Elbow
Elbow Dislocation
A Patient’s Guide to Elbow Dislocation
Introduction
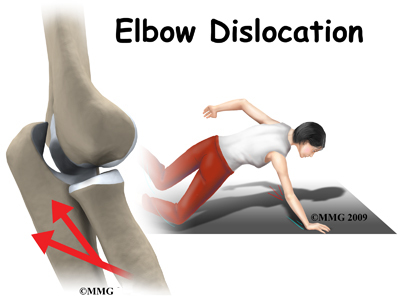
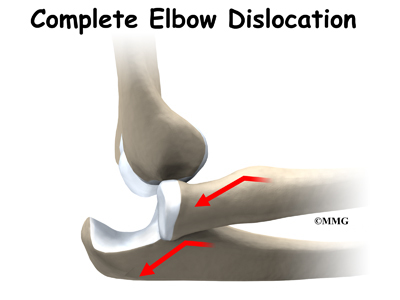
When the joint surfaces of an elbow are forced apart, the elbow is dislocated. The elbow is the second most commonly dislocated joint in adults (after shoulder dislocation). Elbow dislocation can be complete or partial. A partial dislocation is referred to as a subluxation. The amount of force needed to cause an elbow dislocation is enough to cause a bone fracture at the same time. These two injuries (dislocation-fracture) often occur together.
This guide will help you understand
- how the condition develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
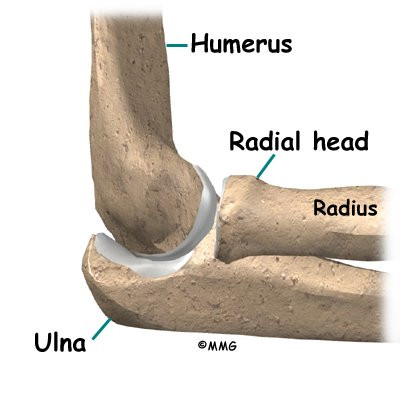
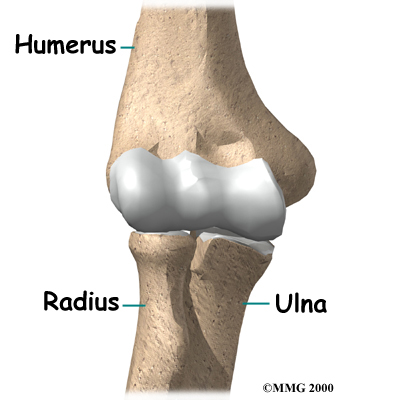
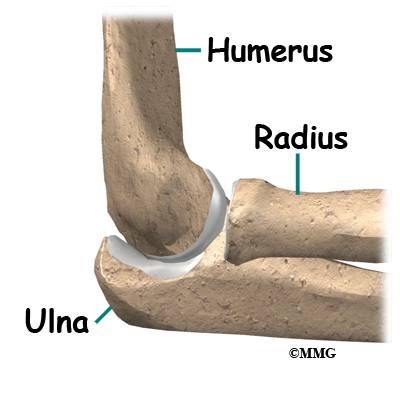
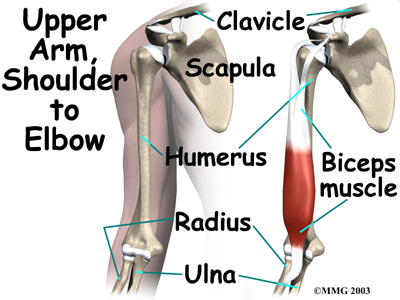
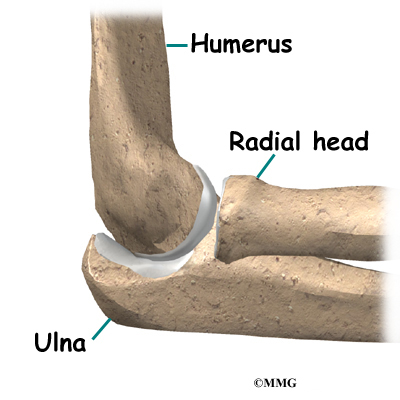
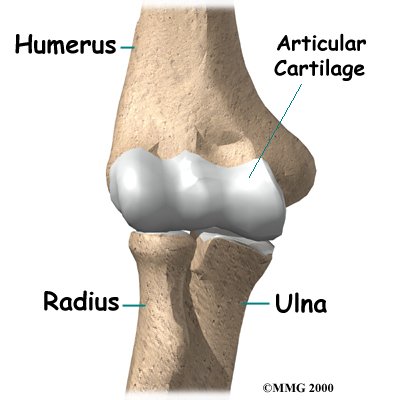
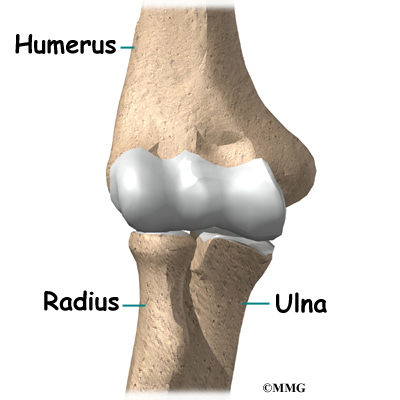
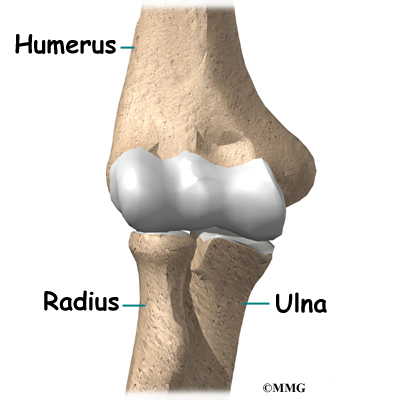
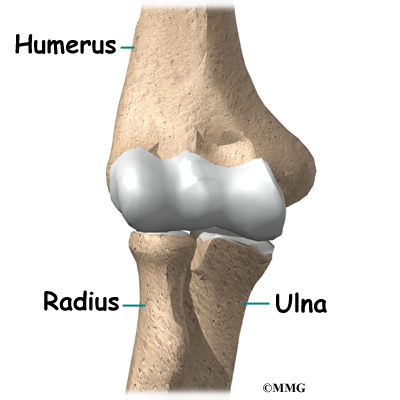
The bones of the elbow are the humerus (the upper arm bone), the ulna (the larger bone of the forearm, on the opposite side of the thumb), and the radius (the smaller bone of the forearm on the same side as the thumb).
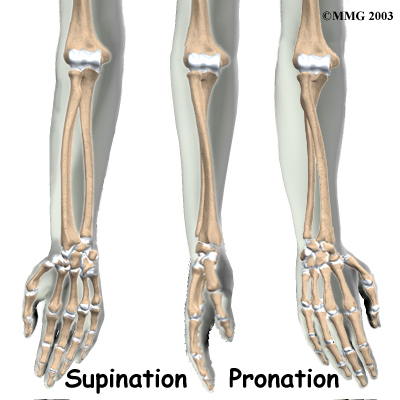
The elbow itself is essentially a hinge joint, meaning it bends and straightens like a hinge. But there is a second joint where the end of the radius (the radial head) meets the humerus. This joint is complicated because the radius has to rotate so that you can turn your hand palm up and palm down. At the same time, it has to slide against the end of the humerus as the elbow bends and straightens. The joint is even more complex because the radius has to slide against the ulna as it rotates the wrist as well. As a result, the end of the radius at the elbow is shaped like a smooth knob with a cup at the end to fit on the end of the humerus. The edges are also smooth where it glides against the ulna.
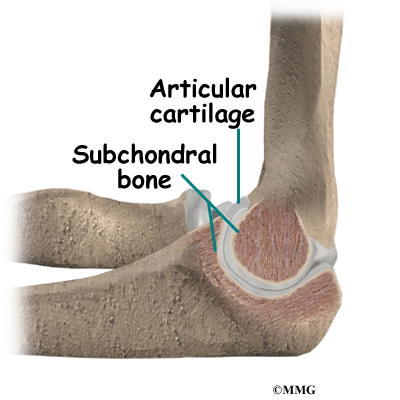
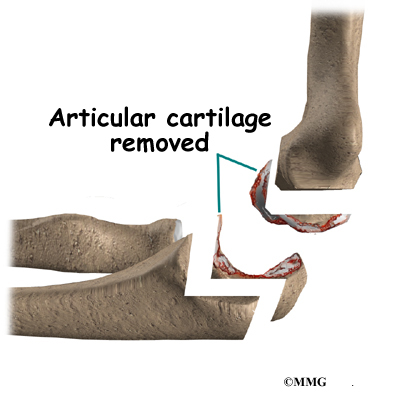
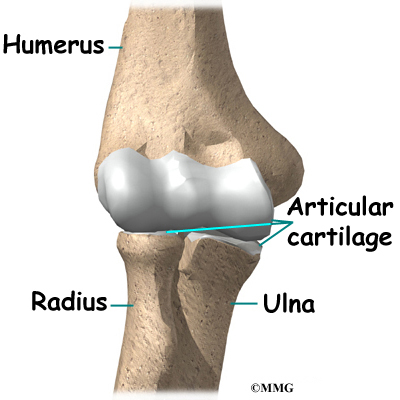
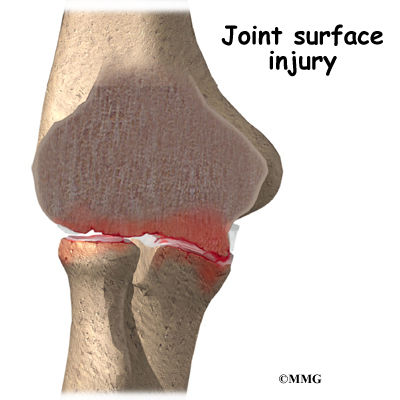
Articular cartilage is the material that covers the ends of the bones of any joint. Articular cartilage can be up to one-quarter of an inch thick in the large, weight-bearing joints. It is a bit thinner in joints such as the elbow, which don’t support weight. Articular cartilage is white, shiny, and has a rubbery consistency. It is slippery, which allows the joint surfaces to slide against one another without causing any damage. In the elbow, articular cartilage covers the end of the humerus, the end of the radius, and the end of the ulna.
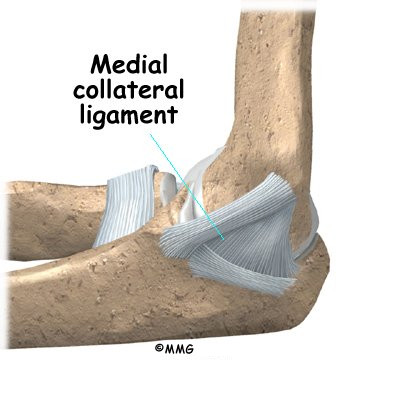
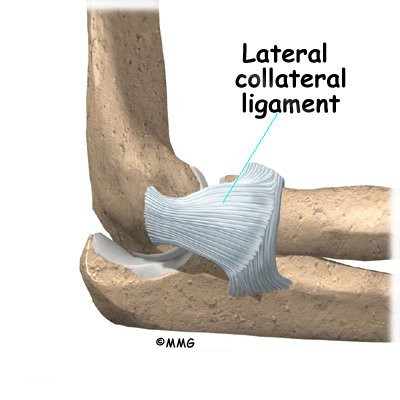
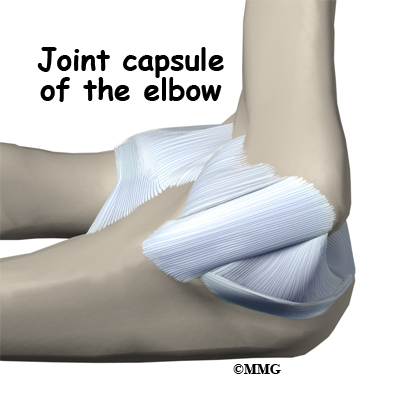
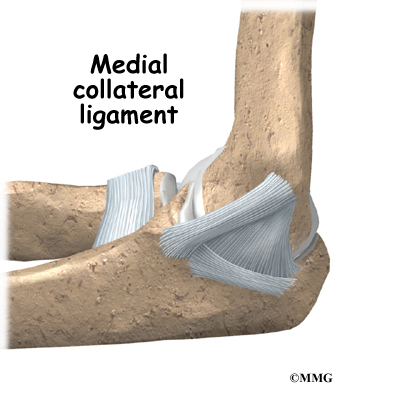
There are several important ligaments in the elbow. Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine together to form a joint capsule. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid called synovial fluid.
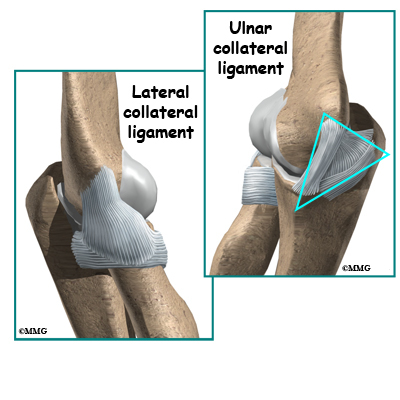
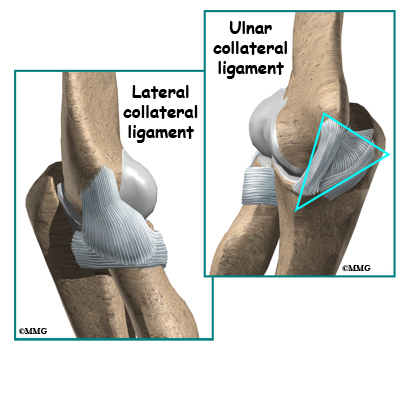
In the elbow, two of the most important ligaments are the medial collateral ligament and the lateral collateral ligament. The medial collateral is on the inside edge of the elbow, and the lateral collateral is on the outside edge. Together these two ligaments connect the humerus to the ulna and keep it tightly in place as it slides through the groove at the end of the humerus. These ligaments are the main source of stability for the elbow. They can be torn when there is an injury to or dislocation of the elbow. If they do not heal correctly the elbow can be too loose, or unstable.
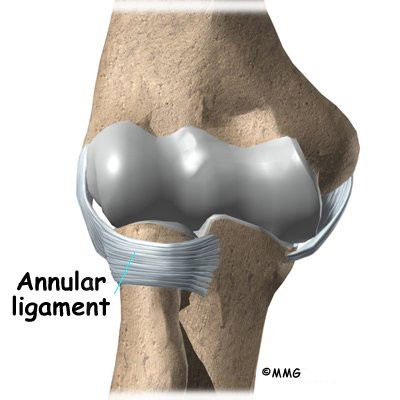
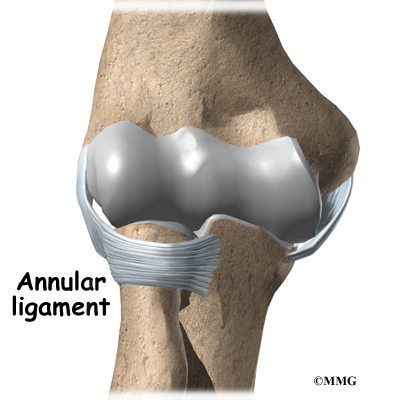
There is also an important ligament called the annular ligament that wraps around the radial head and holds it tight against the ulna. The word annular means ring-shaped. The annular ligament forms a ring around the radial head as it holds it in place. This ligament can be torn when the entire elbow or just the radial head is dislocated.
Causes
What causes this condition?
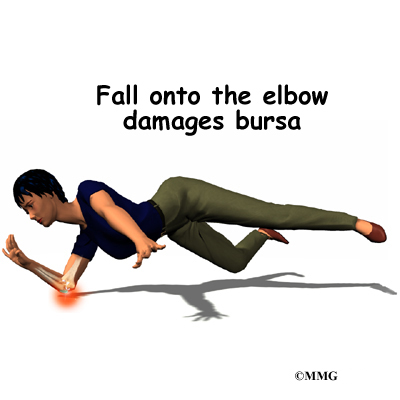
Elbow dislocation is often the result of trauma. The most common trauma resulting in an elbow dislocation is a fall onto an outstretched hand and arm. When the hand hits the ground, the force is transmitted through the forearm to the elbow. This force pushes the elbow out of its socket.
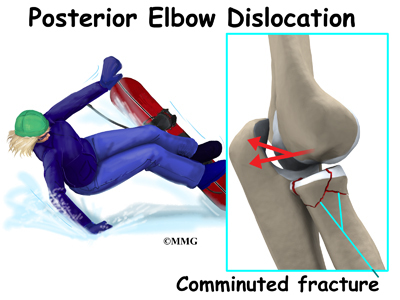
This can also result in a fracture/dislocation. About half of all elbow dislocations in teens and young adults occur as a result of a sports activity. The most common elbow dislocations are associated with sports such as gymnastics, cycling, roller-blading, or skateboarding.
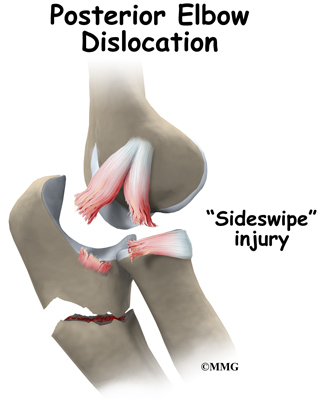
Dislocation can also occur from a sideswipe injury. This type of injury occurs when the driver of an automobile has the elbow out the open window during a car accident. The force of the impact causes a severe fracture-dislocation of the elbow.
Symptoms
What are the symptoms?
If the elbow is fully dislocated, it will look out of joint. There may be dimples or indentations of the skin over the dislocation where the bones have shifted position. Pain can be intense until the arm is relocated. The pain is often relieved immediately after the joint is put back in place. There may be some residual tenderness around the joint.
If ligaments or other soft tissues are torn, there can be swelling and bruising around the elbow. Bruising is not immediately obvious but appears several days after the injury. Injury to any of the three nerves that cross the elbow (median, ulnar, radial nerves) can cause neurologic symptoms such as numbness, tingling, and/or weakness of the forearm, wrist, and hand. If a bone fracture is also involved the fracture can cut or damage a nerve causing temporary or permanent paralysis.
