Hip
Hip Anatomy Animated Tutorial
Artificial Joint Replacement of the Hip, Anterior Approach
A Patient’s Guide to Artificial Joint Replacement of the Hip, Anterior Approach
Introduction
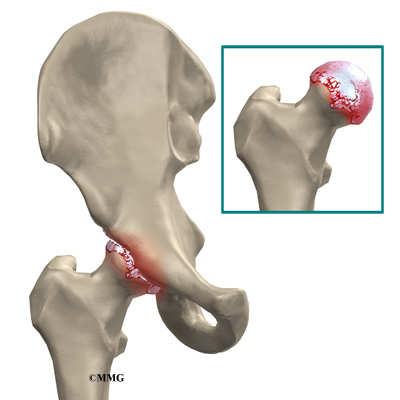
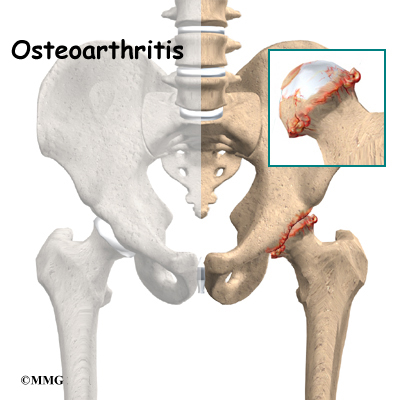
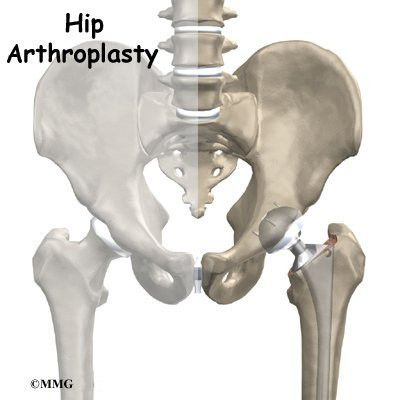
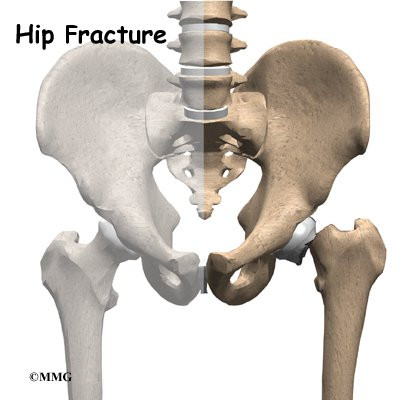
A hip that is painful as a result of osteoarthritis (OA) can severely affect your ability to lead a full, active life. Over the last 25 years, major advancements in hip replacement have improved the outcome of the surgery greatly. Hip replacement surgery (also called hip arthroplasty) is becoming more and more common as the population of the world begins to age.
There are several different ways of entering the hip joint to perform surgery on the hip; these are referred to by orthopaedic surgeons as “approaches” to the hip. The two most common approaches used in the past to perform artificial hip replacement are the “posterior” approach and the “anterolateral” approach. A new, less invasive approach to the hip joint that was pioneered over the last 20 years is being used more frequently today. Each approach has its own benefits, but the newer anterior approach is felt by many to be the best option today. In this document, we will be discussing the anterior approach.
In addition to reading this article, be sure to watch our Artificial Hip Replacement Anterior Approach (Hip Arthroplasty) Animated Tutorial Video.
This guide will help you understand
- what your surgeon hopes to achieve
- the benefits of the anterior approach
- what happens during the procedure
- what to expect after your operation
Anatomy
How does the hip normally work?
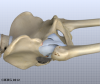
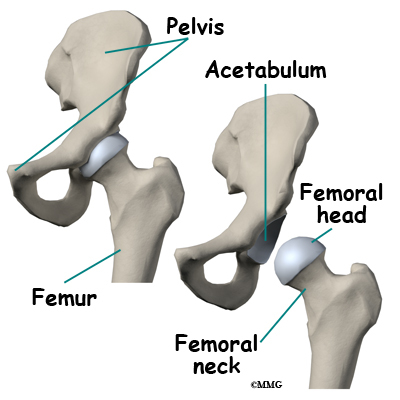
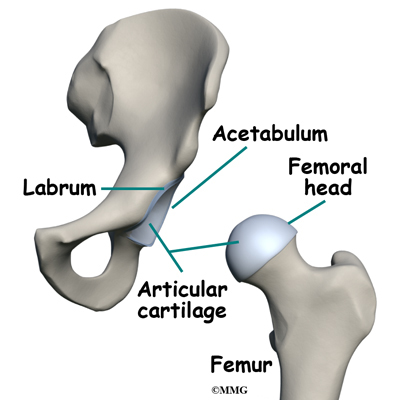
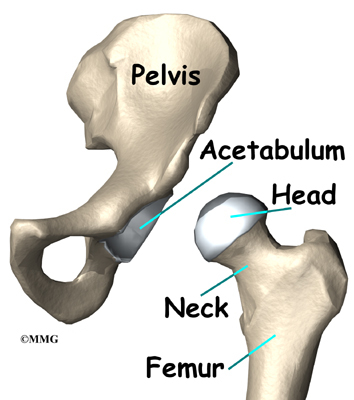
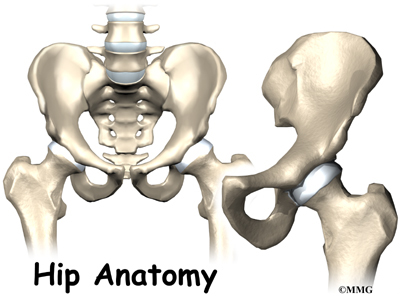
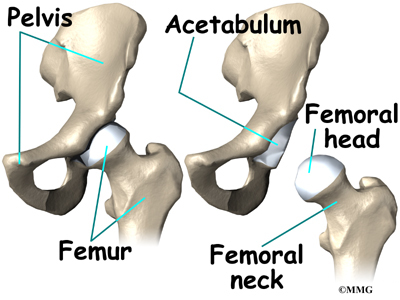
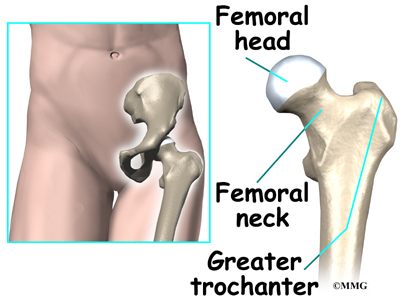
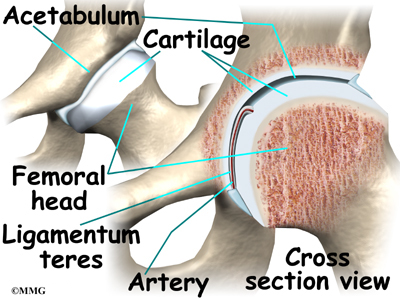
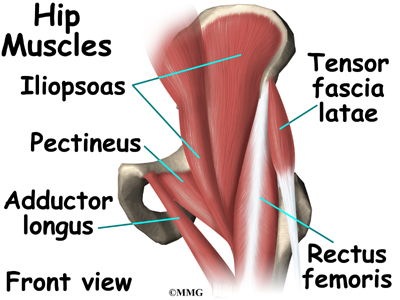
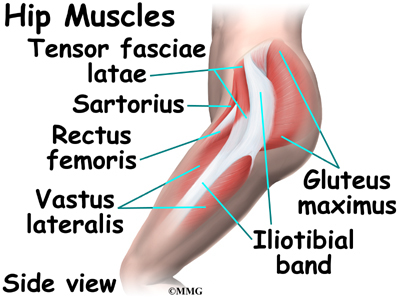
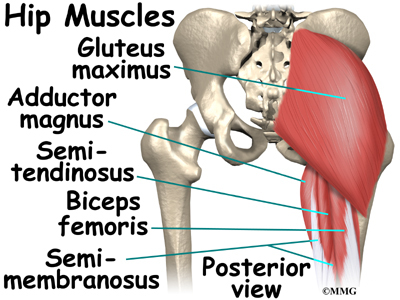
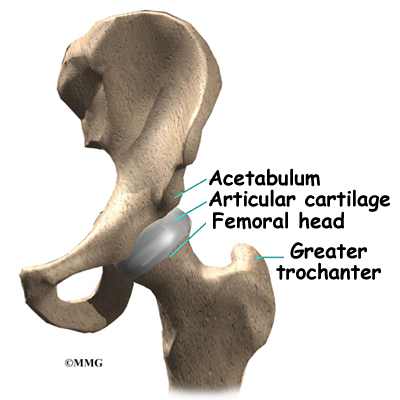
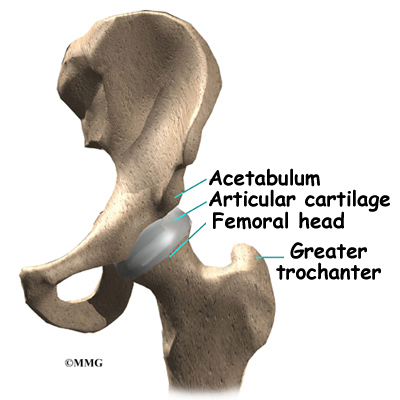
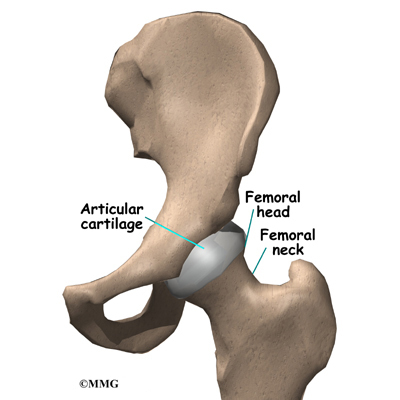
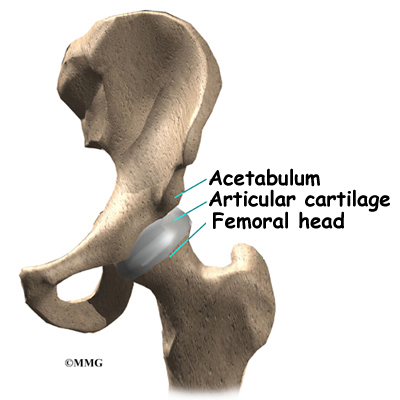
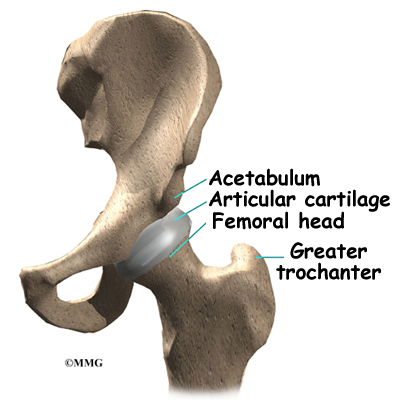
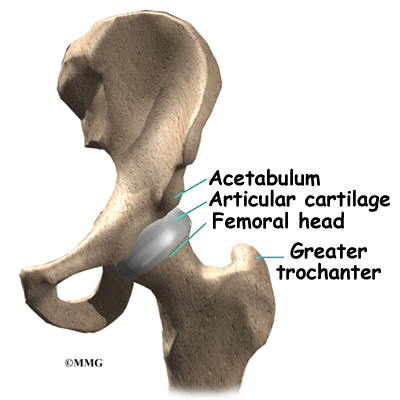
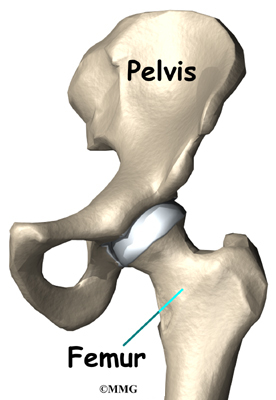
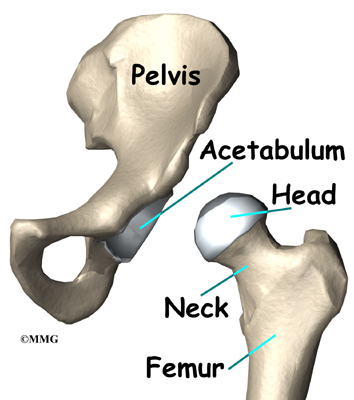
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone, known as the femoral head. The thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
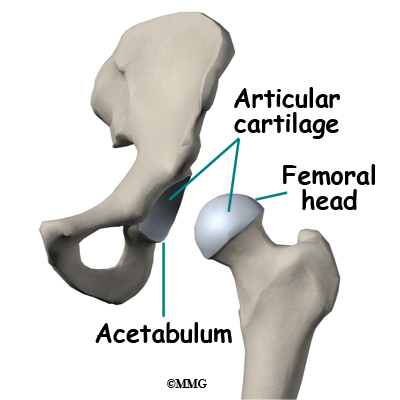
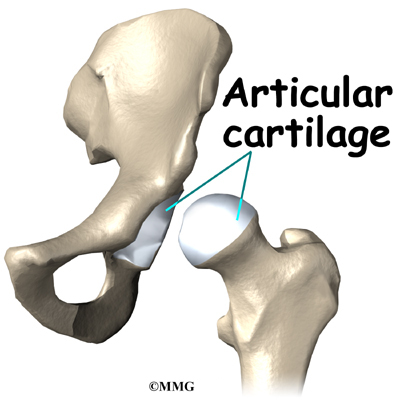
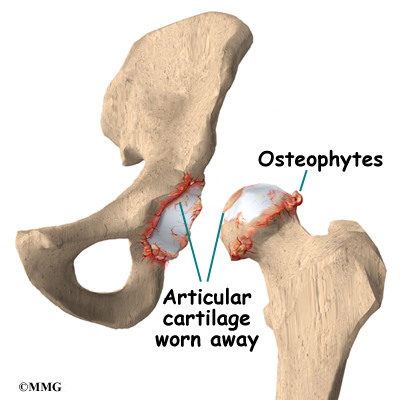
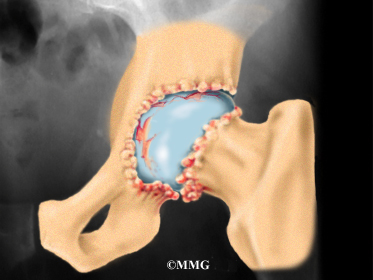
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
The main reason for replacing any arthritic joint with an artificial joint is to stop the bones from rubbing against each other. This rubbing causes pain. Replacing the painful and arthritic joint with an artificial joint gives the joint a new surface, which moves smoothly without causing pain. The goal is to help people return to many of their activities with less pain and greater freedom of movement.
Over the last decade, many surgeons have begun using smaller and smaller incisions to perform surgeries that once required larger incisions. This has been made possible due to the development of better tools and techniques to perform the procedures, as well as the use of computer assisted imaging. This trend is sometimes referred to as minimally invasive surgery.
There are many benefits to using smaller incisions including less damage to normal tissue and less blood loss. The anterior approach does not require the cutting of any muscles or tendons around the hip joint. Patients tend to recover quicker and are able to leave the hospital sooner after surgery. In the case of artificial hip replacement, using a smaller incision can result in less damage to the ligaments around the hip that provide stability to the joint. This means that the risk of dislocation of the artificial joint during recovery after surgery is lessened.
Many surgeons have adopted the anterior approach to the hip joint in order to utilize these minimally invasive techniques. Many research studies show that the risk of dislocation after surgery when using the anterior approach is significantly less that other approaches. The anterior approach is considered to be the most stable of all the approaches to the hip.
Related Document: A Patient’s Guide to Osteoarthritis of the Hip
Preparation
How should I prepare for surgery?
The decision to proceed with surgery should be made jointly by you and your surgeon only after you feel that you understand as much about the procedure as possible.
Once the decision to proceed with surgery is made, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation. You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery.
One purpose of the preoperative physical therapy visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the movement and strength of each hip.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will begin to practice some of the exercises you will use just after surgery. You will also be trained in the use of either a walker or crutches. Whether the surgeon uses a cemented or noncemented approach may determine how much weight you will be able to apply through your foot while walking.
This procedure requires the surgeon to open up the hip joint during surgery. This puts the hip at some risk for dislocation after surgery. To prevent dislocation, patients follow guidelines about which hip positions to avoid (called hip precautions). Your therapist will review these precautions with you during the preoperative visit and will drill you often to make sure you practice them at all times for at least six weeks. Some surgeons give the OK to discontinue the precautions after six to 12 weeks because they feel the soft tissues have gained enough strength by this time to keep the joint from dislocating. Finally, the therapist assesses any needs you will have at home once you’re released from the hospital.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
You may be asked to donate some of your own blood before the operation. Because of the trend towards newer minimally invasive techniques, hip replacement surgery today results in much less blood loss during surgery. You probably will not be asked to donate blood and probably will not require a blood transfusion after surgery. But, if your surgeon feels the surgery may be more complex and require a blood transfusion after surgery, this blood can be donated three to five weeks before the operation. During the time before the operation, your body will make new blood cells to replace the loss. At the time of the operation, if you need to have a blood transfusion you will receive your own blood back from the blood bank.
Surgical Procedure
Before we describe the procedure, let’s look first at the artificial hip itself.
The Artificial Hip
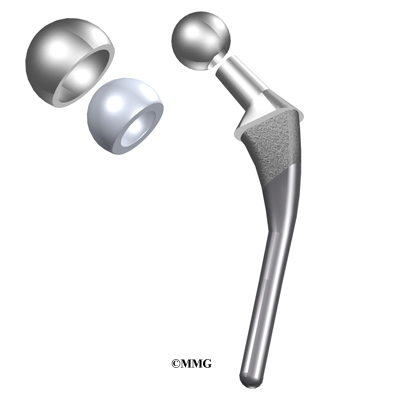
There are two major types of artificial hip replacements:
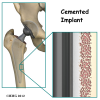
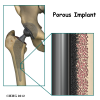
- cemented prosthesis
- noncemented prosthesis
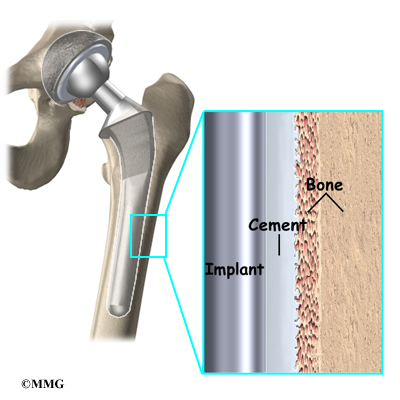
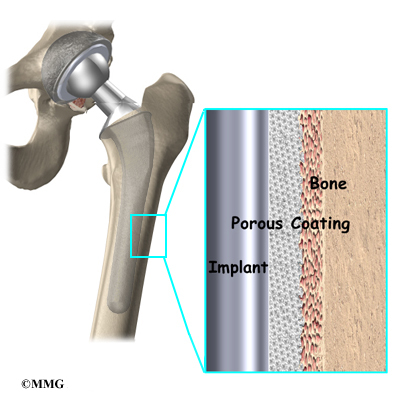
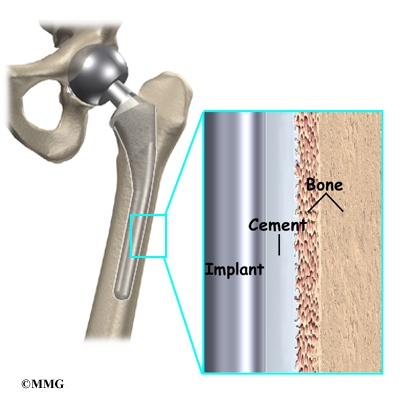
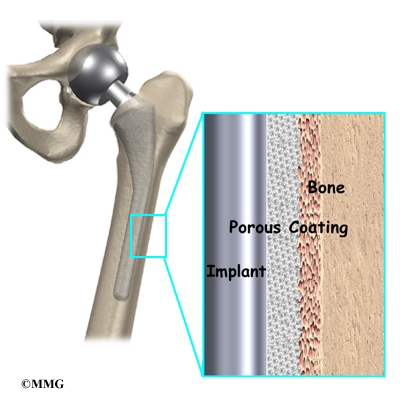
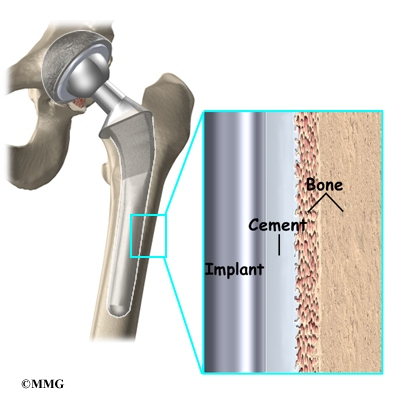
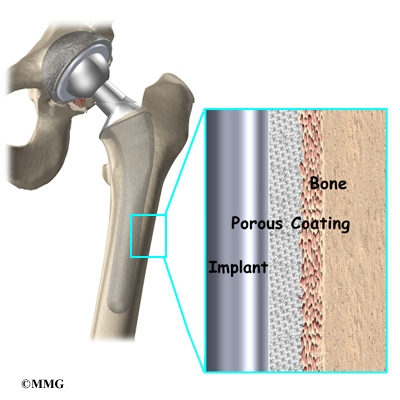
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An noncemented prosthesis bears a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
Both are still widely used. In some cases a combination of the two types is used in which the ball portion of the prosthesis is cemented into place, and the socket not cemented. The decision about whether to use a cemented or noncemented artificial hip is usually made by the surgeon based on your age and lifestyle, and the surgeon’s experience.
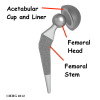
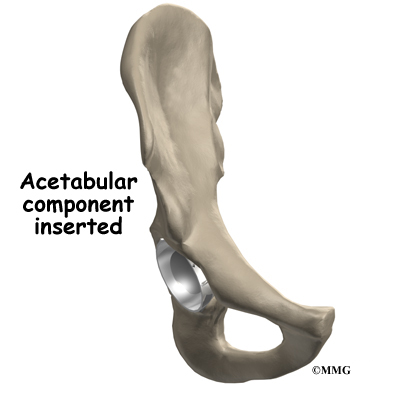
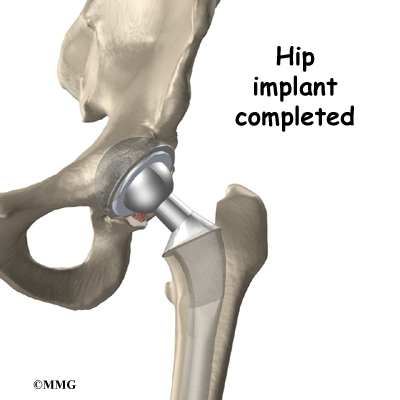
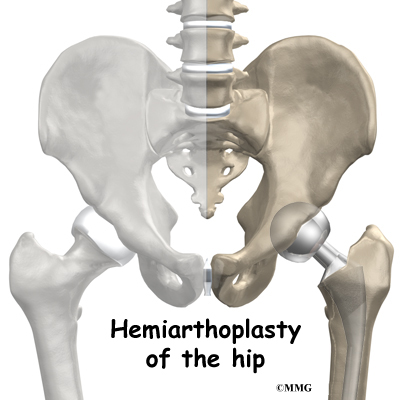
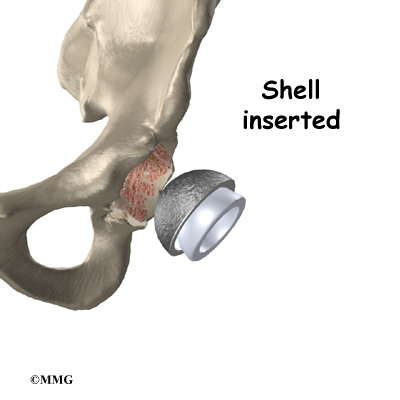
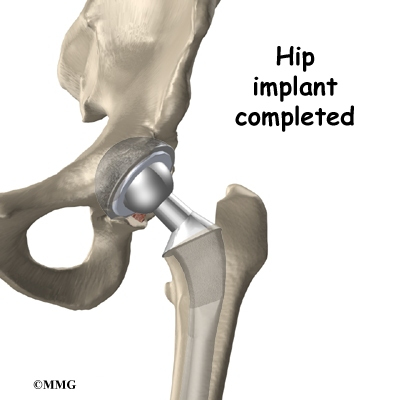
Each prosthesis is made of two main parts. The acetabular component (socket) replaces the acetabulum. The acetabular component is made of a metal shell with a plastic inner liner that provides the bearing surface. The plastic used is so tough and slick that you could ice skate on a sheet of it without much damage to the material.
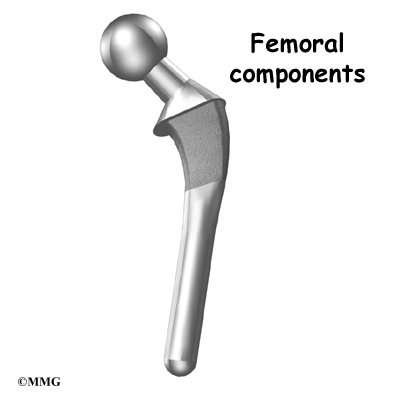
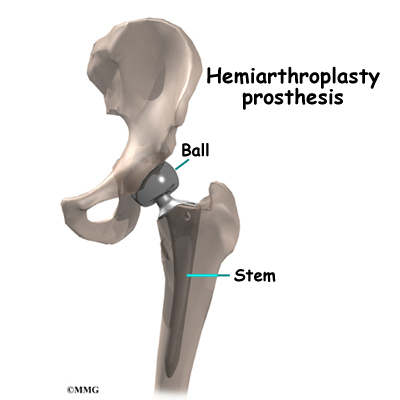
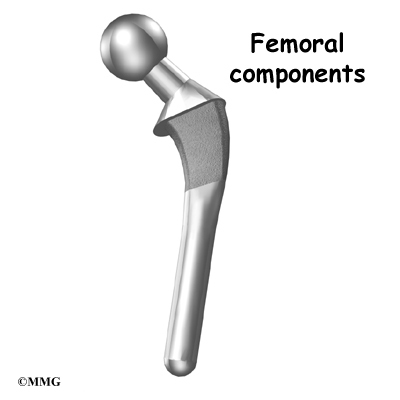
The femoral component (stem and ball) replaces the femoral head. The femoral component is made of metal. Sometimes, the metal stem is attached to a ceramic ball.
The Operation
Some type of anesthesia is necessary to perform a hip replacement. The procedure can be performed under general anesthesia or using some type of spinal anesthesia, such as an epidural or spinal. General anesthesia means that you are put completely asleep and a tube inserted into your windpipe to breathe for you while you are under the anesthesia. With a spinal type of anesthetic, you will be numb from the waist down after receiving an injection of anesthetic medication into your spinal canal. You will probably also be given medications to make you unaware of what is going on around you, but you will not have a tube inserted into your windpipe – you will breathe on your own. You should plan on discussing your options with your surgeon and anesthesiologist.
The surgeon begins by making an incision on the side of the thigh to allow access to the hip joint. Several different approaches can be used to make the incision. The choice is usually based on the surgeon’s training and preferences. For the anterior approach, an incision is made on the side of the thigh. This incision is usually around 4 to 6 inches but may be lengthened if more room is needed to complete the operation.
