthoplasty. This is because the tissue is often scarred and thinner than when the original knee replacement was done. The blood supply to the skin may not be normal due to damage to the blood vessels from one or more previous knee surgeries. As mentioned earlier, previous skin incisions can make it hard for the incision to close after knee revision surgery, leading to complications. When the incision doesn’t heal right, the chances of infection go up. The wound may continue to ooze, creating optimal conditions for bacterial growth.
Poor incision healing is more likely to occur in patients with one or more of the following factors:
- anemia
- obesity
- past wound healing problems
- weak immune system
- tobacco habit
- poor circulation
- diabetes mellitus
Your surgeon’s goal is to prevent problems with the incision. If problems do happen, however, one or more additional surgeries will likely be needed.
After Surgery
What happens after surgery?
After surgery, your knee is covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming.
If a general anesthesia was used, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Several measures may be taken for patients who are at risk of incision problems. Some surgeons believe it is important to place a drain in the knee for a few days after surgery. The idea is that the drain will help keep swelling down. Too much swelling can pull the new incision apart and allow the wound to ooze. These factors place the knee at risk for infection. The practice of putting a drain in the knee is controversial, however, as some surgeons think that implanting the drain carries by itself an even bigger risk of infection.
A second measure to improve wound healing is to supply extra oxygen for three to four days through a nasal cannula. (A nasal cannula delivers oxygen through two small prongs placed into the nose.) The idea is that the added oxygen circulating in the blood stream will speed up the healing process and reduce the risk of incision problems.
You may also have physical therapy treatments once or twice each day as long as you are in the hospital. Therapy treatments will address the range of motion in the knee. Your therapist may also demonstrate exercises to improve knee mobility and engage the thigh and hip muscles. Ankle movements help pump swelling out of the leg and prevent the possibility of a blood clot.
When you are stabilized, your therapist will help you up for a short outing using your crutches or walker. After surgery, you may not be allowed to put weight on the affected leg for a period of time. This varies from surgeon to surgeon.
Most patients are able to go home after spending four to seven days in the hospital. You’ll be on your way home when you can get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and access the bathroom. It is also important that you regain a good muscle contraction of the quadriceps muscle and that you gain improved knee range of motion. Patients who need extra care may be sent to a different unit of the hospital until they are safe and ready to go home.
Most orthopedic surgeons recommend that you have routine checkups after your revision surgery. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends. You should always consult your orthopedic surgeon if you begin to have pain in your artificial joint or if you begin to suspect something is not working correctly.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your physical therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will review your exercise program and make recommendations about your safety.
Your staples will be removed two weeks after surgery. Patients are usually able to drive within eight weeks and walk without a walking aid by two to three months. Upon the approval of the surgeon, patients are generally able to resume sexual activity by six to eight weeks after surgery.
You may see a physical therapist for outpatient therapy. Your therapist may use heat, ice, or electrical stimulation if you are still having swelling or pain.
During this time, you should continue to use your walker or crutches as instructed. If you had a cemented procedure, you’ll advance the weight you place on your sore leg as much as you feel comfortable. If you had a noncemented procedure, place only the toes down until you’ve had a follow-up X-ray and your surgeon or therapist directs you to put more weight through your leg (usually by the fifth or sixth week after surgery). Most patients progress to using a cane in six to eight weeks.
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, thigh, and calf muscles. Endurance can be improved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the knee joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the knee. Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
Your therapist will work with you to help keep your revised knee joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your revised knee joint. Heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may need to consider alternate jobs to avoid work activities that require heavy lifting, crawling, and climbing.
The therapist’s goal is to help you maximize strength, walk normally, and improve your ability to do your activities. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Meniscal Injuries
A Patient’s Guide to Meniscal Injuries
Introduction
The meniscus is a commonly injured structure in the knee. The injury can occur in any age group. In younger people, the meniscus is fairly tough and rubbery, and tears usually occur as a result of a forceful twisting injury. The meniscus grows weaker with age, and meniscal tears can occur in aging adults as the result of fairly minor injuries, even from the up-and-down motion of squatting.
This guide will help you understand
- where the meniscus is located in the knee
- how an injured meniscus causes problems
- what can be done for an injured meniscus
Anatomy
What is a meniscus, and what does it do?
There are two menisci between the shinbone (tibia) and thighbone (femur) in the knee joint. (Menisci is plural for meniscus.)
The C-shaped medial meniscus is on the inside part of the knee, closest to your other knee. (Medial means closer to the middle of the body.) The U-shaped lateral meniscus is on the outer half of the knee joint. (Lateral means further out from the center of the body.)