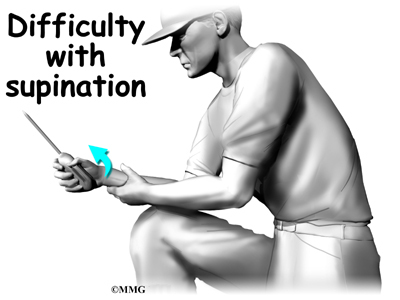
Pain and an inability to straighten the elbow or pain when turning the hand the palm up (supination) is typical. There is often tenderness along the lateral aspect of the elbow (side of the elbow away from the body).
Diagnosis
How do doctors diagnose this condition?
The history and physical examination are probably the most important tools the physician uses to guide his or her diagnosis. Moving the elbow passively is painful, especially extension and supination. The doctor will check for any signs of injury to the nerves or blood vessels.
X-ray is the best way to look for dislocation or fracture-dislocation.
After the joint is relocated, other imaging studies may be ordered to look for damage to the joint cartilage, bone, ligaments, and other soft tissues. If bone detail is difficult to identify on an X-ray, a computed tomography (CT) scan may be done. If it is important to evaluate the ligaments, a magnetic resonance image (MRI) can be helpful.
Treatment
What treatment options are available?
Nonsurgical Treatment
It is possible for the elbow to relocate by itself. This is more likely when there is a subluxation, rather than a complete dislocation. Sometimes the elbow can be reduced or put back in place by a trained medical person applying a quick motion to the forearm. There are several different methods used for manual (closed) reduction. Closed reduction refers to the fact that the elbow can be put back in joint without surgery. An open incision is not needed.
Manual reduction can be done in an emergency on site (e.g., at an athletic event or car accident) by a trained medical person but usually the procedure is done in a clinic or hospital setting. You would be given medications first to help with the pain.
Surgery
If there is too much swelling, it may be necessary to delay surgery for a few days up to a week. The elbow will be reduced right away and the arm immobilized while waiting for the swelling to subside.
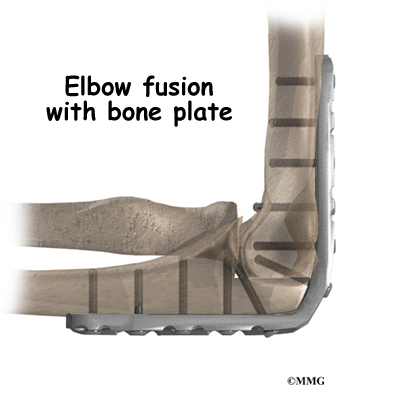
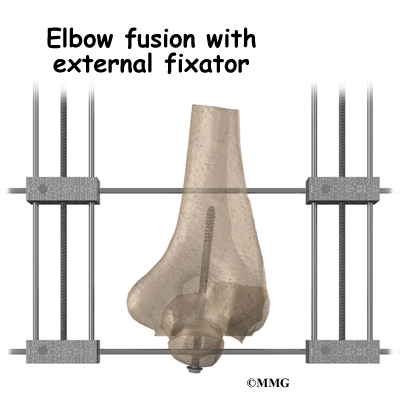
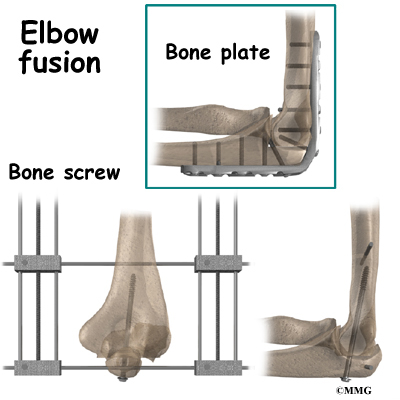
If there has been damage to the bones and/or ligaments, surgery may be needed to restore alignment and function. The type of surgery depends on the extent of the damage. Wires, pins, or even an external fixation device may be needed to hold everything together until healing occurs.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
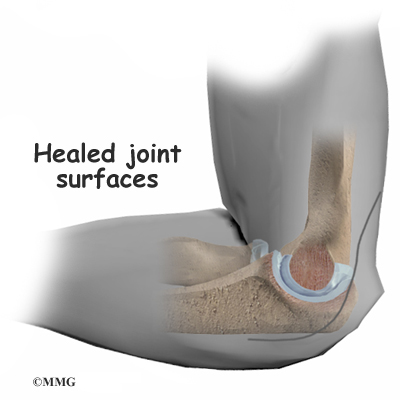
Simple elbow dislocations heal well with few (if any) problems. You may notice a slight loss of elbow motion, especially when trying to straighten the arm. This should not affect your overall motion and function. X-rays may be taken while the elbow heals. This will show if the bones of the elbow joint are healing in a reduced position with good alignment.
The arm may be immobilized for 10 to 14 days to allow the ligament to heal. Gentle range of motion may be allowed during that time but you should rely on your physician to advise you. Type of activities and movements allowed are determined according to the type of injury that’s present.
After immobilization, physical therapy may begin. The goal is to restore normal motion, joint proprioception (sense of position), and motor control. The program will progress to include strengthening.
Rehabilitation for the athlete includes sport-specific training is part of the rehab program. Your physical therapist will guide you through this process. Most athletes can resume sports participation three to six weeks after an elbow dislocation. The timing of return to sports depends on the type of sport (e.g., throwing sports may require a longer rehab). Dislocation of the dominant hand may require longer rehab before full motion and strength are restored.
Some athletes continue to wear a protective splint and/or use taping to stabilize the joint during the transition back into action. This can help protect the joint during motion and activity during the final phase of healing.
It’s best to avoid any further traction on the elbow until healing has occurred. Pulling a heavy door open, carrying a heavy purse, or lifting a heavy backpack are a few examples of activities and movements that put a traction force through the elbow. These kinds of movements should be avoided until healing occurs
After Surgery
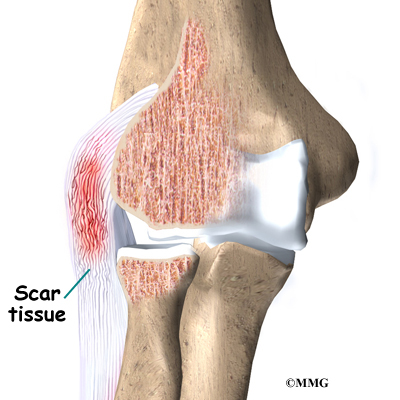
Post-operative immobilization is often required, especially for complex injuries. This could be a cast, dynamic splint, or postoperative range-of-motion (ROM) brace. The adjustable ROM brace is used to improve elbow motion gradually while allowing soft tissue healing. It helps minimize scar tissue formation and may contribute to fewer complications (such as arthritis) later on.
After immobilization, physical therapy may begin. The goal is to restore normal motion, joint proprioception (sense of position), and motor control. The program will progress to include strengthening. Rely on your doctor and therapist to guide you through the healing process.
As in conservative care, some athletes continue to wear a protective splint and/or use taping to stabilize the joint during the transition back into action. This can help protect the joint during motion and activity during the final phase of healing.
It’s best to avoid any further traction on the elbow until healing has occurred. Pulling a heavy door open, carrying a heavy purse, or lifting a heavy backpack are a few examples of activities and movements that put a traction force through the elbow. These kinds of movements should be avoided until healing occurs. Your doctor and/or therapist will advise you as you progress through the healing process.
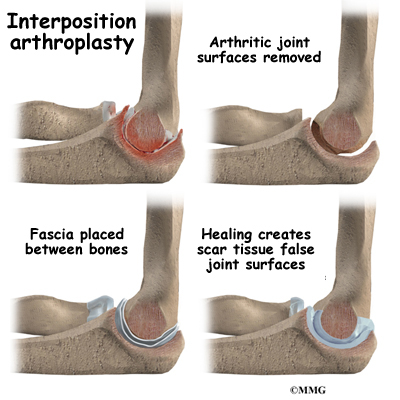
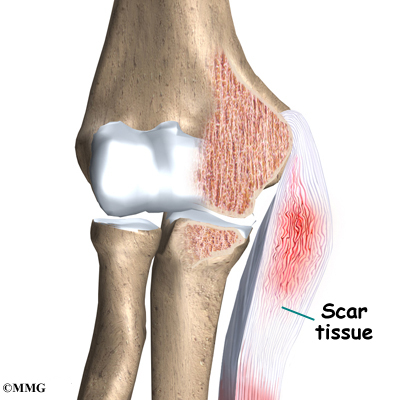
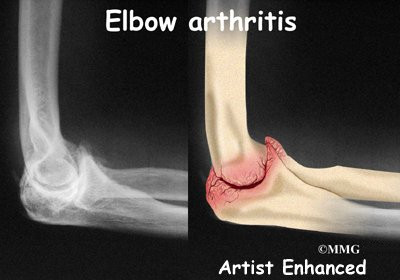
Scar tissue can cause a stiff elbow. Recurrent dislocation is also possible. If either of these problems develops, additional reconstructive surgery may be needed. For some patients, arthritis is a long-term result of elbow injury. This is more likely if there is a history of recurrent elbow dislocations.
Ulnar Collateral Ligament Reconstruction (Tommy John Surgery)
A Patient’s Guide to Ulnar Collateral Ligament Reconstruction (Tommy John Surgery)
Introduction
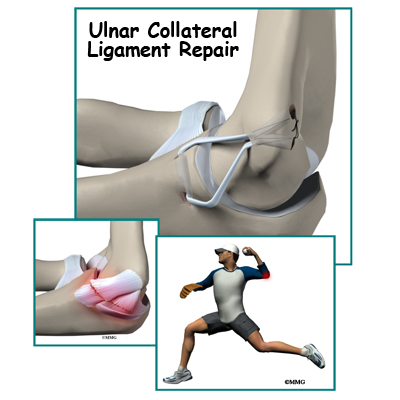
The doctors call it a UCLR ulnar collateral ligament reconstruction. Baseball players and fans call it Tommy John surgery — named after the pitcher (Los Angeles Dodgers) who was the first to have the surgery in 1974. It is one of the major advancements in sports medicine in the last quarter century.
This guide will help you understand:
- what your surgeon hopes to achieve
- how do I prepare for this procedure
- what happens during the procedure
- what to expect as you recover
Anatomy
What’s the normal anatomy of the elbow?
The bones of the elbow are the humerus (the upper arm bone), the ulna (the larger bone of the forearm, on the opposite side of the thumb), and the radius (the smaller bone of the forearm on the same side as the thumb).
There are several important ligaments in the elbow. Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine together to form a joint capsule. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid called synovial fluid.
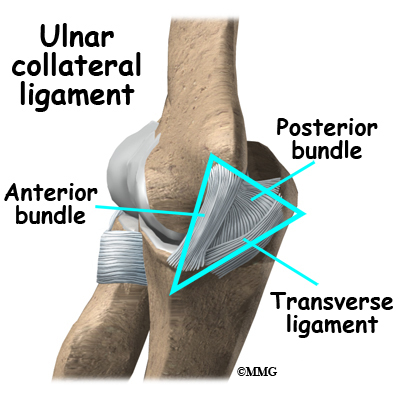
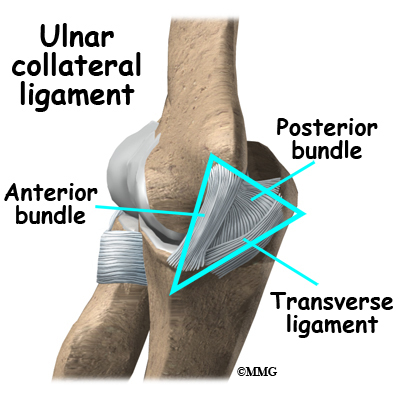
In the elbow, two of the most important ligaments are the ulnar collateral ligament (UCL) and the lateral collateral ligament. The UCL is also known as the medial collateral ligament. The ulnar collateral ligament is on the medial (the side of the elbow that’s next to the body) side of the elbow, and the lateral collateral is on the outside. The ulnar collateral ligament is a thick band of ligamentous tissue that forms a triangular shape along the medial elbow. It has an anterior bundle, posterior bundle, and a thinner, transverse ligament.
Together these two ligaments, the ulnar (or medial) collateral and the lateral collateral, connect the humerus to the ulna and keep it tightly in place as it slides through the groove at the end of the humerus. These ligaments are the main source of stability for the elbow. They can be torn when there is an injury or dislocation of the elbow. If they do not heal correctly the elbow can be too loose or unstable. The ulnar collateral ligament can also be damaged by overuse and repetitive stress, such as the throwing motion.
Rationale
What does my surgeon hope to achieve?
Surgical treatment is designed to restore medial stability of the elbow. Full return to previous activities is the main goal. This is especially true for those athletes who want to remain active and competitive in sports. Many throwing athletes who develop this condition have pain in the elbow during and after throwing activities. They may also develop numbness and tingling in the hand due to stretching of the ulnar nerve at the elbow. Successful treatment of the condition should improve or eliminate these symptoms.
Who can benefit from this procedure?
Throwing athletes (especially baseball pitchers) at the college and professional level are affected most often by this injury requiring surgery. Minor league athletes and younger sports participants may also develop this injury requiring surgical care. Anyone with this injury who has not benefited (gotten better) with conservative care is a candidate for surgery.
Preparation
How should I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Reconstruction
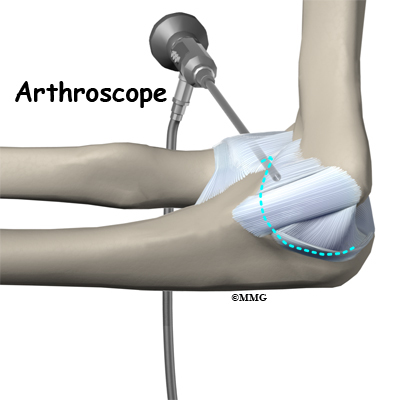
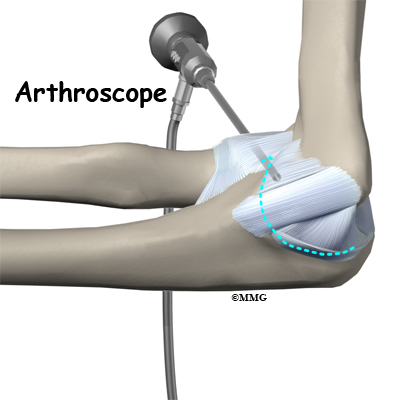
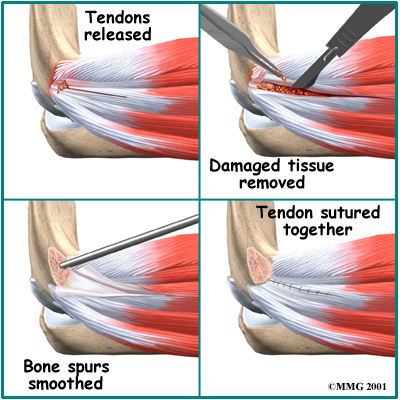
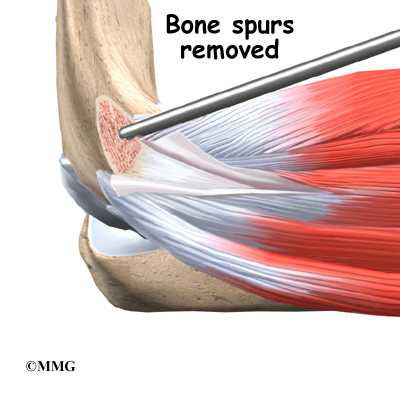
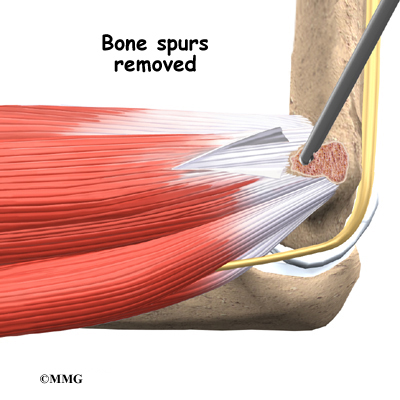
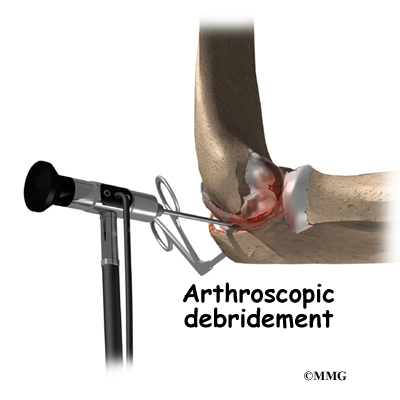
If you are having problems that may be coming from inside the joint, such as arthritis and loose bodies, your surgeon may perform an arthroscopy before the actual reconstruction procedure is done. During this procedure, a small TV camera is inserted into the elbow joint through two or three small (1/4 inch) incisions. Using special instruments your surgeon will be able to evaluate the joint, remove any loose bodies and bone spurs that may be causing problems. Arthroscopy is not always necessary.
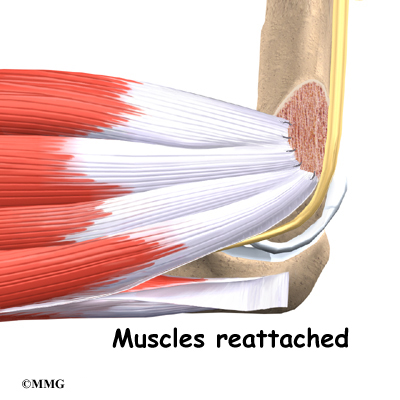
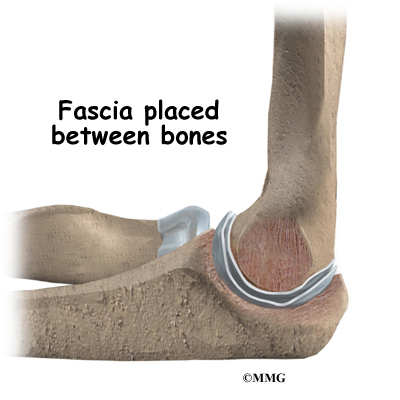
The reconstruction is performed through an incision on the medial (inside) side of the elbow joint. The damaged ulnar collateral ligament along the medial side of the elbow is replaced with a tendon harvested from somewhere else in the body. The tendon graft can come from the patient’s own forearm, hamstring, knee, or foot. This is called an autograft.