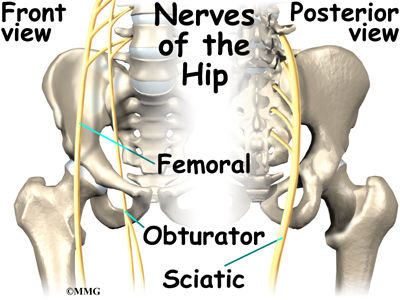
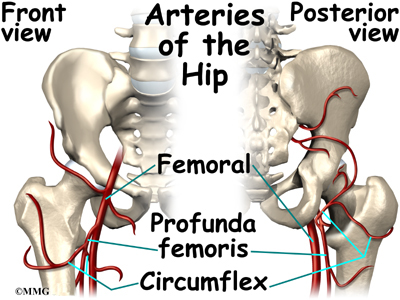
Once the skin incision is made, the muscles below the skin are separated to allow access to the hip joint. The nerves and blood vessels that run down the thigh in front of the hip joint are protected with special metal retractors. The anterior hip capsule that covers the front of the hip joint is opened by making an incision in the joint capsule.
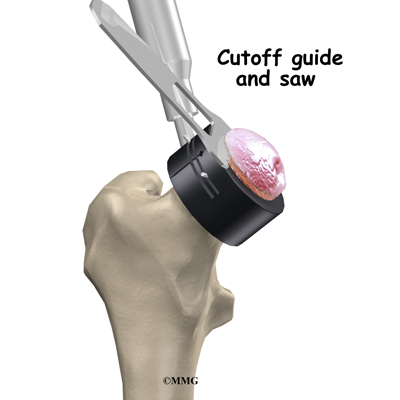
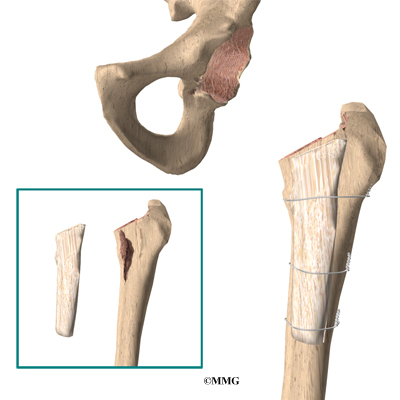
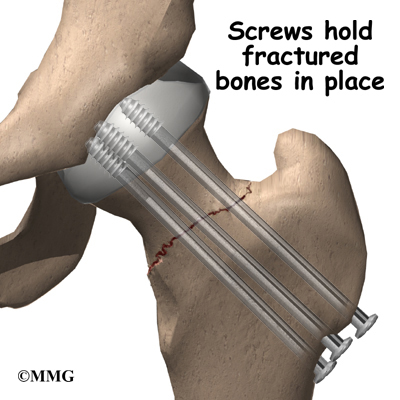
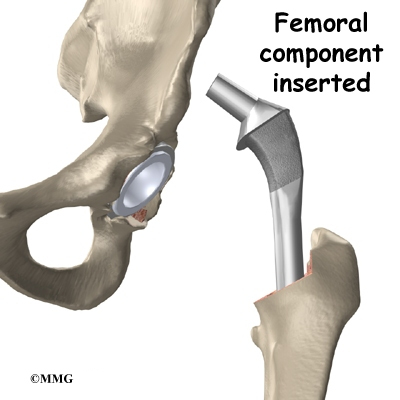
Once the hip joint is entered, the surgeon dislocates the femoral head from the acetabulum. Then the femoral head is removed by cutting through the femoral neck with a power saw.
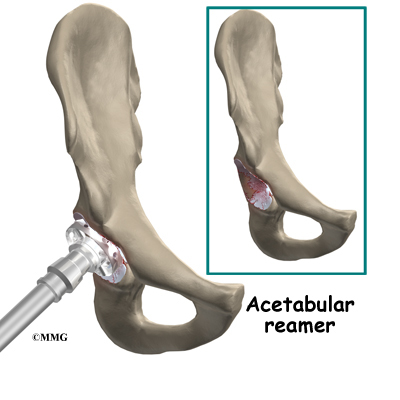
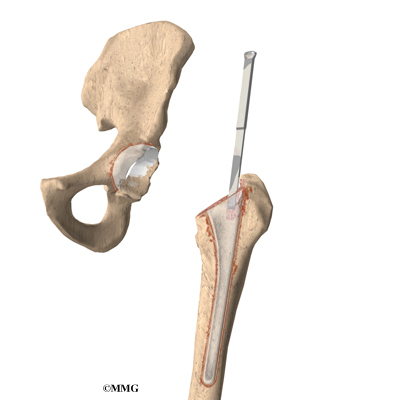
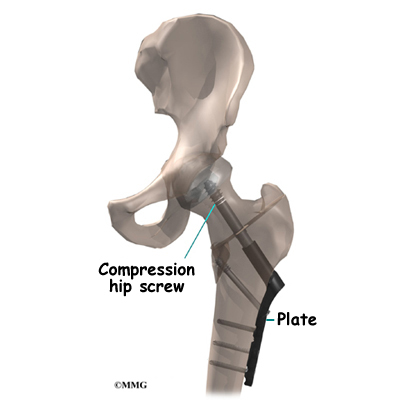
Attention is then turned toward the socket. The surgeon uses a power drill and a special reamer (a cutting tool used to enlarge or shape a hole) to remove cartilage from inside the acetabulum. The surgeon shapes the socket into the form of a half-sphere. This is done to make sure the metal shell of the acetabular component will fit perfectly inside. After shaping the acetabulum, the surgeon tests the new component to make sure it fits just right.
In the noncemented variety of artificial hip replacement, the metal shell is held in place by the tightness of the fit or by using screws to hold the shell in place. In the cemented variety, a special epoxy-type cement is used to anchor the acetabular component to the bone.
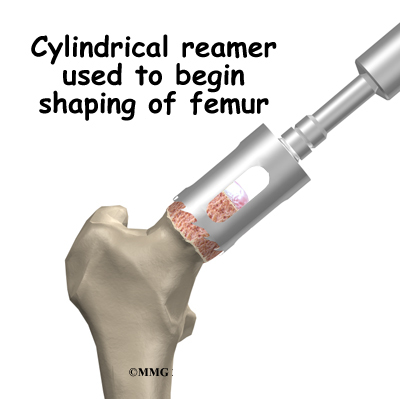
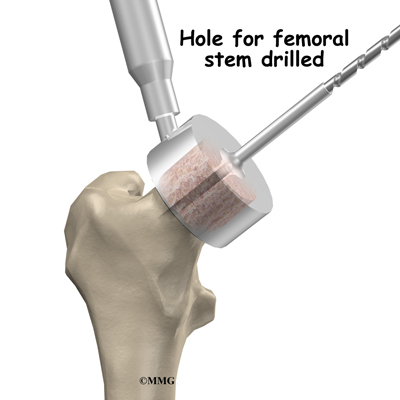
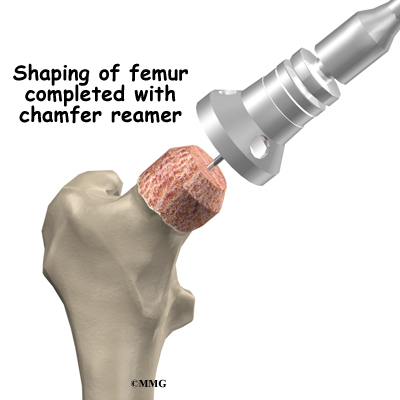
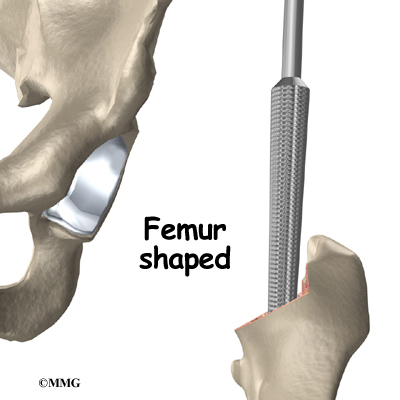
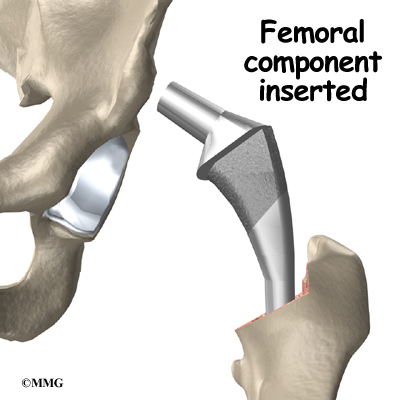
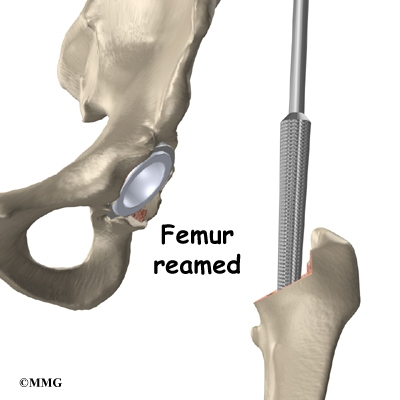
To begin replacing the femur, a drill is used to create the initial space to begin the process of preparing the femoral canal. Once the drilling is complete special rasps (filing tools) are used to shape the hollow femur to the exact shape of the metal stem of the femoral component. Once the size and shape are satisfactory, the stem is inserted into the femoral canal.
Again, in the noncemented variety of femoral component the stem is held in place by the tightness of the fit into the bone (similar to the friction that holds a nail driven into a hole that is slightly smaller than the diameter of the nail). In the cemented variety, the femoral canal is enlarged to a size slightly larger than the femoral stem, and the epoxy-type cement is used to bond the metal stem to the bone.
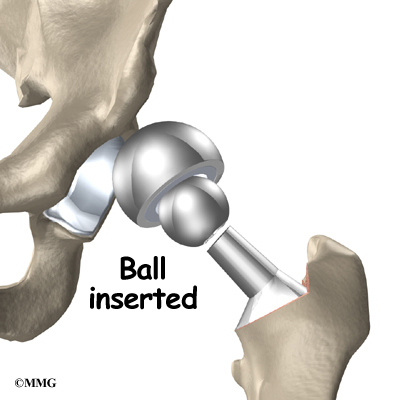
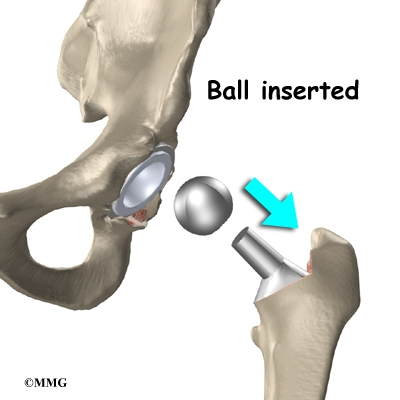
The metal ball that makes up the femoral head is then inserted. The hip is relocated and tested for range of motion and stability. The surgeon literally moves the leg in a full range of motion while watching the ball move in the plastic socket. The purpose of this step is to make sure that the hip moves well through the normal range of motion and does not tend to dislocate.
Once the surgeon is satisfied that everything fits properly, the incision is closed with stitches. Several layers of stitches are used under the skin, and either stitches or metal staples are then used to close the skin. A bandage is applied to the incision, and you are returned to the recovery room.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hip replacement surgery include
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be given during surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
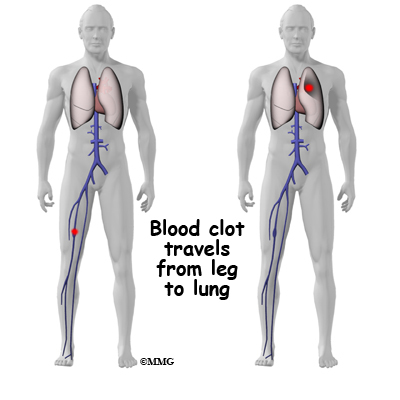
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following artificial joint replacement surgery. The chance of getting an infection following total hip replacement is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
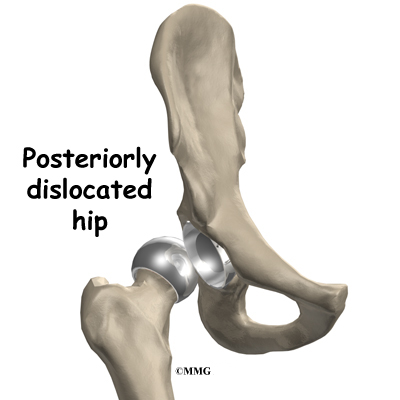
Dislocation
Just like your real hip, an artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. Once of the reasons that surgeons choose the anterior approach is that the risk of dislocation is much less than other approaches. But, there is still a small risk of dislocation even after using the anterior approach. The physical therapist will instruct you very carefully how to avoid activities and positions which may have a tendency to cause a hip dislocation. A hip that dislocates more than once may need to have another operation to make it more stable.
Loosening
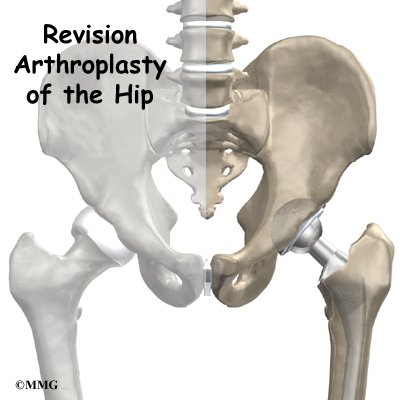
The main reason that artificial joints eventually fail continues to be the loosening of the metal or cement from the bone. Great advances have been made in extending how long an artificial joint will last,but any artificial joint may eventually loosen and require a revision. A “revision” is the term used to describe removing the old artificial joint parts and replacing them with new parts. Today you can expect 15 to 20 years of service from an artificial hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the hip.
Related Document: A Patient’s Guide to Revision Arthroplasty of the Hip
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Special boots and stockings are usually placed on your feet and legs to help prevent blood clots from forming.
If your surgery was performed under general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physical therapy treatments are scheduled one to three times each day as long as you are in the hospital. Your first treatment is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you’ll begin walking longer distances using your crutches or walker. Most patients are safe to put comfortable weight down when standing or walking. However, if your surgeon used a noncemented prosthesis, you may be instructed to limit the weight you bear on your foot when you are up and walking. Your therapist will review exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
Patients are usually able to go home after spending one to four days in the hospital. You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who still need extra care may be sent to a rehabilitation unit until they are safe and ready to go home.
Most orthopedic surgeons recommend that you have checkups on a routine basis after your artificial joint replacement. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends.
Patients who have an artificial joint will sometimes have episodes of pain, but if you have a period that lasts longer than a couple of weeks you should consult your surgeon. During the examination, the orthopedic surgeon will try to determine why you are feeling pain. X-rays may be taken of your artificial joint to compare with the ones taken earlier to see whether the joint shows any evidence of loosening.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will review your exercise program, continue working with you on your hip precautions, and make recommendations about your safety. These safety tips include using raised commode seats and bathtub benches, and raising the surfaces of couches and chairs. This keeps your hip from bending too far when you sit down. Bath benches and handrails can improve safety in the bathroom. Other suggestions may include the use of strategic lighting and the removal of loose rugs or electrical cords from the floor.
You should use your walker or crutches as instructed. You surgeon will advise you and your therapist how fast you can increase the weight you place through your leg. Most patients progress to using a cane in two to four weeks. In some cases, you may allowed to bear full weight almost immediately.
You may have your sutures or staples removed ten days to two weeks after surgery. Patients are usually able to drive within three weeks and walk without a walking aid by six weeks. Upon the approval of the surgeon, patients are generally able to resume sexual activity by one to two months after surgery.
The need for physical therapy usually requires a few visits in outpatient physical therapy. More visits may be needed for patients who have problems walking or who need to get back to heavier types of work or activities. Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program. When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Finally, if your surgeon feels additional physical therapy is necessary, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
Many patients have less pain and better mobility after having hip replacement surgery. But, you will need to follow some guidelines to help keep your new joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new hip joint. Heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may need to consider alternate jobs to avoid work activities that require heavy demands of lifting, crawling, and climbing.
<!–
//Document link: A Patient’s Guide to Rehabilitation After Total Hip Replacement; rehab_thr.txt]
–>
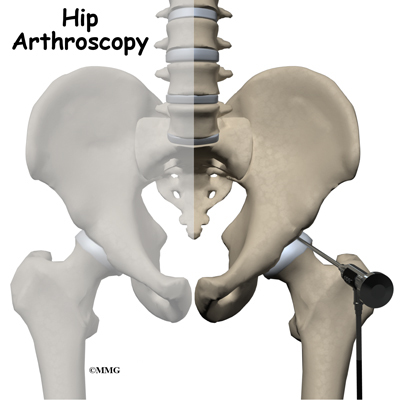
Hip Arthroscopy
A Patient’s Guide to Hip Arthroscopy
Introduction
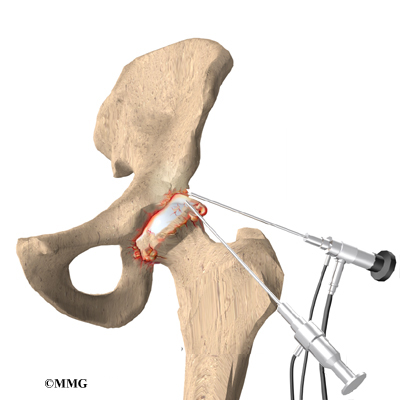
A hip arthroscopy is a procedure where a small video camera attached to a fiberoptic lens is inserted into the hip joint to allow a surgeon to see without making a large incision. Arthroscopy is now used to evaluate and treat orthopedic problems in many different joints of the body. While not as common as arthroscopy of the knee and shoulder, hip arthroscopy is used to evaluate and treat certain problems affecting the hip joint and the space outside the hip joint known as the greater trochanteric bursa.
This guide will help you understand
- what parts of the hip are treated during hip arthroscopy
- what types of conditions are treated with hip arthroscopy
- what to expect before and after hip arthroscopy
Anatomy
What parts of the hip are involved?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone. The thigh bone itself is called the femur, and the ball on the end is the femoral head. The ball and socket arrangement gives the hip a large amount of motion needed for daily activities like walking, squatting, and stair-climbing.
The surfaces of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
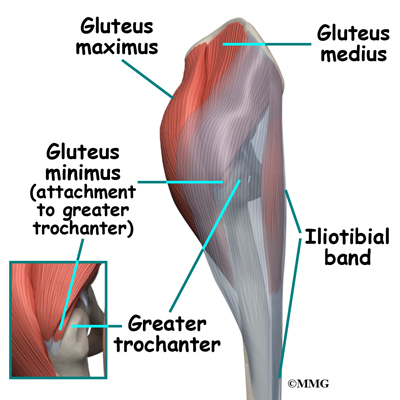
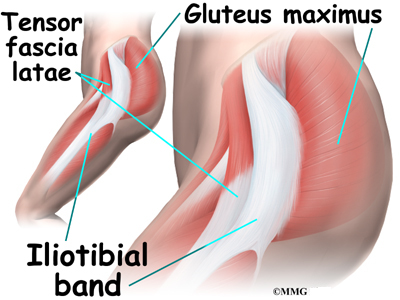
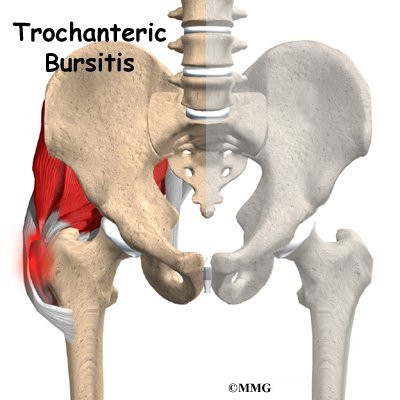
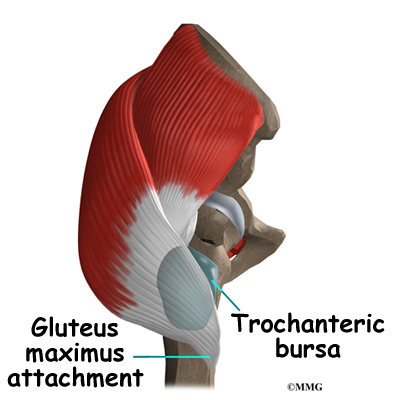
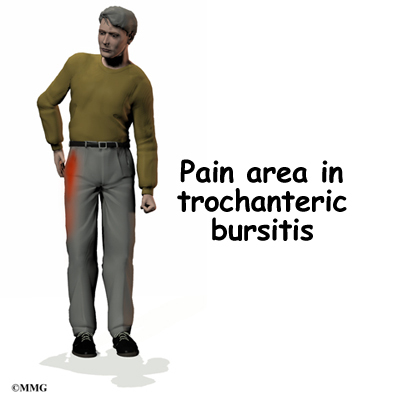
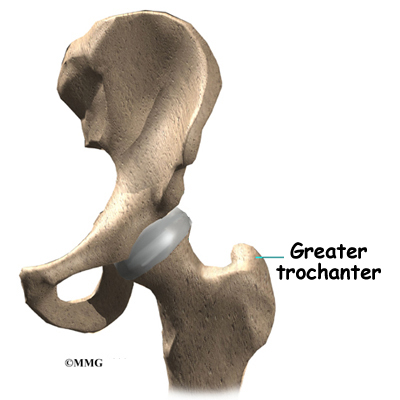
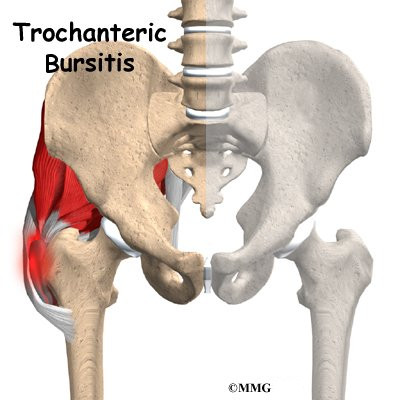
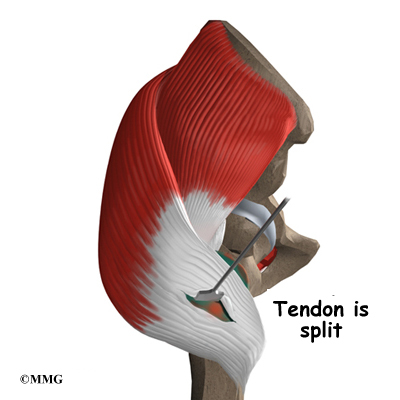
The gluteus maximus is the largest of three gluteal muscles of the buttock. This muscle spans the side of the hip and joins the iliotibial band. The iliotibial band is a long tendon that passes over the bursa on the outside of the greater trochanter. It runs down the side of the thigh and attaches just below the outside edge of the knee. Two other buttock muscles attach to the greater trochanter, the gluteus medius and the gluteus minimus. These muscles are known as the abductors because they function to pull the lower leg away from the body – a motion that is called abduction. These muscles can be torn where they attach to the greater trochanter causing pain and and weakness as well as a snapping sensation.
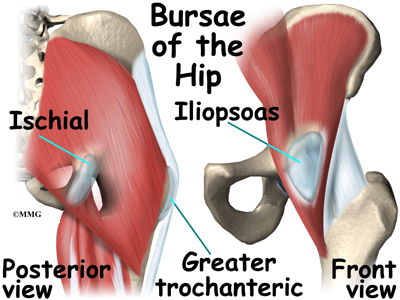
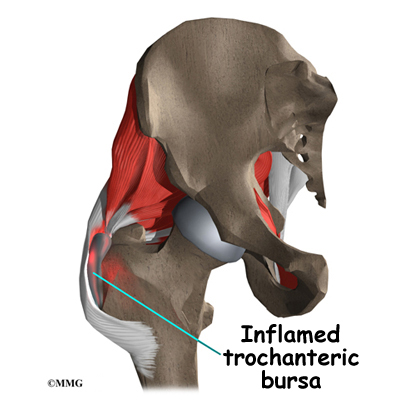
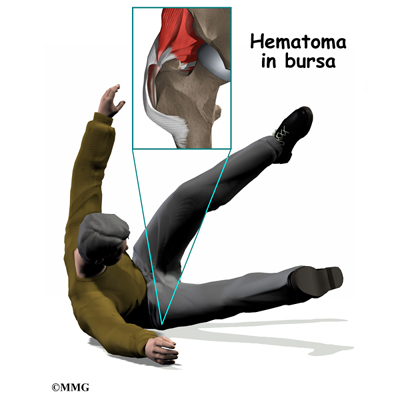
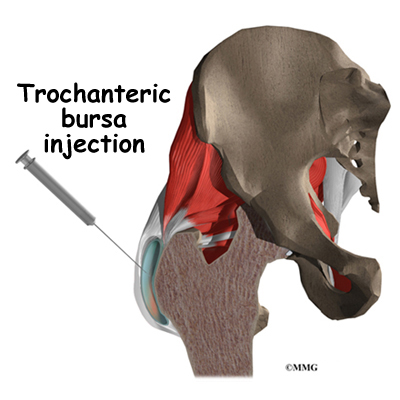
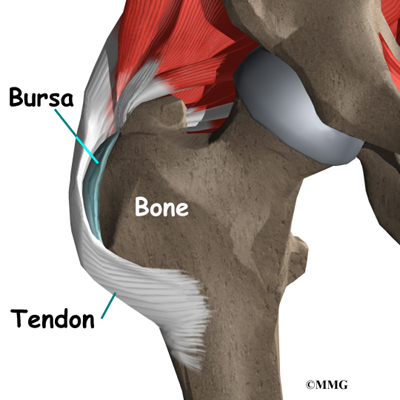
Where friction must occur between muscles, tendons, and bones, there is usually a bursa. A bursa is a thin sac of tissue that contains a bit of fluid to lubricate the area where the friction occurs. The bursa is a normal structure, and the body will even produce a bursa in response to friction. The bursa next to the greater trochanter is called the greater trochanteric bursa.
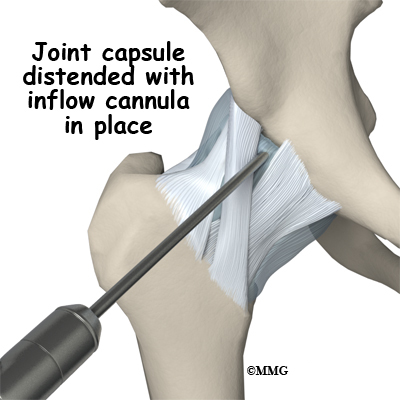
The hip joint is surrounded by a water-tight pocket called the joint capsule. This capsule is formed by ligaments, connective tissue and synovial tissue. When the joint capsule is filled with sterile saline and is distended, the surgeon can insert the arthroscope into the pocket that is formed, turn on the lights and the camera and see inside the hip joint as if looking into an aquarium. The surgeon can see nearly everything that is inside the hip joint including: (1) the joint surfaces of the femoral head and acetabulum (2) the acetabular labrum and (3) the synovial lining of the joint.
The arthroscope can also be inserted into the space outside the hip joint – the greater trochanteric bursa. This allows the surgeon to see the attachment of the gluteus medius muscle and the inside of the bursa.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does my surgeon hope to accomplish?
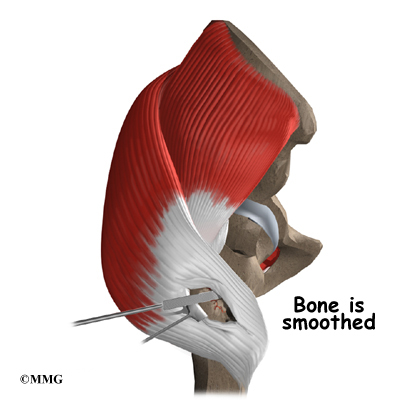
When hip arthroscopy first became available it was used primarily to look inside the hip joint and make a diagnosis. Today, hip arthroscopy is used in performing a wide range of different types of surgical procedures on the hip joint including confirming a diagnosis, removing loose bodies, removing or repairing a torn labrum, debriding excess inflamed bursa tissue, repairing a tear in the gluteus medius tendon and fixing fractures of the joint surface.