These two menisci act like shock absorbers in the knee. Forming a gasket between the shinbone and the thighbone, they help spread out the forces that are transmitted across the joint. Walking puts up to two times your body weight on the joint. Running puts about eight times your body weight on the knee. As the knee bends, the back part of the menisci takes most of the pressure.
Articular cartilage is a smooth, slippery material that covers the ends of the bones that make up the knee joint. The articular cartilage allows the surfaces to slide against one another without damage to either surface.
By spreading out the forces on the knee joint, the menisci protect the articular cartilage from getting too much pressure on one small area on the surface of the joint. Without the menisci, the forces on the knee joint are concentrated onto a small area, leading to damage and degeneration of the articular cartilage, a condition called osteoarthritis.
The menisci add stability to the knee joint. They convert the surface of the shinbone into a shallow socket, which is more stable than its otherwise flat surface. Without the menisci, the round femur would slide on top of the flat surface of the tibia.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
How do meniscal problems develop?
Meniscal injuries can occur at any age, but the causes are somewhat different for each age group. In younger people, the meniscus is a fairly tough and rubbery structure. Tears in the meniscus in patients under 30 years old usually occur as a result of a fairly forceful twisting injury. In the younger age group, meniscal tears are more likely to be caused by a sport activity. The entire inner rim of the medial meniscus can be torn in what is called a bucket handle tear. The meniscus can also have a flap torn from the inner rim.
The tissue that forms the menisci weakens with age, making the menisci prone to degeneration and tearing. People of older ages often end up with a tear as result of a minor injury, such as from the up-and-down motion of squatting. Most often, there isn’t one specific injury to the knee that leads to the degenerative type of meniscal tear. These tears of the menisci are commonly seen as a part of the overall condition of osteoarthritis of the knee in aging adults. Degenerative tears cause the menisci to fray and become torn in many directions.
Symptoms
What does a torn meniscus feel like?
The most common problem caused by a torn meniscus is pain. The pain may be felt along the edge of the knee joint closest to where the meniscus is located. Or the pain may be more vague and involve the whole knee.
The knee may swell, causing it to feel stiff and tight. This is usually because fluid accumulates inside the knee joint. This is sometimes called water on the knee. This is not unique to meniscal tears, since it can also occur when the knee becomes inflamed.
The knee joint can also lock up if the tear is large enough. Locking refers to the inability to completely straighten out the knee. This can happen when a fragment of the meniscus tears free and gets caught in the hinge mechanism of the knee, like a pencil stuck in the hinge of a door.
A torn meniscus can cause long-term problems. The constant rubbing of the torn meniscus on the articular cartilage may cause the joint surface to become worn, leading to knee osteoarthritis.
Related Document: A Patient’s Guide to Osteoarthritis of the Knee
Diagnosis
How do doctors identify this problem?
Diagnosis begins with a history and physical exam. Your doctor will try to determine where the pain is located, whether you’ve had any locking, and if you have any clicks or pops with knee movement. X-rays will not show the torn meniscus. X-rays are mainly useful to determine if other injuries are present.
Magnetic resonance imaging (MRI) is very good at showing the meniscus. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This machine creates pictures that look like slices of the area. Usually, this test is done to look for injuries, such as tears in the menisci or ligaments of the knee. This test does not require any needles or special dye and is painless.
If there is uncertainty in the diagnosis following the history and physical examination, or if other injuries in addition to the meniscal tear are suspected, the MRI scan may be suggested.
If the history and physical examination indicate a torn meniscus, arthroscopy may be suggested to confirm the diagnosis and treat the problem at the same time. Arthroscopy is an operation that involves inserting a miniature fiber-optic TV camera into the knee joint, allowing the orthopedic surgeon to look at the structures inside the joint directly. The arthroscope lets the surgeon see the condition of the articular cartilage, the ligaments, and the menisci.
Treatment
What can be done for this injury?
Nonsurgical Treatment
Initial treatment for a torn meniscus focuses on decreasing pain and swelling in the knee. Rest and anti-inflammatory medications, such as aspirin, can help decrease these symptoms. You may need to use crutches until you can walk without a limp.
Some patients may receive physical therapy treatments for meniscal problems. Therapists treat swelling and pain with the use of ice, electrical stimulation, and rest periods with your leg supported in elevation. Exercises are used to help you regain normal movement of joints and muscles.
Surgery
If the knee keeps locking up and can’t be straightened out, surgery may be recommended as soon as reasonably possible to remove the torn part that is getting caught in the knee joint. But even a less severely torn meniscus may not heal on its own. If symptoms continue after nonsurgical treatment, surgery will probably be suggested to either remove or repair the torn portion of the meniscus.