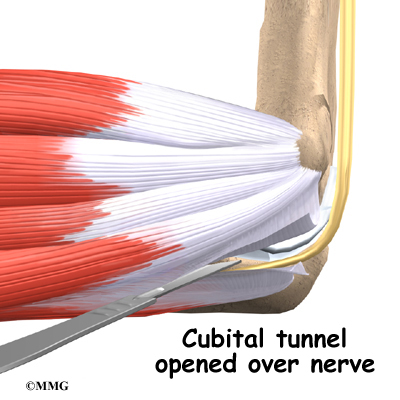
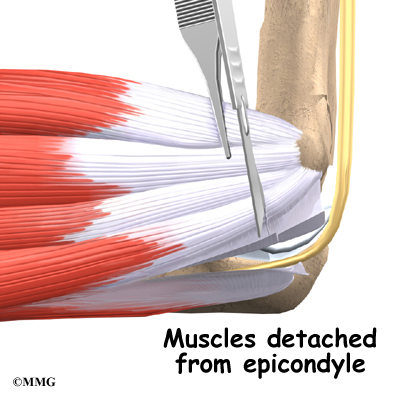
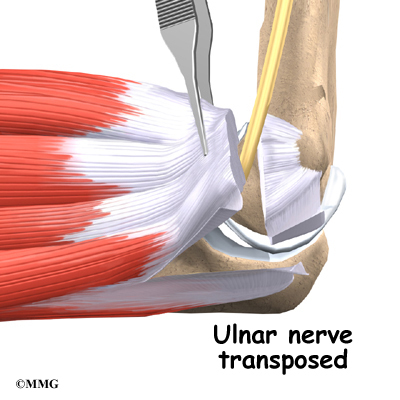
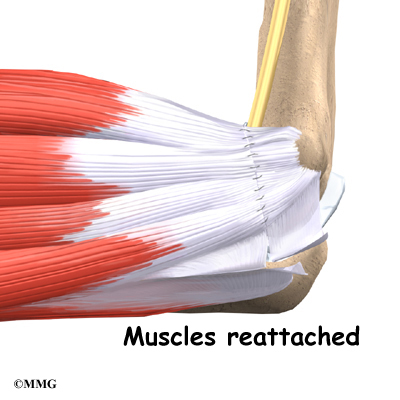
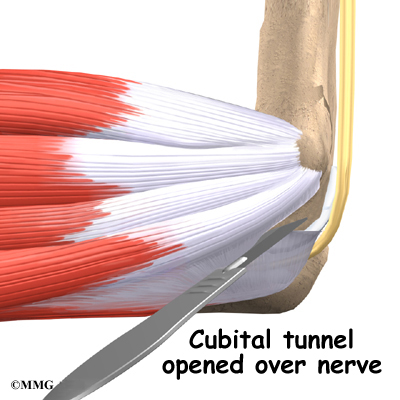
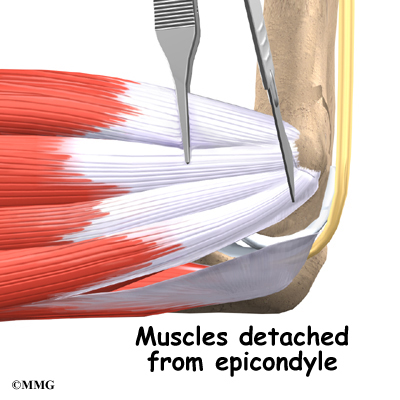
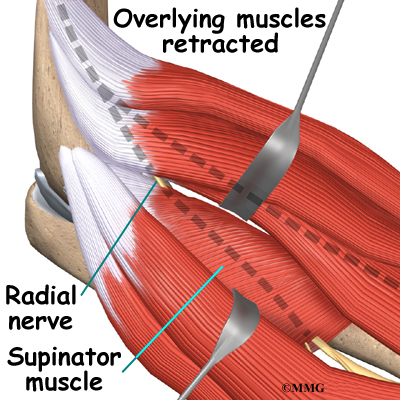
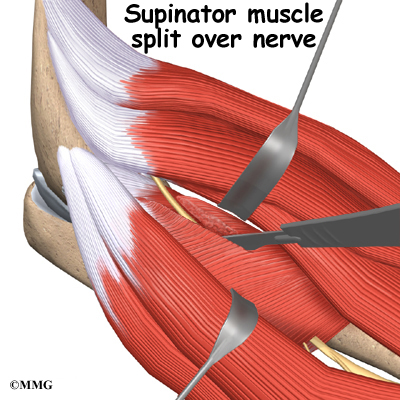
Over the years the way that surgeons perform this operation have improved. In the early days, the muscles on the inside of the elbow joint and forearm (the flexor muscles) were completely detached from the humerus and the ulnar nerve was re-routed from its normal position in the cubital tunnel on the back side of the elbow. This was done to be able to see the joint and protect the nerve. As surgeons have understood this problem more completely, these two parts of the operation have been eliminated. Now, the flexor muscles are not detached, but are split and retracted to allow the surgeon to see the areas of the elbow joint required to perform the operation successfully. The ulnar nerve is re-routed only if the patient was having symptoms of ulnar nerve damage before the operation. These improvements have resulted in a less invasive procedure with a decreased rate of complications.
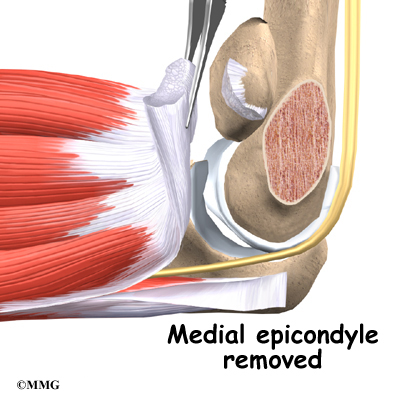
One common technique used to replace the damaged ulnar collateral ligament is called the docking technique. The surgeon drills two holes in the ulna and three in the medial epicondyle (the small bump of bone on the inside of the elbow at the end of the humerus). The two holes in the ulna form a tunnel that the tendon graft will be looped through. The three holes in the medial epicondyle form a triangle. The bottom hole will be bigger than the top two holes, so that the surgeon can slide the end of the tendon graft into the bottom hole. The two top holes are used to pull the tendon graft into the tunnel using sutures that are attached to the graft and threaded through the two holes.
After the tendon is harvested, sutures are attached to both ends. The tendon is looped through the lower tunnel formed in the ulna, and stretched across the elbow joint. The two sutures attached to the ends of the graft are threaded into the larger bottom tunnel in the medial epicondyle and each is threaded out one of the upper, smaller holes.
Using these two sutures, the surgeon pulls the end of the graft farther into the upper tunnel until the amount of tension is correct to hold the joint in position. The surgeon carefully puts the elbow through its full arc of motion and readjusts the tension on the sutures until he is satisfied that the proper ligamentous tension is restored. The two sutures are tied together to hold the tendon graft in that position.
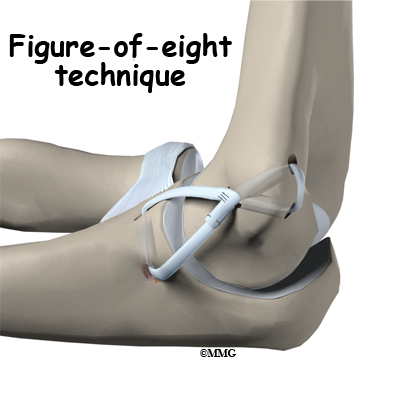
Another common technique to reconstruct the ulnar collateral ligament is the figure of eight technique. In this technique, the tendon graft is threaded through two pairs of holes – two drilled in the medial epicondye and two in the ulna. The graft is looped through the holes in a figure of eight fashion. The two ends of the tendon are sutured to the tendon itself.
If there is any concern that the ulnar nerve has been stretched and damaged due to the instability (as mentioned above), it may be re-routed so that it runs in front of the elbow joint rather than through the cubital tunnel in the back of the elbow. The incision is sutured together and the elbow is placed in a large bandage and splint.
There are several newer techniques being developed that hopefully will make the procedure even less invasive while retaining the success that the docking technique has enjoyed.
Complications
What might go wrong?
As with all surgical procedures, complications can occur. This topic doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are
- anesthesia complications
- infection
- nerve or blood vessel damage
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. You may be given antibiotics before the operation to reduce the risk of infection. If an infection occurs, you will most likely need more antibiotics to cure it.
Nerve or Blood Vessel Damage
Because the operation is performed so close to the nerves and vessels, it is possible to injure them during surgery. All of the nerves that travel down the arm pass across the elbow. The ulnar nerve is especially at risk for damage. Problems such as pain, numbness, and weakness in the arm and hand can be the consequences of nerve scarring, entrapment, or traction injury from the original trauma or from the procedure.
This condition is called a neuropathy. It may be temporary with gradual resolution of symptoms over a period of many months. If it doesn’t resolve on its own or with physical therapy, further surgery may be needed. In a small number of cases, this complication is permanent.
Studies show that up to half of the patients treated by ligament reconstruction are left with a loss of full motion. The main problem is a five to 10 degree loss of extension (the elbow doesn’t straighten all the way). This deformity does not affect strength or function. Earlier, more aggressive rehab may restore motion but at the risk of impaired healing of the graft.
Long-term complications can include chronic pain with throwing and chronic instability of the elbow.
After Surgery
What should I expect as I recover?
Repair or Reconstruction
The postoperative program is the same for repairs or reconstruction. At first your arm will be immobilized in a bulky dressing and a posterior splint for the first 10 days. It holds the elbow in a position of 90 degrees of flexion and neutral forearm rotation while leaving the wrist free to move. If non-absorbable sutures are used to close the incision, you may need these removed in 10 days.
You’ll have about a four-inch long incision along the inside of your elbow. There may be some discomfort after surgery. Your surgeon can give you pain medicine to control the discomfort. You should keep your elbow elevated above the level of your heart for several days to avoid swelling and throbbing. Keep your elbow propped up on a stack of pillows when sleeping or sitting.
Rehabilitation
What should I expect during my rehabilitation?
Gentle hand grip and shoulder and wrist mobilization exercises are allowed right away after surgery. Postoperative immobilization is discontinued in seven to 10 days at which time active range of motion for the elbow are started. Your surgeon may want you to wear a special hinged brace to protect the elbow.
Your therapist will instruct you in the active range of motion exercises to be done daily. Strengthening exercises for the entire upper quadrant (shoulder, arm, wrist, and hand) are included in the post-operative program. Specific strengthening exercises to help the athlete prepare for his or her particular sport begin around four months post-op. Up until this time, any stress to the medial elbow is avoided.
With careful adherence to the rehab program and completing the exercises daily, pitchers can get their full range of motion back in six to eight weeks. The program will progress to strength training with weight exercises. For the next four months, they can increase the weight they use and start doing exercises that emphasize all parts of their arm.
Flexibility, conditioning, coordination, and strengthening are part of the daily program. You may use ice after throwing sessions to help control inflammation. Plyometric exercises are used throughout the training period. An aerobic portion of the exercise program is also advised to help the athlete return to sports at the same level (or even higher level) as before the surgery. Good, overall physical condition is important to prevent injury as the athlete returns to sports activity.
At times in your rehab and recovery, you may find it necessary to move back to a previous level of training if symptoms of pain and swelling recur. Your therapist will guide you through the advancement (and regression) of your program. Additional training to restore normal joint proprioception (sense of joint position) and proper throwing mechanics is also provided.
Based on long-term studies of athletes over the years, the chances of a complete recovery after surgery are estimated at 85 to 90 percent. The process of rehabilitation to return to a level of playing equal to before the injury takes about a year for pitchers and about six months for position players.
The most often used criteria for resuming full (competitive) sports participation include 1) no pain with throwing, 2) full shoulder and elbow range of motion, 3) normal forearm strength, and 4) good throwing biomechanics.
The tendon graft is very weak immediately after the surgery. Transforming a tendon into a functioning ligament requires a very gradual rebuilding process. Athletes are encouraged to go slowly and not test the limits of the graft. The key to a successful UCLR (Tommy John) is to rehab for a long-term career, not to try for shortcuts during the first year of recovery.
Ulnar Collateral Ligament Injuries
A Patient’s Guide to Ulnar Collateral Ligament Injuries
Introduction
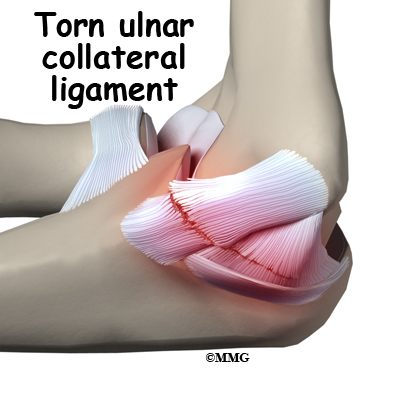
The ulnar collateral ligament (UCL) can become stretched, frayed or torn through the stress of repetitive throwing motions, causing ulnar collateral ligament injuries.
Professional pitchers have been the athletes treated most often for this problem. Javelin throwers and football, racquet sports, ice hockey, and water polo players have also been reported to injure the UCL. A fall on an outstretched arm can also lead to UCL rupture (often with elbow dislocation).
This guide will help you understand
- how the problem develops
- what causes this condition
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What parts of the elbow are affected?
The bones of the elbow are the humerus (the upper arm bone), the ulna (the larger bone of the forearm, on the opposite side of the thumb), and the radius (the smaller bone of the forearm on the same side as the thumb).
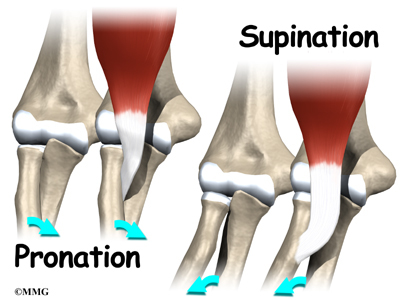
The elbow itself is essentially a hinge joint, meaning it bends and straightens like a hinge. But there is a second joint where the end of the radius (the radial head) meets the humerus. This joint is complicated because the radius has to rotate so that you can turn your hand palm up and palm down (pronation/supination). At the same time, it has to slide against the end of the humerus as the elbow bends and straightens.
The joint is even more complex because the radius has to slide against the ulna as it rotates the wrist as well. As a result, the end of the radius at the elbow is shaped like a smooth knob with a cup at the end to fit on the end of the humerus. The edges are also smooth where it glides against the ulna.
There are several important ligaments in the elbow. Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine together to form a joint capsule. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid called synovial fluid.
In the elbow, two of the most important ligaments are the ulnar collateral ligament (UCL) and the lateral collateral ligament. The UCL is also known as the medial collateral ligament. The ulnar collateral ligament is on the medial (the side of the elbow that’s next to the body) side of the elbow, and the lateral collateral is on the outside. The ulnar collateral ligament is a thick band of ligamentous tissue that forms a triangular shape along the medial elbow. It has an anterior bundle, posterior bundle, and a thinner, transverse ligament.
Together these two ligaments, the ulnar (or medial) collateral and the lateral collateral, connect the humerus to the ulna and keep it tightly in place as it slides through the groove at the end of the humerus. These ligaments are the main source of stability for the elbow. They can be torn when there is an injury or dislocation of the elbow. If they do not heal correctly the elbow can be too loose or unstable. The ulnar collateral ligament can also be damaged by overuse and repetitive stress, such as the throwing motion.
Causes
What causes ulnar collateral ligament (UCL) injuries?
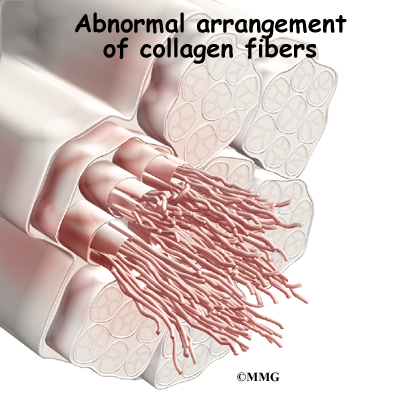
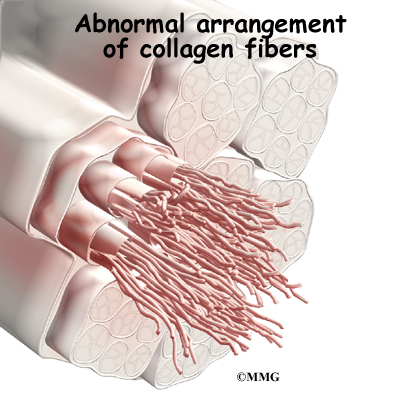
The ulnar collateral ligament can become stretched, frayed or torn through the stress of repetitive throwing motions. If the force on the soft tissues is greater than the tensile strength of the structure, then tiny tears of the ligament can develop. Months (and even years) of throwing hard cause a process of microtears, degeneration, and finally, rupture of the ligament. The dominant arm is affected most often. Eventually the weakened tendon my rupture completely causing a pop and immediate pain. The athlete may report the injury occurred during a single throw, but the reality is usually that the ligament simply finally became weakened to the point that it finally ruptured.
Professional pitchers have been the athletes treated most often for this problem. Javelin throwers and football, racquet sports, ice hockey, and water polo players have also been reported to injure the UCL. A fall on an outstretched arm can also lead to UCL rupture (often with elbow dislocation).
However, the general profile associated with this injury may be changing. Today, more and more children ages 10 to 18 are affected. Longer seasons with extended practice time and more tournaments increase the risk of UCL injury. Throwing volume, pitch type, and throwing mechanics can all contribute to the problem.
Children have their own unique risk factor in that they have an open growth plate in the elbow called the medial epicondylar physis. Force along the inside of the elbow during throwing is more likely to cause failure at the area of the growth plate than at the UCL. This injury is often termed Little League Elbow. Reconstruction of the UCL may not be needed in this age group unless the injury to the UCL occurs after the growth plate is closed. Sometimes the ligament avulses or pulls away, taking a piece of the growth plate with it. When the condition has been present for some time, the ligament is not all that may be damaged. The entire elbow joint is at risk due to the abnormal forces caused by the repetitive stress injury.
Related Document: A Patient’s Guide to Adolescent Osteochondritis Dissecans of the Elbow
Symptoms
What does the condition feel like?