Your surgeon’s goal is to fix or improve your problem by performing a suitable surgical procedure; the arthroscope is a tool that improves the surgeons ability to perform that procedure. The arthroscope image is magnified and allows the surgeon to see better and clearer. The arthroscope allows the surgeon to see and perform surgery using much smaller incisions. This results in less tissue damage to normal tissue and can shorten the healing process. But remember, the arthroscope is only a tool. The results that you can expect from a hip arthroscopy depend on what is wrong with your hip, what can be done inside your hip to improve the problem and your effort at rehabilitation after the surgery.
Preparations
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, ability to do your activities, and the movement and strength of each hip.
A second purpose of the preoperative visit is to prepare you for surgery. The therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you will probably be admitted for surgery early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during hip arthroscopy?
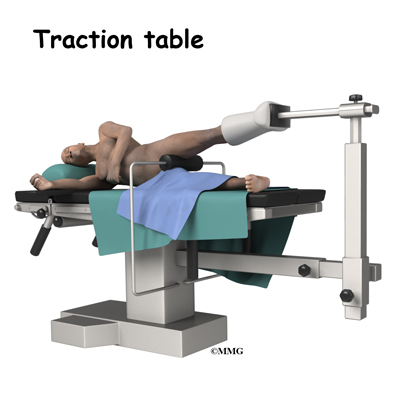
Before surgery you will be placed under either general anesthesia or a type of spinal anesthesia. A special operating room table called a traction table will be used.
The hip joint is very tight with little space between the ball and the socket. By applying traction, the surgeon is able to increase this space and allow the arthroscope to be inserted into that space. The end of the arthroscope will be moved about in this space to look throughout the joint. Finally, sterile drapes are placed to create a sterile environment for the surgeon to work. There is a great deal of equipment that surrounds the operating table including the TV screens, cameras, light sources, and surgical instruments.
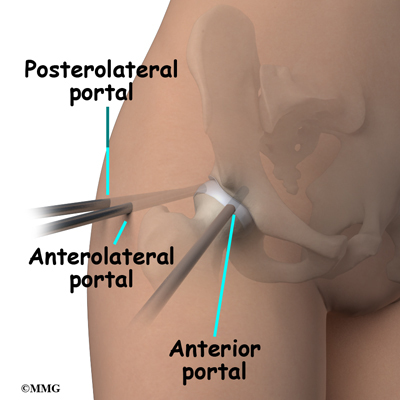
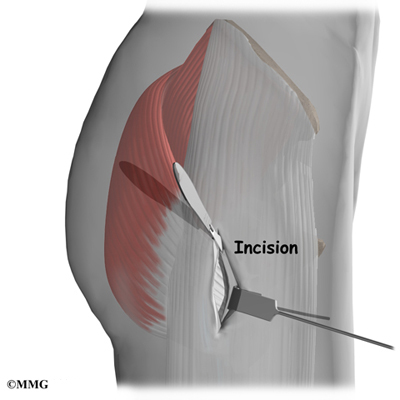
The surgeon begins the operation by making two or three small openings into the hip, called portals. These portals are where the arthroscope and surgical instruments are placed inside the hip. Care is taken to protect the nearby nerves and blood vessels. A small metal or plastic tube (or cannula) will be placed through one of the portals to inflate the hip with sterile saline.
The arthroscope is a small fiber-optic tube that is used to see and operate inside the joint. The arthroscope is a small metal tube about 1/4 inch in diameter (slightly smaller than a pencil) and about seven inches in length. The fiberoptics inside the metal tube of the arthroscope allows a bright light and TV camera to be connected to the outer end of the arthroscope. The light shines through the fiberoptic tube and into the hip joint. A TV camera is attached to the lens on the outer end of the arthroscope. The TV camera projects the image from inside the hip joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the hip) while moving the arthroscope to different places inside the hip joint and bursa.
Over the years since the invention of the arthroscope, many very specialized instruments have been developed to perform different types of surgery using the arthroscope to see what is going on while the instruments are being used. Today, many surgical procedures that once required large incisions for the surgeon to see and fix the problem can be done with much smaller incisions. For example, simple removal of a torn labrum or loose body can be done using two or three small 1/4 inch incisions. More extensive surgical procedures may require larger incisions. Your surgeon may decide during the procedure that the problem requires a more traditional open type operation. If this has been discussed before the operation the surgery may be performed immediately; if not, the arthroscopic procedure will be concluded and a later operation planned. Your surgeon will discuss the details of what was found at the time of the arthroscopy and what more needs to be done in the later operation.
Once the surgical procedure is complete, the arthroscopic portals and surgical incisions will be closed with sutures or surgical staples. A large bandage will be applied to the hip. You may be placed in compression stockings; compressive stockings reduce swelling and help prevent blood clots in the leg. Once the bandage has been placed, you will be taken to the recovery room.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur during hip arthroscopy. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hip arthroscopy are
- anesthesia complications
- thrombophlebitis
- infection
- equipment failure
- slow recovery
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following hip arthroscopy, it is possible that a postoperative infection may occur. This is very uncommon and happens in less than 1% of cases. You may experience increased pain, swelling, fever and redness, or drainage from the incisions. You should alert your surgeon if you think you are developing an infection.
Infections are of two types: superficial or deep. A superficial infection may occur in the skin around the incisions or portals. A superficial infection does not extend into the joint and can usually be treated with antibiotics alone. If the hip joint itself becomes infected, this is a serious complication and will require antibiotics and possibly another surgical procedure to drain the infection.
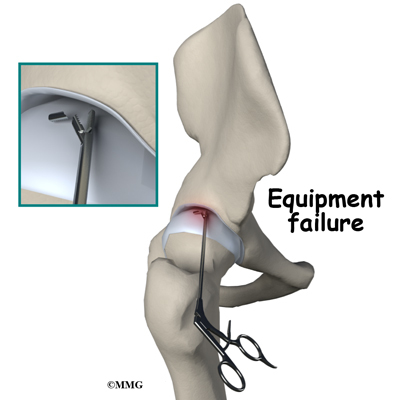
Equipment Failure
Many of the instruments used by the surgeon to perform hip arthroscopy are small and fragile. These instruments can be broken resulting in a piece of the instrument floating inside of the joint. The broken piece is usually easily located and removed, but this may cause the operation to last longer than planned. There is usually no damage to the hip joint due to the breakage.
Different types of surgical devices (screws, pins, and suture anchors) are used to hold tissue in place during and after arthroscopy. These devices can cause problems. If one breaks, the free-floating piece may hurt other parts inside the hip joint, particularly the articular cartilage. The end of the tissue anchor may poke too far through tissue and the point may rub and irritate nearby tissues. A second surgery may be needed to remove the device or fix problems with these devices.
Slow Recovery
Not everyone gets quickly back to routine activities after hip arthroscopy. Because the arthroscope allows surgeons to use smaller incisions than in the past, many patients mistakenly believe that less surgery was necessary. This is not always true. The arthroscpe allows surgeons to do a great deal of reconstructive surgery inside the hip without making large incisions. How fast you recover from hip arthroscopy depends on what type of surgery was done inside your hip. Simple problems that require simple procedures using the arthroscope generally get better faster. Patients with extensive damage to the hip articular cartilage tend to require more complex and extensive surgical procedures. These more extensive reconstructions take longer to heal and have a slower recovery. You should discuss this with your surgeon and make sure that you have realistic expectations of what to expect following arthroscopic hip surgery.
After Surgery
What happens after hip arthroscopy?
Hip arthroscopy is usually done on an outpatient basis meaning that patients go home the same day as the surgery. More complex reconstructions that require larger incisions and surgery that alters bone may require a short stay in the hospital to control pain more aggressively and monitor the situation carefully. You may also begin physical therapy while in the hospital.
The portals are covered with surgical strips, the larger incisions may have been repaired with either surgical staples or sutures. Crutches are commonly used after hip arthroscopy. They may only be needed for one to two days after a simple procedures.
Follow your surgeon’s instructions about how much weight to place on your foot while standing or walking. Avoid doing too much, too quickly. You may be instructed to use a cold pack on the hip and to keep your leg elevated and supported.
Rehabilitation
What will my recovery be like?
Your rehabilitation will depend on the type of surgery required. You may not need formal physical therapy after simple procedures such as a labral debridement. Some patients may simply do exercises as part of a home program after some simple instructions.
Many surgeons have patients take part in formal physical therapy after any type of hip arthroscopy procedure. Generally speaking, the more complex the surgery the more involved and prolonged your rehabilitation program will be. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. Physical therapists will also work with patients to make sure they are putting only a safe amount of weight on the affected leg.
Today, the arthroscope is used to perform quite complicated major reconstructive surgery using very small incisions. Remember, just because you have small incisions on the outside, there may be a great deal of healing tissue on the inside of the hip joint. If you have had major reconstructive surgery, you should expect full recovery to take several months. The physical therapist’s goal is to help you keep your pain under control and improve the range of motion and strength of your hip. When you are well under way, regular visits to your therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Femoroacetabular Impingement
A Patient’s Guide to Femoroacetabular Impingement of the Hip
Introduction
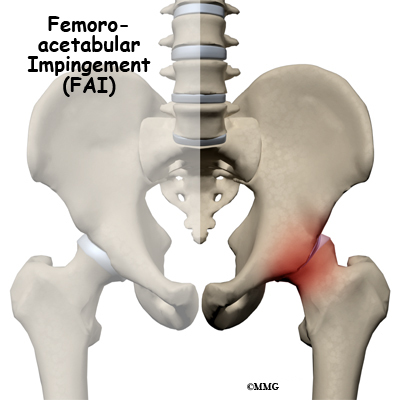
Femoroacetabular impingement (FAI) occurs in the hip joint. Impingement refers to some portion of the soft tissue around the hip socket getting pinched or compressed. Femoroacetabular tells us the impingement is occurring where the femur (thigh bone) meets the acetabulum (hip socket). There are several different types of impingement. They differ slightly depending on what gets pinched and where the impingement occurs.
This guide will help you understand
- what parts of the hip are involved
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the body is affected?
Femoroacetabular refers to the place in the hip where the round head of the femur (thigh bone) comes in contact with the acetabulum or hip socket. Two types of impingement are known to cause pinching of the soft tissues in this area.
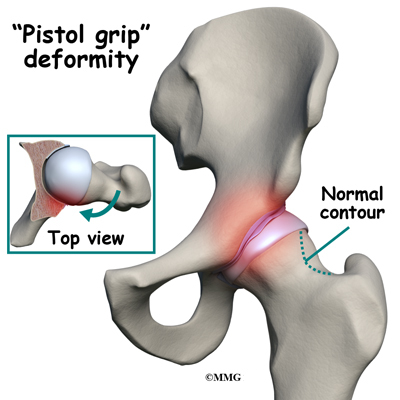
The first is called cam-type impingement. This occurs when the round head of the femur isn’t as round as it should be. It’s more of a pistol grip shape. It’s even referred to as a pistol grip deformity. The femoral head isn’t round enough on one side (and it’s too round on the other side) to move properly inside the socket.
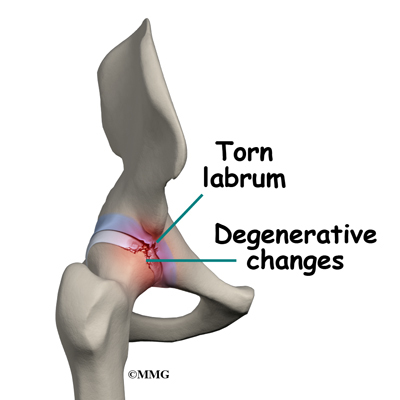
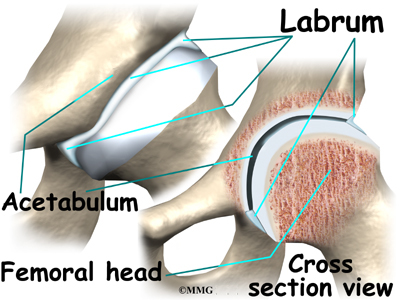
The result is a shearing force on the labrum and the articular cartilage, which is located next to the labrum. The labrum is a dense ring of fibrocartilage firmly attached around the acetabulum (socket). It provides depth and stability to the hip socket. The articular cartilage is the protective covering over the hip joint surface.
Sometimes cam-type impingement occurs as a result of some other hip problem (e.g., Legg-Calvé-Perthes disease, slipped capital femoral epiphysis or SCFE). But most of the time, it occurs by itself and is the main problem. Men are affected by cam-type impingement more often than women.
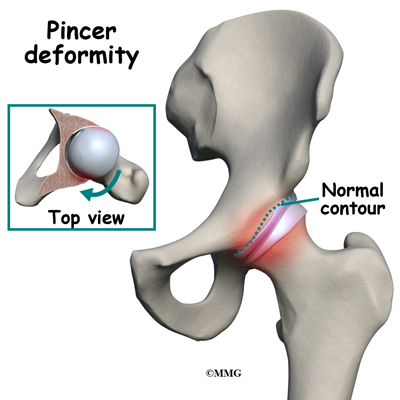
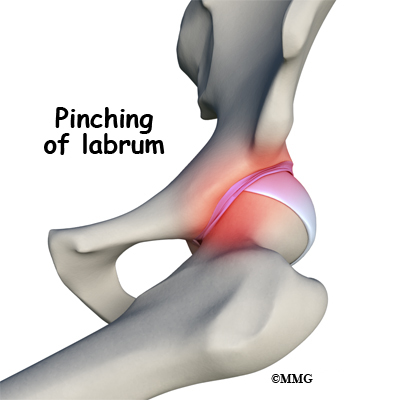
The second type of impingement is called pincer-type (more common in women). In this type, the socket covers too much of the femoral head. As the hip moves, the labrum comes in contact with the femoral neck just below the femoral head.
Pincer-type impingement is usually caused by some other problem. It could be as a result of 1) hip dysplasia, 2) a complication after osteotomy surgery to correct hip dysplasia, or 3) an abnormal position of the acetabulum called retroversion. Hip dysplasia is a deformity of the hip (either of the femoral head or the acetabulum, or both) that can lead to hip dislocation.
Related Document: Developmental Dysplasia of the Hip in Children
Related Document: Perthes Disease
Related Document: Slipped Capital Femoral Epiphysis
Causes
What causes this problem?
The cause of the problem has been under considerable debate for a long time. Now with better imaging studies, we know that some subtle changes in the shape of the femoral head may be the cause of FAI. Other anatomical changes in the angle of the hip may also contribute to this problem.
The basic problem is that the head of the femur butts up against the cartilage rim around the acetabulum and pinches it. An alternate type of femoral acetabular impingement causes abnormal jamming of the head-neck junction.
Normally, the femoral head moves smoothly inside the hip socket. The socket is just the right size to hold the head in place. If the acetabulum is too shallow or too small, the hip can dislocate. In the case of FAI, the socket may be too deep.
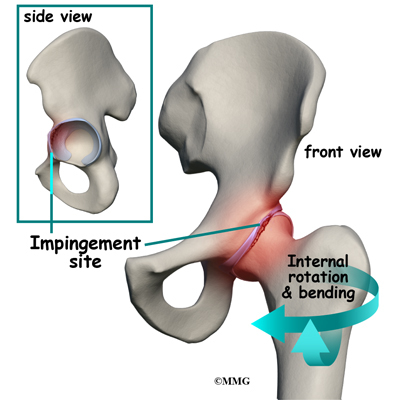
The rim of the cartilage hangs too far over the head. When the femur flexes (bends) and internally rotates, the cartilage gets pinched. Over time, this pinching or impingement of the labrum can cause fraying and tearing of the edges and/or osteoarthritic changes at the impingement site.
At the same time, with changes in the shape and structure of the hip, there are changes in normal hip movement. There may be too much hip adduction and internal rotation. Hip adduction refers to movement of the leg toward the body. Muscle weakness of the hip abductor muscles, hip extensors, and hip external rotators add to the problem. Hip abduction is moving the leg away from the body.
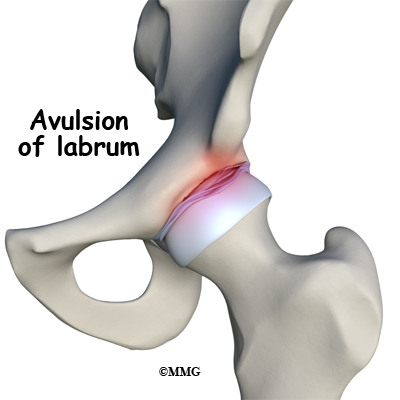
With the combined effects of anatomic changes in the hip and the resultant muscle imbalances, repetitive motions can create mini-traumas to the hip joint. The result can be an additional problem: partial or complete labral tears. A complete rupture is referred to as an avulsion where the labrum is separated from the acetabular cartilage where it normally attaches.
Symptoms
What does this condition feel like?
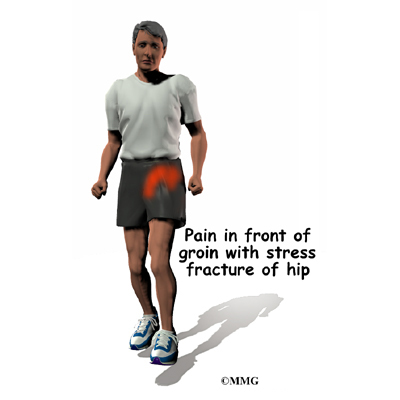
The first noticeable symptom of femoroacetabular impingement is often deep groin pain with activities that stress hip motion. Prolonged walking is especially difficult. Although the condition is often present on both sides, the symptoms are usually only felt on one side. In some cases, the groin pain doesn’t start until the person has been sitting and starts to stand up. There is often a slight limp because of pain and limited motion.
Groin pain associated with femoroacetabular impingement can be accompanied by clicking, locking, or catching when chronic impingement has resulted in a labral tear.
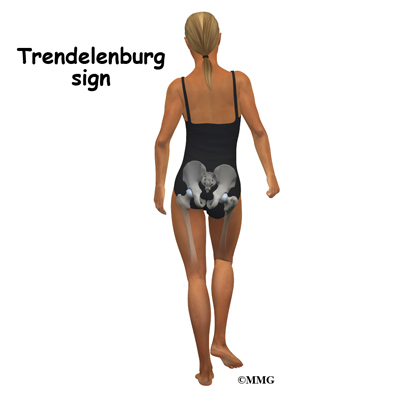
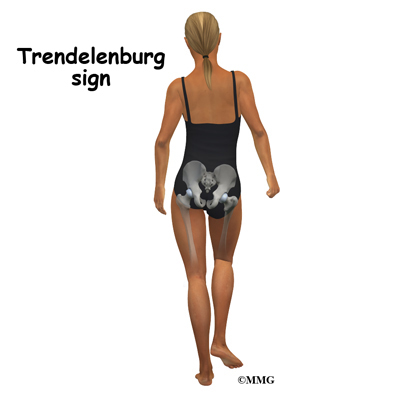
When femoroacetabular impingement and a labral tear are both present, symptoms get worse with long periods of standing, sitting, or walking. Pivoting on the involved leg is also reproduces the pain. Some patients have a positive Trendelenburg sign (hip drops down on the right side when standing on the left leg and vice versa).
As is often the case, one problem can lead to others. With femoroacetabular impingement, hip bursitis can develop. The gluteal (buttock) muscles may be extra tender or sore from trying to compensate and correct the problem. The pain can be constant and severe enough to limit all recreational activities and sports participation.
Related Document: Labral Tears of the Hip
Diagnosis
How do doctors diagnose the problem?
The diagnosis begins with a patient interview and history. Then the orthopedic surgeon performs a physical exam. The physician looks at pelvic and hip motion and palpates muscles and tendons for areas of tenderness.
Several tests can be done to identify what’s going on. The patient lies on the table on his or her back. The examiner bends the leg up, internally rotates the hip, and presses the knee toward the other leg. This position puts the hip in such a position that impingement occurs and reproduces the painful symptoms.
The clinical exam is followed up by imaging studies including X-rays, MRIs, and CT scans. X-rays show the presence of any extra bone build up as well as the position and alignment of the bones and joint. X-rays show the shape of the femoral head.
Any asymmetries (i.e., where the head is no longer an even round shape) are visible on X-rays. The radiologist and orthopedic surgeon reviewing the radiographs also look for three signs as an indication that there is retroversion: the crossover sign, the posterior wall sign, and the ischial sign.
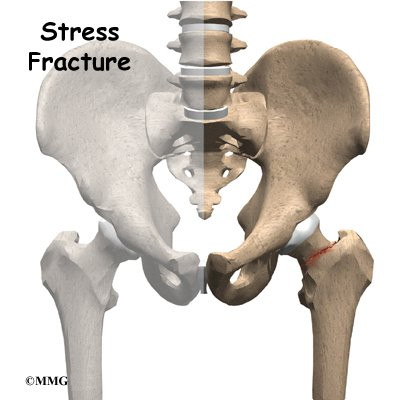
MRIs can show any damage to the labrum but not necessarily any changes to the surface of the hip joint. The presence of edema (swelling) under the bone may show up and requires further evaluation to decide if it is from femoroacetabular impingement or some other cause (e.g., cyst, tumor, stress fracture). Using MRI with a dye injected into the joint (called magnetic resonance arthrography or MRA) provides greater detail of the joint surface and may be needed.
CT scans help show the exact shape of the bone and reveal any abnormalities in the bone structure. CT scans might be the most helpful when arthroscopic surgery is planned. It gives the surgeon a better idea of what needs to be done to reshape the bone. If the procedure is going to be done with an open incision, then the CT scan isn’t necessary. The surgeon will see everything once the area is opened up.
Treatment
What can be done for this condition?
Once all the test results are available, a course of action is determined. This may be conservative (nonoperative) care with antiinflammatories and physical therapy. In some cases, surgery is recommended right away. Early diagnosis and surgical correction may be able to restore normal hip motion. Delaying surgery is possible for other patients but the long-term effect(s) of putting surgery off have not been determined.
Nonsurgical Treatment
A physical therapist will carry out an examination of joint motion; hip, trunk, and knee muscle strength; posture; alignment; and gait/movement analysis (looking at walking/movement patterns). A plan of care is designed for each patient based on his or her individual factors and characteristics.
Nonoperative care starts with activity modification (e.g., avoiding pivoting on the involved leg when there is a labral tear, avoiding prolonged periods of inactivity or activity). This part of the program must be followed for at least six months (often longer).
Improving biomechanical function of the hip involves strengthening appropriate muscles, restoring normal neuromuscular control, and addressing any postural issues. Tight muscles around the hip can contribute to pinching between the femoral head and acetabulum in certain positions. A program of flexibility and stretching exercises won’t change the bony abnormalities present but can help lengthen the muscles and reduce contact and subsequent impingement.
Some patients may also benefit from intra-articular injection with a numbing agent combined with an antiinflammatory (steroid) medication. Anyone needing surgery will also benefit from physical therapy first to address muscle imbalances resulting in abnormal movement patterns that lead to femoral acetabular impingement.
Surgery
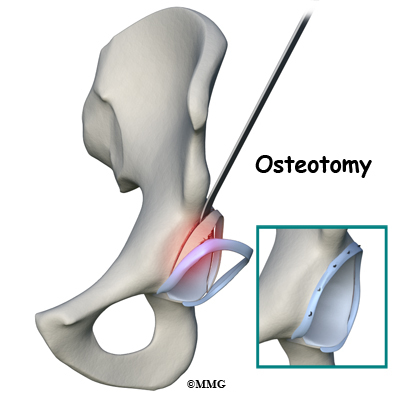
Surgery is advised when there is persistent pain despite a good effort at conservative care and when there are obvious structural abnormalities of the hip. Once it has been decided that surgery is the way to go, the surgeon has three choices: 1) full open incision and correction of the problem, 2) arthroscopic surgery, and 3) osteotomy.
With the fully open surgical procedure, the head of the femur is dislocated from the socket to make the changes and corrections and reshape it. With arthroscopic surgery, dislocation is not required. Osteotomy (reshaping the socket) is done for pincer-type impingement.
Whenever possible, the surgeon tries to save the hip. But when there is extensive damage to the cartilage, hip resurfacing or total joint replacement may be needed. There are many factors to consider when making this decision. The patient’s age, findings on imaging studies, type and severity of deformity, and the presence of arthritic changes are important.
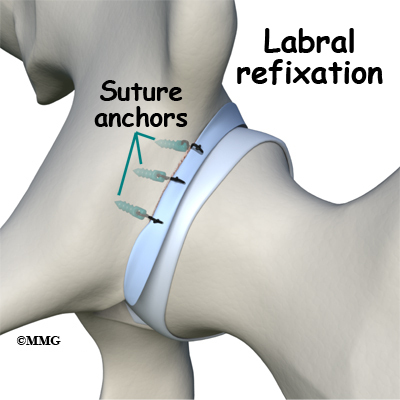
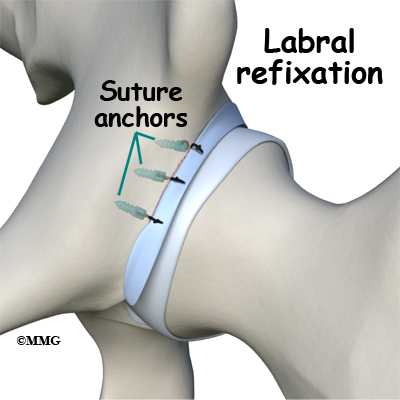
If there is a labral tear, surgery is usually done arthroscopically to repair (whenever possible) the damage. The surgeon trims the acetabular rim and then reattaches the torn labrum. This procedure is called labral refixation.
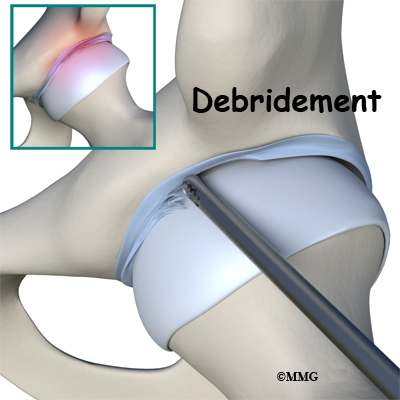
Each layer of tissue is sewn back together and reattached as closely as possible to its original position (called the footprint) along the acetabular rim. When repair is not possible, then debridement (shaving or removing) the torn tissue or pieces of tissue may be necessary.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
The goal of conservative management is to relieve pain and improve function by correcting muscle strength imbalances. When both legs have nearly equal strength, it is possible to resume a full and normal level of all activities (so long as there is no pain during any of those movements or activities).
For the young or active adult, this includes activities of daily living as well as recreational and sports participation. Older adults experiencing labral tears associated with the impingement problem may expect to be able to resume normal daily functions but may still find it necessary to limit prolonged sitting or standing positions.
After Surgery
Correction of the problem can result in improved function and pain relief. The hope is that early treatment can prevent arthritic changes but long-term studies have not been done to proven this idea.
After surgery, patients will be restricted to a partial weight-bearing status. The exact recommendations will depend on the amount of bone removed and whether or not the labrum was torn and repaired. Activity restriction is important for the first few weeks after surgery in order to avoid fatiguing or overloading the hip muscles.
Stationary bike exercises are allowed early on so long as the bike seat is kept high enough to avoid pinching at the hip during the flexion portion of the pedal cycle. Athletes and sports participants will be guided back to full participation by the physical therapist, usually five to six months after rehab. Many patients report continued improvements in their symptoms even up to the end of the first year after surgery.