Surgeons use an arthroscope (mentioned earlier) during surgery for an injured meniscus. Small incisions are made in the knee to allow the insertion of the camera into the joint.
Partial Meniscectomy
The procedure to take out the damaged portion of the meniscus is called a partial meniscectomy. The surgeon makes another small incision. This opening is needed to insert surgical instruments into the knee joint. The instruments are used to remove the torn portion of the meniscus, while the arthroscope is used to see what is happening.
Surgeons would rather not take out the entire meniscus. This is because the meniscus helps absorb shock and adds stability to the knee. Removal of the meniscus increases the risk of future knee arthritis. Only if the entire meniscus is damaged beyond repair is the entire meniscus removed.
Meniscal Repair
Whenever possible, surgeons prefer to repair a torn meniscus, rather than remove even a small piece. Young people who have recently torn their meniscus are generally good candidates for repair. Older patients with degenerative tears are not.
View animation of suture anchor placement
To repair the torn meniscus, the surgeon inserts the arthroscope and views the torn meniscus. Some surgeons use sutures to sew the torn edges of the meniscus together. Others use special fasteners, called suture anchors, to anchor the torn edges together.
Meniscal Transplantation
Surgeons are beginning to experiment with different ways to replace a damaged meniscus. One way is by transplanting tissue, called an allograft, from another person’s body. Further investigation is needed to see how well these patients do over a longer period of time.
Related Document: A Patient’s Guide to Meniscal Surgery
Rehabilitation
What should I expect from treatment?
Nonsurgical Rehabilitation
Nonsurgical rehabilitation for a meniscal injury typically lasts six to eight weeks. Therapists use methods such as electrical stimulation and ice to reduce pain and swelling. Exercises to improve knee range of motion and strength are added gradually. If your doctor prescribes a brace, your therapist will work with you to obtain and use the brace.
You can return to your sporting activities when your quadriceps and hamstring muscles are back to nearly their full strength and control, you are not having swelling that comes and goes, and you aren’t having problems with the knee giving way.
After Surgery
Rehabilitation proceeds cautiously after surgery on the meniscus, and treatments will vary depending on whether you had part of the meniscus taken out or your surgeon repaired or replaced the meniscus.
Patients are strongly advised to follow the recommendations about how much weight can be borne while standing or walking. After a partial meniscectomy, your surgeon may instruct you to place a comfortable amount of weight on your operated leg using a walking aid. After a meniscal repair, however, patients may be instructed to keep their knee straight in a locked knee brace and to put only minimal or no weight on their foot when standing or walking for up to six weeks.
Patients usually need only a few therapy visits after meniscectomy. Additional treatments may be scheduled if there are problems with swelling, pain, or weakness. Rehabilitation is slower after a meniscal repair or allograft procedure. At first, expect to see the physical therapist two to three times a week. If your surgery and rehabilitation go as planned, you may only need to do a home program and see your therapist every few weeks over a six-to eight-week period.
Glucosamine and Chondroitin Sulfate for Osteoarthritis of the Knee
A Patient’s Guide to Glucosamine and Chondroitin Sulfate for Osteoarthritis of the Knee
Introduction
Nonsurgical treatment of knee osteoarthritis (OA) focuses on reducing pain and maintaining or improving joint function. Doctors commonly prescribe acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and swelling in arthritic patients. Newer NSAIDs called COX-2 inhibitors are showing promise as well.
In recent years, two unique compounds have been used by people with knee OA. These compounds are gaining greater acceptance among many doctors. Glucosamine and chondroitin sulfate are dietary supplements usually taken in pill form that are thought to protect and possibly help repair cartilage cells.
Glucosamine and chondroitin sulfate are somewhat controversial treatments. While some studies have supported their effectiveness in relieving the symptoms of knee OA, the research still leaves many unanswered questions, especially about long-term effects.
This guide will help you understand
- what doctors believe the supplements can do
- how the treatments are administered
- what to expect after treatment
Anatomy
What part of the knee joint does OA affect?
The main problem in knee OA is degeneration of the articular cartilage. Articular cartilage is the smooth lining that covers the ends of bones where they meet to form the joint. The cartilage gives the knee joint freedom of movement by decreasing friction.
The articular cartilage is kept slippery by joint fluid made by the joint lining (the synovial membrane). The fluid, called synovial fluid, is contained in a soft tissue enclosure around synovial joints called the joint capsule.