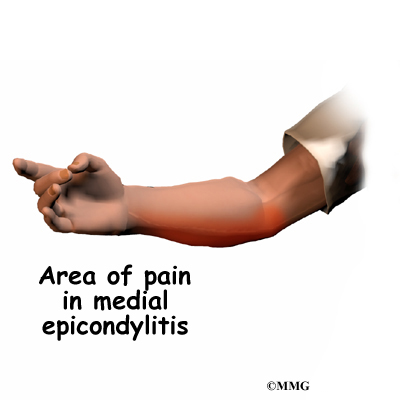
Pain along the inside of the elbow is the main symptom of this condition. Throwing athletes report it occurs most often during the acceleration phase of throwing. If there are loose fragments or uneven joint surfaces, you may also notice popping, catching, or grinding.
Sometimes swelling can be seen along the inside of the elbow. If the ligament was ruptured, there may be bruising in the same area. Some patients have a slight loss of elbow motion. Closing the hand and clenching the fist reproduces the painful symptoms.
Sometimes swelling can be seen along the inside of the elbow. If the ligament was ruptured, there may be bruising in the same area. Some patients have a slight loss of elbow motion. Closing the hand and clenching the fist reproduces the painful symptoms.
Diagnosis
How will my doctor diagnose this condition?
The diagnosis is based on your history and symptoms. Your physician will complete an examination of the shoulder and elbow, performing specific tests to look for areas of tightness or laxity (looseness). Most patients will report tenderness along the inside of the elbow to palpation of the UCL ligament.
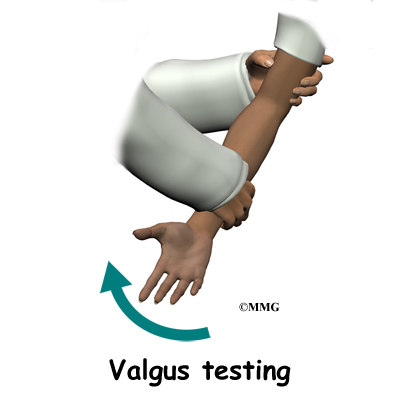
Valgus stress tests are done at the elbow to test for joint stability. The examiner places force toward the inside of the elbow as the joint is moved from a position of slight flexion into full extension. Too much motion or opening of the joint at the medial joint line called gapping may be observed or felt by palpation. The examiner may also feel the crepitation (popping, crunching) as the joint moves.
Standard X-rays are taken to look for bone spurs, loose fragments, or calcification in the ulnar collateral ligament. If the joint is gapping enough to sublux (partially dislocate), valgus stress radiographs may be taken.
Magnetic resonance imaging (MRI) with contrast dye is used to diagnose ligamentous rupture. The test doesn’t always show a problem when there is one. This is called a false-negative result. Ultrasound and CT scans may be helpful. Some surgeons prefer to use arthroscopy to make the final diagnosis. The presence and severity of valgus gapping can be confirmed. Studies using these more advanced test methods to diagnose UCL injuries are being done. More data is needed before they become routine in the diagnosis of UCL injuries.
Treatment
What treatment options are available?
Nonsurgical Treatment
Many athletes with elbow instability from UCL injury can be treated successfully with rehabilitation and without invasive procedures. At first, symptoms may be treated with rest and/or activity modification (fewer pitches per game, per practice, per day). The athlete’s posture, strength, and release of the ball must be analyzed and corrected. The use of curve balls should be avoided during the early phases of rehabilitation.
Antiinflammatory drugs and analgesics may be used to reduce pain and inflammation. Icing may help but must be used with caution. Too much cold can cause a worsening of the swelling as the body sends more blood to the area to warm things up. And cold can be an irritant to the already damaged (and irritated) nerve.
Many athletes are able to return to play without further treatment. If conservative (nonoperative) care does not change the picture, then surgery may be needed.
Surgery
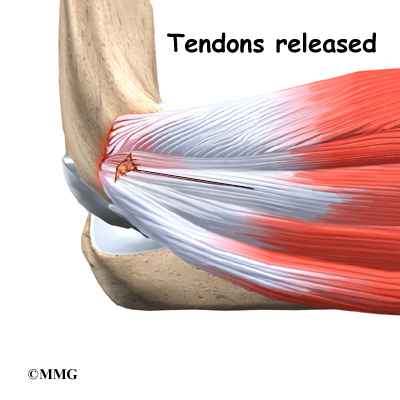
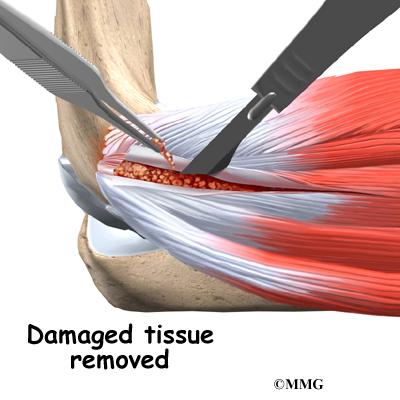
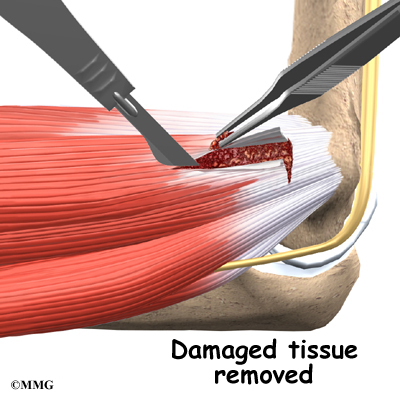
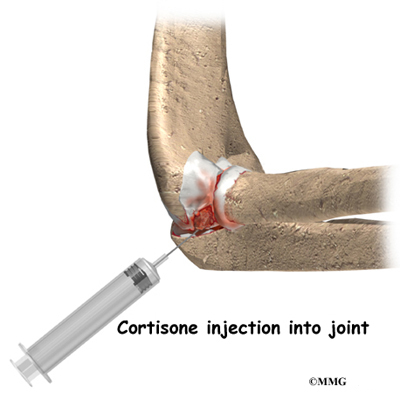
When the condition fails to respond to conservative care described above, surgery may be indicated. If pain is the primary symptom and there is no evidence that the elbow joint is grossly unstable, the surgeon may use an arthroscope (a tiny fiber-optic TV camera) to look inside the elbow and see the condition of the joint and the soft tissues. It may be possible to debride any tissue fragments or frayed edges. During debridement, the surgeon carefully cleans the area by removing any dead or damaged tissue. Any bone spurs or areas of calcium build-up are also removed.
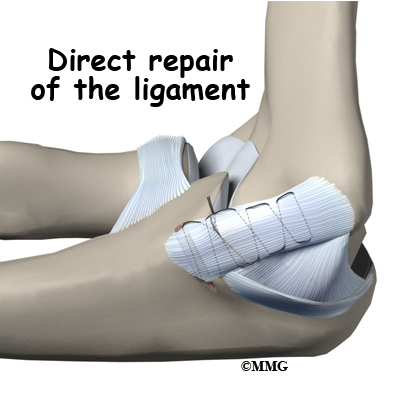
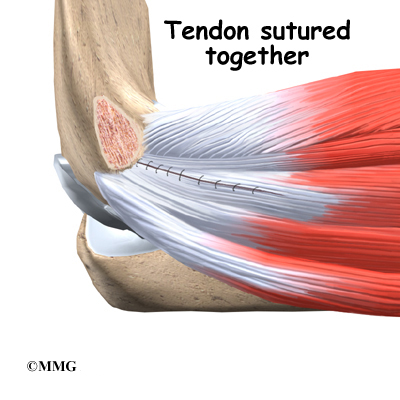
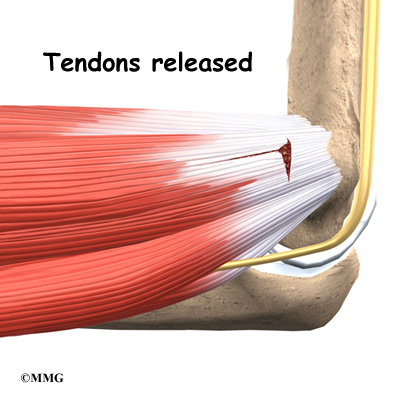
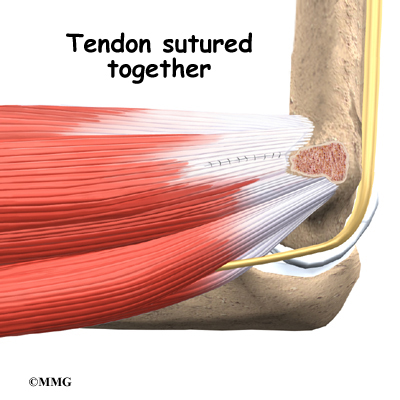
If the ulnar collateral ligament has been injured acutely due to a fall on the outstretched arm, a direct repair of the ligament may be possible. If the ligament has pulled off the bone, it may be reattached with sutures through holes drilled in the bone. If the ligament is damaged by constant overuse and is not strong enough to restore stability to the elbow joint if it is simply re-attached or repaired, then the ligament must be replaced with a new ligament. This is termed a ligament reconstruction. During a reconstruction, the ulnar collateral ligament along the medial (inside) of the elbow is replaced with a tendon graft harvested from somewhere else in the body (autograft). One common technique used to replace the damaged ulnar collateral ligament is called the docking technique.
Related Document: A Patient’s Guide to Ulnar Collateral Ligament Reconstruction
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Other modalities such as electrical stimulation and ultrasound with cortisone (called phonophoresis) may be used by a physical therapist when needed. Steroid injections are not usually recommended for this condition.
The athlete will work with the physical therapist to develop a daily program of stretching and strengthening. Stretching exercises for the muscles of the forearm are included. A strengthening program for the entire elbow/arm complex will be prescribed. High repetition, low weight exercise training is used to increase endurance without placing additional stress across the joint.
The therapist will also address any problems with flexibility, strength, and conditioning at the shoulder. Plyometric strengthening of the entire arm starts with the forearm muscles (flexors and pronators) and progresses to include the biceps, triceps, and rotator cuff of the upper arm. Plyometrics refers to training the nerves to fire quickly and the muscles to contract strong and fast. Plyometrics help develop explosive movements to improve muscular power and force. The goal is to increase the speed of the pitch (or throw for other throwing athletes).
After Surgery
Arthroscopic Debridement
Gentle range of motion exercises are started right away. Full motion is restored as the pain and swelling resolve. Elbow strengthening exercises are begun within the first few days to week after the procedure. A rehabilitation program is started and progressed, including a gradual throwing program. Full sports participation can be anticipated within one to three months.
Repair or Reconstruction
The postoperative program is the same for repairs or reconstruction. At first your arm will be immobilized in a bulky dressing.
You will be referred to a physical therapist to begin a rehabilitation program.
Gentle handgrip and shoulder and wrist mobilization exercises are allowed right away after surgery. Postoperative immobilization is discontinued in seven to 10 days at which time active range of motion for the elbow is started. Your surgeon may want you to wear a special hinged brace to protect the elbow.
Your therapist will instruct you in the active range of motion exercises to be done daily. Strengthening exercises for the entire upper quadrant (shoulder, arm, wrist, and hand) are included in the post-operative program. Specific strengthening exercises to help the athlete prepare for his or her particular sport begin around four months post-op. Up until this time, any stress to the medial elbow is avoided.
See also: Ulnar Collateral Ligament Reconstruction or Tommy John Surgery
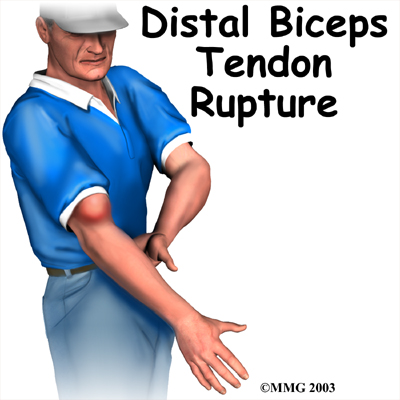
Distal Biceps Rupture
A Patient’s Guide to Distal Biceps Rupture
Introduction
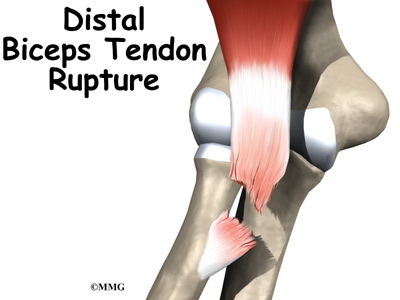
A distal biceps rupture occurs when the tendon attaching the biceps muscle to the elbow is torn from the bone. This injury occurs mainly in middle-aged men during heavy work or lifting. A distal biceps rupture is rare compared to ruptures where the top of the biceps connects at the shoulder. Distal biceps ruptures make up only three percent of all biceps tendon ruptures.
This guide will help you understand
- what parts of the elbow are affected
- the causes of distal biceps rupture
- ways to treat this problem
Anatomy
What parts of the elbow are affected?
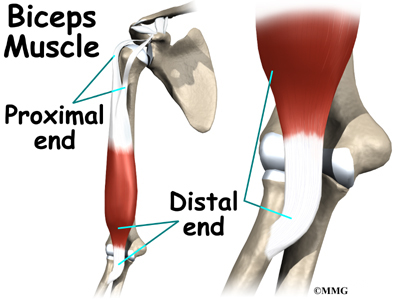
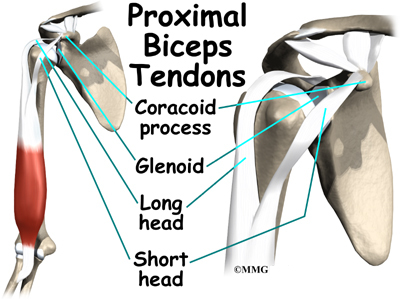
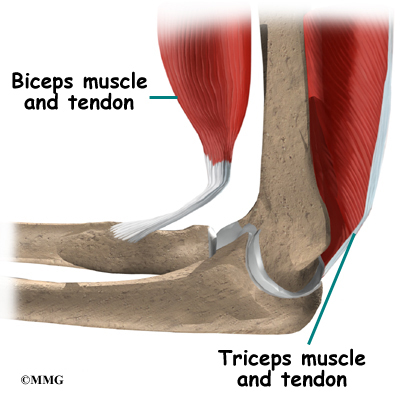
The biceps muscle goes from the shoulder to the elbow on the front of the upper arm. Tendons attach muscles to bone. Two separate tendons connect the upper part of the biceps muscle to the shoulder. One tendon connects the lower end of the biceps to the elbow.
The lower biceps tendon is called the distal biceps tendon. The word distal means that the tendon is further down the arm. The upper two tendons of the biceps are called the proximal biceps tendons, because they are closer to the top of the arm.
The distal biceps tendon attaches to a small bump on the radius bone of the forearm. This small bony bump is called the radial tuberosity. The radius is the smaller of the two bones between the elbow and the wrist that make up the forearm. The radius goes from the outside edge of the elbow to the thumb side of the wrist. It parallels the larger bone of the forearm, the ulna. The ulna goes from the inside edge of the elbow to the wrist.
The upper (proximal) end of the biceps has two attachments to the shoulder. The main attachment is the long head of the biceps. It connects the biceps muscle to the top of the shoulder socket, called the glenoid. The short head of the biceps angles up and in to its attachment on the corocoid process of the shoulder blade. The corocoid process is a small bony knob in the front of the shoulder.
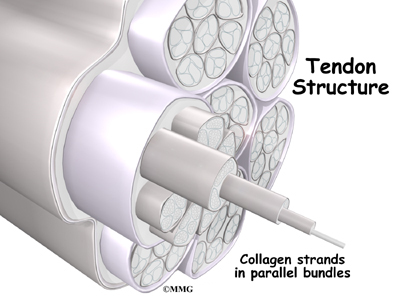
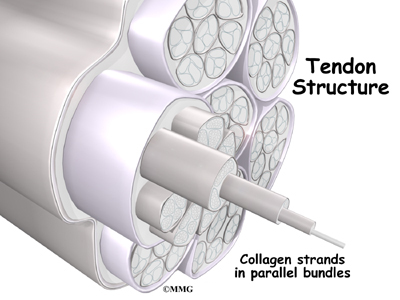
Tendons are made up of strands of a material called collagen. The collagen strands are lined up in bundles next to each other.
Because the collagen strands in tendons are lined up, tendons have high tensile strength. This means they can withstand high forces that pull on both ends of the tendon. When muscles contract, they pull on one end of the tendon. The other end of the tendon pulls on the bone, causing the bone to move.
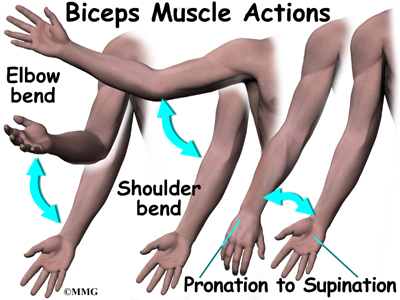
Contracting the biceps muscle can bend the elbow upward. The biceps can also help flex the shoulder, raising the arm up. And the biceps can rotate, or twist, the forearm in a way that points the palm of the hand up. This movement is called supination. Supination positions the hand as if you were carrying a tray.
Causes
Why did I develop a rupture of the distal biceps?
The most common cause of a distal biceps rupture happens when a middle-aged man lifts a box or other heavy item with his elbows bent. Often the load is heavier than expected, or the load may shift unexpectedly during the lift. This forces the elbow to straighten, even though the biceps muscle is working hard to keep the elbow bent. The biceps muscle contracts extra hard to help handle the load. As tension on the muscle and tendon increases, the distal biceps tendon snaps or tears where it connects to the radius.
Symptoms
What does a ruptured distal biceps feel like?
When the distal biceps tendon ruptures, it usually sounds and feels like a pop directly in front of the elbow. At first the pain is intense. The pain often subsides quickly after a complete rupture because tension is immediately taken off the pain sensors in the tendon. Swelling and bruising in front of the elbow usually develop shortly after the pop. The biceps may appear to have balled up near the elbow. The arm often feels weak with attempts to bend the elbow, lift the shoulder, or twist the forearm into supination (palm up).
The distal biceps tendon sometimes tears only part of the way. When this happens, a pop may not be felt or heard. Instead, the area in front of the elbow may simply be painful, and the arm may feel weak with the same arm movements that are affected in a complete rupture.