Labral Tears of the Hip
A Patient’s Guide to Labral Tears of the Hip
Introduction
Acetabular labrum tears (labral tears) can cause pain, stiffness, and other disabling symptoms of the hip joint. The pain can occur if the labrum is torn, frayed, or damaged. Active adults between the ages of 20 and 40 are affected most often, requiring some type of treatment in order to stay active and functional. New information from ongoing studies is changing the way this condition is treated from a surgical approach to a more conservative (nonoperative) path.
This guide will help you understand
- what parts of the hip are involved
- how the condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the hip are involved?
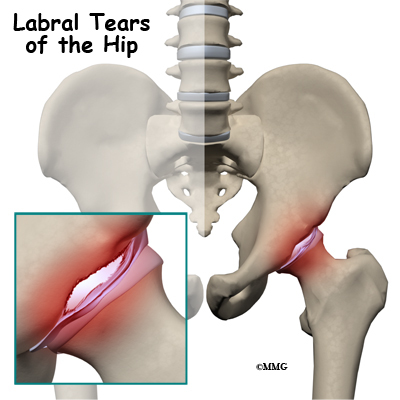
The acetabular labrum is a fibrous rim of cartilage around the hip socket that is important in normal function of the hip. It helps keep the head of the femur (thigh bone) inside the acetabulum (hip socket). It provides stability to the joint.
Our understanding of the acetabular labrum has expanded just in the last 10 years. The availability of high-power photography and improved lab techniques have made it possible to take a closer look at the structure of this area of the hip.
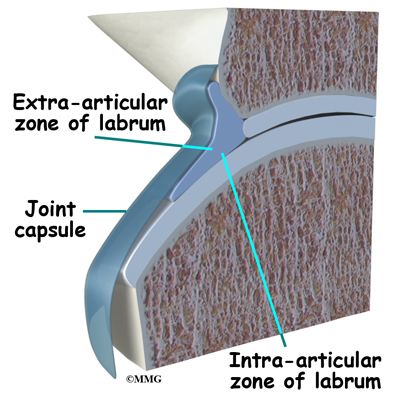
The labrum is a piece of connective tissue around the rim of the hip socket (acetabulum). It has two sides: one side is in contact with the head of the femur, the other side touches and interconnects with the joint capsule. The capsule is made up of strong ligaments that surround the hip and help hold it in place while still allowing it to move in many directions,
Finding out that there are two separate zones of the labrum was an important discovery. The extra-articular side (next to the joint capsule) has a good blood supply but the intra-articular zone (next to the joint) is mostly avascular (without blood). That means any damage to the extra-articular side is more likely to heal while the intra-articular side (with a very poor blood supply) does not heal well after injury or surgical repair.
The labrum helps seal the hip joint, thus maintaining fluid pressure inside the joint and providing the overall joint cartilage with nutrition. Without an intact seal, the risk of early degenerative arthritis increases. A damaged labrum can also result in a shift of the hip center of rotation. A change of this type increases the impact and load on the joint. Without the protection of the seal or with a hip that’s off-center, repetitive motion can create multiple small injuries to the labrum and to the hip joint. Over time, these small injuries can add to wear and tear in the hip joint.
Causes
How does this condition develop?
It was once believed that a single injury was the main reason labral tears occurred (running, twisting, slipping). But with improved radiographic imaging and anatomy studies, it’s clear now that abnormal shape and structure of the acetabulum, labrum, and/or femoral head can also lead to the problem.
Injury is still a major cause for labral tears. Anatomical changes that contribute to labral tears combined with repetitive small injuries lead to a gradual onset of the problem. Athletic activities that require repetitive pivoting motions or repeated hip flexion cause these type of small injuries.
What are these “anatomical changes”? The most common one called femoral acetabular impingement (FAI) is a major cause of hip labral tears. With FAI, there is decreased joint clearance between the junction of the femoral head and neck with the acetabular rim.
Related Document: Femoroacetabular Impingement of the Hip
When the leg bends, internally rotates, and moves toward the body, the bone of the femoral neck butts up against the acetabular rim pinching the labrum between the femoral neck and the acetabular rim. Over time, this pinching, or impingement, of the labrum causes fraying and tearing of the edges. A complete rupture is referred to as an avulsion where the labrum is separated from the edge of the acetabulum where it normally attaches.
Changes in normal hip movement combined with muscle weakness around the hip can lead to acetabular labrum tears. Other causes include capsular laxity (loose ligaments), hip dysplasia (shallow hip socket), traction injuries, and degenerative (arthritic) changes associated with aging. Anyone who has had a childhood hip disease (such as Legg-Calvé-Perthes disease, hip dysplasia, slipped capital femoral epiphysis) is also at increased risk for labral tears.
Related Document: Perthes Disease
Related Document: Developmental Dysplasia of the Hip in Children
Related Document: Slipped Capital Femoral Epiphysis
Symptoms
What does this condition feel like?
Pain in the front of the hip (most often in the groin area) accompanied by clicking, locking, or catching of the hip are the main symptoms reported with hip acetabular labral tears. Joint stiffness and a feeling of instability where the hip and leg seem to give away are also common. The pain may radiate (travel) to the buttocks, along the side of the hip, or even down to the knee.
Symptoms get worse with long periods of standing, sitting, or walking. Pivoting on the involved leg is avoided for the same reason (causes pain). Some patients walk with a limp or have a positive Trendelenburg sign (hip drops down on the right side when standing on the left leg and vice versa).
The pain can be constant and severe enough to limit all recreational activities and sports participation.
Diagnosis
How will my doctor diagnose this condition?
The history and physical examination are the first tools the physician uses to diagnose hip labral tears. There may or may not be a history of known trauma linked with the hip pain. When there are anatomic and structural causes or muscle imbalances contributing to the development of labral tears, symptoms may develop gradually over time.
Your doctor will perform several tests. One common test is the impingement sign. This test is done by bending the hip to 90 degrees (flexion), turning the hip inward internal rotation) and bringing the thigh towards the other hip (adduction).
Making the diagnosis isn’t always easy. In fact, this problem is frequently misdiagnosed at first. That’s because there are many possible causes of hip pain. The pain associated with labral tears can be hard to pinpoint. Your doctor must rely on additional tests to locate the exact cause of the pain. For example, injecting a local anesthetic agent (lidocaine) into the joint itself can help determine if the pain is coming from inside (versus outside) the joint.
X-rays provide a visual picture of any changes out of the ordinary of the entire structure and location of the hip position. Magnetic resonance imaging (MRI) gives a clearer picture of the soft tissues (e.g., labrum, cartilage, tendons, muscles).
One other test called a magnetic resonance arthrography (MRA) is now considered the gold standard for diagnosis. Studies show that MRA is highly sensitive and specific for labral tears. This test may replace arthroscopic examination as the main diagnostic tool. Arthroscopic examination is still 100 per cent accurate but requires a surgical procedure.
With MRAs, contrast dye (gadolinium) is injected into the hip joint. Any irregularity in the joint surface will show up when the dye seeps into areas where damage has occurred. MRAs give the surgeon an excellent view of the location and extent of the tear as well as any bony abnormalities that will have to be addressed during surgery.
Treatment
What treatment options are available?
In the past, when arthroscopic surgery was the only way to confirm the presence of a labral tear, the surgeon would just go ahead and remove the torn edges or pieces during the arthroscopic examination procedure. However, studies over the years have called this approach into question. With removal of the labrum, changes in the way the hip functioned, increased friction of the joint, and increased load on the joint led to degenerative changes and osteoarthritis.
Surgeons stopped cutting out the torn labrum and started repairing it instead. Physical therapists started doing studies that showed strengthening muscles and resolving issues of muscle imbalances could reduce the need for surgery with the traditional risks (e.g., bleeding, infection, poor wound healing, negative reactions to anesthesia).
More efforts are being made now to manage labral tears with conservative (nonoperative) care. This is a possibility most often when there are no symptoms of labral pathology. Patients with confirmed labral tears but who have normal hip anatomy or only mild changes in the shape and structure of the hip may also benefit from conservative care.
Nonsurgical Treatment
Physical therapy will probably be suggested. Your physical therapist will carry out an examination of joint motion; hip, trunk, and knee muscle strength; posture; alignment; and gait/movement analysis (looking at walking/movement patterns). A plan of care is designed for each patient based on his or her individual factors and characteristics.
Nonoperative care starts with activity modification. You should avoid pivoting on the involved leg and avoid prolonged periods of weight-bearing activities. You physical therapist will work with you to on strengthen your hip muscles, restore normal neuromuscular control, and improve your posture. All of these things can improve your hip function and reduce your pain.
Tight muscles around the hip can contribute to pinching between the femoral head and acetabulum in certain positions. A program of flexibility and stretching exercises won’t change the bony abnormalities present but can help lengthen the muscles and reduce contact and subsequent impingement.
A special strap called the SERF strap (SERF means Stability through External Rotation of the Femur) made of thin elastic may be applied around the thigh, knee, and lower leg to pull the hip into external rotation. The idea is to use the strap to improve hip control and leg movement during dynamic activities. It is important to strengthen the muscles at the same time to perform the same task and avoid depending on external support on a long-term basis.
Some patients may also benefit from intra-articular injection with cortisone. Cortisone is a very potent antiinflammatory medication. Injection into the hip joint may reduce the symptoms of pain for several weeks to months.
Surgery
Arthroscopy is commonly used to repair the torn labrum. The arthroscope is a small fiber-optic tube that is used to see and operate inside the joint. A TV camera is attached to the lens on the outer end of the arthroscope. The TV camera projects the image from inside the hip joint on a TV screen next to the surgeon. The surgeon actually watches the TV screen (not the hip) while moving the arthroscope to different places inside the hip joint and bursa.
During this procedure, your surgeon will trim the torn and frayed tissue around the acetabular rim and reattach the torn labrum to the bone of the acetabular rim. This procedure is called labral refixation. Each layer of tissue is sewn back together and reattached as closely as possible to its original position along the acetabular rim.
When repair is not possible, then debridement of the torn labral tissue may be necessary. Debridement simply means that the torn or weakened portions of the labrum are simply removed. This prevents the torn fragments from getting caught in the hip joint and causing pain and further damage to the hip joint.
In some cases, open treatment of femoroacetabular impingement and/or correction of bone abnormalities are required. These procedures are much more involved and usually will require a stay of several days in the hospital.
Related Document: A Patient’s Guide to Femoroacetabular Impingement
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
The goal of conservative management is to relieve pain and improve function by correcting muscle strength imbalances. When both legs have nearly equal strength, it is possible to resume a full and normal level of all activities as long as there is no pain during any of those movements or activities.
For the young or active adult, this includes activities of daily living as well as recreational and sports participation. Older adults experiencing labral tears from degenerative arthritis may expect to be able to resume normal daily functions, but may still find it necessary to limit prolonged sitting or standing positions.
After Surgery
Correction of the problem causing labral tears can result in improved function and pain relief. The hope is that early treatment can prevent arthritic changes but long-term studies have not been done to proven this idea.
Recovery after surgery needed to address hip labral tears usually takes four to six months. In other words, patients can expect to resume normal activities six months after surgery. Many athletes or highly active adults find this time frame much too long for their goals and preferences.
Patients who follow the recommended rehab plan of care respond well to progression of the exercises and seem to recover faster. Discharge from rehab takes place when the patient can perform all exercises with good form and without pain or other symptoms. Any repeat episodes of groin and/or hip pain must be reported to the orthopedic surgeon for evaluation right away.
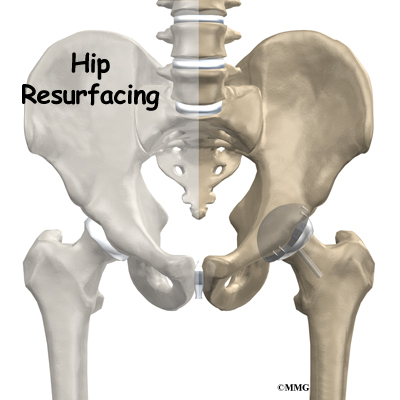
Hip Resurfacing Arthroplasty
A Patient’s Guide to Hip Resurfacing Arthroplasty
Introduction
A hip that is painful as a result of osteoarthritis (OA) can severely affect your ability to lead a full, active life. Over the last 25 years, major advancements in hip replacement have greatly improved the outcome of the surgery.
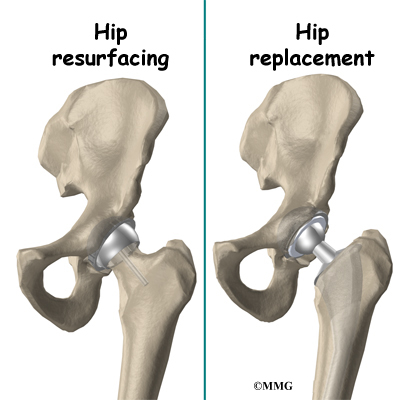
Hip resurfacing arthroplasty is a type of hip replacement that replaces the arthritic surface of the joint but removes far less bone than the traditional total hip replacement. Because the hip resurfacing removes less bone, it may be preferable for younger patients that are expected to need a second, or revision, hip replacement surgery as they grow older and wear out the original artificial hip replacement.
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the procedure
- what to expect after your operation
Anatomy
What parts of the hip are involved?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone, known as the femoral head. Hip resurfacing may only affect the head of the femur or it may involve both the femoral head and the hip socket.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
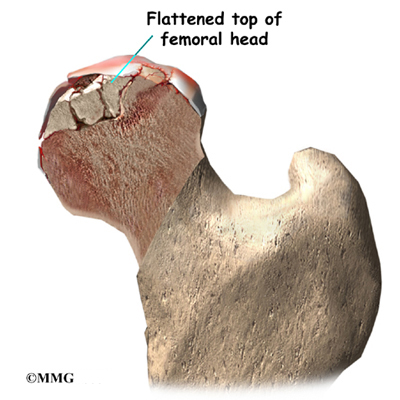
The main reason for replacing any arthritic joint with an artificial implant is to stop the bones from rubbing against each other. This rubbing causes pain. Replacing the painful and arthritic joint with a new surface, allows the joint to move smoothly without pain. The goal is to help people return to many of their activities with less pain and greater freedom of movement.
The most important reason to do a hip resurfacing rather than a traditional artificial hip replacement, is to remove as little bone around the hip as possible. This is especially important when you may need a second, or revision, hip replacement as you grow older.
The most common cause for revision of an artificial hip is loosening of the pieces of the artificial hip joint where it attaches to the bone. The loosening process results in wearing away of the bone around the metal components, or parts of the artificial joint. This is especially true around the stem of the femoral component that fits inside of the femoral shaft in the traditional artificial joint. The femoral component used during hip resurfacing is placed on the outside of the femoral head and the femoral shaft is never disturbed. This means that when a revision is needed, the femoral shaft can be used to hold the femoral component as if there has never been an artificial joint and the bone in this area is virginal.
Hip resurfacing is a good option for adults younger than 60 years who have arthritis and can be expected to require a revision of their hip replacement. This procedure is not advised for anyone with bone cysts, inflammatory arthritis, or for patients with severe arthritis or osteoporosis. Generally, a traditional total hip replacement is preferred in those cases.
Preparation
How should I prepare for surgery?
The decision to proceed with surgery should be made jointly by you and your surgeon only after you feel that you understand as much about the procedure as possible. Many patients wonder when they should consider surgery. Most surgeons agree that surgery is advised when a patient’s pain and discomfort limit daily life and activities.
Once the decision to proceed with surgery is made, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation. You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery.
One purpose of the preoperative physical therapy visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the movement and strength of each hip.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will begin to practice some of the exercises you will use just after surgery.
You will also be trained in the use of crutches or a walker. Your therapist will also assess any needs you will have at home or work once you’re released from the hospital.
You may be asked to donate some of your own blood before the operation. This blood can be donated three to five weeks before the operation, and your body will make new blood cells to replace the loss. At the time of the operation, if you need to have a blood transfusion you will receive your own blood back from the blood bank.
Surgical Procedure
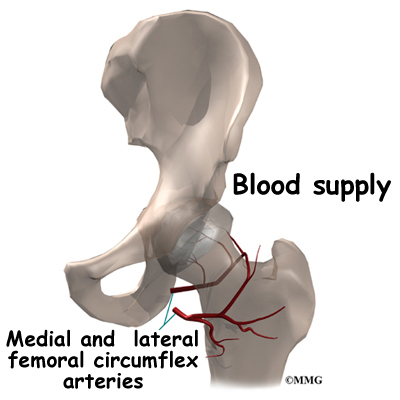
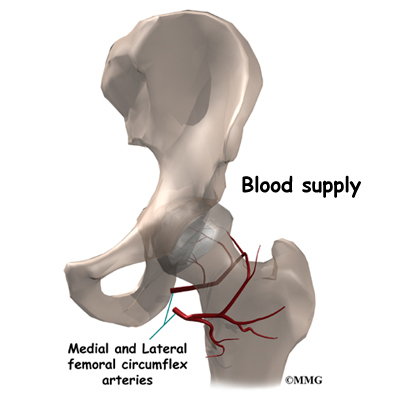
Surgeons perform this operation using several different incisions, or approaches, to the hip joint. The anterior approach from the front of the hip and the posterior approach from the back of the hip. There is no one right approach. Many surgeons prefer the posterior approach because it keeps the joint capsule intact. Keeping the joint capsule intact may reduce the risk of dislocation after the surgery and damage the blood supply less. Either approach is commonly used depending on the training and experience of the surgeon.
The operation begins by making an incision in the side of the thigh. This allows the surgeon to see both the femoral head and the acetabulum (or socket). The femoral head is then dislocated out of the socket. Special powered instruments are used to shape the bone of the femoral head so that the new metal surface will fit snugly on top of the bone.
The cap is placed over the smoothed head like a tooth capped by the dentist. The cap is held in place with a small peg that fits down into the bone. The patient must have enough healthy bone to support the cap.
The hip socket may remain unchanged but more often it is replaced with a thin metal cup. A special tool called a reamer is used to remove the cartilage from the acetabulum and shape the socket to fit the acetabular component. Once the shape is correct, the acetabular component is pressed into place in the socket. Friction holds the metal liner in place until bone grows into the holes in the surface and attaches the metal to the bone.
Complications
What could go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hip resurfacing arthroplasty surgery include
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- femoral neck fracture
- leg length inequality
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following artificial joint replacement surgery. The chance of getting an infection following hip joint resurfacing is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
Dislocation
Just like your real hip, an artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. The physical therapist will instruct you very carefully how to avoid activities and positions that may have a tendency to cause a hip dislocation. A hip that dislocates more than once may have to be revised to make it more stable. This means another operation.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Loosening
The main reason that artificial joints eventually fail continues to be the loosening of the metal or cement from the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from an artificial hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the hip.
Related Document: A Patient’s Guide to Revision Arthroplasty of the Hip
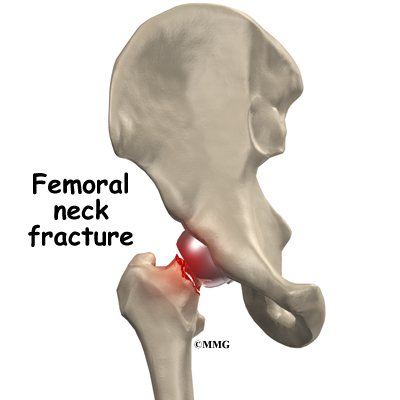
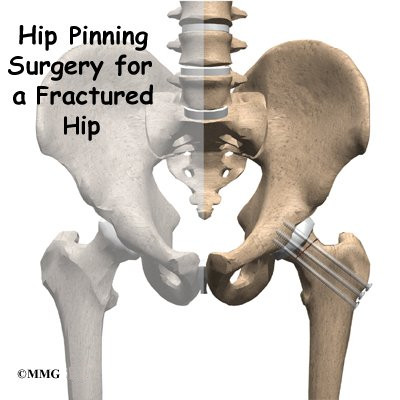
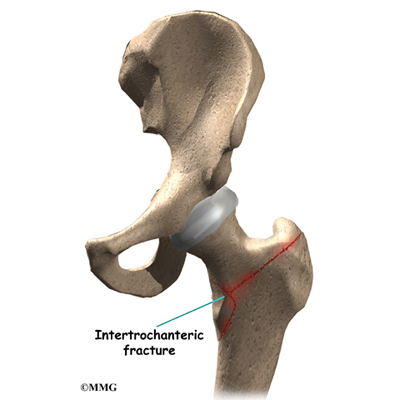
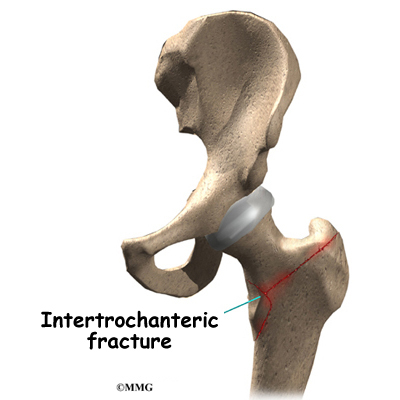
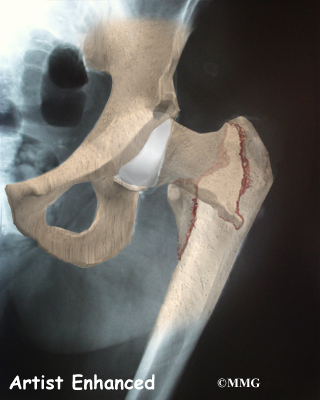
Fracture of the Femoral Neck
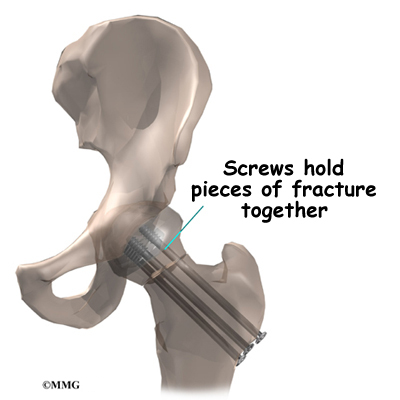
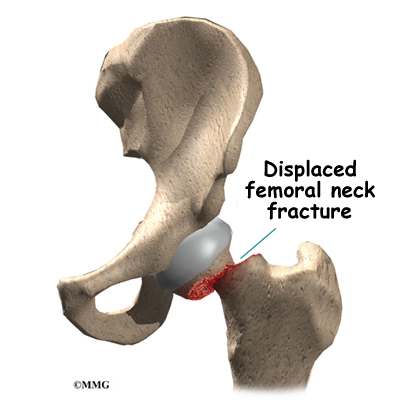
Fracture of the femoral neck is a unique complication of hip resurfacing. The replacement cap fits over the femoral head and ends just about where the femoral neck begins. This meeting point is an area of increased stress risk. Patient obesity, decreased bone mass, and surgical error are common risk factors in femoral neck fracture.
Leg Length Inequality
If there is any bone loss a difference in leg length can occur. When a surgeon does a traditional artificial hip replacement, the leg can be lengthened or shortened to match the other side. Because much less bone is removed during hip joint resurfacing, the surgeon cannot adjust the length of the leg. If you have a leg length difference before the procedure it will remain essentially the same.
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use a breathing device known as an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physical therapy treatments are scheduled one to three times each day as long as you are in the hospital. Your first session is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you’ll begin walking longer distances using your crutches. Most patients are safe to put comfortable weight down when standing or walking. However, if your surgeon used an uncemented prosthesis, you may be instructed to limit the weight you bear on your foot when you are up and walking.
Your therapist will review exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
This procedure requires the surgeon to open up the hip joint during surgery. This puts the hip at some risk for dislocation after surgery. To prevent dislocation, patients follow strict guidelines about which hip positions to avoid (called hip precautions). Your therapist will review these precautions with you during the preoperative visit and will drill you often to make sure you practice them at all times for at least six weeks. Some surgeons give the OK to discontinue the precautions after six to 12 weeks because they feel the soft tissues have gained enough strength by this time to keep the joint from dislocating.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Patients are usually able to go home after spending two to four days in the hospital. You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who still need extra care may be sent to a different hospital unit until they are safe and ready to go home.
Your staples will be removed two weeks after surgery.
Most orthopedic surgeons recommend that you have checkups on a routine basis after your joint resurfacing. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends.
Patients who have a joint implant will sometimes have episodes of pain, but if you have pain that lasts longer than a couple of weeks, you should consult your surgeon. During the examination, the orthopedic surgeon will try to determine why you are feeling pain. X-rays may be taken of your hip to compare with the ones taken earlier to see if there is any evidence of fracture or loosening.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your therapist may see you for one to six outpatient visits. This is to ensure you are safe in and about the home and workplace and getting in and out of a car. Your therapist will review your exercise program, continue working with you on your hip precautions, and make recommendations about your safety. Your therapist may use heat, ice, or electrical stimulation to reduce any swelling or pain.
You should use your crutches or cane(s) as instructed. Your surgeon may only want you to place the toes of your operated leg down for up to six weeks after surgery. You’ll advance the weight you place through your sore leg as tolerated.
Patients are usually able to drive within three weeks and walk without a walking aid by six weeks. Upon the approval of the surgeon, patients are generally able to resume sexual activity by one to two months after surgery.
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent home program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Many patients have less pain and better mobility after having hip resurfacing. Your therapist will work with you to help keep your new joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new hip joint.
There is a belief that with hip resurfacing the patient can return to full participation in recreational or professional sports. Long-term results have not been studied to support this idea. Most surgeons agree that joint resurfacing allows patients to be more active than is acceptable for a standard total hip replacement.
Although resurfacing materials are strong, they aren’t immune to wear and tear. Surgeons still advise patients to avoid high-impact activities. Heavy sports that require jogging, running, jumping, quick stopping and starting, and cutting are discouraged. Repetitive impact can strain the resurfacing, increasing the risk of loosening.
Your therapist’s goal is to help you maximize strength, weight shift evenly, walk normally, and improve your ability to do your activities. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Hip Anatomy
A Patient’s Guide to Hip Anatomy
Introduction
The hip joint is a true ball-and-socket joint. This arrangement gives the hip a large amount of motion needed for daily activities like walking, squatting, and stair-climbing.
Understanding how the different layers of the hip are built and connected can help you understand how the hip works, how it can be injured, and how challenging recovery can be when this joint is injured. The deepest layer of the hip includes the bones and the joints. The next layer is made up of the ligaments of the joint capsule. The tendons and the muscles come next.
In addition to reading this article, be sure to watch our Hip Anatomy Animated Tutorial Video.
This guide will help you understand
- the parts that make up the hip
- how these parts work together
Important Structures
The important structures of the hip can be divided into several categories. These include
- bones and joints
- ligaments and tendons
- muscles
- nerves
- blood vessels
- bursae
Bones and Joints
The bones of the hip are the femur (the thighbone) and the pelvis. The top end of the femur is shaped like a ball. This ball is called the femoral head. The femoral head fits into a round socket on the side of the pelvis. This socket is called the acetabulum.
The femoral head is attached to the rest of the femur by a short section of bone called the femoral neck. A large bump juts outward from the top of the femur, next to the femoral neck. This bump, called the greater trochanter, can be felt along the side of your hip. Large and important muscles connect to the greater trochanter. One muscle is the gluteus medius. It is a key muscle for keeping the pelvis level as you walk.
Articular cartilage is the material that covers the ends of the bones of any joint. Articular cartilage is about one-quarter of an inch thick in the large, weight-bearing joints like the hip. Articular cartilage is white and shiny and has a rubbery consistency. It is slippery, which allows the joint surfaces to slide against one another without causing any damage. The function of articular cartilage is to absorb shock and provide an extremely smooth surface to make motion easier. We have articular cartilage essentially everywhere that two bony surfaces move against one another, or articulate.