An important substance present in articular cartilage and synovial fluid is called hyaluronic acid. Hyaluronic acid helps joints collect and hold water, improving lubrication and reducing friction. It also acts by allowing cells to move and work within the joint.
When the articular cartilage degenerates, or wears away, the bone underneath is uncovered and rubs against bone. Small outgrowths called bone spurs, or osteophytes, may form in the joint.
Related Document: A Patient’s Guide to Knee Anatomy
Rationale
What do doctors hope to achieve with these compounds?
Glucosamine and chondroitin sulfate occur naturally in the body, mainly in joint cartilage. They can also be made and given in pill form or by injection. The theory is that these supplements can help protect, or possibly even repair, damaged cartilage. Scientific studies lend support to the benefits that these supplements have on reducing pain, swelling, and tenderness, along with improving knee joint mobility.
Laboratory experiments suggest that glucosamine introduced to the body is absorbed by the synovial fluid. Glucosamine supplements also seem to encourage production of hyaluronic acid. Doctors think that normal hyaluronic acid levels in the knee joint keep the cartilage healthy and suppress pain in patients with knee OA.
Glucosamine and chondroitin sulfate also help fight inflammation, which in turn reduces joint pain, swelling, and tenderness from knee OA. These compounds seems to work in a different way than NSAIDs. They take longer to achieve the same beneft, but the results tend to last longer than NSAIDs. Most importantly, they have fewer side effects than NSAIDs. It’s possible that some patients may get good pain relief with a combination of the two.
Though the data isn’t conclusive, these two supplements have been shown to decrease pain and improve joint mobility in patients with knee OA. Most people start to notice a difference after taking the supplements for four weeks. Maximum benefits happen by eight to 12 weeks, and the benefits seem to last even after treatment has ended.
Preparation
How will I prepare for treatment?
Begin by gathering information. The Arthritis Foundation provides valuable information about these two supplements (www.arthritis.org).
Talk to your doctor. Not all forms of arthritis respond to these supplements. Realize that taking care of knee OA involves many possible treatments. Glucosamine and chondroitin sulfate are not magic bullets. They are one form of treatment in a comprehensive approach to knee OA.
Related Document: A Patient’s Guide to Osteoarthritis
Procedure
How are these treatments administered?
Doctors commonly prescribe oral glucosamine in doses of 500 milligrams three times per day or 1,000 milligrams twice per day. A patient may get a quicker response with a higher dosage. Obese patients may require higher dosages. Most studies of chondroitin sulfate use a dosage of 1,200 milligrams daily.
Complications
What might go wrong?
One potential benefit beyond pain relief for both glucosamine and chondroitin sulfate seems to be that patients experience fewer side effects with these drugs than with NSAIDs.
Most people can take these supplements without complications. The main complaints are gastrointestinal problems. These clear up when patients stop taking the supplement. Although rare, negative reactions may include nausea and vomiting, headache, painful digestion, softened or loose stool, abdominal pain, heartburn, throbbing or fluttering of the heart, skin reaction, edema (swelling), and discomfort in the legs.
Patients who take numerous medications should seek the advice of their doctor before supplementing with glucosamine and chondroitin sulfate. As glucosamine sulfate affects the way insulin works, diabetics are encouraged to monitor their blood glucose levels carefully and to alert their doctor of any marked changes. Also, children, pregnant women, and patients who are on blood thinners should only take chondroitin sulfate with the approval of their doctor.
After Care
What happens after treatment?
Many patients report ongoing benefits, even after they stop taking these supplements. Past studies have shown that the ability of these compounds to fight inflammation may be slower to take effect than NSAIDs. Yet the benefits seem to outlast NSAIDs. Until further studies are done, it is not proven that these supplements rebuild damaged cartilage. Given the possible protection to the cartilage, however, some doctors have their patients use these supplements in hopes of maintaining joint health.
Rehabilitation
Alhough glucosamine and chondroitin sulfate appear to have a useful place in treating knee OA, it is not recommended they be used alone. Managing knee OA works best using a variety of proven strategies. Patients do best when they also
- Get aerobic exercise.
- Do strengthening and range-of-motion exercises. These are most often taught and monitored by a physical therapist.
- Lose weight.
- Use heat and cold packs.
- Wear wedged insoles in their shoes.
- Use equipment to help take pressure off the joints, such as a cane.
- Participate in education programs or support groups.
By decreasing pain and increasing joint movement, glucosamine and chondroitin sulfate may help patients maximize their ability to take care of their knee OA. Be sure to talk to your doctor to see whether these supplements will benefit your particular condition.