Diagnosis
How can my doctor be sure I have ruptured the distal biceps?
An early diagnosis is best. If surgery is needed, people who’ve ruptured their distal biceps tendon usually have better results when surgery is done soon after the injury.
Your doctor will first take a detailed medical history. You will need to answer questions about your pain, how your pain affects you, your regular activities, and past injuries to your elbow.
The physical exam is often most helpful in diagnosing a rupture of the distal biceps tendon. Your doctor may position your elbow and forearm to see which movements are painful and weak. By feeling the muscle and tendon, your doctor can often tell if the tendon has ruptured off the bone.
X-rays may be ordered. X-rays are mainly used to find out if there are other injuries in the elbow. Plain X-rays do not show soft tissues like tendons. They will not show a distal biceps rupture unless a small piece of bone got pulled off the radius as the tendon ruptured. This type of injury is called an avulsion fracture.
Your doctor may also order a magnetic resonance imaging (MRI) scan to see if the biceps tendon is only partially torn or if the tendon fully ruptured. An MRI is a special imaging test that uses magnetic waves to create pictures of the elbow in slices. The MRI can also show if there are other problems in the elbow.
Treatment
What can I do to treat this problem?
Nonsurgical Treatment
Many doctors prefer to treat distal biceps tendon ruptures with surgery. Nonsurgical treatments are usually only used for people who do minimal activities and require minimal arm strength. Nonsurgical treatments are only used if arm weakness, fatigue, and mild deformity aren’t an issue. If you are an older individual who can tolerate loss of strength, or if the injury occurs in your nondominanat arm, you and your doctor may decide that surgery is not necessary.
Not having surgery often results in significant loss of strength. Flexion of the elbow is somewhat affected, but supination (which is the motion of twisting the forearm, such as when you use a screwdriver) can be very affected. A distal biceps rupture that is not repaired reduces supination strength by about 50 percent.
Nonsurgical measures may include a sling to rest the elbow. Patients may be given anti-inflammatory medicine to help ease pain and swelling and get them back to activities sooner. These medications include common over-the-counter drugs such as ibuprofen.
Your doctor may have you work with a physical or occupational therapist. At first, your therapist will give you tips how to rest your elbow and how to do your activities without putting extra strain on the joint. Your therapist may apply ice and electrical stimulation to ease pain. Exercises are used to gradually strengthen other muscles that can help do the work of a normal biceps muscle.
Surgery
People who need normal arm strength get best results with surgery to reconnect the tendon right away. Surgery is needed to avoid tendon retraction. When the tendon has been completely ruptured, contraction of the biceps muscle pulls the tendon further up the arm. When the tendon recoils from its original attachment and remains there for a very long time, the surgery becomes harder, and the results of surgery are not as good.
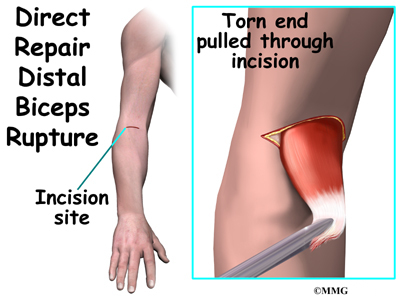
Direct Repair
Direct repair surgery is commonly done soon after the rupture. Doing a direct repair soon after the injury lessens the risk of tendon retraction.
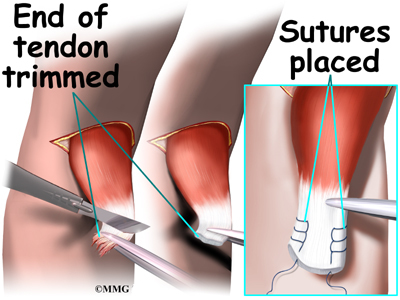
In a direct repair, the surgeon begins by making a small incision across the arm, just above the elbow. Forceps are inserted up into this incision to grasp the free end of the ruptured biceps tendon. The surgeon pulls on the forceps to slide the tendon through the incision. Attention is given to the free end of the tendon. A scalpel is used to slice off the damaged and degenerated end. Sutures are then crisscrossed through the bottom inch of the distal biceps tendon.
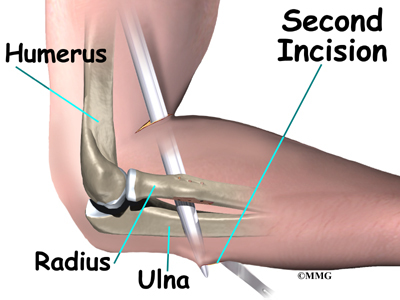
A curved instrument is passed through the incision and directly between the radius and ulna bones. The surgeon pushes the instrument through this space, puncturing the muscles and soft tissues. The surgeon feels the back side of the forearm for the spot where the instrument is protruding. A second incision is made at this spot.
The original attachment on the radius, the radial tuberosity, is prepared. An instrument called a burr shaves off the surface of the tuberosity. The burr is then used to create a small cavity in the bone for the tendon to fit inside. Three small holes are drilled into the top of the rim of bone to secure the sutures.
The tendon is passed between the radius and ulna, exiting through the second incision that was made on the back of the forearm. The sutures are threaded into the three holes that were drilled into the rim of the radial tuberosity. The surgeon ties the sutures, securing the newly reattached biceps tendon. When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed either in a cast or a range-of-motion brace.
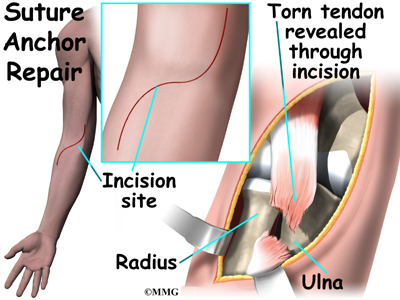
Suture Anchor Method
A new method of anchoring the torn tendon to the radius is gaining popularity. This method uses special anchors, called suture anchors, to fix the tendon in place. The procedure requires only one incision and appears to lessen the risk of myositis ossificans. Myositis ossificans is an abnormal healing response that causes bone to form in the muscles and soft tissues.
The surgeon begins by making a single incision across the arm, just above the elbow. Along the outside edge of the arm, the incision curves and goes upward for a short distance. The skin and underlying tissues are pulled back using retractors. This reveals the front of the lower biceps muscle and allows the surgeon to avoid injuring nearby nerves and arteries. The fascia (connective covering over the muscle) is cut away so the surgeon can see the radial tuberosity.
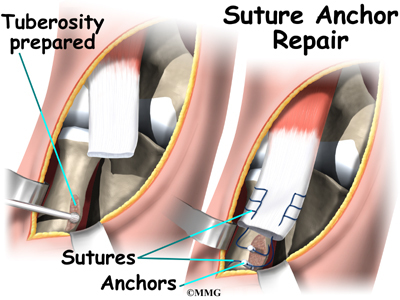
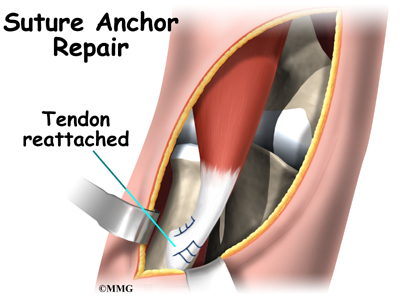
The original attachment on the radius, the radial tuberosity, is prepared by shaving off the surface with a burr. The burr is then used to create a small cavity in the bone for the tendon to fit inside. Two small suture anchors are embedded into the cavity in the radial tuberosity. These anchors can either be screwed into the bone or implanted like a staple. Each anchor has a long thread (suture) connected to it. The suture is woven into the lower end of the tendon and crisscrossed upward. The surgeon slides the sutures back and forth, which coaxes the end of the tendon into the cavity. When the end of the tendon is positioned in the cavity, the surgeon tightens the sutures, fixing the tendon in place.
When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed either in a cast or a range-of-motion brace.
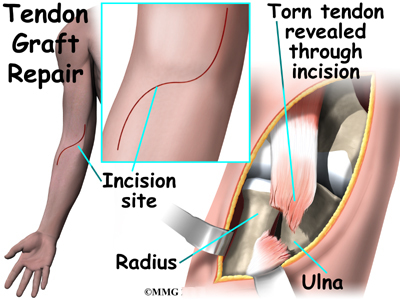
Graft Repair
If more than three or four weeks have passed since the rupture, the surgeon will usually need to make a larger incision in the front of the elbow. Also, because the tendon will have retracted further up the arm, graft tissue will be needed in order to reconnect the biceps to its original point of attachment on the radial tuberosity.
The surgeon begins by making a curved incision across the arm, just above the elbow joint. The incision curves along the front surface of the upper arm to expose the lower part of the biceps muscle. The surface of the radial tuberosity is removed. A burr is used to create a small cavity within the tuberosity. Several suture holes are drilled around the rim of the tuberosity.
A curved instrument is passed through the incision and directly between the radius and ulna bones. The surgeon pushes the instrument through this space, puncturing the muscles and soft tissues. The surgeon feels the back of the forearm to find the point where the instrument is protruding. A second incision is made at this spot.
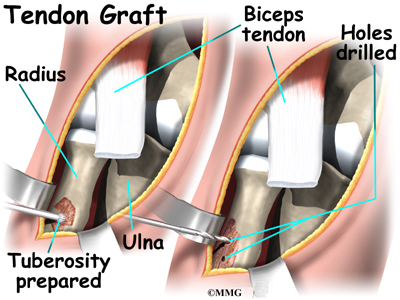
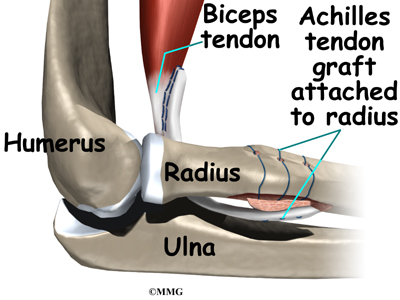
The surgeon then prepares a graft of tissue to lengthen the retracted biceps tendon. Some surgeons use a piece of hamstring tendon for the graft. Others use a section of the Achilles tendon where it attaches to the heel. This type of graft is usually an allograft, meaning that the tissue is taken from a cadaver (human tissue preserved for medical purposes).
When the Achilles tendon allograft is used, the surgeon leaves a small piece of the heel bone attached to the piece of tendon. Small holes are drilled into the piece of bone. Sutures are woven through these holes and will later be used to secure the end of the graft to the radial tuberosity. In this way, the graft will have a bone-to-bone connection that heals together. The healed bone solidly fixes the the graft to the radial tuberosity. After the graft is in place, its top end is then stitched over the front of the biceps muscle.
Next, the lower end of the graft is passed between the radius and ulna, exiting through the second incision that was made on the back of the forearm. The sutures from the bony end of the graft are threaded into holes that were drilled into the rim of the radial tuberosity earlier. The surgeon ties the sutures, securing the graft to the radius.
When the surgeon is satisfied with the repair, the skin incisions are closed, and the elbow is placed in a protective brace.
Rehabilitation
How soon can I use my elbow again?
Nonsurgical Rehabilitation
When a ruptured biceps tendon is treated nonsurgically, you may need to avoid heavy arm activity for three to four weeks. As the pain and swelling resolve, it will become safe to begin doing more normal activities.
If the tendon is only partially torn, recovery takes longer. Patients usually need to rest the elbow using a protective splint or sling. As symptoms ease, you will usually begin a carefully progressed rehabilitation program under the supervision of a physical or occupational therapist. The program often involves one to two months of therapy.
After Surgery
Rehabilitation takes even longer after surgery. Immediately after surgery, your surgeon may cast your elbow for up to six weeks. Some surgeons prefer to use a special range-of-motion brace with careful elbow motion starting within one to two weeks. When you start therapy, your first few sessions may involve ice and electrical stimulation treatments to help control pain and swelling from the surgery. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
You will gradually start exercises to improvement movement in the forearm, elbow, and shoulder. You need to be careful to avoid doing too much, too quickly.
Exercises for the biceps muscle are avoided until at least four to six weeks after surgery. Your therapist may begin with light isometric strengthening exercises. These exercises work the biceps muscle without straining the healing tendon.
At about six weeks, you start doing more active strengthening. As you progress, your therapist will teach you exercises to strengthen and stabilize the muscles and joints of the wrist and hand, elbow, and shoulder. Other exercises will work your elbow in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow.
You may require therapy for two to three months. It generally takes four to six months to safely begin doing forceful biceps activity. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Elbow Anatomy
A Patient’s Guide to Elbow Anatomy
Introduction
At first, the elbow seems like a simple hinge. But when the complexity of the interaction of the elbow with the forearm and wrist is understood, it is easy to see why the elbow can cause problems when it does not function correctly. Part of what makes us human is the way we are able to use our hands. Effective use of our hands requires stable, painless elbow joints.
In addition to reading this article, be sure to watch our Elbow Anatomy Animated Tutorial Video.
This guide will help you understand
- what parts make up the elbow
- how those parts work together
Important Structures
The important structures of the elbow can be divided into several categories. These include
- bones and joints
- ligaments and tendons
- muscles
- nerves
- blood vessels
Bones and Joints
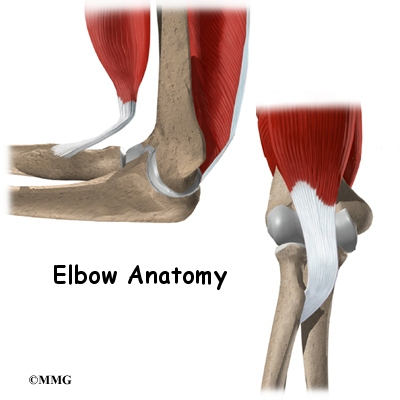
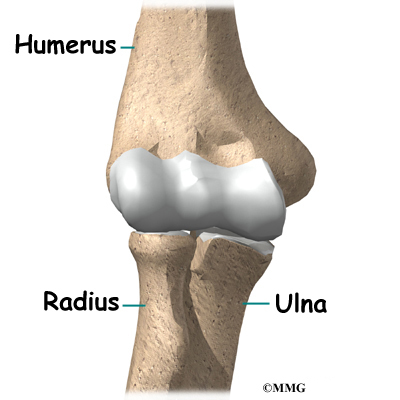
The bones of the elbow are the humerus (the upper arm bone), the ulna (the larger bone of the forearm, on the opposite side of the thumb), and the radius (the smaller bone of the forearm on the same side as the thumb). The elbow itself is essentially a hinge joint, meaning it bends and straightens like a hinge. But there is a second joint where the end of the radius (the radial head) meets the humerus. This joint is complicated because the radius has to rotate so that you can turn your hand palm up and palm down. At the same time, it has to slide against the end of the humerus as the elbow bends and straightens. The joint is even more complex because the radius has to slide against the ulna as it rotates the wrist as well. As a result, the end of the radius at the elbow is shaped like a smooth knob with a cup at the end to fit on the end of the humerus. The edges are also smooth where it glides against the ulna.
Articular cartilage is the material that covers the ends of the bones of any joint. Articular cartilage can be up to one-quarter of an inch thick in the large, weight-bearing joints. It is a bit thinner in joints such as the elbow, which don’t support weight. Articular cartilage is white, shiny, and has a rubbery consistency. It is slippery, which allows the joint surfaces to slide against one another without causing any damage.
The function of articular cartilage is to absorb shock and provide an extremely smooth surface to make motion easier. We have articular cartilage essentially everywhere that two bony surfaces move against one another, or articulate. In the elbow, articular cartilage covers the end of the humerus, the end of the radius, and the end of the ulna.
Ligaments and Tendons
There are several important ligaments in the elbow. Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine together to form a joint capsule. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid called synovial fluid.
In the elbow, two of the most important ligaments are the medial collateral ligament and the lateral collateral ligament. The medial collateral is on the inside edge of the elbow, and the lateral collateral is on the outside edge. Together these two ligaments connect the humerus to the ulna and keep it tightly in place as it slides through the groove at the end of the humerus. These ligaments are the main source of stability for the elbow. They can be torn when there is an injury or dislocation to the elbow. If they do not heal correctly the elbow can be too loose, or unstable.
There is also an important ligament called the annular ligament that wraps around the radial head and holds it tight against the ulna. The word annular means ring shaped, and the annular ligament forms a ring around the radial head as it holds it in place. This ligament can be torn when the entire elbow or just the radial head is dislocated.
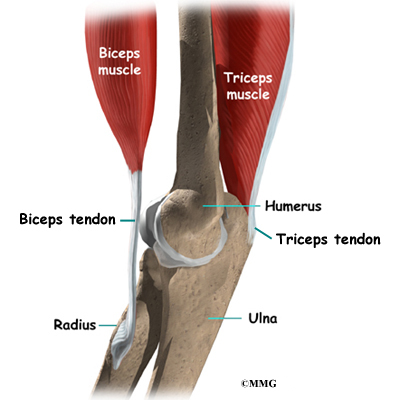
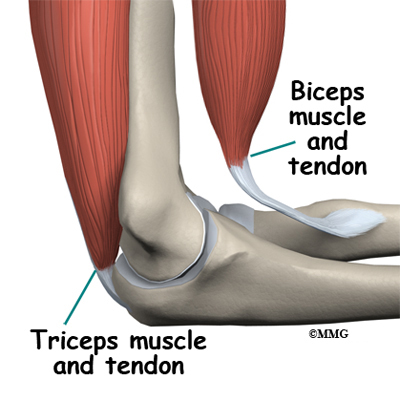
There are several important tendons around the elbow. The biceps tendon attaches the large biceps muscle on the front of the arm to the radius. It allows the elbow to bend with force. You can feel this tendon crossing the front crease of the elbow when you tighten the biceps muscle. The triceps tendon connects the large triceps muscle on the back of the arm with the ulna. It allows the elbow to straighten with force, such as when you perform a push-up.