In the hip, articular cartilage covers the end of the femur and the socket portion of the acetabulum in the pelvis. The cartilage is especially thick in the back part of the socket, as this is where most of the force occurs during walking and running.
Ligaments and Tendons
There are several important ligaments in the hip. Ligaments are soft tissue structures that connect bones to bones. A joint capsule is a watertight sac that surrounds a joint. In the hip, the joint capsule is formed by a group of three strong ligaments that connect the femoral head to the acetabulum. These ligaments are the main source of stability for the hip. They help hold the hip in place.
A small ligament connects the very tip of the femoral head to the acetabulum. This ligament, called the ligamentum teres, doesn’t play a role in controlling hip movement like the main hip ligaments. It does, however, have a small artery within the ligament that brings a very small blood supply to part of the femoral head.
A long tendon band runs alongside the femur from the hip to the knee. This is the iliotibial band. It gives a connecting point for several hip muscles. A tight iliotibial band can cause hip and knee problems.
A special type of ligament forms a unique structure inside the hip called the labrum. The labrum is attached almost completely around the edge of the acetabulum. The shape and the way the labrum is attached create a deeper cup for the acetabulum socket. This small rim of cartilage can be injured and cause pain and clicking in the hip.
Muscles
The hip is surrounded by thick muscles. The gluteals make up the muscles of the buttocks on the back of the hip. The inner thigh is formed by the adductor muscles. The main action of the adductors is to pull the leg inward toward the other leg. The muscles that flex the hip are in front of the hip joint. These include the iliopsoas muscle. This deep muscle begins in the low back and pelvis and connects on the inside edge of the upper femur. Another large hip flexor is the rectus femoris. The rectus femoris is one of the quadriceps muscles, the largest group of muscles on the front of the thigh. Smaller muscles going from the pelvis to the hip help to stabilize and rotate the hip.
Finally, the hamstring muscles that run down the back of the thigh start on the bottom of the pelvis. Because the hamstrings cross the back of the hip joint on their way to the knee, they help to extend the hip, pulling it backwards.
Nerves
All of the nerves that travel down the thigh pass by the hip. The main nerves are the femoral nerve in front and the sciatic nerve in back of the hip. A smaller nerve, called the obturator nerve, also goes to the hip.
These nerves carry the signals from the brain to the muscles that move the hip. The nerves also carry signals back to the brain about sensations such as touch, pain, and temperature.
Blood Vessels
Traveling along with the nerves are the large vessels that supply the lower limb with blood. The large femoral artery begins deep within the pelvis. It passes by the front of the hip area and goes down toward the inner edge of the knee. If you place your hand on the front of your upper thigh you may be able to feel the pulsing of this large artery.
The femoral artery has a deep branch, called the profunda femoris (profunda means deep). The profunda femoris sends two vessels that go through the hip joint capsule. These vessels are the main blood supply for the femoral head. As mentioned earlier, the ligamentum teres contains a small blood vessel that gives a very small supply of blood to the top of the femoral head.
Other small vessels form within the pelvis and supply the back portion of the buttocks and hip.
Bursae
Where friction occurs between muscles, tendons, and bones there is usually a structure called a bursa. A bursa is a thin sac of tissue that contains fluid to lubricate the area and reduce friction. The bursa is a normal structure. The body will even produce a bursa in response to friction.
Think of a bursa like this. If you press your hands together and slide them against one another, you produce some friction. In fact, when your hands are cold you may rub them together briskly to create heat from the friction. Now imagine that you hold in your hands a small plastic sack that contains a few drops of salad oil. This sack would let your hands glide freely against each other without a lot of friction.
A bursa that sometimes causes problems in the hip is sandwiched between the bump on the outer hip (the greater trochanter) and the muscles and tendons that cross over the bump. This bursa, called the greater trochanteric bursa, can get irritated if the iliotibial band (discussed earlier) is tight. Another bursa sits between the iliopsoas muscle where it passes in front of the hip joint. Bursitis here is called iliopsoas bursitis. A third bursa is over the ischial tuberosity, the bump of bone in your buttocks that you sit on.>
Summary
As you can see, the hip is complex with a design that provides a good amount of stability. It allows good mobility and range of motion for doing a wide range of daily activities. Many powerful muscles connect to and cross by the hip joint, making it possible for us to accelerate quickly during actions like running and jumping.
Avascular Necrosis of the Hip
A Patient’s Guide to Avascular Necrosis of the Hip
Introduction
Bones are living tissue, and like all living tissue they rely on blood vessels to bring blood to keep them alive. Most living tissues have blood vessels that come from many directions into the tissue. If one blood vessel is damaged it may not cause problems, since there may be a backup blood supply coming in from a different direction. But certain joints of the body have only a few blood vessels that bring in blood. One of these joints is the hip. This document will describe what happens when this blood supply is damaged and results in what is called avascular necrosis (AVN) of the hip. Another name for this condition is osteonecrosis (which means “bone death”).
This guide will help you understand
- how AVN develops
- how doctors diagnose the condition
- what treatments are available
Anatomy
Where does AVN develop?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone. The thigh bone itself is called the femur, and the ball on the end is the femoral head. Thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
All of the blood supply comes into the ball that forms the hip joint through the neck of the femur (the femoral neck), a thinner area of bone that connects the ball to the shaft. If this blood supply is damaged, there is no backup. Damage to the blood supply can cause death of the bone that makes up the ball portion of the femur. Once this occurs, the bone is no longer able to maintain itself.
Living bone is always changing. To maintain a bone’s strength, bone cells are constantly repairing the wear and tear that affects the bone tissue. If this process stops the bone can begin to weaken, just like rust can affect the metal structure of a bridge. Eventually, just like a rusty bridge, the bone structure begins to collapse.
When AVN occurs in the hip joint, the top of the femoral head (the ball portion) collapses and begins to flatten. This occurs because this is where most of the weight is concentrated. The flattening creates a situation where the ball no longer fits perfectly inside the socket. Like two pieces of a mismatched piece of machinery, the joint begins to wear itself out. This leads to osteoarthritis of the hip joint, and pain.
Related Document: A Patient’s Guide to Osteoarthritis of the Hip
Related Document: A Patient’s Guide to Hip Anatomy
Causes
Why do I have this problem?
There are many causes of AVN. Anything that damages the blood supply to the hip can cause AVN.
Injury to the hip itself can damage the blood vessels. Fractures of the femoral neck (the area connecting the ball of the hip joint) can damage the blood vessels. A dislocation of the hip out of the socket can tear the blood vessels. It usually takes several months for AVN to show up, and it can even become a problem up to two years following this type of injury.
Some medications are known to cause AVN. Corticosteroids (cortisone) such as prednisone or methylprednisolone are the most common drugs known to lead to AVN. This is usually only a problem in patients who must take cortisone every day due to other diseases, such as advanced arthritis, or to prevent rejection of an organ transplant.
Sometimes there is no choice, and cortisone has to be prescribed to treat a condition, knowing full well that AVN could occur. AVN has not been proven to be caused by local injection with cortisone, such as one or two injections into joints to treat arthritis or bursitis. But some patients have developed AVN within the first month of taking these drugs orally (pills by mouth). Patients taking both corticosteroids and statin drugs (cholesterol-lowering medications) seem to have the greatest risk for developing femoral head osteonecrosis.
A clear link exists between AVN and lifestyle choices such as smoking and alcohol abuse . Smoking causes blood vessels to constrict or narrow thereby limiting the amount of blood flow to an area such as the hip with its already limited backup supply. Excessive alcohol intake somehow damages the blood vessels and leads to AVN. Deep sea divers and miners who work under great atmospheric pressures also are at risk for damage to the blood vessels. The pressure causes tiny bubbles to form in the blood stream which can block the blood vessels to the hip, damaging the blood supply.
Then there is a long list of other diseases and conditions that are associated with increased incidence of femoral head osteonecrosis. These are referred to as nontraumatic causes. For example, there is a link between osteonecrosis and more commonly known problems like leukemia, sickle cell diseases, and HIV infection and less well-known diseases such as Gaucher disease, hyperuricemia (a condition commonly called “gout”), and Caisson’s disease.
Symptoms
What does AVN feel like?
The first symptom of AVN is pain when weight is placed on the hip. The pain can be felt in the groin area, the buttock area, and down the front of the thigh. As the problem progresses, the symptoms include development of a limp when walking and stiffness in the hip joint. Eventually, the pain will also be present at rest and may even interfere with sleep.
Diagnosis
How do doctors identify the condition?
The diagnosis of AVN begins with a history and physical examination. Your doctor will want to know about your occupation, what other medical problems you have, and your medication use. You’ll be asked whether you drink alcohol. A physical examination will be done to determine how much stiffness you have in the hip and whether you have a limp. Once this is done, X-rays will most likely be ordered.
X-rays will usually show AVN if it has been present for long enough. In the very early stages, it may not show up on X-rays even though you are having pain. In the advanced stages, the hip joint will be very arthritic, and it may be hard to tell whether the main problem is AVN or advanced osteoarthritis of the hip. Either way, the treatment is basically the same.
If the X-rays fail to show AVN, you may have a bone scan done to determine if the pain in your hip is coming from early AVN. A bone scan involves injecting tracers into your blood stream. Several hours later, a large camera is used to take a picture of the bone around the hip joint. If there is no blood supply to the femoral head, the picture will show a blank spot where the femoral head should be outlined on the film.
The bone scan has pretty much been replaced with magnetic resonance imaging (MRI) today. The MRI scan is probably the most common test used to look for AVN of the hip. The MRI scanner uses magnetic waves instead of radiation. Multiple pictures of the hip bones are taken by the MRI scanner. The images look like slices of the bones. The MRI scan is very sensitive and can show even small areas of damage to the blood supply of the hip, even just hours after the damage has occurred.
Your surgeon will use these imaging studies in order to plan the best treatment approach for you. He or she will look at where the damage has occurred, the size of any lesions, whether or not there has been any collapse of the bone, and if any arthritic changes have developed. Based on these findings, the condition will be classified as either mild, moderate, or severe.
Treatment
What can be done for the condition?
Once AVN has occurred, the treatment choices are determined by how far along the problem is and your symptoms. Other factors that guide treatment decisions include your age, activity level, general health (and any specific health problems present), and life expectancy. For example, patients with other serious health problems or with a limited life expectancy might be treated with nonoperative care. While the symptoms may be reduced with pain medications and anti-inflammatory medications, no medical treatments will restore the blood supply to the femoral head and reverse the AVN.
Nonsurgical Treatment
If AVN is caught early, keeping weight off the sore-side foot when standing and walking may be helpful. Patients are shown how to use a walker or crutches to protect the hip. The idea is to permit healing and to prevent further damage to the hip. Patients may be shown stretches to avoid a loss of range of motion in the hip.
Anti-inflammatory medicine is often used to ease pain. Bisphosphonates are another group of medications that can be helpful. One particular bisphosphonate (Fosamax normally used for the treatment of osteoporosis) has been shown effective in reducing the risk of femoral head collapse in patients with avascular necrosis. In some cases, surgeons also prescribe biophysical treatment modalities such as electrical stimulation or shock wave therapy in an attempt to get the bone to heal. Sometimes these measures may help delay the need for surgery, but they rarely reverse the problem.
Surgery
If the femoral head has not begun to collapse, your surgeon may suggest an operation to try to increase the blood supply to the femoral head. Several operations have been designed to do this.
Decompressing the Femoral Head
The simplest operation is to drill one or several holes through the femoral neck and into the femoral head, trying to reach the area that lacks blood supply. The drill bores out a plug of bone within the femoral head. This operation is thought to do two things: (1) it creates a channel for new blood vessels to quickly form into the area that lacks blood supply, and (2) it relieves some of the pressure inside the bone of the femoral head. Relieving this pressure seems to help decrease the pain patients experience from AVN.
Decompression is often accompanied by the use of bone grafts with or without growth factors, a procedure designed to stimulate bone growth at the site of the defect. The donated bone comes from the patient (taken from the pelvic bone or lower leg). The bone is crushed up into tiny pieces and applied to the hole or defect caused by the necrotic process.
The decompression operation (with or without bone grafting) is done through a very small incision in the side of the thigh. The surgeon watches on a fluoroscope as a drill is used. A fluoroscope is a type of X-ray that shows the bones on a TV screen. The surgeon uses the fluoroscope to guide the drill where it needs to go. This operation is usually done as an outpatient procedure, and you will be able to go home with crutches the same day.
Fibular Bone Graft
A more complicated procedure to try to increase the blood supply to the femoral head is a vascularized fibular bone graft procedure. This is actually a tissue transplant. The graft is taken from the fibula (the thin bone that runs next to the shin bone). The graft is vascularized, meaning it has a blood supply of its own. Because it supports the femoral head, the graft is also referred to as a strut graft.
The surgeon removes a piece of the small bone in your lower leg (the fibula) along with the blood vessels to the bone. The surgeon then drills a hole through the side of the femur and into the femoral head. The surgeon attaches the blood vessels from the fibula to one of the blood vessels around the hip. This creates instant blood flow into the bone graft and into the head of the femur. This operation does two things: (1) it brings blood flow to the femoral head through the bone graft, and (2) the fibular bone graft is strong and keeps the femoral head from collapsing as the bone heals itself. This procedure is an inpatient procedure and will require you to stay in the hospital for several days.
This is a very complicated operation and is not commonly done. It is not always successful because the blood supply to the graft is fragile and may not form completely.
Rotational Osteotomy
In cases of small lesions involving less than one-third of the surface of the femoral head, rotational osteotomy has been very successful. The procedure involves making a cut through the bone and turning the head of the femur so that the necrotic bone is no longer bearing any weight.
Artificial Hip Replacement
When AVN is in the advanced stages, the condition is no different from osteoarthritis of the hip joint. Your surgeon will probably recommend replacing the hip with an artificial hip joint. For those patients with a limited bone defect that only affects the femoral head and does not extend into the hip socket, a resurfacing procedure might be considered. Hip resurfacing arthroplasty is a type of hip replacement that replaces the arthritic surface of the joint but removes far less bone than the traditional total hip replacement.
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Hip
Related Document: A Patient’s Guide to Hip Resurfacing Arthroplasty
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
You may work with a physical therapist who will show you ways to safely move and stretch your hip. The goal is to keep your hip mobile and to avoid losing range of motion. Your therapist will also instruct you to use a walker or crutches. Keeping weight off your hip while you are standing or walking may help the bone to heal while protecting the femur from further damage.
After Surgery
After a simple drilling operation, you will probably use crutches for six weeks or so. The drill holes weaken the bone around the hip, making it possible to fracture the hip. Using crutches allows the bone to heal safely and reduce the risk that you may fracture your hip. Patients who have had bone and blood vessels grafted are required to limit how much weight they place on the hip for up to six months.
When you are safe in putting full weight through the leg, your doctor may have you work with a physical therapist to help regain hip range of motion and strength.
Patients who require hip resurfacing or artificial hip joint replacement follow a structured program of physical therapy beginning shortly after surgery.
Trochanteric Bursitis of the Hip
A Patient’s Guide to Trochanteric Bursitis of the Hip
Introduction
A common spot for bursitis is on the side of the hip. Here a large tendon passes over the bony bump on the side of the hip. The bony bump is called the greater trochanter. Inflammation in the bursa between the tendon and the greater trochanter is called trochanteric bursitis. This problem is common in older individuals. It may also occur in younger patients who are extremely active in exercises such as walking, running, or biking.
- how trochanteric bursitis develops
- how doctors diagnose the condition
- what treatments are available
Anatomy
Where is the trochanteric bursa, and what does it do?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone (femur), or femoral head. Thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
The greater trochanter is the large bump on the outside of the upper end of the femur. This bump is the point where the large buttock muscles that move the hip connect to the femur. The gluteus maximus is the largest of these muscles. It attaches lower down on the femur.
Where friction occurs between muscles, tendons, and bones, there is usually a structure called a bursa. A bursa is a thin sac of tissue that contains fluid to lubricate the area and reduce friction. The bursa is a normal structure. The body will even produce a bursa in response to friction.
Related Document: A Patient’s Guide to Hip Anatomy
Causes
Why do I have this problem?
Sometimes a bursa can become inflamed (swollen and irritated) because of too much friction or because of an injury to the bursa. An inflamed bursa can cause pain because movement makes the structures around the bursa rub against it.
Friction can build in the bursa during walking if the long tendon on the side of the thigh is tight. It is unclear what causes this tightening of the tendon. The gluteus maximus attaches to this long tendon. As you walk, the gluteus maximus pulls this tendon over the greater trochanter with each step. When the tendon is tight, it rubs against the bursa. The rubbing causes friction to build in the bursa, leading to irritation and inflammation. Friction can also start if the outer hip muscle (gluteus medius) is weak, if one leg is longer than the other, or if you run on banked (slanted) surfaces.
View animation of rubbing on the bursa
Most cases of trochanteric bursitis appear gradually with no obvious underlying injury or cause. Trochanteric bursitis can occur after artificial replacement of the hip joint or other types of hip surgery. The cause may be a combination of changes in the way the hip works, the way it is aligned, or the way scar tissue has formed from the healing incision.
A fall on the hip can cause bleeding into the bursa, forming a hematoma. The bleeding is not serious, but the bursa may react to the blood by becoming inflamed. The inflammation causes the bursa to become thickened over time. This thickening, constant irritation, and inflammation may result in the condition becoming chronic, or long lasting.
Symptoms
What does the condition feel like?
The first symptom of trochanteric bursitis is usually pain. The pain can be felt in the area of the hip right over the bump that forms the greater trochanter. Eventually the pain may radiate down the outside of the thigh. As the problem progresses, the symptoms produce a limp when walking and stiffness in the hip joint. Eventually, the pain will also be present at rest and may even cause a problem with sleeping.
Diagnosis
How do doctors identify the problem?
The diagnosis of trochanteric bursitis begins with a history and physical examination. This is usually all that is necessary to make the diagnosis. Your doctor will want to know when the pain began and which motions cause the pain. A physical examination will be done to determine how much stiffness you have in the hip and if you have a limp. Once this is done, X-rays will most likely be ordered to make sure that there are no other abnormalities in the hip.
X-rays will usually not show trochanteric bursitis. If X-rays are suggested they are to rule out other problems that may be causing your hip pain. Sometimes it is difficult to tell whether the pain you are suffering is from trochanteric bursitis or underlying arthritis of the hip joint. An X-ray may give more information about the condition of the hip joint itself.
Related Document: A Patient’s Guide to Osteoarthritis of the Hip
An injection of a local anesthetic into the bursa can help your doctor diagnose trochanteric bursitis. If the injection removes the pain immediately, then the diagnosis is probably trochanteric bursitis. Most physicians will also add a bit of cortisone medication to the novocaine to help treat the condition at the same time.
Treatment
What can be done for the condition?
The treatment of trochanteric bursitis usually begins with simple measures. Treatment becomes more involved if simple measures fail. The vast majority of patients with trochanteric bursitis will never require surgery.
Nonsurgical Treatment
Trochanteric bursitis is often treated successfully without surgery. Younger patients who have this condition because of overuse can usually be treated by reducing their activities or changing the way they do their activities. Combining this with an exercise program of stretching and strengthening and perhaps a brief course of anti-inflammatory medications will usually resolve the problem.
Your doctor may also prescribe sessions with a physical therapist. Treatments are used to calm inflammation and may include heat or ice applications. Therapists use hands-on treatment and stretching to help restore full hip range of motion. Improving strength and coordination in the buttock and hip muscles also enables the femur to move in the socket smoothly and can help reduce friction on the bursa. You may need therapy treatments for four to six weeks before full motion and function return.
If rehabilitation fails to reduce your symptoms, an injection of cortisone into the bursa may ease your symptoms and give temporary relief of the condition. Cortisone is a powerful anti-inflammatory medication. It can reduce swelling and pain when injected directly into the bursa. The injection will probably not cure the problem. But it may control the symptoms for months.
Surgery
Surgery is rarely needed to treat trochanteric bursitis. When all else fails and the pain is disabling, your doctor may recommend surgery. Several types of surgical procedures are available to treat trochanteric bursitis.
The primary goal of all procedures designed to treat this condition is to remove the thickened bursa, to remove any bone spurs that may have formed on the greater trochanter, and to relax the large tendon of the gluteus maximus. Some surgeons prefer to simply lengthen the tendon a bit, and some prefer to remove a section of the tendon that rubs directly on the greater trochanter. Both procedures give good results.
Related Document: A Patient’s Guide to Trochanteric Bursitis Surgery
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
Even if you don’t need surgery, you may need to follow a program of rehabilitation exercises. Your doctor may recommend that you work with a physical therapist. Your therapist can create a program of stretching and strengthening for your hip. It is very important to maintain a balance of flexibility and strength of the hip. You will probably progress to a home program within four to six weeks.
After Surgery
If you have surgery, your hip will be bandaged with a well-padded dressing. Physical therapy sessions may be needed for up to two months after surgery. The first few treatment sessions will focus on controlling the pain and swelling after surgery. You will then begin exercises that gradually stretch and strengthen the muscles around the hip joint. Your therapist will help you retrain these muscles to keep the ball of the femur moving smoothly in the socket. Your therapist will give you tips on ways to do your activities without straining the hip joint.
Hip Arthritis
A Patient’s Guide to Osteoarthritis of the Hip
Introduction
Osteoarthritis (OA) is a common problem for many people after middle age. OA is sometimes referred to as degenerative, or wear-and-tear, arthritis. OA commonly affects the hip joint. In the past, little was done for the condition. Now doctors have many ways to treat hip OA so patients have less pain, better movement, and improved quality of life.
This guide will help you understand
- how OA develops in the hip
- how doctors diagnose the condition
- what can be done for your pain
Anatomy
Which part of the hip does OA affect?
Articular cartilage is the smooth lining that covers the surfaces of the ball-and-socket joint of the hip. The cartilage gives the joint freedom of movement by decreasing friction. The layer of bone just below the articular cartilage is called subchondral bone. The main problem in OA is degeneration of the articular cartilage.
When the articular cartilage degenerates, or wears away, the subchondral bone is uncovered and rubs against bone. Small outgrowths called bone spurs or osteophytes may form in the joint.
Related Document: A Patient’s Guide to Hip Anatomy
Causes
How does OA develop?
OA of the hip can be caused by a hip injury earlier in life. Changes in the movement and alignment of the hip eventually lead to wear and tear on the joint surfaces. The alignment of the hip can be altered from a fracture in the bones around or inside the hip. If the fracture changes the alignment of the hip, this can lead to excessive wear and tear, just like the out-of-balance tire that wears out too soon on your car. Cartilage injuries, infection, or bleeding within the joint can also damage the joint surface of the hip.
Not all cases of OA are related to alignment problems or a prior injury, however. Scientists believe genetics makes some people prone to developing OA in the hip.
Scientists also believe that problems in the subchondral bone may trigger changes in the articular cartilage. As mentioned, the subchondral bone is the layer of bone just beneath the articular cartilage. Normally, the articular cartilage protects the subchondral bone. But some medical conditions can make the subchondral bone too hard or too soft, changing how the cartilage normally cushions and absorbs shock in the joint.
Avascular necrosis (AVN) is another cause of degeneration of the hip joint. In this condition, the femoral head (the ball portion of the hip) loses a portion of its blood supply and actually dies. This leads to collapse of the femoral head and degeneration of the joint. AVN has been linked to alcoholism, fractures and dislocations of the hip, and long-term cortisone treatment for other diseases.
Related Document: A Patient’s Guide to Avascular Necrosis of the Hip
Symptoms
What does OA of the hip joint feel like?
The symptoms of hip OA usually begin as pain while putting weight on the affected hip. You may limp, which is the body’s way of reducing the amount of force that the hip has to deal with. The changes that happen with OA cause the affected hip to feel stiff and tight due to a loss in its range of motion. Bone spurs will usually develop, which can also limit how far the hip can move. Finally, as the condition becomes worse, pain may be present all the time and may even keep you awake at night.
Diagnosis
How do doctors identify the problem?
The diagnosis of hip OA starts with a complete history and physical examination by your doctor. X-rays will be required to determine the extent of the cartilage damage and suggest a possible cause for it.
Other tests may be required if there is reason to believe that other conditions are contributing to the degenerative process. Magnetic resonance imaging (MRI) may be necessary to determine whether your hip condition is from problems with AVN.
Blood tests may be required to rule out systemic arthritis or infection in the hip.
Treatment
What can be done for the condition?
Nonsurgical Treatment
OA can’t be cured, but therapies are available to ease symptoms and to slow down the degeneration of the joint. Recent information shows that your condition may be maintained and in some cases improved.
Your physician may prescribe medicine to help control your pain. Acetaminophen (Tylenol) is a mild pain reliever with few side effects. Some people may also get relief of pain with anti-inflammatory medication, such as ibuprofen and aspirin. Newer anti-inflammatory medicines called COX-2 inhibitors show promising results and seem not to cause as much stomach upset or other intestinal problems.
Medical studies have shown that glucosamine and chondroitin sulfate can also help people with OA. These supplements seem to have nearly the same benefits as anti-inflammatory medicine with fewer side affects. Many doctors feel the research supports these supplements and are encouraging their patients to use them.
If you aren’t able to get your symptoms under control, a cortisone injection may be prescribed. Cortisone is a powerful anti-inflammatory medication, but it has secondary effects that limit its usefulness in the treatment of OA. Multiple injections of cortisone may actually speed up the process of degeneration.
Repeated injections also increase the risk of developing a hip joint infection, called septic arthritis. Any time a joint is entered with a needle, there is the possibility of an infection. Most physicians use cortisone sparingly, and avoid multiple injections unless the joint is already in the end stages of degeneration and the next step is an artificial hip replacement.
Physical therapy plays a critical role in the nonsurgical treatment of hip OA. A primary goal is to help you learn how to control symptoms and maximize the health of your hip. You will learn ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs. A cane or walker may be needed to ease pressure when walking. Range-of-motion and stretching exercises will be used to improve hip motion. You will be shown strengthening exercises for the hip to steady the joint and protect it from shock and stress. Your therapist can suggest tips for getting your tasks done with less strain on the joint.
Surgery
In some cases, surgical treatment of OA may be appropriate.
Arthroscopy
Surgeons can use an arthroscope to check the condition of the articular cartilage in a joint. An arthroscope is a miniature TV camera inserted into the joint though a small incision. While checking the condition of the cartilage, your surgeon may try a few different techniques to give you relief from pain. One method involves cleaning the joint by removing loose fragments of cartilage. Another method involves simply flushing the joint with a saline solution, after which some patients report relief.
This procedure is sometimes helpful for temporary relief of symptoms. Hip arthroscopy is relatively new, and it is unclear at this time which patients will benefit.
Osteotomy
When the alignment of the hip joint is altered from disease or trauma, more pressure than normal is placed on the surfaces of the joint. This extra pressure leads to more pain and faster degeneration of the joint surfaces.
In some cases, surgery to realign the angles of the pelvic socket or femur (thighbone) can result in shifting pressure to the other healthier parts of the hip joint. The goal is to spread the forces over a larger surface in the hip joint. This can help ease pain and delay further degeneration.
The procedure to realign the angles in the joint is called osteotomy. In this procedure, the bone of either the pelvic socket or femur is cut, and the angle of the joint is changed. The procedure is not always successful. Generally it will reduce your pain but not eliminate it altogether. The advantage to this approach is that very active people still have their own hip joint, and once the bone heals, there are fewer restrictions in activity levels.
An osteotomy procedure in the best of circumstances is probably only temporary. It is thought that this operation buys some time before a total hip replacement becomes necessary.