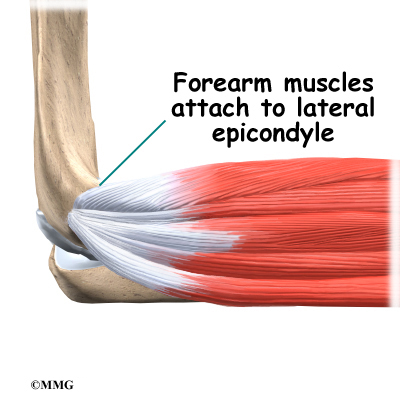
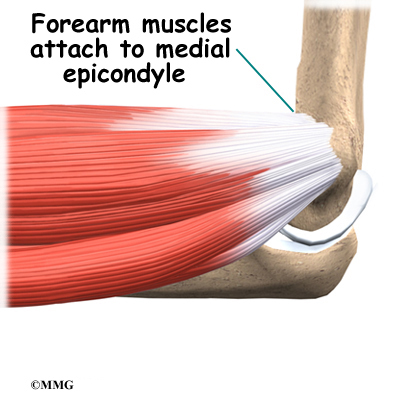
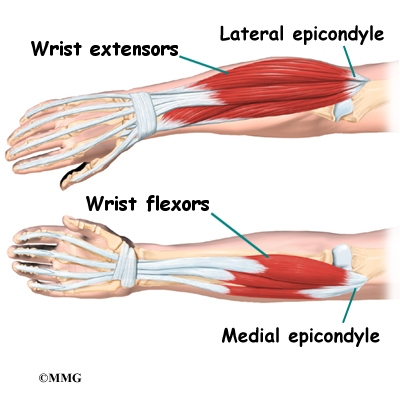
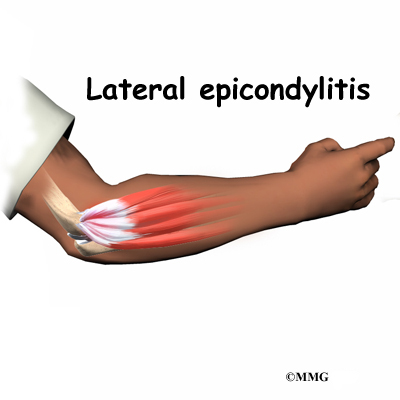
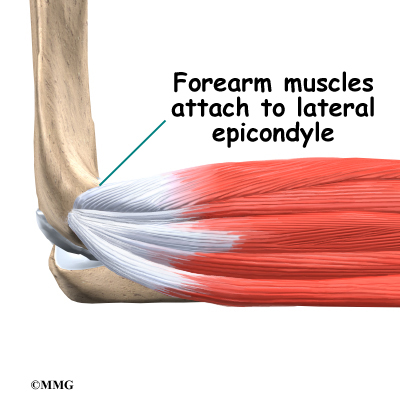
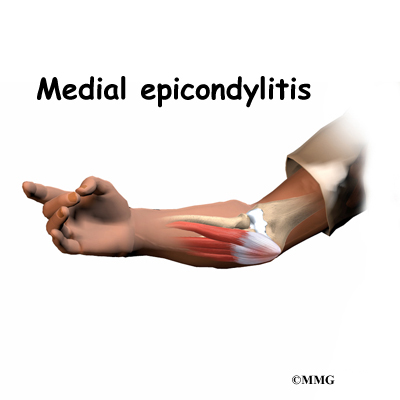
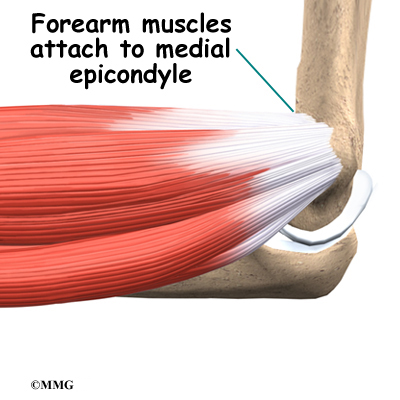
The muscles of the forearm cross the elbow and attach to the humerus. The outside, or lateral, bump just above the elbow is called the lateral epicondyle. Most of the muscles that straighten the fingers and wrist all come together in one tendon to attach in this area. The inside, or medial, bump just above the elbow is called the medial epicondyle. Most of the muscles that bend the fingers and wrist all come together in one tendon to attach in this area. These two tendons are important to understand because they are a common location of tendonitis.
Muscles
The main muscles that are important at the elbow have been mentioned above in the discussion about tendons. They are the biceps, the triceps, the wrist extensors (attaching to the lateral epicondyle) and the wrist flexors (attaching to the medial epicondyle).
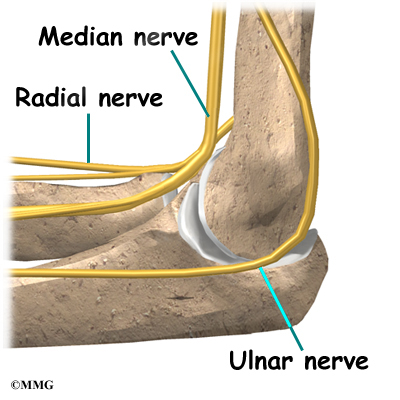
Nerves
All of the nerves that travel down the arm pass across the elbow. Three main nerves begin together at the shoulder: the radial nerve, the ulnar nerve, and the median nerve. These nerves carry signals from the brain to the muscles that move the arm. The nerves also carry signals back to the brain about sensations such as touch, pain, and temperature.
Some of the more common problems around the elbow are problems of the nerves. Each nerve travels through its own tunnel as it crosses the elbow. Because the elbow must bend a great deal, the nerves must bend as well. Constant bending and straightening can lead to irritation or pressure on the nerves within their tunnels and cause problems such as pain, numbness, and weakness in the arm and hand.
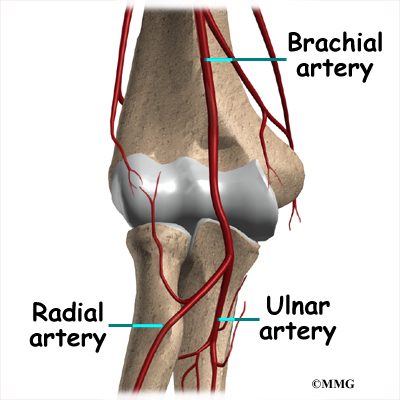
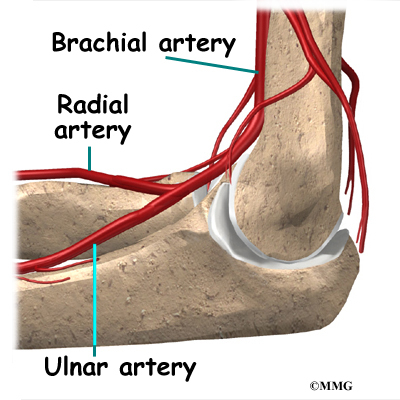
Blood Vessels
Traveling along with the nerves are the large vessels that supply the arm with blood. The largest artery is the brachial artery that travels across the front crease of the elbow. If you place your hand in the bend of your elbow, you may be able to feel the pulsing of this large artery. The brachial artery splits into two branches just below the elbow: the ulnar artery and the radial artery that continue into the hand. Damage to the brachial artery can be very serious because it is the only blood supply to the hand.
Summary
As you can see, the elbow is more than a simple hinge. It is designed to provide maximum stability as we position our forearm to use our hand. When you realize all the different ways we use our hands every day and all the different positions we put our hands in, it is easy to understand how hard daily life can be when the elbow doesn’t work well.
Elbow Replacement
A Patient’s Guide to Artificial Joint Replacement of the Elbow
Introduction
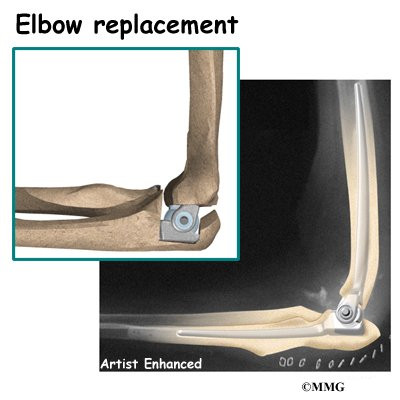
Elbow joint replacement (also called elbow arthroplasty) can effectively treat the problems caused by arthritis of the elbow. The procedure is also becoming more widely used in aging adults to replace joints damaged by fractures. The artificial elbow is considered successful by more than 90 percent of patients who have elbow joint replacement.
This guide will help you understand
- how the elbow joint works
- what happens during surgery to replace the elbow joint
- what you can expect after elbow joint replacement
Anatomy
How does the elbow joint work?
The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm.
The ulna and the humerus meet at the elbow and form a hinge. This hinge allows the arm to straighten and bend. The large triceps muscle in the back of the arm attaches to the point of the ulna (the olecranon). When this muscle contracts, it straightens out the elbow. The biceps muscles in the front of the arm contracts to bend the elbow.
Inside the elbow joint, the bones are covered with articular cartilage. Articular cartilage is a slick, smooth material. It protects the bone ends from friction when they rub together as the elbow moves. Articular cartilage is soft enough to act as a shock absorber. It is also tough enough to last a lifetime, if it is not injured.
The connection of the radius to the humerus allows rotation of the forearm. The upper end of the radius is round. This round end turns against the ulna and the humerus as the forearm and hand turn from palm down (pronation) to palm up supination).
Rationale
What makes elbow joint replacement surgery necessary?
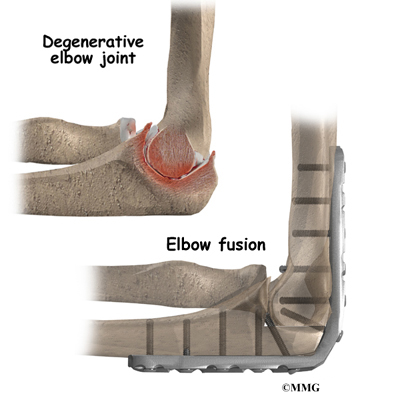
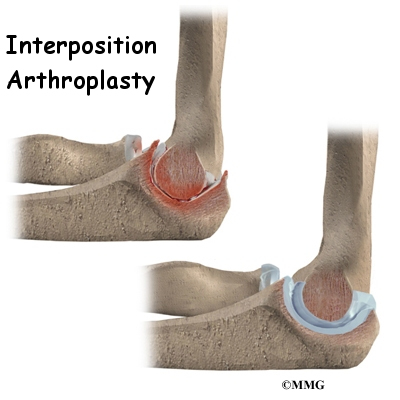
A joint replacement surgery is usually considered a last resort for a badly damaged and painful elbow joint. The artificial joint replaces the damaged surfaces with metal and plastic that are designed to fit together and rub smoothly against each other. This takes away the pain of bone rubbing against bone.
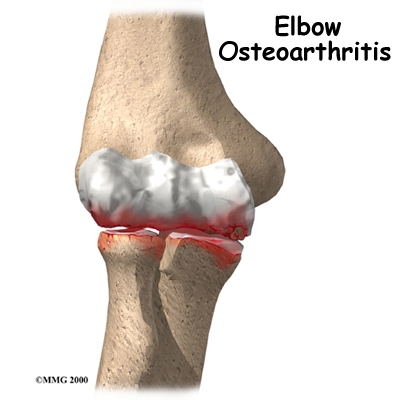
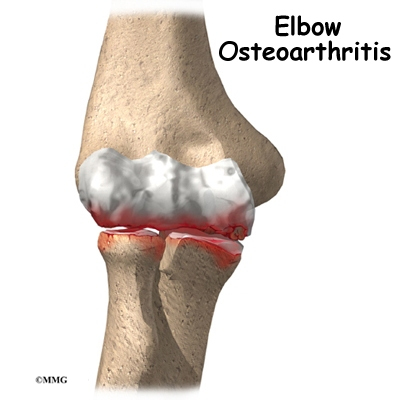
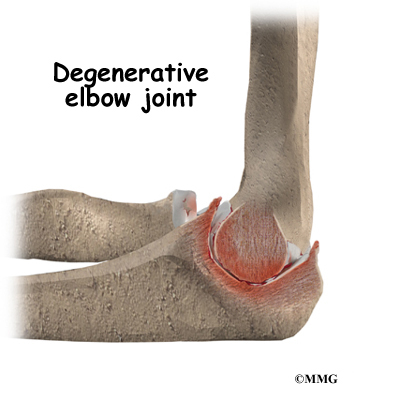
The most common reason for an artificial elbow replacement is arthritis. There are two main types of arthritis, degenerative and systemic. Degenerative arthritis is also called wear-and-tear arthritis, or osteoarthritis. Any injury to the elbow can damage the joint and lead to degenerative arthritis. Arthritis may not show up for many years after the injury.
There are many types of systemic arthritis. The most common form is rheumatoid arthritis. All types of systemic arthritis are diseases that affect many, or even all, of the joints in the body. Systemic arthritis causes destruction of the joints’ articular cartilage lining.
An elbow joint replacement may also be used immediately following certain types of elbow fractures, usually in aging adults. Elbow fractures are difficult to repair surgically in the best of circumstances. In many aging adults, the bone is also weak from osteoporosis. (People with osteoporosis have bones that are less dense than they should be.) The weakened bone makes it much harder for the surgeon to use metal plates and screws to hold the fractured pieces of bone in place long enough for them to heal together. In cases like this, it is sometimes better to remove the fractured pieces and replace the elbow with an artificial joint.
Preparation
What do I need to know before surgery?
You and your surgeon should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical or occupational therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this pre-operative visit is to record a baseline of information. Your therapist will check your current pain levels, ability to do your activities, and the movement and strength of each elbow.
A second purpose of the pre-operative therapy visit is to prepare you for surgery. You’ll begin learning some of the exercises you’ll use during your recovery. And your therapist can help you anticipate any special needs or problems you might have at home, once you’re released from the hospital.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. Come prepared to stay in the hospital for at least one night.
Surgical Procedure
What happens during an elbow replacement surgery?
Replacement surgery is usually not considered until it has become impossible to control your symptoms without surgery. If replacement becomes necessary, it can be a very effective way to take away the pain of arthritis and to regain use of your elbow.
Before we describe the procedure, let’s look first at the artificial elbow itself.
The Artificial Elbow
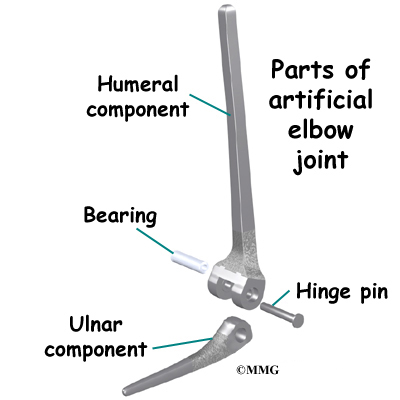
There is more than one kind of artificial elbow joint (also called a prosthesis). The most common types are like a hinge.
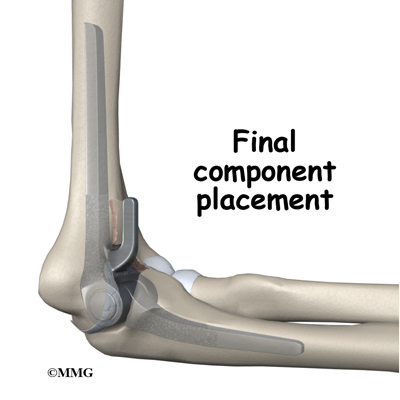
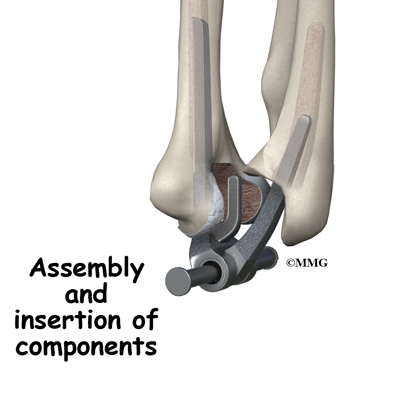
Each prosthesis has two parts. The humeral component replaces the lower end of the humerus in the upper arm. The humeral component has a long stem that anchors it into the hollow center of the humerus. The ulnar component replaces the upper end of the ulna in the lower arm. The ulnar component has a shorter metal stem that anchors it into the hollow center of the ulna.
The hinge between the two components is made of metal and plastic. The plastic part of the hinge is tough and slick. It allows the two pieces of the new joint to glide easily against each other as you move your elbow. The hinge allows the elbow to bend and straighten smoothly.
There are two different ways to hold the artificial elbow in place:
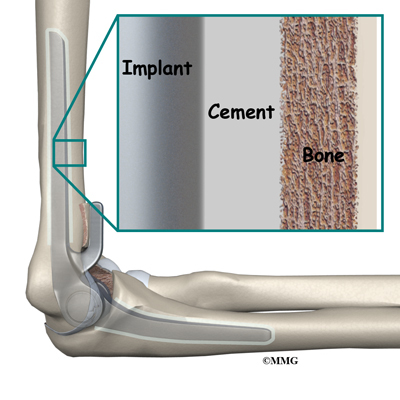
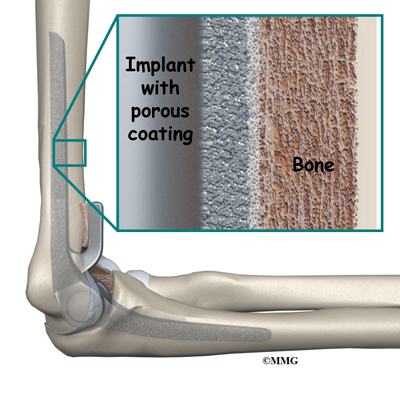
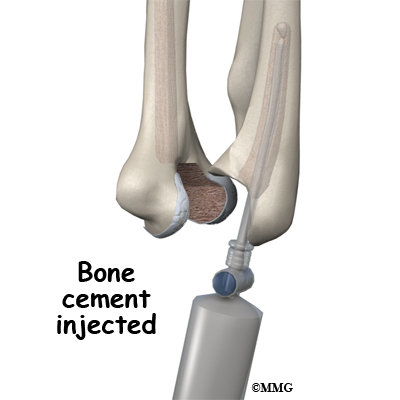
A cemented prosthesis uses a special type of epoxy cement to glue it to the bone.
An uncemented prosthesis has a fine mesh of holes on the surface. Over time, the bone grows into the mesh, anchoring the prosthesis to the bone.
The Operation
Most elbow replacement surgeries are done under general anesthesia. General anesthesia puts you to sleep. In some cases surgery is done with regional anesthesia, which deadens only the nerves of the arm. If you use regional anesthesia, you may also get medications to help you drift off to sleep, so you are not aware of the surgery.
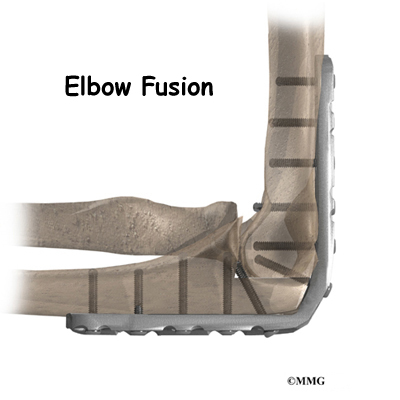
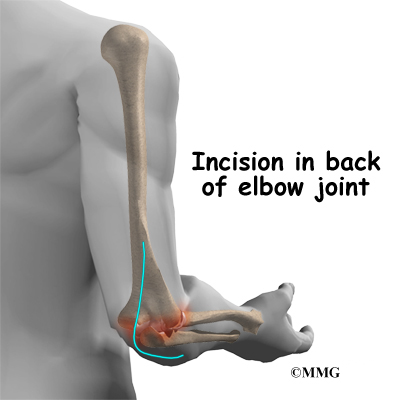
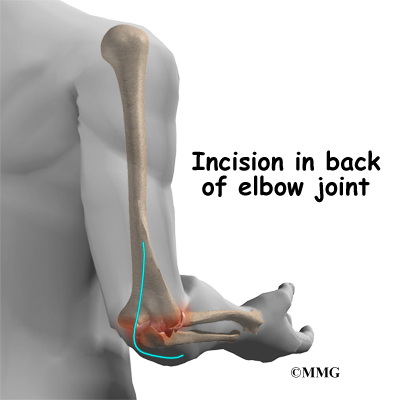
After the anesthesia, the surgeon makes an incision in the back of the elbow joint. The incision is made on the back side because most of the blood vessels and nerves are on the inside of the elbow. Entering from the back side helps prevent damage to them. The tendons and ligaments are then moved out of the way. Care must be taken to move the ulnar nerve, which runs along the elbow to the hand.
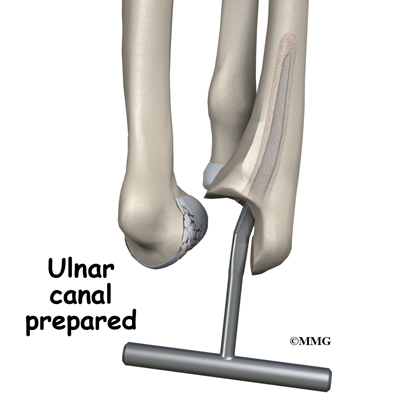
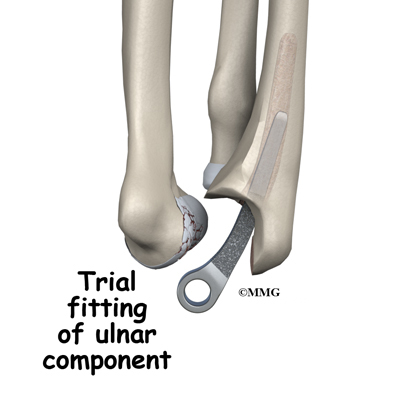
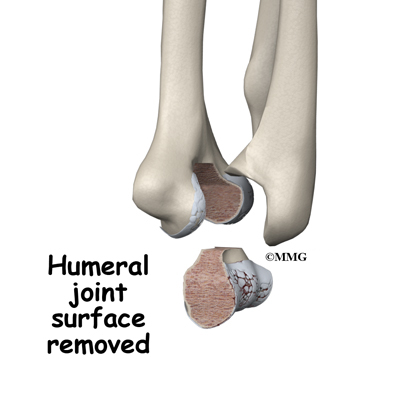
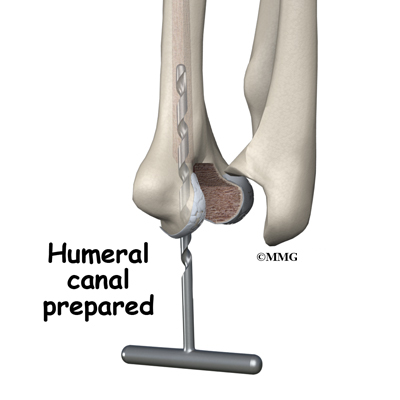
Once the joint is exposed, the first step is to remove the joint surfaces of the ulna and the radius. This is usually done with a surgical saw. The surgeon then uses a special rasp to hollow out the marrow space within the ulna to hold the metal stem of the ulnar component. The ulnar component is then to test the fit. If necessary, the surgeon will use the rasp to reshape the hole in the ulna.
When the ulnar component has been fitted correctly, the surgeon repeats the procedure on the humerus.
After the humeral component has been fitted, the surgeon puts together the pieces of the implant and checks to see if the hinge is working correctly. The implant is then removed, and the bone is prepared to cement it in place. The pieces are cemented in place and put together. After another check for proper fit and motion, the surgeon sews up the incision.
Your elbow will probably be placed in a bulky dressing and splint. You will then be awakened and taken to the recovery room.
Complications
Does elbow replacement surgery cause any problems?
As with all major surgical procedures, complications can occur. This is not intended to be a complete list of complications. Some of the most common complications following elbow replacement are
- anesthesia
- infection
- loosening
- nerve or blood vessel injury
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Infection following joint replacement surgery can be very serious. The chances of developing an infection after most artificial joint replacements are low, about one or two percent. Elbow replacement has a somewhat higher chance of infection, for many reasons. The skin is thin around the elbow, and no muscles cover the joint. This makes wound complications more common. Elbow replacements are also done more often in people who have rheumatoid arthritis. This disease and the drugs used to treat it affect the body’s immune system, making it harder to fight off infections.
Sometimes infections show up very early, before you leave the hospital. Other times infections may not show up for months, or even years, after the operation. Infection can also spread into the artificial joint from other infected areas. Once an infection lodges in your joint, it is almost impossible for your immune system to clear it. You may need to take antibiotics when you have dental work or surgical procedures on your bladder and colon. The antibiotics reduce the risk of spreading germs to the artificial joint.
Loosening
The major reason that artificial joints eventually fail is that they loosen where the metal or cement meets the bone. A loose joint implant can cause pain. If the pain becomes unbearable, another operation will probably be needed to fix the artificial joint.
There have been great advances in extending the life of artificial joints. However, most implants will eventually loosen and require another surgery. Younger, more active patients have a higher risk of loosening. In the case of an artificial knee joint, you could expect about 12 to 15 years, but artificial elbow joints tend to loosen sooner.
Nerve or Blood Vessel Injury
All of the large nerves and blood vessels to the forearm and hand travel across the elbow joint. Because surgery takes place so close to these nerves and vessels, it is possible to injure them during surgery. The result may be temporary if the nerves have been stretched by retractors holding them out of the way during the procedure. It is very uncommon to have permanent injury to either the nerves or the blood vessels, but it is possible.
After Surgery
What can I expect right after surgery?
After surgery, your elbow will probably be covered by a bulky bandage and a splint. Depending on the type of implant used, your elbow will either be positioned straight or slightly bent. You may also have a small plastic tube that drains blood from the joint. Draining prevents excessive swelling from the blood. (This swelling is sometimes called a hematoma.) The draining tube will probably be removed within the first day. Assisted elbow movements are started by an occupational or physical therapist the day after surgery.
Your surgeon will want to check your elbow within five to seven days. Stitches will be removed after 10 to 14 days, though most of your stitches will be absorbed into your body. You may have some discomfort after surgery. You will be given pain medicine to control the discomfort you have.
You should keep your elbow elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting.
Rehabilitation
How soon will I be able to use my elbow again?
A physical or occupational therapist will direct your rehabilitation program. Recovery takes up to three months after elbow replacement surgery. The first few therapy treatments will focus on controlling the pain and swelling from surgery. Heat treatments may be used. Your therapist may also use gentle massage and other types of hands-on treatments to ease muscle spasm and pain.
Then you’ll begin gentle range-of-motion exercises. Strengthening exercises are used to give added stability around the elbow joint. You’ll learn ways to lift and carry items in order to do your tasks safely and with the least amount of stress on your elbow joint. As with any surgery, you need to avoid doing too much, too quickly.
Some of the exercises you’ll do are designed get your elbow working in ways that are similar to your work tasks and daily activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your new elbow joint. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Your therapist’s goal is to help you keep your pain under control, improve your strength and range of motion, and maximize the use of your elbow. When you are well under way, regular visits to the therapist’s office will end. Your therapist will continue to be a resource for you, but you will be in charge of doing exercises as part of an ongoing home program.
Cubital Tunnel Syndrome
A Patient’s Guide to Cubital Tunnel Syndrome
Introduction
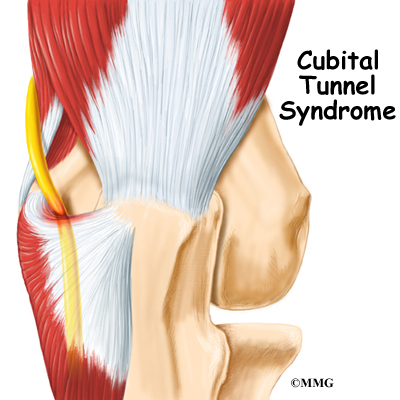
Cubital tunnel syndrome is a condition that affects the ulnar nerve where it crosses the inside edge of the elbow. The symptoms are very similar to the pain that comes from hitting your funny bone. When you hit your funny bone, you are actually hitting the ulnar nerve on the inside of the elbow. There, the nerve runs through a passage called the cubital tunnel. When this area becomes irritated from injury or pressure, it can lead to cubital tunnel syndrome.
This guide will help you understand
- what causes this condition
- ways to make the pain go away
- what you can do to prevent future problems
Anatomy
What is the cubital tunnel?
The ulnar nerve actually starts at the side of the neck, where the individual nerve roots leave the spine. The nerve roots exit through small openings between the vertebrae. These openings are called neural foramina.
The nerve roots join together to form three main nerves that travel down the arm to the hand. One of these nerves is the ulnar nerve.
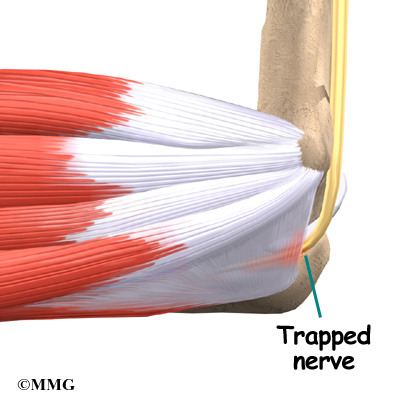
The ulnar nerve passes through the cubital tunnel just behind the inside edge of the elbow. The tunnel is formed by muscle, ligament, and bone. You may be able to feel it if you straighten your arm out and rub the groove on the inside edge of your elbow.
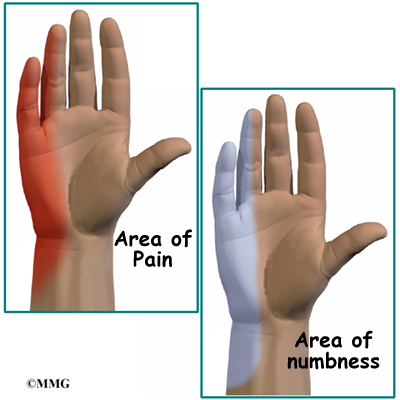
The ulnar nerve passes through the cubital tunnel and winds its way down the forearm and into the hand. It supplies feeling to the little finger and half the ring finger. It works the muscle that pulls the thumb into the palm of the hand, and it controls the small muscles (intrinsics) of the hand.
Causes
What causes cubital tunnel syndrome?
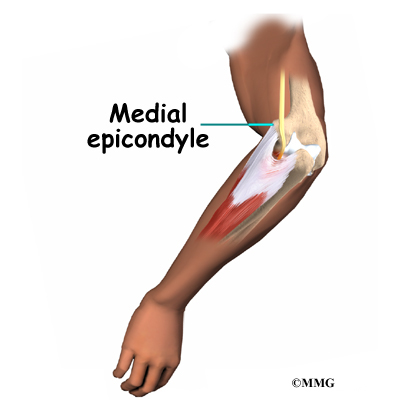
Cubital tunnel syndrome has several possible causes. Part of the problem may lie in the way the elbow works. The ulnar nerve actually stretches several millimeters when the elbow is bent. Sometimes the nerve will shift or even snap over the bony medial epicondyle. (The medial epicondyle is the bony point on the inside edge of the elbow.) Over time, this can cause irritation.
One common cause of problems is frequent bending of the elbow, such as pulling levers, reaching, or lifting. Constant direct pressure on the elbow over time may also lead to cubital tunnel syndrome. The nerve can be irritated from leaning on the elbow while you sit at a desk or from using the elbow rest during a long drive or while running machinery. The ulnar nerve can also be damaged from a blow to the cubital tunnel.
Symptoms
What does cubital tunnel syndrome feel like?
Numbness on the inside of the hand and in the ring and little fingers is an early sign of cubital tunnel syndrome. The numbness may develop into pain. The numbness is often felt when the elbows are bent for long periods, such as when talking on the phone or while sleeping. The hand and thumb may also become clumsy as the muscles become affected.
Tapping or bumping the nerve in the cubital tunnel will cause an electric shock sensation down to the little finger. This is called Tinel’s sign.
Related Document: A Patient’s Guide to Medial Epicondylitis
Diagnosis
How will my doctor know I have cubital tunnel syndrome?
Your doctor will take a detailed medical history. You will be asked questions about which fingers are affected and whether or not your hand is weak. You will also be asked about your work and home activities and any past injuries to your elbow.
Your doctor will then do a physical exam. The cubital tunnel is only one of several spots where the ulnar nerve can get pinched. Your doctor will try to find the exact spot that is causing your symptoms. The prodding may hurt, but it is very important to pinpoint the area causing you trouble.
You may need to do special tests to get more information about the nerve. One common test is the nerve conduction velocity (NCV) test. The NCV test measures the speed of the impulses traveling along the nerve. Impulses are slowed when the nerve is compressed or constricted.
The NCV test is sometimes combined with an electromyogram (EMG). The EMG tests the muscles of the forearm that are controlled by the ulnar nerve to see whether the muscles are working properly. If they aren’t, it may be because the nerve is not working well.
Treatment
How can I make my pain go away?
Nonsurgical Treatment
The early symptoms of cubital tunnel syndrome usually lessen if you just stop whatever is causing the symptoms. Anti-inflammatory medications may help control the symptoms. However, it is much more important to stop doing whatever is causing the pain in the first place. Limit the amount of time you do tasks that require a lot of bending in the elbow. Take frequent breaks. If necessary, work with your supervisor to modify your job activities.
If your symptoms are worse at night, a lightweight plastic arm splint or athletic elbow pad may be worn while you sleep to limit movement and ease irritation. Wear it with the pad in the bend of the elbow to keep the elbow straight while you sleep. You can also wear the elbow pad during the day to protect the nerve from the direct pressure of leaning.
Doctors commonly have their patients with cubital tunnel syndrome work with a physical or occupational therapist. At first, your therapist will give you tips how to rest your elbow and how to do your activities without putting extra strain on your elbow. Your therapist may apply heat or other treatments to ease pain. Exercises are used to gradually stretch and strengthen the forearm muscles.
Surgery
Your symptoms may not go away, even with changes in your activities and nonsurgical treatments. In that case, your doctor may recommend surgery to stop damage to the ulnar nerve.
The goal of surgery is to release the pressure on the ulnar nerve where it passes through the cubital tunnel. There are two different kinds of surgery for cubital tunnel syndrome. It is not clear whether one operation is better than the other.
Ulnar Nerve Transposition
One method is called ulnar nerve transposition. In this procedure, the surgeon forms a completely new tunnel from the flexor muscles of the forearm. The ulnar nerve is then moved (transposed) out of the cubital tunnel and placed in the new tunnel. The following images show each step
Medial Epicondylectomy
The other method simply removes the medial epicondyle on the inside edge of the elbow, a procedure called medial epicondylectomy. By getting the medial epicondyle out of the way, the ulnar nerve can then slide through the cubital tunnel without pressure from the bony bump. The following images show each step:
Cubital tunnel surgery is often done as an outpatient procedure. This means you won’t have to stay in the hospital overnight. Surgery can be done using a general anesthetic, which puts you to sleep, or a regional anesthetic. A regional anesthetic blocks the nerves in only one part of your body. In this case, you would have an axillary block, which would affect only the nerves of the arm.
Rehabilitation
What can I expect after treatment?
Nonsurgical Rehabilitation
If nonsurgical treatments are successful, you may see improvement in four to six weeks. Your physical or occupational therapist works with you to ease symptoms and improve elbow function. Special exercises may be used to help the ulnar nerve glide within the cubital tunnel. Treatment progresses to include strengthening exercises that mimic daily and work activities.
You may need to continue wearing your elbow pad or splint at night to control symptoms. Try to do your activities using healthy body and wrist alignment. Limit repeated motions of the arm and hand, and avoid positions and activities where the elbow is held in a bent position.
After Surgery
Recovery after elbow surgery depends on the procedure used by your surgeon. If you only had the medial epicondyle removed, you’ll have a soft bandage wrapped over your elbow after surgery. Therapy can progress quickly after this type of surgery. Treatments start out with range-of-motion exercises and gradually work into active stretching and strengthening. You just need to be careful to avoid doing too much, too quickly.
Therapy goes slower after ulnar nerve transposition surgery. You could require therapy for three months. This is because the flexor muscles had to be sewn together to form the new tunnel. Your elbow will be placed in a splint and wrapped in bulky dressing, and your elbow will be immobilized for three weeks.
When the splint is removed, therapy will begin with passive movements. In passive exercises, your elbow is moved, but your muscles stay relaxed. Your therapist gently moves your arm and gradually stretches your wrist and elbow. You may be taught how to do passive exercises at home.
Active therapy starts six weeks after surgery. You begin to use your own muscle power in active range-of-motion exercises. Light isometric strengthening exercises are started. You may begin careful strengthening of your hand and forearm by squeezing and stretching special putty. These exercises work the muscles without straining the healing tissues.
At about eight weeks, you’ll start doing more active strengthening. Your therapist will give you exercises to help strengthen and stabilize the muscles and joints in the wrist, elbow, and shoulder. Other exercises are used to improve fine motor control and dexterity of the hand.