Artificial Hip Replacement
An artificial hip replacement is the ultimate solution for advanced hip OA. Surgeons prefer not to put a new hip joint in patients less than 60 years old. This is because younger patients are generally more active and might put too much stress on the joint, causing it to loosen or even crack. A revision surgery to replace a damaged joint is harder to do, has more possible complications, and is usually less successful than a first-time joint replacement surgery.
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Hip
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Nonsurgical rehabilitation of hip OA is used to maximize the health of your hip and to prolong the time before any type of surgery is necessary. If you attend physical therapy as part of nonsurgical rehabilitation, you will probably progress to a home program within two to four weeks.
In cases of advanced OA where surgery is called for, patients may see a physical therapist before surgery to discuss exercises, special precautions to be followed just after surgery, and to practice walking with crutches or a walker.
After Surgery
Shortly after surgery, your physical therapist will see you in your hospital room. You’ll practice getting out of bed and walking using your walker or a pair of crutches. Exercises are used to improve muscle tone and strength in the hip and thigh muscles and to help prevent the formation of blood clots.
During your recovery, you should follow your surgeon’s instructions about how much weight you can put down while standing or walking. After you return home from the hospital, your surgeon may have you work with a physical therapist for up to six in-home visits.
These visits are to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review special hip precautions and make sure you are placing a safe amount of weight on your foot when standing or walking. Home therapy visits end when you are safe to get out of the house.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
A few additional visits in outpatient physical therapy may be needed for patients who still have problems walking or who need to get back to physically heavy work or activities.
The therapist’s goal is to help you maximize hip strength, restore a normal walking pattern, and do your activities without risking further injury to your hip. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Hip Pinning Surgery for a Fractured Hip
A Patient’s Guide to Hip Pinning Surgery for a Fractured Hip
Introduction
A fractured hip can be a life-threatening problem. The hip fracture isn’t usually a difficult problem to treat with surgery. But once the fracture occurs, it brings with it all the potential medical complications that can arise when aging adults are confined to bed. The goal of treatment is to get patients moving as quickly as possible after surgery. Surgery to pin the broken ends of the fracture together is fairly simple and allows patients to get up and begin moving shortly after surgery.
This guide will help you understand
- what the surgeon hopes to achieve
- what happens during the procedure
- what to expect as you recover
Anatomy
How is the hip designed?
The femur is the large bone of the thigh. The ball-shaped femoral head on the end of the femur fits into a socket in the pelvis called the acetabulum. The femoral neck is a thinner part of the femur. It is the short section of bone that connects the femoral head to the main shaft of the bone. The bump on the outside of the femur just below the femoral neck is called the greater trochanter. This is where the large muscles of the buttock attach to the femur.
Hip fractures in aging adults happen either in the femoral neck or the intertrochanteric area. Fractures occur at about the same frequency for both areas.
Related Document: A Patient’s Guide to Hip Anatomy
Related Document: A Patient’s Guide to Hip Fractures
Rationale
What does the surgeon hope to achieve?
Fixing the broken ends of the hip with metal pins or screws is a fairly simple procedure. The procedure requires only a small incision on the side of the hip, and the pins and screws usually provide a solid connection for the broken bones. Patients are able to move right away after surgery, so they are more likely to avoid the serious complications that can arise with being immobilized in bed.
Most hip fractures would actually heal without surgery, but the problem is that the patient would be in bed for eight to 12 weeks. Surgeons have learned over the years that confining an aging adult to bed for this period of time has a far greater risk of creating serious complications than the surgery required to fix a broken hip. The goal of the hip pinning procedure is to set the bones securely in place, allowing the patient to get out of bed as soon as possible.
The hip pinning procedure is used successfully after most fractures within the femoral neck. When the fractured bones have displaced, however, surgeons do not all agree that the hip pinning procedure is the best choice. This is because displaced fractures can damage the blood supply going to the femoral head, leading to avascular necrosis (AVN), a condition that causes the bone of the femoral head to die. With displaced fractures, the risk of developing AVN is so high that some surgeons may suggest not fixing the fracture but instead removing the femoral head and replacing it with an artificial replacement, or prosthesis. This is suggested because pinning the fracture carries a high chance that you will need a second operation several months later if the femoral head dies due to AVN.
Related Document: A Patient’s Guide to Avascular Necrosis of the Hip
Preparation
How should I prepare for surgery?
The hip pinning procedure is usually an emergency surgery, so it is unlikely that you will have had time to plan and prepare. Ideally a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital.
The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, make sure you have needed supplies, and set up follow-up appointments with your surgeon, doctor, and physical therapist.
Surgical Procedure
What happens during the operation?
The operation can be done using either a general anesthetic (one that puts you to sleep) or a spinal block. The spinal block puts your body to sleep from the waist down. With a spinal block, the anesthesiologist will also give you medications so that you won’t be aware the operation is being done.
Once you have anesthesia, your surgeon will make sure the skin of your hip is free of infection by cleaning the skin with a germ-killing solution.
With the patient lying flat on a special table, the foot and leg are supported. Tension is applied to get the fractured bones to line up. The surgeon checks the alignment using a fluoroscope, a type of X-ray machine that shows the image on a TV screen.
A small incision is made on the side of the thigh. The surgeon uses the fluoroscope to guide the metal screws or pins into the correct position to hold the bones together. The fluoroscope allows the surgeon to see the X-ray image of the hip while the screws are placed through the femoral neck.
The soft tissues are put back in place, and metal staples or sutures are used to close the incision.
Complications
What might go wrong?
The main complications after a hip fracture sometimes develop as a result of being immobilized in bed. These may include pneumonia, bedsores, and mental confusion.
Complications that can result from the hip pinning surgery itself include
- anesthesia complications
- thrombophlebitis
- infection
- nerve or blood vessel injury
- avascular necrosis of the femoral head
- nonunion of the bones
This is not intended to be a complete list of possible complications.
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Any surgery carries the risk of infection. You will probably be given antibiotics before the procedure to reduce the risk. If you get an infection, you will need more antibiotics. If the areas around the metal pins or screws become infected, you may need surgery to drain the infection.
Nerve or Blood Vessel Injury
Several nerves and blood vessels travel in the area where the surgery is performed. It is possible to injure either the nerves or the blood vessels during surgery, but this is extremely unlikely during this type of surgery. Nerve problems may well be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to either the nerves or the blood vessels, but it is possible.
Avascular Necrosis (AVN)
As described earlier, all of the blood supply comes into the ball that forms the hip joint through the neck of the femur bone. If this blood supply is damaged, there is no backup. Damage to the blood supply can lead to the bone that makes up the ball portion of the femur actually dying. Once this occurs, the bone is no longer able to maintain itself. When the neck of the femur fractures, the blood supply may be damaged, leading to problems with avascular necrosis. The risk of AVN is much higher when the fracture causes a large displacement in the bones. AVN can show up as late as two years after the surgery.
Nonunion
Sometimes the bones do not bond together as planned. This is called a nonunion, or pseudarthrosis. This condition requires another operation to add more fixation or actually replace the head of the femur, a procedure called hemiarthroplasty.
Related Document: A Patient’s Guide to Hemiarthroplasty of the Hip
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. If your surgeon used a general anesthesia, a nurse or respiratory therapist will guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
A physical therapist will direct your recovery after surgery. You’ll be encouraged to move from your hospital bed to a chair several times the first day after surgery. You’ll be encouraged to begin getting up and walking with your crutches or walker but may need to keep from placing too much weight on your foot while you stand or walk. You’ll be safe to go home when you can get up and move about safely with your walker or crutches, you are able to do your exercises, and your caregiver has made all the needed preparations for you to go home.
After surgery, you should keep the dressing on your hip until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery. You should support your outer hip with a pillow when you sit or recline.
Rehabilitation
What should I expect during my recovery?
Once discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on walking and strength. In some cases you may require additional visits at home before beginning outpatient physical therapy. Home therapy visits end when you are safe to get out of the house.
Additional outpatient physical therapy visits are sometimes needed for patients who still have problems walking or who need to get back to physically heavy work or activities.
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, and thigh. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
The therapist’s goal is to help you maximize hip range of motion and strength, restore a normal walking pattern, and do your activities without risking further injury to the hip. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Revision Arthroplasty of the Hip
A Patient’s Guide to Revision Arthroplasty of the Hip
Introduction
Over the past 30 years, artificial hip replacements have become increasingly common. Millions of people have gotten a new hip joint. The first time a joint is replaced with an artificial joint, the operation is called a primary joint replacement. As people live longer and more people receive artificial joints, some of those joints begin to wear out and fail. When an artificial hip joint fails, a second operation is required to replace the failing joint. This procedure is called a revision arthroplasty.
This guide will help you understand
- why revision surgery becomes necessary
- what happens during the operation
- what to expect during your recovery
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Hip
Anatomy
How is the hip designed?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone, or femoral head. Thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
Why do revisions become necessary?
The most common reasons that a revision needs to be done are
- mechanical loosening
- infection in the joint
- fracture of the bone around the joint
- instability of the implant
- wear of one or more parts of the implant
- breakage of the implant
Mechanical Loosening
Mechanical loosening means that for some reason (other than infection) the attachment between the artificial joint and the bone has become loose. There are many reasons why this can occur. It may be that, given enough time, all artificial joints will eventually become loose. This is one reason that surgeons like to wait until absolutely necessary to put in an artificial joint. The younger you are when an artificial joint is put in, the more likely it is that the joint will loosen and require a revision. Mechanical loosening can occur in cemented or uncemented artificial joints. (The different types of joints are described later.)
Infection
If an artificial joint becomes infected, it may become stiff and painful. It may also begin to lose its attachment to the bone. An infected artificial joint will probably have to be revised to try to cure the infection. In the hip joint, an infected artificial joint may be able to be exchanged for a new artificial joint at the same operation. You will still need to be placed on antibiotics for several weeks or months after the exchange operation.
Fractures
A fracture may occur near an artificial joint. It is sometimes necessary to use a new artificial joint to fix the fracture. For example, if the femur (thighbone) breaks right below the stem of an artificial hip, it may be easier to replace the femoral part of the artificial joint with a new joint with a longer stem to hold the fracture together while it heals, similar to fixing the fracture with a metal rod.
Instability
Instability means that the joint dislocates (the metal ball slips out of the plastic socket). This is very painful when it happens. If it happens more than once, it’s time to consider revising the artificial hip joint to keep it from coming out of joint.
Wear
As surgeons have become better at understanding how to put in an artificial joint so that it does not loosen as fast, we have begun to see actual wear of the plastic parts of the artificial joints. In some cases, if the wear is discovered in time, the revision may only require changing the plastic part of the artificial joint. If the wear continues until metal is rubbing on metal, the whole joint may need to be replaced.
Breakage
Finally, another type of wear can occur that breaks the metal due to the constant stress that the artificial joint undergoes everyday. In weight-bearing joints such as the hip, this is greatly affected by how much you weigh and how active you are.
Preparations
What happens before surgery?
Your surgeon will carefully plan the revision operation. Before the operation, many possible options and complications will have to be taken into account. Your surgeon will discuss these with you. Be sure to ask if there are parts of the procedure, your recovery, or the risks associated with a revision joint replacement that you have questions about.
Once the decision to proceed with surgery is made, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation.
You may be scheduled for a bone scan so the surgeon can check for loosening of the artificial joint. When an artificial joint is loose, the bone around the artificial joint reacts by trying to form new bone, a process called remodeling. The bone scan is done by injecting you with a weak radioactive chemical. Several hours later, a large camera is used to take a picture of the bone around the artificial joint. If the artificial joint is loose and there is remodeling going on, the picture will show a hot spot where the chemical has been added to the newly forming bone. The brighter the hot spot, the more likely that the artificial joint is loose.
If your surgeon suspects that the artificial hip joint is loose, other tests may be necessary to find out why the hip joint is loose. Before any plans are made to revise the artificial joint, most orthopedic surgeons will want to make sure that the hip is not loose due to infection. Your surgeon may order blood tests to look for signs of infection and may suggest placing a needle into the joint and removing fluid to send to the laboratory and check for infection. Replacing any artificial joint that is infected is much more involved than replacing a noninfected, loose artificial joint. In some cases, infection will make a revision impossible.
You may also need to spend time with the physical therapist who will manage your rehabilitation after the surgery. The therapist will begin the teaching process before surgery to ensure that you are ready for rehabilitation afterwards. One purpose of the preoperative visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the movement and strength of each hip.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will begin to practice some of the exercises you will use just after surgery. You will also be trained in the use of either a walker or crutches.
This surgery requires the surgeon to open up the hip joint to revise the artificial replacement. This puts the hip at some risk for dislocation after surgery. To prevent dislocating their hip, patients follow strict guidelines about which hip positions they are to avoid, called hip precautions. Your therapist will go over these precautions with you in the preoperative visit and will drill you often to make sure you practice them at all times for six to 12 weeks after surgery.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Finally, the physical therapist will assess any needs you may have at home once you’re released from the hospital.
You may be asked to donate some of your own blood before the operation. This blood can be donated three to five weeks earlier. Your body will make new blood cells to replace the loss. If you need to have a blood transfusion during the operation, you will receive your own blood back from the blood bank.
Surgical Procedure
What happens during the operation?
Before describing the revision procedure, let’s look at the revision prosthesis itself.
The Revision Prosthesis
There are two major types of revision implants:
- cemented prosthesis
- uncemented prosthesis
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis has a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
Both are widely used in revision hip surgery. In some cases, a combination of the two types is used in which the ball portion of the prosthesis is cemented into place, and the socket not cemented. The decision about whether to use a cemented or uncemented prosthesis during the revision surgery is usually made by the surgeon based on your age, your lifestyle, and the surgeon’s experience.
Each prosthesis is made of two main parts. The acetabular component (socket) replaces the acetabulum. The acetabular component is made of a metal shell with a plastic inner liner that provides the bearing surface. The plastic used is very tough and slick, so tough and slick that you could ice skate on a sheet of the plastic without damaging it much.
A special type of acetabular component may be used during the revision surgery. This is because the bone of the pelvis may have worn away somewhat since the initial replacement was done. The bone may be weaker, or areas of the bone may be missing. These special components are designed to spread the weight across a wider area on the acetabulum. They attach to the stronger bone outside the area of wear and tear.
The femoral component (stem and ball) replaces the femoral head. The femoral component is made of metal. Sometimes, the metal stem is attached to a ceramic ball.
There are special types of revision stems as well. This is because the bone of the femur is usually not the same as when the initial replacement was done. The bone may be weaker, or areas of the bone may be missing. A longer stem can reach further down the femoral shaft and distribute your body weight better.
The Operation
Revision joint replacements are much different from primary joint replacements. One reason that revision procedures are not routine is that there is almost always bone loss around the primary prosthesis. The surgeon deals with this problem by placing a bone graft or some other material around the artificial joint to reinforce the bone. This bone graft may come from your own body, such as bone taken from the pelvis during the same operation. This is commonly called an autograft.
If the amount of bone needed is too large to take from your body, your surgeon may choose to use bone graft from the bone bank. This type of bone graft has been taken from someone else and placed in the bone bank. This type of transplant is called an allograft.
When the primary artificial joint has been put in using cement, the cement has to be removed from the socket of the hip as well as from the femoral canal (the bone marrow space in the thighbone).
Because the bone is often fragile and the cement is hard, removing the cement sometimes can lead to a fracture of the femur during the operation. This is not unusual, and in most cases the surgeon will simply continue with the operation and fix the fracture as well. In some cases, the femur must be broken open to remove all the cement and the artificial joint. This is one reason that revisions are challenging.
During the operation, samples of bone and marrow tissue are usually removed and sent to a laboratory to see if any infection is present.
If the laboratory tests show an infection, a new artificial hip joint will probably be put in, and you will be placed on antibiotics for several months.
After application of bone and other materials to rebuild the socket and the femur, a new prosthesis is implanted. Because the natural shape can hardly ever be imitated after rebuilding the bone, most of the time a specially designed prosthesis has to be used. All of this is carefully planned by the surgeon before the operation.
A revision joint replacement of the hip is more complex and unpredictable than a primary joint replacement. Since many factors can influence its longevity, your surgeon will not be able to say exactly how long your revision will last.
In some cases, if an artificial joint fails, it may not be possible to put another artificial joint back in. This can occur if the primary joint has failed because of an infection that cannot be controlled, if the bone has been destroyed so much that it will not support an artificial joint, or if your medical condition will not tolerate a major operation.
Sometimes a choice other than hip revision is best because a big operation might result in a failure, or even death. Removing the prosthesis and not replacing it doesn’t mean the patient can’t walk anymore, but walking will be much more difficult because the leg grows shorter and the power in the leg is reduced.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following revision arthroplasty of the hip include
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- myositis ossificans
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following an artificial joint revision. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder and colon to reduce the risk of spreading germs to the joint.
The risk of infection is higher in revision joint replacement than in primary joint replacement. In a primary hip replacement, the risk of infection is 0.5 to one percent. It goes up to two percent or more in revision cases. These figures are only an estimate and vary between different scientific studies.
Dislocation
Just like your real hip, the revised artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. A physical therapist will instruct you very carefully on how to avoid activities and positions that may have a tendency to cause a hip dislocation.
Myositis Ossificans
Myositis ossificans is a curious problem that can affect the hip after both a primary hip replacement and a revision hip replacement. The condition occurs when the soft tissue around the hip joint begins to develop calcium deposits. Myositis means inflammation of muscle and ossificans refers to the formation of bone. This can lead to a situation where bone actually forms completely around the hip joint. This leads to stiffness in the hip resulting in much less motion in the hip joint than normal. It also causes pain.
Myositis ossificans is more common in people who have a long history of osteoarthritis with multiple bones spurs. Something about the genetic makeup in these people makes them more likely to produce bone tissue. Major reconstruction operations such as a hip revision seem to do more damage to the surrounding tissues than primary hip replacements. The operation is simply longer and harder to do. Calcium deposits are also more likely to form.
The treatment of myositis ossificans may actually begin before you get it. In cases where you are at high risk for developing this condition, your surgeon may recommend that you take medications such as indomethacin after surgery. This medication reduces the tendency for bone to form and may protect you from developing myositis ossificans.
A much more effective method that has been used a great deal to prevent the development of myositis ossificans involves radiation treatments immediately after surgery. These are the same type of radiation treatments used to treat cancer. Several short radiation treatments begun the day after surgery and continued for three to five days seem to drastically reduce the risk of developing myositis ossificans.
If myositis ossificans forms despite these precautions, treatment will depend on how much it affects your hip–how much pain it causes and how much it restricts motion. In some severe cases, you may choose to have a second operation to remove the calcified tissue that has formed. This is usually followed by radiation treatments to prevent the calcium deposits from returning.
Loosening
The major reason that artificial joints eventually fail continues to be a process of loosening where the metal or cement meets the bone. A loose revised prosthesis is a problem because it causes pain. Once the pain becomes unbearable, another revision surgery may be needed. The rate of loosening of revision arthroplasties is higher than in primary arthroplasties.
After Surgery
What happens after surgery?
After surgery, your hip is covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physical therapy treatments are scheduled one to three times each day as long as you remain in the hospital. Your first treatment is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you’ll begin walking longer distances using your crutches or walker.
You may not be allowed to put weight on the affected leg for a period of time. This varies from surgeon to surgeon and is also affected by how well your surgeon thinks the operation went.
Your therapist will go over exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
You will need to follow hip dislocation precautions–just like after your first artificial hip replacement. The risk of dislocation after a revision is higher than after a primary hip replacement.
Patients are usually able to go home after spending four to seven days in the hospital. You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who require extra care may be sent to a different unit until they are safe and ready to go home.
Most of the time your surgeon will see you one or more times during outpatient visits. Depending on what is learned from the examination and X-rays, you may start to put full weight on your leg. Because the operation is more complicated than primary replacement surgery and the period of walking on crutches may take longer, you must realize that it will take at least a year to be able to perform all normal daily activities. In some patients the possibilities are more limited than before. Be aware that a revision hip prosthesis is not as good as a primary prosthesis. There is always a chance that the donor bone will disappear in time because it is dead material and will be reabsorbed by the body. This means that loosening can occur once more. Today no other materials are available that are superior to donor bone.
Most orthopedic surgeons recommend that you have routine checkups after your revision surgery. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends. You should always consult your orthopedic surgeon if you begin to have pain in your artificial joint or if you begin to suspect something is not working correctly.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your physical therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will review your exercise program, continue working with you on your hip precautions, and make recommendations about your safety.
These recommendations may include that you use a raised commode seat and bathtub bench, and that you raise the surfaces of couches and chairs in your home. This keeps your hip from bending too far when you sit down. Bath benches and handrails can improve safety in the bathroom. Other suggestions include the use of strategic lighting and the removal of loose rugs or electrical cords from the floor.
You should continue to use your walker or crutches as instructed. If you had a cemented procedure, you’ll advance the weight you place through your sore leg as much as you feel comfortable. If you had a noncemented procedure, your surgeon may want you to place only the toes down for up to six weeks after surgery. Most patients progress to using a cane in four to six weeks.
Your staples will be removed two weeks after surgery. Patients are usually able to drive within three weeks and walk without a walking aid by two to three months. Upon the approval of the surgeon, patients are generally able to resume sexual activity by one to two months after surgery.
Home therapy visits end when you are safe to get out of the house, which may take up to three weeks.
The need for physical therapy usually ends when home care is completed. A few additional visits in outpatient physical therapy may be needed for patients who are still having problems walking or who need to get back to heavier types of work or activities.
Your therapist may use heat, ice, or electrical stimulation if you have swelling or pain.
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby activities.
Many patients have less pain and better mobility after hip revision surgery. Your therapist will work with you to help keep your revised joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your revised hip joint. Heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may need to consider alternate jobs to avoid work activities that require heavy lifting, crawling, and climbing.
The therapist’s goal is to help you maximize strength, walk normally, and improve your ability to do your activities. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Stress Fracture of the Hip
A Patient’s Guide to Stress Fracture of the Hip
Introduction
Stress fractures of the hip once most commonly affected military personnel who marched and ran day after day. Today, stress fractures of the hip are more common in athletes, especially distance runners.
There are two types of stress fractures. Insufficiency fractures are breaks in abnormal bone under normal force. Fatigue fractures are breaks in normal bone that has been put under extreme force. Fatigue fractures are usually caused by new, strenuous, very repetitive activities, such as marching or distance running. Most stress fractures of the hip are fatigue fractures. The stress fractures this article refers to are fatigue fractures.
This guide will help you understand
- how a stress fracture develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What is a stress fracture, and what part of the hip is involved?
The femur is the large bone in the thigh. The ball-shaped head of the femur fits into a socket in the pelvis, called the acetabulum. When a stress fracture occurs in the hip, it usually involves the femoral neck, the short section of bone that connects the head of the femur to the main shaft of the bone. The femoral neck is a thinner part of the femur. Stress fractures are hairline cracks in the bone that can grow larger over time if not treated properly.
The femoral neck has to withstand extreme force even during normal activities, such as standing still. The normal contraction of muscles during walking makes this stress even higher. Running triples the stress on the femoral neck.
Surgeons put fatigue fractures of the femoral neck into three categories. Compression fractures occur on the underside of the femoral neck. Tension fractures occur on the upper side of the bone and can cause more problems than fractures on the underside of the femoral neck. In displaced fractures, the bone cracks all the way through, and the two bones no longer line up correctly.
A displaced stress fracture is a very serious problem in a young adult because it may lead to damage to the blood vessels going into the upper end of the hip bone. This can cause a very serious complication known as avascular necrosis (AVN) of the hip.
Related Document: A Patient’s Guide to Avascular Necrosis of the Hip
Patients with fatigue stress fractures of the hip are also likely to have muscle and tendon injuries and swelling of the synovial lining (the lubricated lining) of the hip joint.
Stress fractures can also happen in the shaft of the femur bone, the greater trochanter, and the pelvis bone. The greater trochanter is a large bump below the neck of the femur. The buttock muscles that move the hip connect to this part of the femur.
Related Document: A Patient’s Guide to Hip Anatomy
Causes
Why do I have this problem?
Doctors think that putting extreme stress on the bone over and over again causes stress fractures of the hip. Think of how you can break a metal paper clip by bending it back and forth repeatedly.
Bones can usually adapt to repetitive stress, and any change in the function of a bone causes it to change the way it is built. This is how small bumps and ridges form on bones. The tendons pull on these areas, and the bone adapts by building up. This is normal. But extreme stress repeated too often can overwhelm the bone’s ability to adapt. This is especially true when someone suddenly begins a new, strenuous, repetitive activity such as running.
Fatigue fractures are related to both the amount of exercise and how fast people increase their exercise program. The more people run or march, the more likely they are to develop a fatigue fracture. Research suggests that most athletes who develop stress fractures have been training for at least two years, six or more times a week. A stress fracture is more likely to occur after an increase in how far, how often, and how hard a person goes.
Women are up to 10 times more likely to develop fatigue fractures than men. The reasons for this are unclear. Hormonal changes may make women athletes’ bones more likely to fracture. Eating disorders, which are more common in women athletes, may also make bones more likely to fracture.
Age also makes stress fractures of the hip more likely. This is thought to be due to declining levels of physical fitness more than age.
Symptoms
What does a stress fracture of the hip feel like?
Most patients with stress fractures of the hip feel pain in the front of the groin while standing and moving. Rest usually makes the pain go away. Patients may limp. Strenuous activities, such as running and climbing stairs, may be so painful that the patient must stop doing them.
Diagnosis
How do doctors identify the condition?
Your doctor will take a detailed medical history and ask many questions about your activities and exercise. Your doctor will also physically examine the painful hip. One of your doctor’s main goals will be to determine if other problems, such as muscle or tendon injuries, are causing some or all of your pain.
Your doctor will probably suggest taking an X-ray of your hip. The X-ray may help rule out other problems, but it probably will not show the stress fracture.
Your doctor may recommend other imaging tests that are more likely to show a stress fracture. A bone scan may be suggested to look for early signs of a stress fracture. A bone scan involves injecting tracers into your blood stream. The tracers then show up on special X-rays of your hip. The tracers build up in areas of extra strain to bone tissue, such as a stress fracture.
The magnetic resonance imaging (MRI) scan is especially useful in telling fatigue fractures from other types of injuries with similar symptoms. The MRI is being used increasingly in cases where doctors suspect a stress fracture.
Treatment
What can be done for the problem?
The treatment your doctor recommends will depend on the type of fracture you have.
Nonsurgical Treatment
Doctors most often recommend nonsurgical treatment for compression-type fatigue fractures. You must stay off the affected leg, using crutches if necessary, and rest the hip for at least four to six weeks. Pain can be treated with hot and cold treatments and medication. With care, the fractures tend to heal by themselves.
Surgeons do not all agree on how to treat tension fractures. If the fracture is not at risk for displacing, surgeons may have patients use crutches to keep strain off the hip during standing and walking. X-rays are taken every few weeks to make sure the bone is healing. If the tension fracture is in danger of displacing, however, most surgeons will operate. This is because the complication of AVN can cause the femoral head to actually lose its blood supply and collapse. This leads very rapidly to degenerative arthritis of the hip joint. Because these effects can be so devastating, most surgeons recommend surgery if they feel that the stress fracture is in danger of displacing.
Surgery
In some patients with a fracture under the femoral neck, MRIs and other imaging tests sometimes show an unstable fracture that needs to be surgically fixed.
The surgical procedure is the same whether the stress fracture is stable or there is only a slight displacement of the bones. If your surgeon recommends surgery for a stress fracture of the hip, several large metal screws will be inserted through the femoral neck to hold the fractured bones in place while the fracture heals.
To perform this procedure, a small incision is made on the side of the upper thigh. With the help of a special X-ray machine called a fluoroscope, the surgeon can insert the metal screws into the proper position while watching the X-ray image on a TV screen.
When the ends of the bones show a large displacement, surgeons aren’t in total agreement about which surgery is best. Most surgeons agree that younger, active patients benefit if surgery is done to save the femoral head. This method also uses screws to connect the two sections of bone.
To avoid problems with AVN, other surgeons feel that older, less active patients should have part or all of the hip joint replaced. If the socket of the joint is healthy, the surgeon may decide to replace only the ball portion of the joint, a procedure called hemiarthroplasty.
The procedure to replace both the ball and the socket with an artificial joint is called total hip arthroplasty.
Related Document: A Patient’s Guide to Hemiarthroplasty of the Hip
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Hip
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
Treating a stress fracture without surgery requires patients to strictly avoid putting weight down on the foot of the injured leg when they are standing or walking. Some surgeons allow their patients to use crutches and touch only their toes down on the injured side. Others prefer that their patients rely on crutches to completely avoid putting any weight down.
Your surgeon will probably have X-rays taken every few weeks to make sure the bones are lined up and healing. When your surgeon sees that the bones are healing, you’ll be able to put more weight on your foot as you stand and walk. A physical therapist may direct your rehabilitation to help you improve strength and flexibility in the hip and to make sure you are able to safely resume your activities.
After Surgery
Recovery after surgery for hip fracture depends on the type of procedure used. The aim of most surgical procedures for a fractured hip is to help people get moving and walking as quickly as possible. This helps them avoid dangerous complications that can happen from being immobilized, such as pneumonia, blood clots, joint stiffness, and pain.
A physical therapist may work with you in the hospital soon after surgery. Treatments are used to help you begin walking with crutches or a walker, to help you access the bathroom, and to gradually improve your hip motion and strength.
During your recovery, you should follow your surgeon’s instructions about how much weight you can put down while standing or walking.
After you return home from the hospital, your surgeon may have you work with a physical therapist for two to four in-home visits. These visits are to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your hip precautions, and make sure you are placing a safe amount of weight on your foot when standing or walking. Home therapy visits end when you are safe to get out of the house.
A few additional visits in outpatient physical therapy may be needed for patients who are still having problems walking or who need to get back to physically heavy work or activities.
The therapist’s goal is to help you maximize hip strength, restore a normal walking pattern, and help you do your activities without risking further injury to your hip. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Trochanteric Bursitis Surgery
A Patient’s Guide to Trochanteric Bursitis Surgery
Introduction
The bump of bone on the outside of the hip bone is called the greater trochanter. A fluid-filled sac, called a bursa, lies next to the greater trochanter. When the bursa in this area becomes thickened and inflamed, surgery may be needed to remove the bursa and to reduce tension on the tendon that glides over it.
This guide will help you understand
- what the surgeon hopes to achieve
- what happens during the procedure
- what to expect during your recovery
Anatomy
Why did my trochanteric bursa become a problem?
Where friction must occur between muscles, tendons, and bones, there is usually a bursa. A bursa is a thin sac of tissue that contains a bit of fluid to lubricate the area where the friction occurs. The bursa is a normal structure, and the body will even produce a bursa in response to friction.
The bursa next to the greater trochanter is called the greater trochanteric bursa. The gluteus maximus is the largest of three gluteal muscles of the buttock. This muscle spans the side of the hip and joins the iliotibial band. The iliotibial band is a long tendon that passes over the bursa on the outside of the greater trochanter. It runs down the side of the thigh and attaches just below the outside edge of the knee.
Walking causes the gluteus maximus to pull on the tendon. If the tendon is tight, it will start to press and rub against the greater trochanteric bursa. It is unclear why the tendon becomes tight. The rubbing causes friction to build in the greater trochangeric bursa, leading to irritation and inflammation in the bursa.
View animation of rubbing on the bursa
Friction can also start if the outer hip muscle (gluteus medius) is weak, if one leg is longer than the other, or if you run on banked (slanted) surfaces.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
The primary goal of the surgical procedure for this condition is to remove the thickened bursa, to remove any bone spurs (knobby outgrowths) that may have formed on the greater trochanter, and to relax the large tendon of the gluteus maximus. Some surgeons prefer to simply lengthen the tendon a bit, and some prefer to remove a section of the tendon that rubs directly on the greater trochanter. Both procedures give good results by taking pressure off the bursa.
Preparation
What do I need to do before surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. The amount of time patients spend in the hospital varies. You will need to stay until your medical condition has stabilized and you can safely use crutches or a walker.
Surgical Procedure
What happens during the operation?
Before surgery begins, you will be given anesthesia. There are two basic options: a general anesthetic (one that puts you to sleep) or a regional block (one that numbs the area to be worked on). For hip surgery the most common type of regional anesthetic available is either a spinal block or an epidural block. Both of these regional blocks numb the body from the waist down.
If you choose to have a regional anesthetic, you may also be given medication to allow you to drift off to sleep if you are anxious. Either type of anesthetic can be used to perform this procedure. Be sure to discuss this with your surgeon.
To begin the surgical procedure, an incision is made in the side of the thigh over the area of the greater trochanter. The surgeon continues the incision through the tissues that lie over the bursa.
The tendon is then split so that the trochanteric bursa and the bone of the greater trochanter can be seen. The tendon is split lengthwise. The bursa sac is removed. The bone of the greater trochanter is smoothed, and any bone spurs are removed.
At this point the tendon may be lengthened or released and not repaired. If the surgeon chooses not to repair the tendon, scar tissue will eventually heal the loose edges of the tendon. As it heals, it will be looser than before surgery, so it won’t rub on the greater trochanter quite so much. The skin is closed with stitches.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following surgery for trochanteric bursitis include
- anesthesia complications
- thrombophlebitis (DVT)
- infection
- nerve or blood vessel injury
- failure of the operation
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Any operation carries a small risk of infection. This procedure is no different. You will probably be given antibiotics before the operation to reduce the risk of infection. If an infection occurs you will most likely need antibiotics to cure the infection. You may need additional operations to drain the infection if it involves the area around the hip.
Nerve or Blood Vessel Injury
Several smaller nerves travel in the area where the surgery is performed. It is possible to injure the nerves during surgery, but this is extremely unlikely during this type of surgery. Nerve problems may well be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to the nerves, but it is possible.
Failure of the Operation
This operation may not be successful. All operations have a chance of failure, and this operation is no different. Even after going through the procedure, you may continue to have pain from trochanteric bursitis. This is clearly not the expected outcome, and the majority of patients are relieved by the procedure.
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Try to avoid a lot of activity within the first week after surgery. Support your outer hip with a pillow when you sit or recline. During this time, you may also be instructed to use crutches to keep from placing weight on your hip while you stand or walk.
Keep the dressing on your hip until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery. If your surgeon chooses to use dissolvable stitches, these will not need to be removed.
Rehabilitation
What should I expect during my recovery?
Rehabilitation after surgery can be a slow process. You will probably need to attend physical therapy sessions for several weeks, and you should expect full recovery to take several months. Getting the hip moving as soon as possible is important. However, this must be balanced with the need to protect the healing muscles and tissues.
Ice and electrical stimulation treatments may be used during your first few therapy sessions to help control pain and swelling from the surgery. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Treatments include range-of-motion exercises and gradually work into active stretching and strengthening. Active therapy starts two to three weeks after surgery. You may begin with light isometric strengthening exercises. These exercises work the muscles without straining the healing tissues.
At about four weeks you may start doing more active strengthening. Exercises focus on improving the strength and control of the buttock and hip muscles. Your therapist will help you retrain these muscles to keep the ball of the femur moving smoothly in the socket.
Some of the exercises you’ll do are designed get your hip working in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your hip. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Compression Fixation for a Fractured Hip
A Patient’s Guide to Compression Fixation for a Fractured Hip
Introduction
A fractured hip can be a life-threatening problem. The hip fracture itself isn’t usually a difficult problem to treat with surgery. But once the fracture occurs, it brings with it all the potential medical complications that can arise when aging adults are confined to bed. The goal of treatment is to get patients moving as quickly as possible after surgery. Fixing the fracture with a compression hip screw and metal plate is fairly simple and usually allows patients to get up and start moving shortly after surgery.
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the operation
- what to expect during your recovery
Anatomy
What part of the hip is involved?
The femur is the large bone in the thigh. The ball-shaped femoral head fits into a socket in the pelvis, called the acetabulum. The femoral neck is a thinner part of the femur. It is the short section of bone next to the femoral head that connects the femoral head to the main shaft of the femur.
The intertrochanteric region of the hip is just below the femoral neck. A fracture in this area is called an intertrochanteric hip fracture. This type of fracture is most common when a person falls and fractures the hip. There is usually more than one fracture with more pieces of broken bone to be held together.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
Fixing the hip fracture surgically with a special type of metal plate and screw, called a compression screw, does two things. First, it helps align the bone fragments and hold them in the proper position. Second, the fixation device is strong enough to keep the bones in place as you begin to move about. Before these devices were used, a patient needed to remain in bed usually with traction to hold the bones in alignment. The fixation now holds the bones in place while the bone heals. This allows you to get out of bed sooner because the metal plate and screw are strong enough to hold the bone fragments in place as you move.
The procedure requires only a small incision on the side of the hip, and the plate and screw usually provide a solid connection for the broken bones. Since patients are able to get moving right away after surgery, they are more likely to avoid the serious complications that can arise with being immobilized in bed.
Preparation
What happens before surgery?
Compression fixation for a fractured hip is usually an emergency surgery, so it is likely you may not have had time to plan and prepare. Ideally a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital.
The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, make sure you have needed supplies, and make follow-up appointments with your surgeon, doctor, and physical therapist.
Surgical Procedure
What happens during the operation?
Sometimes, a fractured hip only requires a simple pinning procedure. The procedure for the compression hip screw, however, is more involved. There are usually several fragments of bone that need to be held together. There is also more blood lost during the surgery, which could require that you have a blood transfusion during the operation.
Related Document: A Patient’s Guide to Hip Pinning Surgery for a Fractured Hip
This operation can be done using either a general anesthetic or a spinal block. A general anesthetic puts you completely to sleep. A spinal block puts your body to sleep only from the waist down. The anesthesiologist will also give you medications so that you won’t be aware the operation is being done.
Once you have anesthesia, your surgeon will make sure the skin of your hip is free of infection by cleaning the skin with a germ-killing solution.
With the patient lying flat on a special table, the foot and leg are supported. Tension is applied to get the fractured bones to line up. The surgeon checks the alignment using a fluoroscope, a type of X-ray machine that shows the image on a TV screen.
Next, the surgeon makes an incision over the side of the thigh. A large metal screw is placed through the side of the hip into the femoral head. With the help of the fluoroscope, the surgeon attaches a metal plate to the side of the femur with four to eight small metal screws. The procedure can usually be finished in less than an hour depending on how many fragments of bone are involved in the fracture.
The soft tissues are put back in place, and metal staples or sutures are used to close the incision.
Complications
What might go wrong?
Complications after a hip fracture are sometimes the result of being immobilized in bed. These may include pneumonia, bed sores, mental confusion, and blood clots (deep venous thrombosis).
Related Document: A Patient’s Guide to Hip Fracture
Complications that can result from the compression fixation surgery itself include
- anesthesia complications
- infection
- thrombophlebitis (DVT)
- nerve or blood vessel injury
- nonunion of the bones
This is not intended to be a complete list of possible complications.
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any surgery carries the risk of infection. You will probably be given antibiotics before the procedure to reduce the risk. If you get an infection, you will need more antibiotics. If the areas around the metal screws or plate become infected, you may need surgery to drain the infection.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Nerve or Blood Vessel Injury
Several nerves and blood vessels travel in the area where the surgery is performed. It is possible to injure either the nerves or the blood vessels during surgery, but this is extremely unlikely during this type of procedure. Nerve problems may be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to either the nerves or the blood vessels, but it is possible.
Nonunion
Sometimes the bones do not bond together as planned. This is called a nonunion, or pseudarthrosis. This condition requires another operation to add more fixation or to replace the head of the femur, a procedure called hemiarthroplasty.
Related Document: A Patient’s Guide to Hemiarthroplasty of the Hip
After Surgery
What happens after the operation?
After surgery, your hip will be covered with a padded dressing. If your surgeon used a general anesthesia, a nurse or respiratory therapist will guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
A physical therapist will direct your recovery after surgery. You’ll be encouraged to move from your hospital bed to a chair several times the first day after surgery. You’ll be encouraged to begin getting up and walking with your crutches or walker, but you may need to keep from placing too much weight on your foot while you stand or walk. You’ll be ready to go home when you can move about safely with your walker or crutches, you are able to do your exercises, and your caregiver has made all the needed preparations for you at home.
You should keep the dressing on your hip until you return to the surgeon. Avoid getting the stitches wet. Your stitches will be removed 10 to 14 days after surgery. Remember to support your outer hip with a pillow when you sit or recline.
Rehabilitation
What should I expect during my recovery?
Once discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure that you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on walking and strength. In some cases you may require additional visits at home before beginning outpatient physical therapy. Home therapy visits end when you are safe to get out of the house.
Additional outpatient physical therapy visits are sometimes needed for patients who are still having problems walking or who need to get back to physically heavy work or activities.
Your therapist may use hands-on stretches for improving range of motion. Strength exercises address key muscle groups including the buttock, hip, and thigh. Endurance can be achieved through stationary biking, lap swimming, and using an upper body ergometer (upper cycle).
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip. Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
The therapist’s goal is to help you maximize hip range of motion and strength, restore a normal walking pattern, and do your activities without risking further injury. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Hip Fractures
A Patient’s Guide to Hip Fractures
Introduction
As the population ages, the number of hip fractures that occur each year rises. A fracture of the hip in an aging adult is not simply a broken bone. It is a life-threatening illness. The hip fracture itself is rarely a difficult problem to solve. But once the fracture occurs, it brings with it all the potential medical complications that can arise when aging patients are confined to bed. The complications are what can turn a simple break into a life-threatening illness.
Hip fractures in children and young adults are much different. The information in this document applies only to hip fractures in the elderly.
This guide will help you understand
- how hip fractures happen
- how doctors diagnose the problem
- what treatment options are available
Anatomy
How does the hip work?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone, or femoral head. The femoral head is attached to the rest of the femur by a short section of bone called the femoral neck. The bump on the outside of the femur just below the femoral neck is called the greater trochanter. This is where the large muscles of the buttock attach to the femur.
Thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip. The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
All of the blood supply to the femoral head (the ball portion of the hip) comes through the neck of the femur. If this blood supply is damaged, there is no backup. One of the problems with hip fractures is that damage can occur to these blood vessels when the hip breaks. This can lead to the bone of the femoral head actually dying. Once this occurs, the bone is no longer able to maintain itself. This can lead to one of the complications of a hip fracture called avascular necrosis (AVN).
Related Document: A Patient’s Guide to Avascular Necrosis of the Hip
Related Document: A Patient’s Guide to Hip Anatomy
Causes
Why do I have this problem?
Injury is an obvious cause of hip fractures. In the elderly population, an injury can result from something as simple losing one’s balance and falling to the ground. While many hip fractures probably occur this way, it is also true that the fall may have happened as a result of fracturing the hip. The hip actually breaks first, causing the person to fall.
Osteoporosis can weaken the neck of the femur to the point that any increased stress may cause the neck of the femur to break suddenly. An uncertain step may result in a twist to the hip joint that places too much stress across the neck of the femur. The femoral neck breaks, and the patient falls to the ground. It happens so quickly that it is unclear to the patient whether the fall or the break occurred first.
Related Document: A Patient’s Guide to Osteoporosis
Symptoms
What does a hip fracture feel like?
A hip fracture, like any broken bone, causes pain. The fracture makes putting weight on the leg extremely difficult. When a hip fracture occurs in an aging adult who lives alone, it may be hours before anyone finds the patient. The patient sometimes cannot get to the phone to alert anyone. This is the first life-threatening situation. This situation can result in dehydration, or if the fracture occurs outside in a cold environment, the patient may develop hypothermia. Both of these conditions can be deadly.
Diagnosis
How do doctors identify the problem?
The diagnosis of a hip fracture usually occurs in the emergency room. The diagnosis begins with a history and physical examination. It is important that the doctor be advised of any other medical problems the patient has so that treatment of the hip fracture can be planned. Most of the information from the history and physical examination will be used to try to evaluate the overall physical condition of the patient. Tests such as chest X-rays, blood work, and electrocardiograms may be ordered to assess the patient’s overall condition.
X-rays are typically used to determine if a hip fracture has occurred and, if so, what type of fracture it is. The orthopedic surgeon will use the X-rays to determine if a surgical procedure will be necessary and to decide what type of procedure to suggest.
In a few cases, X-rays may not show the fracture. If the hip continues to hurt and the doctor is suspicious that a hip fracture is present, magnetic resonance imaging (MRI) may be suggested. The MRI scanner uses magnetic waves rather than radiation to take multiple pictures of the hip bones. The MRI machine is very sensitive and can show fractures that do not show up on regular X-rays.
This test is done to be certain there is no fracture before allowing the patient to put weight on the leg. Walking on a fractured hip may cause the two sides of the fracture to displace, or move apart, so that they no longer line up correctly. A fracture that has not displaced is much easier to treat than one that has. A displaced fracture also increases the risk of damaging the blood supply to the femoral head, causing AVN (discussed earlier).
Treatment
What can be done for the problem?
The treatment for a hip fracture begins immediately by making sure the patient is medically stable. Once the doctor is sure that the patient is stable, decisions concerning the treatment of the fracture can be made.
Nonsurgical Treatment
Rarely is a fracture considered stable, meaning that it will not displace if the patient is allowed to sit in a chair. But if the fracture does seem stable, the patient may be treated without surgery if the doctor feels that the patient will be able to get out of bed within several days.
Most hip fractures would actually heal without surgery, but the problem is that the patient would be in bed for eight to 12 weeks. Doctors have learned over the years that placing an aging adult in bed for this period of time has a far greater risk of creating serious complications than the surgery required to fix a broken hip. This is the main reason that surgery is recommended to nearly all patients with fractured hips.
Surgery
Nearly all hip fractures in the elderly are treated with some type of surgical operation to fix the fractured bones. If possible, the surgery is normally done within 24 hours of admission to the hospital.
The goal of any surgical procedure to treat a fractured hip is to hold the broken bones securely in position, allowing the patient to get out of bed as soon as possible. Many methods have been invented to treat the different types of fractures. Most hip fractures are treated in one of three ways: with metal pins, with a metal plate and screws, or replacing the broken femoral head with an artificial implant.
Metal Pins
Fractures that occur through the neck of the femur, if they are still in the correct position, may require only two or three metal pins to hold the two pieces of the fracture together. This procedure, called hip pinning, is fairly simple and allows patients to begin putting weight down right after surgery.
Related Document: A Patient’s Guide to Hip Pinning Surgery for a Fractured Hip
Metal Plate and Screws
Some hip fractures occur below the femoral neck in the area called the intertrochanteric region. These fractures are called intertrochanteric hip fractures. These hip fractures are usually truly the result of a fall and often are the hardest type of fracture to treat. They often involve more than one break. As a result, several pieces of broken bone must be held together.
Surgeons usually try to fix this type of fracture using a metal plate and compression hip screw. This approach helps align the bones and relies on the force of the muscles to compress the fractured bones together so they will heal.
Related Document: A Patient’s Guide to Compression Fixation for a Fractured Hip
Artificial Replacement of the Femoral Head (Hemiarthroplasty)
When the hip fracture occurs through the neck of the femur and the ball is completely displaced, there is a very high chance that the blood supply to the femoral head has been damaged. This makes it very likely that AVN of the femoral head will occur as a complication of this type of hip fracture.
As mentioned earlier, AVN causes the bone of the femoral head to die. The femoral head begins to collapse weeks later, causing more problems in the months to come. This will most likely result in a second operation several months later to replace the hip due to the AVN. The likelihood of this is so great that most surgeons will recommend removing the femoral head immediately and replacing it with an artificial femoral head made of metal. This operation is called a hemiarthroplasty. (Hemi means half, and arthroplasty means artificial joint.) The procedure is called hemiarthroplasty because only half of the joint is replaced. The socket of the hip joint is left intact.
Related Document: A Patient’s Guide to Hemiarthroplasty of the Hip
Complications
What might go wrong?
The complications that can develop after a hip fracture are what make the injury a life-threatening problem. Some complications can result from surgery, but many can occur whether the fracture is treated with surgery or not.
Most of the complications that occur after a hip fracture result from having to put an aging adult on bed rest. In general, this seems to make all the medical problems the patient has worse. Some of the more common problems that a hip fracture can increase the likelihood of include
- anesthesia
- pneumonia
- pressure ulcers
- thrombophlebitis
- mental confusion
Getting the patient out of bed and moving can reduce the risk of developing all these complications. If an operation is necessary to stabilize the fracture and get the patient out of bed quickly, this will actually reduce the overall risk of developing these complications. That doesn’t mean that the complications may not still occur after surgery, but they are far easier to treat if the patient can be mobilized.
Anesthesia
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Pneumonia
Bed rest can increase the risk of developing pneumonia in older patients. If anesthesia is required for surgery, the risk is even greater. After any injury that requires bed rest, you will need to do several things to keep your lungs working their best. Your nurse will coach you to take deep breaths and cough frequently. Getting out of bed, even upright in a chair, allows the lungs to work much better. As soon as possible, you will be allowed to sit in a chair.
The hospital’s respiratory therapists have several tools to help maintain optimal lung function. The incentive spirometer is a small device that measures how hard you are breathing and gives you a tool to improve your deep breathing. If you have any other lung disease, such as asthma, the respiratory therapist may also use medications that are given through breathing treatments to help open the air pockets in the lungs.
Pressure Ulcers (Bedsores)
Hip fractures cause pain when you move, even in bed. As a result, you stop moving around to shift your weight from time to time as you normally would. When you are lying down, there is pressure on the skin in certain areas. This pressure actually stops the blood flow to the skin by closing off the blood vessels that go to that area. Usually this isn’t a problem because you soon shift your weight, moving the pressure to another area. This shifting of the pressure allows the blood flow to return to the area of skin and prevents any damage.
But if something prevents you from shifting and the pressure stays constant in one area, that area of skin may eventually become damaged due to lack of blood flow. This damage is called a pressure ulcer or bedsore. The pressure causes the skin to actually die, similar to skin that has been burned with heat. First the area hurts, then it begins to blister, and then it turns into an open sore. These sores are difficult to heal if they are large. They may actually require a skin graft. They can become infected, causing other problems.
The best treatment is to prevent bedsores in the first place. Hospitals use special mattresses and special water beds to help distribute weight evenly in people who must be confined to bed. Nurses also routinely move patients in bed to make sure the skin is not getting too much pressure in one area. Still, the best way to prevent pressure ulcers is to get you out of bed and moving.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can result from bed rest and inactivity. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots break apart, they can travel to the lungs, where they lodge in the capillaries (smallest blood vessels in the body) and cut off the blood supply to a portion of the lungs. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the blood vessels.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Mental Confusion
Aging adults who suffer a hip fracture and go to the hospital are under a lot of stress. Unfamiliar surroundings, pain medications, and the stress of the injury can lead to changes in a patient’s behavior. This is sometimes called the sundowner syndrome because it seems to get worse at night. This can be very frightening to both patients and their families. Fortunately, it is almost always temporary. It can cause problems because patients can become difficult to handle and won’t follow instructions. They may try to get out of bed and can damage the hip further.
The best treatment for mental confusion is usually to get patients moving and out of the hospital. Familiar surroundings, familiar faces, and activity are the best treatments. Medications are used when necessary, and it may be necessary to restrain patients during this period so that they will not hurt themselves further. Other medical conditions can cause confusion, and the doctor will make sure that these are not present. But, again, usually the mental confusion is temporary and will go away in a matter of days.
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
Hip fractures usually require surgery. Nonsurgical rehabilitation is only used in a few instances after a hip fracture in an aging adult. A patient with other complicating illnesses who fractures a hip may be treated with traction. A traction pull on the injured limb is a means, other than surgery, of helping the bone fragments to line up.
Patients who have a stable fracture (mentioned earlier) may also receive nonsurgical rehabilitation. These patients may require a few days’ bed rest before getting assistance to stand and walk. When the doctor determines that the fracture has healed, a formal program of physical therapy lasting four to six weeks may be prescribed.
After Surgery
The aim of most surgical procedures for a fractured hip is to help people get moving and walking as quickly as possible. This helps them avoid dangerous complications that can arise from being immobilized in bed, such as pneumonia, blood clots, joint stiffness, and pain.
A physical therapist usually works with patients in the hospital soon after surgery. You’ll be assisted from your bed to a chair several times each day. You’ll begin walking with a walker or crutches, practice accessing the bathroom, and start doing exercises to tone the muscles around the hip and thigh and to prevent the formation of blood clots.
The amount of weight that can be placed on the operated leg depends on the type of surgery performed. Most patients are able to start weight bearing right away after surgery. Depending on the severity of the fracture, patients may only be able to place partial weight down right away.
Patients who require hemiarthroplasty follow a different treatment plan. This surgery is more involved and requires the surgeon to open up the hip joint during surgery. This puts the hip at some risk for dislocation after surgery. To prevent hip dislocation after surgery, patients follow strict guidelines about which hip positions they must avoid, called hip precautions. Patients follow these precautions at all times for at least six weeks after surgery, until the soft tissues gain enough strength to keep the joint from dislocating. Patients may be instructed to use their walker or crutches to limit the amount of weight they place on the operated leg.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
After you return home from the hospital, your surgeon may have you work with a physical therapist for two to four in-home visits. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your hip precautions, and make sure you are placing a safe amount of weight on your foot when standing or walking. Home therapy visits end when you are safe to get out of the house.
Additional visits to outpatient physical therapy may be needed for patients who have problems walking or who need to get back to physically heavy work or activities.
The therapist’s goal is to help you maximize hip strength, restore a normal walking pattern, and help you do your activities without risking further injury. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Hip Fracture Surgery Rehabilitation
A Patient’s Guide to Rehabilitation Following Hip Fracture Surgery
Introduction
A hip fracture can present complications due to being immobilized. The goal of rehabilitation after hip fracture surgery is to help you begin moving as quickly as possible to avoid the serious complications that can happen with being immobilized in bed.
This guide will help you understand
- precautions to keep in mind after surgery
- expectations for your therapy evaluation and treatments
- safe exercises to improve your mobility and strength
Precautions after Surgery
Surgeons use different methods to surgically treat hip fractures. As a result, the precautions you’ll follow after surgery depend on your surgeon’s preference and the way the surgery was done.
Rest
Avoid activities that put a strain on the surgical area. If you feel pain, stop or alter what you are doing. Pain at this stage indicates strain or irritation. During your activities, let pain guide your decisions about what you do.
Artificial Hip Precautions
If you had hemiarthroplasty surgery, use your hip precautions at all times.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Weightbearing
You will use a walking aid, such as a walker or crutches, after surgery. The amount of weight you are able to bear when standing or walking will depend on the type of procedure you had and the advice of your surgeon.
Toe-Touch Weightbearing
After a noncemented hemiarthroplasty or for procedures using metal plates and pins, you should touch only your toes down on the side where the surgery was done.
Comfortable Weightbearing
After a cemented hemiarthroplasty or if a compression screw was used, you will likely be given the okay to place a comfortable amount of weight on your foot while standing or walking.
Exercises
Any exercises you do should be done only following instruction by your surgeon or therapist. The kinds of exercises you do depend on your particular procedure. Extra pain after these or other exercises usually indicates that you are overdoing it. You may need to change the number of repetitions, the amount of pressure applied, or how often you are doing your exercises.
Therapy Visits
Inpatient Therapy
A physical or occupational therapist will direct your recovery after surgery. Patients usually stay in the hospital between three and seven days after hip fracture surgery. You’ll be encouraged to move from your hospital bed to a chair several times the first day after surgery. Then you’ll begin getting up and walking using your crutches or walker. However, you may need to keep from placing too much weight on your foot while you stand or walk. You’ll be safe to go home when you can get up and move about safely with your walker or crutches, you are able to do your exercises, and your caregiver has made all the needed preparations for you to go home.
Home Therapy
Once discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will make recommendations about your safety, review your exercise program, and continue working with you on walking and strengthening. In some cases you may require additional visits at home before beginning outpatient physical or occupational therapy. Home therapy visits end when you are safe to get out of the house.
Outpatient Therapy
Your surgeon may prescribe four to eight weeks of therapy in an outpatient clinic. The goals of treatment are to help you regain hip range of motion, maximize your strength, walk without a limp, and resume your activities.
On your first visit to outpatient therapy, your therapist will ask many questions about your condition. Your answers will help guide your therapist’s examination. You will probably be asked how your condition is affecting your day-to-day activities. Rating your pain or symptoms on a scale of one to ten helps your therapist gauge how you’re doing now and how your pain and symptoms change with treatment. Here are some other questions your therapist may ask you.
- How is your hip feeling since the surgery?
- Are you feeling pain now?
- How do your symptoms affect your daily activities?
Therapy Examination
After reviewing your answers, your therapist will do an examination that may include some or all of the following checks.
Posture
Your therapist may check your overall posture, including the alignment of your back, pelvic bones, hips, knees, and ankles. Your therapist will also check the surgical area to make sure the incisions are healing. By comparing each side, your therapist can determine if there is swelling, bruising, or any loss in muscle size.
Gait
By watching you walk, your therapist can check to see that you are putting only a safe amount of weight through your operated leg and that your walking aid is adjusted for you.
Range of Motion
Your therapist may check the range of motion (ROM) in your hip. This is a measurement of how far you can move your hip in different directions. Measurements might include forward (flexion) and back (extension) motions, rotating the hip in (internal rotation) and out (external rotation), and side-to-side movements (abduction and adduction). If you are following hip precautions for hemiarthroplasty, care will be taken not to move your hip in directions or positions that stress the surgical hip. The therapist may record your ROM during each visit to chart your progress.
Strength
Your therapist may have you hold against resistance in order to test the muscles around the hip and knee. Muscles that may be checked include the quadriceps (thighs), buttocks, hamstrings, and calves. The results are compared to your other side. Weakness in key muscles will be addressed with a strengthening program.
Palpation
Your therapist will feel the soft tissues around the sore area. This is called palpation. Through palpation, the therapist checks skin temperature and swelling, pinpoints sore areas, and looks for tender points or spasm in the muscles around the sore area.
Planning Your Care
Your therapist will evaluate your answers and your examination results to determine the best way to help you. Then your therapist will write a plan of care. The plan of care lists the treatments that will be used and the goals that you and your therapist decide on to get your daily activities done safely and with the least amount of discomfort. The plan also includes a prognosis, which is your therapist’s idea of how well the treatments will work and how long you’ll need therapy in order to get the most benefit.
Therapy Treatments
Controlling Pain and Symptoms
Your therapist may choose from one or more of the following treatment interventions to begin helping you control your symptoms.
Rest
Rest is an important part of treatment after surgery. If you are having pain with an activity or movement, it usually indicates that there is still irritation. You should try to avoid all movements and activities that increase your pain. Be sure to use your crutches or walker as assigned, and put only the amount of weight on your leg as approved by your surgeon. The goal is to keep your symptoms to a minimum, while promoting healing.
Heat
Heat makes blood vessels vasodilate (get larger), increasing the blood flow. This action helps flush away chemicals that cause pain. It also helps bring in healing nutrients and oxygen. True heat in the form of a moist hot pack, a heating pad, or warm shower or bath is more beneficial than creams that merely give the feeling of heat. Hot packs are usually placed on the sore area for 15 to 20 minutes up to four times each day. Special care must be taken to make sure your skin doesn’t overheat and burn. It’s not a good idea to sleep with an electric hot pad at night. You may find you have less pain and better mobility after applying heat.
Ice
Ice makes blood vessels vasoconstrict (get smaller), decreasing the blood flow. This helps control inflammation and the pain it causes. Ice treatments are easy to do at home. You can use cold packs, ice bags, or ice massage. Cold packs or ice bags are generally placed on the sore area for 10 to 15 minutes up to four times each day. Put a wet towel between the cold pack and your skin. You may feel less pain by applying ice.
Electrical Stimulation
Gentle electrical currents through the skin can help ease pain and decrease swelling. Electrical stimulation eases pain by replacing pain impulses with the impulses of the electrical current. Electrode pads are placed over the sore area, and the stimulation is generally applied for about 15 minutes. Once the pain lets up, the muscles begin to relax. Some patients say electrical stimulation feels like a gentle massage. By relaxing the muscles, you may be able to exercise and do your activities easier.
Therapeutic Exercise
Whether at work, home, or play, your capabilities depend on your physical health and function. Specialized treatments and exercises can help maximize your physical abilities, including movement, balance, and strength. Exercises are used to help improve motion, strength, and endurance in the hip. Your program could also address key muscle groups of the buttocks, thigh, and calf.
Improving Range of Motion (ROM)
The swelling and irritation from a hip surgery can cause stiffness in the hip. To improve your range of motion (ROM), your therapist can use hands-on joint and muscle stretching and specific exercises. Active movement and stretching as part of the clinic and home program can also help restore movement. Getting your hip moving will help with your overall hip ROM, easing pain and making it easier to do your exercise and activities.
Pool Therapy
Exercising in a pool eases movement. The buoyancy of the water makes exercising easier, lends resistance, and helps you begin walking with less stress on your hip. If your surgeon has given you weightbearing restrictions, avoid putting pressure down on the foot of your operated leg, even in the pool. If your therapist works with you in the pool, only a few visits are usually all that are needed before you transition to a regular program on land. If you are getting good benefits in the pool, you may want to plan a program for the longer term that integrates aquatic exercises. You may also want to find the best aquatic facility for your needs and obtain a membership. The warmth of the water can help muscles relax, improve circulation, and ease soreness.
Strengthening
The swelling and pain from your hip problem and surgery can lead to weakened muscles around the hip. When muscles weaken from pain or disuse, other muscles overpower the weaker ones. This type of imbalance changes the way the joints usually work. Strengthening exercises are used to restore muscle balance so the hip joint works smoothly during your movements and activities.
Progressive Resistive Exercises (PREs)
Many kinds of progressive resistive exercises (PREs) are now taught in rehabilitation using pulley systems, free weights, rubber tubing, manual resistance, and computerized exercise devices. These exercises typically start with lighter weights with lots of repetitions, and as endurance increases, more weight is gradually used with fewer repetitions. Using PREs is a way to apply graded resistance to muscle groups to gradually help them gain endurance and strength.
Functional Training
Therapists also use functional training when you need help doing specific activities with greater ease and safety. Functional training simulates day-to-day activities like stair climbing, pivoting, and squatting, depending on which phase of rehabilitation you have completed.
Gait Training
Your therapist will work with you to fine tune the way you walk. By helping you get back to a normal walking pattern, you’ll avoid placing extra strain on the hip joint. You might walk on a treadmill in front of a mirror so you can gauge your walking pattern and make needed corrections. Your therapist will also train you to walk on uneven surfaces and to go up and down stairs safely. The goal is to help you walk normally and safely on a variety of surfaces.
Closed Kinetic Chain Functional Exercises
In closed kinetic chain functional exercises, the leg or foot is fixed on a surface while movement and resistance take place in the joints and muscles above. These types of exercises are important because they are like to the activities we do every day. For example, a partial squat exercise is the same action as lowering yourself onto a chair or couch. A leg press is a lot like the action of going up a stair or step. These exercises add strength and stability around the muscles and joints of the hip and leg.
Balance Exercises
Balance exercises help retrain your position sense, also called joint sense. You can think of these exercises like balance training. Examples include balancing on one leg with your eyes open and closed, walking on uneven or soft surfaces, and practicing on various balance boards. Some therapists also use special manual exercises to improve joint sense. Improving joint sense strengthens and stabilizes the hip joint, easing pain and improving function.
Home Program
Your therapist’s goal is to help you learn ways to keep your symptoms under control and improve your strength and range of motion. Before you are done with therapy, more measurements may be taken to gauge your progress since the beginning of therapy. When you are well under way, your regular visits to the therapist’s office will end. Your therapist will continue to be a resource for you, but you will be in charge of your own ongoing rehabilitation program.
Prevention
Improving your balance, range of motion, and strength can help you control symptoms and avoid future problems. Continue your home program as instructed by your therapist. If you had a hemiarthroplasty, you should continue using your hip precautions until your surgeon says it’s OK to discontinue using them.
Hemiarthroplasty of the Hip
A Patient’s Guide to Hemiarthroplasty of the Hip
Introduction
A hemiarthroplasty is an operation that is used most commonly to treat a fractured hip. The operation is similar to a total hip replacement, but it involves only half of the hip. (Hemi means half, and arthroplasty means joint replacement.) The hemiarthroplasty replaces only the ball portion of the hip joint, not the socket portion. In a total hip replacement, the socket is also replaced.
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the operation
- what to expect after the procedure
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Hip
Anatomy
How does the hip joint work?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone, known as the femoral head. The thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
All of the blood supply to the femoral head (the ball portion of the hip) comes through the neck of the femur (femoral neck), a thinner section of the thigh bone that connects the ball to the main shaft of the bone.
If this blood supply is damaged, there is no backup. One of the problems with hip fractures is that damage can occur to these blood vessels when the hip breaks.
This can lead to the bone of the femoral head actually dying. Once this occurs, the bone is no longer able to maintain itself. This can lead to one of the complications of a hip fracture called avascular necrosis (AVN). This condition occurs when the blood supply to areas of the femoral head are damaged. The dead bone may eventually collapse, causing pain in the hip.
Related Document: A Patient’s Guide to Avascular Necrosis of the Hip
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What do surgeons hope to achieve with the operation?
Fractures of the hip often involve the femoral neck. In many cases, the risk of developing AVN is so high that your surgeon may suggest not trying to fix the fracture. Instead, the femoral head can be removed and replaced with an artificial piece, or prosthesis. This is suggested because fixing the fracture carries a high chance that you will need a second operation several months later if the femoral head dies due to AVN.
When the hip is fractured, the socket portion (the acetabulum) is usually not injured. If the articular cartilage of the hip socket is in good condition, the metal ball of the hemiarthroplasty prosthesis can glide against the cartilage without damaging the surface. This procedure is easier to do than replacing both the ball and the socket, and it allows patients to begin moving right away after surgery. Early movement helps prevent dangerous complications that come from being immobilized in bed.
A fracture of the hip in an aging adult is not simply a broken bone, it is a life-threatening illness. Replacing the damaged section of hip with a hemiarthroplasty can quickly get the patient out of bed and moving to reduce the risk of complications.
Related Document: A Patient’s Guide to Hip Fractures
Preparation
How should I prepare for surgery?
This procedure is usually an emergency surgery, so it is likely you may not have had time to plan and prepare. Ideally, a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital.
The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, prepare your home for your arrival, make sure you have needed supplies, and schedule follow-up appointments with your surgeon, doctor, and physical therapist.
Surgical Procedure
What happens during the operation?
Before we review the procedure, let’s look at the prosthesis that is inserted into your hip during surgery.
The Hemiarthroplasty Prosthesis
As described earlier, the hemiarthroplasty prosthesis replaces the femoral head. The prosthesis is composed of a metal stem that fits into the hollow marrow space of the thighbone (the femur). It also has a metal ball that fits into the socket of the hip joint (the acetabulum).
The femoral head that attaches to the stem may be a separate part. Two types are commonly used by surgeons. Some surgeons prefer a solid metal ball to replace the femoral head. This type of prosthesis is called a unipolar type. Other surgeons prefer to use a bipolar type of prosthesis. The bipolar type has a femoral head that swivels where it attaches to the stem. The bipolar prosthesis was designed to try to reduce the wear and tear on the articular cartilage inside the acetabulum. It is unclear whether the swivel offers any significant advantages. Both types seem to work well.
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis bears a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone. Both methods are still widely used. The decision about whether to use a cemented or uncemented prosthesis is usually made by the surgeon based on your age, the condition of your bones, your lifestyle, and the surgeon’s experience.
The Operation
To begin, the surgeon makes an incision on the side of the thigh to allow access to the hip joint. Several different approaches are used to make the incision. The choice is usually based on the surgeon’s training and preferences.
Once the hip joint is entered, the surgeon removes the femoral head from the acetabulum.
Special rasps (coarse files) are used to shape the hollow femur to the exact shape of the metal stem of the prosthesis. Once the size and shape are satisfactory, the stem is inserted into the femoral canal. Again, in the uncemented variety of femoral component the stem is held in place by the tightness of the fit into the bone (similar to the friction that holds a nail driven into a hole slightly smaller than the diameter of the nail). In the cemented variety, the femoral canal is enlarged to a size slightly larger than the femoral stem, and the epoxy-type cement is used to bond the metal stem to the bone. The metal ball that makes up the femoral head is then attached.
Once the implant is in place, the new artificial hip is relocated (or reduced) back into the hip socket. The surgeon makes sure that the hip works properly and the joint moves easily. The surgeon then closes the incision with several layers of stitches under the skin and uses stitches or metal staples to close the skin. A large bandage is placed on the incision, and you are then returned to the recovery room.
View animation of hemiarthroplasty
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hemiarthroplasty of the hip include
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- loosening
- continued pain
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following any joint replacement surgery, such as hemiarthroplasty. The chance of getting an infection following hemiarthroplasty is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
Dislocation
The operation requires the surgeon to open up the hip joint. This puts the hip at risk of dislocating if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the joint, but there is always a risk. Your physical therapist will instruct you how to avoid activities and positions which may have a tendency to cause a hip dislocation. A hip that dislocates more than once may have to be revised (which means another operation) to make it more stable. Patients with diseases such as Parkinson’s or Alzheimer’s are at higher risk of dislocating their hip.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Loosening
The main reason that joint implants eventually fail continues to be loosening of the metal or cement from the bone. Great advances have been made in extending how long artificial replacement parts will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from replacement parts for the hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the hip.
Continued Pain
A hemiarthroplasty only replaces the ball portion of the hip joint. This means that the metal ball is constantly rubbing against the articular cartilage inside of your natural hip socket. The socket may become arthritic as the cartilage wears out over time. If this occurs, the hip will become painful just like any other arthritic joint. If the pain becomes unbearable, the hemiarthroplasty may need to be converted to a complete artificial joint. This means that the socket will be replaced with a new artificial socket. The metal stem may not need to be replaced.
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physical therapy treatments are scheduled one to three times each day as long as you are in the hospital. Your first treatment is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you’ll begin walking longer distances using your crutches or walker. Most patients are safe to put comfortable weight down when standing or walking. If your surgeon used a noncemented prosthesis, you may be instructed to limit the weight you bear on your foot when you are up and walking.
Your therapist will review your hip precautions. Your therapist will also go over exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
Patients are usually able to go home after spending four to seven days in the hospital. You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely, and consistently remember to use your hip precautions. Patients who still need extra care may be sent to a different hospital unit until they are safe and ready to go home.
Most orthopedic surgeons recommend that you have routine checkups after this type of procedure. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends.
Patients who have hemiarthroplasty surgery will sometimes have episodes of pain, but when you have a period that lasts longer than a couple of weeks you should consult your doctor. During the examination, the orthopedic surgeon will try to determine why you are feeling pain. X-rays may be taken of your hip to compare with the ones taken earlier to see whether the prosthesis shows any evidence of loosening.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will review your exercise program, continue working with you on your hip precautions, and make recommendations about your safety.
These recommendations may include that you use a raised commode seat and bathtub bench, and that you raise the surfaces of couches and chairs. This keeps your hip from bending too far when you sit down. Bath benches and handrails can improve safety in the bathroom. Other suggestions may include the use of strategic lighting and the removal of loose rugs or electrical cords from the floor.
During this period, you should continue to use your walker or crutches as instructed. If you had a cemented prosthesis, you’ll advance the weight you place through your sore leg as much as you feel comfortable. If the prosthesis was not cemented, your surgeon may want you to place only the toes of the operated leg down for up to six weeks after surgery. Most patients progress to using a cane in three to four weeks.
Your staples will be removed two weeks after surgery. Patients are usually able to drive within three weeks and walk without a walking aid by six weeks. Upon the approval of the physician, patients are generally able to resume sexual activity one to two months after surgery.
Home therapy visits end when you are safe to get out of the house, which may take up to three weeks.
The need for physical therapy usually ends when home care is completed. A few additional visits in outpatient physical therapy may be needed for patients who still have problems walking or who need to get back to heavier types of work or activities.
Your therapist may use heat, ice, or electrical stimulation if you are still having swelling or pain.
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
Many patients have less pain and better mobility after having hip replacement surgery. Your therapist will work with you to help keep your hip joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new prosthesis. Heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may need to consider alternate jobs to avoid work activities that require heavy demands of lifting, crawling, and climbing.
The therapist’s goal is to help you maximize strength, walk normally, and improve your ability to do your activities. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Hip Replacement
A Patient’s Guide to Artificial Joint Replacement of the Hip
Introduction
A hip that is painful as a result of osteoarthritis (OA) can severely affect your ability to lead a full, active life. Over the last 25 years, major advancements in hip replacement have improved the outcome of the surgery greatly. Hip replacement surgery (also called hip arthroplasty) is becoming more and more common as the population of the world begins to age.
This guide will help you understand
- what your surgeon hopes to achieve
- what happens during the procedure
- what to expect after your operation
Related Document: A Patient’s Guide to Osteoarthritis of the Hip
Anatomy
How does the hip normally work?
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thigh bone, known as the femoral head. The thick muscles of the buttock at the back and the thick muscles of the thigh in the front surround the hip.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
Related Document: A Patient’s Guide to Hip Anatomy
Rationale
What does the surgeon hope to achieve?
The main reason for replacing any arthritic joint with an artificial joint is to stop the bones from rubbing against each other. This rubbing causes pain. Replacing the painful and arthritic joint with an artificial joint gives the joint a new surface, which moves smoothly without causing pain. The goal is to help people return to many of their activities with less pain and greater freedom of movement.
Preparation
How should I prepare for surgery?
The decision to proceed with surgery should be made jointly by you and your surgeon only after you feel that you understand as much about the procedure as possible.
Once the decision to proceed with surgery is made, several things may need to be done. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation. You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery.
One purpose of the preoperative physical therapy visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the movement and strength of each hip.
A second purpose of the preoperative therapy visit is to prepare you for your upcoming surgery. You will begin to practice some of the exercises you will use just after surgery. You will also be trained in the use of either a walker or crutches. Whether the surgeon uses a cemented or noncemented approach may determine how much weight you will be able to apply through your foot while walking.
This procedure requires the surgeon to open up the hip joint during surgery. This puts the hip at some risk for dislocation after surgery. To prevent dislocation, patients follow strict guidelines about which hip positions to avoid (called hip precautions). Your therapist will review these precautions with you during the preoperative visit and will drill you often to make sure you practice them at all times for at least six weeks. Some surgeons give the OK to discontinue the precautions after six to 12 weeks because they feel the soft tissues have gained enough strength by this time to keep the joint from dislocating.
Related Document: A Patient’s Guide to Artificial Hip Dislocation Precautions
Finally, the therapist assesses any needs you will have at home once you’re released from the hospital.
You may be asked to donate some of your own blood before the operation. This blood can be donated three to five weeks before the operation, and your body will make new blood cells to replace the loss. At the time of the operation, if you need to have a blood transfusion you will receive your own blood back from the blood bank.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the artificial hip itself.
The Artificial Hip
There are two major types of artificial hip replacements:
- cemented prosthesis
- uncemented prosthesis
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis bears a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone.
Both are still widely used. In some cases a combination of the two types is used in which the ball portion of the prosthesis is cemented into place, and the socket not cemented. The decision about whether to use a cemented or uncemented artificial hip is usually made by the surgeon based on your age and lifestyle, and the surgeon’s experience.
Each prosthesis is made of two main parts. The acetabular component (socket) replaces the acetabulum. The acetabular component is made of a metal shell with a plastic inner liner that provides the bearing surface.
The plastic used is so tough and slick that you could ice skate on a sheet of it without much damage to the material.
The femoral component (stem and ball) replaces the femoral head. The femoral component is made of metal. Sometimes, the metal stem is attached to a ceramic ball.
The Operation
The surgeon begins by making an incision on the side of the thigh to allow access to the hip joint. Several different approaches can be used to make the incision. The choice is usually based on the surgeon’s training and preferences.
Once the hip joint is entered, the surgeon dislocates the femoral head from the acetabulum. Then the femoral head is removed by cutting through the femoral neck with a power saw. Attention is then turned toward the socket. The surgeon uses a power drill and a special reamer (a cutting tool used to enlarge or shape a hole) to remove cartilage from inside the acetabulum. The surgeon shapes the socket into the form of a half-sphere. This is done to make sure the metal shell of the acetabular component will fit perfectly inside. After shaping the acetabulum, the surgeon tests the new component to make sure it fits just right.
In the uncemented variety of artificial hip replacement, the metal shell is held in place by the tightness of the fit or by using screws to hold the shell in place. In the cemented variety, a special epoxy-type cement is used to anchor the acetabular component to the bone.
To begin replacing the femur, special rasps (filing tools) are used to shape the hollow femur to the exact shape of the metal stem of the femoral component. Once the size and shape are satisfactory, the stem is inserted into the femoral canal.
Again, in the uncemented variety of femoral component the stem is held in place by the tightness of the fit into the bone (similar to the friction that holds a nail driven into a hole that is slightly smaller than the diameter of the nail). In the cemented variety, the femoral canal is enlarged to a size slightly larger than the femoral stem, and the epoxy-type cement is used to bond the metal stem to the bone.
The metal ball that makes up the femoral head is then inserted.
Once the surgeon is satisfied that everything fits properly, the incision is closed with stitches. Several layers of stitches are used under the skin, and either stitches or metal staples are then used to close the skin. A bandage is applied to the incision, and you are returned to the recovery room.
View animation of removing the femoral head
View animation of reaming the acetabulum
View animation of testing the new acetabular component
View animation of shaping the femur
View animation of inserting the stem
View animation of inserting the metal ball
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following hip replacement surgery include
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- loosening
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of Pulmonary Embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but it is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection can be a very serious complication following artificial joint replacement surgery. The chance of getting an infection following total hip replacement is probably around one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
Dislocation
Just like your real hip, an artificial hip can dislocate if the ball comes out of the socket. There is a greater risk just after surgery, before the tissues have healed around the new joint, but there is always a risk. The physical therapist will instruct you very carefully how to avoid activities and positions which may have a tendency to cause a hip dislocation. A hip that dislocates more than once may have to be revised to make it more stable. This means another operation.
Loosening
The main reason that artificial joints eventually fail continues to be the loosening of the metal or cement from the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision. Hopefully, you can expect 12 to 15 years of service from an artificial hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to revise the hip.
Related Document: A Patient’s Guide to Revision Arthroplasty of the Hip
After Surgery
What happens after surgery?
After surgery, your hip will be covered with a padded dressing. Special boots or stockings are placed on your feet to help prevent blood clots from forming. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in.
If your surgeon used a general anesthesia, a nurse or respiratory therapist will visit your room to guide you in a series of breathing exercises. You’ll use an incentive spirometer to improve breathing and avoid possible problems with pneumonia.
Physical therapy treatments are scheduled one to three times each day as long as you are in the hospital. Your first treatment is scheduled soon after you wake up from surgery. Your therapist will begin by helping you move from your hospital bed to a chair. By the second day, you’ll begin walking longer distances using your crutches or walker. Most patients are safe to put comfortable weight down when standing or walking. However, if your surgeon used a noncemented prosthesis, you may be instructed to limit the weight you bear on your foot when you are up and walking.
Your therapist will review exercises to begin toning and strengthening the thigh and hip muscles. Ankle and knee movements are used to help pump swelling out of the leg and to prevent the formation of blood clots.
Patients are usually able to go home after spending four to seven days in the hospital. You’ll be on your way home when you can demonstrate a safe ability to get in and out of bed, walk up to 75 feet with your crutches or walker, go up and down stairs safely. and consistently remember to use your hip precautions. Patients who still need extra care may be sent to a different hospital unit until they are safe and ready to go home.
Most orthopedic surgeons recommend that you have checkups on a routine basis after your artificial joint replacement. How often you need to be seen varies from every six months to every five years, according to your situation and what your surgeon recommends.
Patients who have an artificial joint will sometimes have episodes of pain, but if you have a period that lasts longer than a couple of weeks you should consult your surgeon. During the examination, the orthopedic surgeon will try to determine why you are feeling pain. X-rays may be taken of your artificial joint to compare with the ones taken earlier to see whether the joint shows any evidence of loosening.
Rehabilitation
What should I expect during my recovery?
After you are discharged from the hospital, your therapist may see you for one to six in-home treatments. This is to ensure you are safe in and about the home and getting in and out of a car. Your therapist will review your exercise program, continue working with you on your hip precautions, and make recommendations about your safety.
These safety tips include using raised commode seats and bathtub benches, and raising the surfaces of couches and chairs. This keeps your hip from bending too far when you sit down. Bath benches and handrails can improve safety in the bathroom. Other suggestions may include the use of strategic lighting and the removal of loose rugs or electrical cords from the floor.
You should use your walker or crutches as instructed. If you had a cemented procedure, you’ll advance the weight you place through your sore leg as much as you feel comfortable. If you had a noncemented procedure, your surgeon may want you to place only the toes of your operated leg down for up to six weeks after surgery. Most patients progress to using a cane in three to four weeks.
Your staples will be removed two weeks after surgery. Patients are usually able to drive within three weeks and walk without a walking aid by six weeks. Upon the approval of the surgeon, patients are generally able to resume sexual activity by one to two months after surgery.
Home therapy visits end when you are safe to get out of the house, which may take up to three weeks.
The need for physical therapy usually ends when home care is completed. But a few additional visits in outpatient physical therapy may be needed for patients who have problems walking or who need to get back to heavier types of work or activities.
Your therapist may use heat, ice, or electrical stimulation to reduce any swelling or pain.
Therapists sometimes treat their patients in a pool. Exercising in a swimming pool puts less stress on the hip joint, and the buoyancy lets you move and exercise easier. Once you’ve gotten your pool exercises down and the other parts of your rehab program advance, you may be instructed in an independent program.
When you are safe in putting full weight through the leg, several types of balance exercises can be chosen to further stabilize and control the hip.
Finally, a select group of exercises can be used to simulate day-to-day activities, such as going up and down steps, squatting, and walking on uneven terrain. Specific exercises may then be chosen to simulate work or hobby demands.
Many patients have less pain and better mobility after having hip replacement surgery. Your therapist will work with you to help keep your new joint healthy for as long as possible. This may require that you adjust your activity choices to keep from putting too much strain on your new hip joint. Heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may need to consider alternate jobs to avoid work activities that require heavy demands of lifting, crawling, and climbing.
The therapist’s goal is to help you maximize strength, walk normally, and improve your ability to do your activities. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.