Some of the exercises you’ll do are designed get your elbow working in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Elbow Fusion
A Patient’s Guide to Elbow Fusion
Introduction
Arthritis of the elbow has many causes, and there are many ways of treating the pain. These treatments can be very successful, at least for a while. But eventually the elbow can become so painful that nonsurgical treatments don’t work anymore. At this point, your doctor may recommend surgery to fuse the elbow. Elbow fusion may also be necessary after severe trauma to the elbow. Fusion surgery is sometimes called arthrodesis.
This guide will help you understand
- how an elbow fusion eases the pain of arthritis
- how the operation is done
- what the recovery process is like
Anatomy
How does the elbow work?
The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm. The ulna and the humerus bones meet at the elbow to form a hinge. This hinge allows the arm to bend and straighten.
View animation of hinge movement
The connection of the radius to the humerus allows rotation of the forearm. The upper end of the radius is round. It turns against the ulna and the humerus as the forearm and hand turn from palm down (pronation) to palm up (supination).
View animation of elbow pronation/supination
Articular cartilage is the smooth, rubbery material that covers the bone surfaces in most joints. It protects the bone ends from friction when they rub together as the joint moves. Articular cartilage also acts sort of like a shock absorber. Damage to the articular cartilage eventually leads to degenerative arthritis.
When the articular cartilage is worn away over time, the bones begin to rub against each other. This causes the pain of degenerative arthritis. Degenerative arthritis is also called osteoarthritis.
Related Document: A Patient’s Guide to Osteoarthritis of the Elbow
Rationale
Why do I need elbow fusion surgery?
A fusion of any joint eliminates pain by making the bones of the joint grow together, or fuse, into one solid bone. Fusions are used in many joints. They were very common before the invention of artificial joints. Fusions are still performed fairly often to treat arthritis pain. An elbow fusion helps get rid of pain because the bones of the joint no longer rub together.
Advanced arthritis can change the alignment of the elbow, leading to deformity. Likewise, elbow injuries can alter normal alignment and eventually produce arthritis. Fusing the bones together improves the alignment and prevents further deformation.
You will not be able to bend your elbow after fusion surgery. An elbow fusion is a tradeoff. You will lose the hinge motion in your elbow, but you will regain a strong, pain-free elbow joint. Regaining strength is especially important to laborers who work with their arms and hands. Some patients may need range of motion more than strength. In these cases, doctors usually recommend surgeries such as interposition arthroplasty or elbow joint replacement.
Related Document: A Patient’s Guide to Interposition Arthroplasty
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Elbow
The radius bone of the forearm is usually not part of the elbow fusion. The end of the radius forms a joint with the ulna. This joint allows you to pronate and supinate (rotate) your forearm and hand. When this joint is a source of pain, the surgeon may remove the round end of the radius near the elbow. This still allows the forearm to rotate.
Preparation
What do I need to do before surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. The amount of time patients spend in the hospital varies.
Surgical Procedure
What happens during elbow fusion surgery?
There are many different types of operations to fuse the elbow. Most of the procedures are designed to remove the articular cartilage from the joint surfaces of the hinge joint and then bind the two surfaces together until they heal. When two raw bone surfaces are held together like this, your body treats them like a broken bone. New bone forms to heal the two pieces together. When the fusion is healed, a strong, solid connection between the humerus and ulna will have replaced the painful arthritic joint.
The first step in an elbow fusion is an incision down the back of the elbow. The incision is made on the back side because most of the blood vessels and nerves are on the inside of the elbow. Entering through the back of the elbow makes them less likely to be damaged.
The surgeon then moves the tendons and ligaments to the side to expose the joint surfaces. Care must be taken to protect the nerves that run beside the elbow joint on their way to the hand. The surgeon then removes the articular cartilage surface of each side of the joint.
The surgeon must then fix the humerus and ulna in place until they can heal together. The elbow is bent to 90 degrees and the bones are carefully aligned. The bones must be properly aligned and immobilized for fusion to occur.
Plate Fixation
There are different ways of holding the bones together. Many surgeons place a metal plate with screw holes onto the back of the elbow, from the humerus to the ulna. The metal plate is attached to the bone with metal screws. The metal plate stays in the arm permanently. It is only removed if it causes problems.
External Fixation
Another way to hold the bones together is to use an external fixator. Surgeons sometimes choose an external fixator if there have been problems with an infection in the elbow joint.
An external fixator involves placing metal pins through the bones above and below the elbow joint. Your surgeon may also place a metal screw inside the ulna and humerus to pull the bones together. The external fixator device is then placed on the elbow outside the skin, after the incision is sewn up. The external fixator attaches to the metal pins, which come through the skin, with metal rods and bolts.
At the end of the fusion operation, the incisions are sutured together. As long as you don’t have an external fixator, the arm is placed in a large splint or cast. It usually takes about 12 weeks for the fusion to become solid. At this point the metal pins and rods of the external fixator are removed.
Complications
Does elbow fusion surgery cause any problems?
As with all major surgical procedures, complications can occur. This is not intended to be a complete list of complications. Some of the most common complications following elbow fusion surgery are
- anesthesia
- infection
- nerve or blood vessel injury
- nonunion
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any surgery carries the risk of infection. You will probably be given antibiotics before the procedure to reduce the risk. If you get an infection, you will need more antibiotics. If the area around the bone graft or metal plate becomes infected, you may need surgery to drain the infection.
Nerve or Blood Vessel Injury
All of the nerves and blood vessels that go to the forearm and hand travel across the elbow joint. Because the operation is performed so close to these nerves and vessels, it is possible to injure them during surgery. When the damage is caused by retractors used during surgery to stretch them out of the way, the nerve symptoms are usually temporary. Permanent injury to the nerves or blood vessels rarely happens, but it is possible.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) If joint motion from a nonunion continues to cause pain, you may need a second operation. In the second procedure, the surgeon usually adds more bone graft and checks that the plates and screws are holding the bones solidly in place. The bones need to be completely immobilized for fusion to occur.
After Surgery
What can I expect after surgery?
After surgery, you will either wear an external fixator for up to 12 weeks or a long-arm cast for about six weeks. Both devices hold the elbow still while the ends of the bones fuse together. Your surgeon will want to check your elbow within five to seven days. Stitches will be removed after 10 to 14 days, although most of them will have been absorbed by your body. You may have some discomfort after surgery. Your surgeon can give you pain medicine to control the discomfort.
You should keep your arm elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting.
Rehabilitation
What will my recovery be like?
Patients who have an external fixator should expect to wear it for up to 12 weeks. When a cast is used, some doctors will replace it with a removable splint after six to eight weeks. If you wear a cast, the joints in your wrist and fingers may feel stiff or sore.
Your surgeon will X-ray your elbow several times after surgery to make sure that the bones are healing properly. Once your surgeon is sure that fusion has occurred, you can safely begin a strengthening program. It will take some time to regain the strength in your arm. As with any surgery, you need to avoid doing too much, too quickly.
If you keep having pain or find that you have stiffness in the shoulder, wrist, or finger joints, you may need a physical or occupational therapist to direct your recovery program. The first few therapy treatments will focus on controlling the pain and swelling. Your therapist may use gentle massage and other types of hands-on treatments to ease muscle spasm and pain. Then you’ll begin gentle range-of-motion exercises for the arm.
Strengthening exercises give you added stability around the elbow joint. Some of the exercises you’ll do are designed to get your arm working in ways that are similar to your work tasks and daily activities. Your therapist will teach you ways to use your arm so that you can do your tasks safely and with the least amount of stress on your elbow. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Your therapist’s goal is to help you keep your pain under control, improve your strength, and learn how to adjust your activities to avoid putting too much strain on your arm and elbow. When you are well under way, your regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you’ll be in charge of doing your exercises as part of an ongoing home program.
Interposition Elbow Arthroplasty
A Patient’s Guide to Interposition Arthroplasty of the Elbow
Introduction
Elbow arthritis may be surgically treated with a procedure called interposition arthroplasty. The term interposition means that new tissue is placed between the damaged surfaces of the elbow joint. In this surgery, tissue is taken from another source to fill in the space in the elbow joint. The soft tissue forms a false joint. This surgery has best results in younger people with healthy tissue around the elbow joint.
This guide will help you understand
- which parts of the elbow are involved
- why this type of surgery is used
- what happens during the procedure
- what to expect before and after surgery
Anatomy
Which parts of the elbow joint are involved?
The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm.
The ulna and the humerus meet at the elbow and form a hinge. This hinge allows the arm to straighten and bend. The large triceps muscle in the back of the arm attaches to the point of the ulna (the olecranon). When this muscle contracts, it straightens out the elbow. The biceps muscle in the front of the arm contracts to bend the elbow.
View animation of hinge movement
View animation of the biceps muscle moving the elbow
Inside the elbow joint, the bones are covered with articular cartilage. Articular cartilage is a slick, smooth material. It protects the bone ends from friction when they rub together as the elbow moves. Articular cartilage is soft enough to act as a shock absorber. It is tough enough to last a lifetime, if it is not injured.
The connection of the radius to the humerus allows rotation of the forearm. The upper end of the radius is round. It turns against the ulna and the humerus as the forearm and hand turn from palm down (pronation) to palm up (supination).
View animation of elbow pronation/supination
Rationale
What does my surgeon hope to achieve?
The main goal of interposition surgery is to ease the pain of osteoarthritis where the surfaces of the elbow joint are rubbing together. A piece of tendon or other soft tissue forms a spacer that separates the surfaces of the joint. Interposition arthroplasty is different than a fusion surgery. Fusion simply binds the joint together, and the elbow loses much movement. Interposition arthroplasty can help take away pain while allowing the elbow joint to retain some movement.
Related Document: A Patient’s Guide to Elbow Fusion
Preparation
What should I do to prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during surgery?
Surgery can last up to 90 minutes. Surgery may be done using general anesthesia, which puts you completely to sleep, or local anesthesia, which numbs only the arm. With a local anesthetic you may be awake during the surgery, but your surgeon will make sure that you won’t be able to see the surgery.
Once you have gotten anesthesia, your surgeon will make sure that the skin of your elbow is free of infection by cleaning it with a germ-killing solution. The surgeon will make an incision along the back of your elbow. The incision is made on the back side because most of the blood vessels and nerves are on the inside of the elbow. Entering from the back side helps prevent damage to them.
The tendons and ligaments are then moved out of the way. Special care is taken to move the ulnar nerve, which runs along the elbow to the hand. Once the ends of the joint are exposed, scar tissue and bone spurs (small points of bone) are removed.
Then the surgeon shapes the ends of the elbow joint. This is done to make space for new tissue between the joint surfaces.
The surgeon then removes a rectangular-shaped piece of fascia tissue from the side of your thigh. (Fascia is a flat connective tissue that wraps around your muscles and organs.) This sheet of tissue is folded three times and sewn onto the end of the humerus bone. The new tissue forms a pad to separate the joint surfaces of the elbow.
Once the new piece of tissue is in place, the soft tissues over the joint are sewn back together.
Metal pins are then placed through the humerus and ulna bones. The pins stick out through the skin. A hinged elbow brace is attached to the pins to hold the surfaces of the elbow joint slightly apart. This device is worn for four to six weeks after surgery.
Complications
What might go wrong?
As with all surgical procedures, complications can occur. This is not intended to be a complete list of complications. Some of the most common complications are
- anesthesia
- infection
- nerve or blood vessel damage
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. Interposition arthroplasty of the elbow is no different. You will probably be given antibiotics before the operation to reduce the risk of infection. If an infection occurs, you will most likely need more antibiotics to cure it. You may need additional operations to drain the infection if it involves the area around the arthroplasty.
Nerve or Blood Vessel Damage
All of the nerves and blood vessels that go to the elbow travel across or near the elbow joint. Because the operation is performed so close to the nerves and vessels, it is possible to injure them during surgery. If the injury was caused by retractors stretching the nerves out of the way, the symptoms are usually temporary. Permanent injury to the nerves or blood vessels is rare, but it can happen.
After Surgery
What do I need to know after surgery?
After surgery, your elbow will be bandaged and supported by a movable splint. The splint holds the surfaces of the joint apart slightly as they heal. Your surgeon will want to check your elbow within five to seven days. Stitches will be removed after 10 to 14 days, though most of them will have been absorbed into your body. You may have some discomfort after surgery. Your surgeon can give you pain medicine to control the discomfort.
You should keep your elbow elevated above the level of your heart for several days to avoid swelling and throbbing. Keep your elbow propped up on a stack of pillows when sleeping or sitting.
Rehabilitation
What should I expect during my recovery period?
After surgery, you’ll wear the elbow brace for up to six weeks to give your elbow time to heal. Then you will probably see a physical or occupational therapist to direct your recovery program. You will need to attend therapy sessions for one to two months, and you should expect full recovery to take up to four months.
The first few therapy treatments will focus on controlling the pain and swelling from surgery. Heat treatments may be used. Your therapist may also use gentle massage and other hands-on treatments to ease muscle spasm and pain.
Then you’ll begin gentle range-of-motion exercises, which may include active elbow movements and passive stretching.
Strengthening exercises are used to give extra stability to the elbow joint. As with any surgery, you need to avoid doing too much, too quickly.
Some of the exercises you’ll do are designed to get your arm working in ways that are similar to your work tasks and daily activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow joint. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Your therapist’s goal is to help you keep control your pain, improve your strength, and maximize your range of motion. When you are well under way, regular visits to your therapist’s office will end. Your therapist will continue to be a resource for you. But you will be in charge of your own exercises as part of an ongoing home program.
Tennis Elbow
A Patient’s Guide to Lateral Epicondylitis (Tennis Elbow)
Introduction
Lateral epicondylitis, commonly known as tennis elbow, is not limited to tennis players. The backhand swing in tennis can strain the muscles and tendons of the elbow in a way that leads to tennis elbow. But many other types of repetitive activities can also lead to tennis elbow: painting with a brush or roller, running a chain saw, and using many types of hand tools. Any activities that repeatedly stress the same forearm muscles can cause symptoms of tennis elbow.
This guide will help you understand
- what parts of the elbow are affected
- the causes of tennis elbow
- ways to make the pain go away
Anatomy
What parts of the elbow are affected?
Tennis elbow causes pain that starts on the outside bump of the elbow, the lateral epicondyle. The forearm muscles that bend the wrist back (the extensors) attach on the lateral epicondyle and are connected by a single tendon. Tendons connect muscles to bone.
Tendons are made up of strands of a material called collagen. The collagen strands are lined up in bundles next to each other.
Because the collagen strands in tendons are lined up, tendons have high tensile strength. This means they can withstand high forces that pull on both ends of the tendon. When muscles work, they pull on one end of the tendon. The other end of the tendon pulls on the bone, causing the bone to move.
When you bend your wrist back or grip with your hand, the wrist extensor muscles contract. The contracting muscles pull on the extensor tendon. The forces that pull on these tendons can build when you grip things, hit a tennis ball in a backhand swing in tennis, or do other similar actions.
Causes
Why did I develop tennis elbow?
Overuse of the muscles and tendons of the forearm and elbow are the most common reason people develop tennis elbow. Repeating some types of activities over and over again can put too much strain on the elbow tendons. These activities are not necessarily high-level sports competition. Hammering nails, picking up heavy buckets, or pruning shrubs can all cause the pain of tennis elbow.
In an acute injury, the body undergoes an inflammatory response. Special inflammatory cells make their way to the injured tissues to help them heal. Conditions that involve inflammation are indicated by -itis on the end of the word. For example, inflammation in a tendon is called tendonitis. Inflammation around the lateral epicondyle is called lateral epicondylitis.
However, tennis elbow often does not involve inflammation. Rather, the problem is within the cells of the tendon. Doctors call this condition tendonosis. In tendonosis, wear and tear is thought to lead to tissue degeneration. A degenerated tendon usually has an abnormal arrangement of collagen fibers.
Instead of inflammatory cells, the body produces a type of cells called fibroblasts. When this happens, the collagen loses its strength. It becomes fragile and can break or be easily injured. Each time the collagen breaks down, the body responds by forming scar tissue in the tendon. Eventually, the tendon becomes thickened from extra scar tissue.
No one really knows exactly what causes tendonosis. Some doctors think that the forearm tendon develops small tears with too much activity. The tears try to heal, but constant strain and overuse keep re-injuring the tendon. After a while, the tendons stop trying to heal. The scar tissue never has a chance to fully heal, leaving the injured areas weakened and painful.
Symptoms
What does tennis elbow feel like?
The main symptom of tennis elbow is tenderness and pain that starts at the lateral epicondyle of the elbow. The pain may spread down the forearm. It may go as far as the back of the middle and ring fingers. The forearm muscles may also feel tight and sore.
The pain usually gets worse when you bend your wrist backward, turn your palm upward, or hold something with a stiff wrist or straightened elbow. Grasping items also makes the pain worse. Just reaching into the refrigerator to get a carton of milk can cause pain. Sometimes the elbow feels stiff and won’t straighten out completely.
Diagnosis
How can my doctor be sure I have tennis elbow?
Your doctor will first take a detailed medical history. You will need to answer questions about your pain, how your pain affects you, your regular activities, and past injuries to your elbow.
The physical exam is often most helpful in diagnosing tennis elbow. Your doctor may position your wrist and arm so you feel a stretch on the forearm muscles and tendons. This is usually painful with tennis elbow. There are also other tests for wrist and forearm strength that can be used to detect tennis elbow.
You may need to get X-rays of your elbow. The X-rays mostly help your doctor rule out other problems with the elbow joint. The X-ray may show if there are calcium deposits on the lateral epicondyle at the connection of the extensor tendon.
Tennis elbow symptoms are very similar to a condition called radial tunnel syndrome. This condition is caused by pressure on the radial nerve as it crosses the elbow. If your pain does not respond to treatments for tennis elbow, your doctor may suggest tests to rule out problems with the radial nerve.
Related Document: A Patient’s Guide to Radial Tunnel Syndrome
When the diagnosis is not clear, your doctor may order other special tests. A magnetic resonance imaging (MRI) scan is a special imaging test that uses magnetic waves to create pictures of the elbow in slices. The MRI scan shows tendons as well as bones.
Ultrasound tests use high-frequency sound waves to generate an image of the tissues below the skin. As the small ultrasound device is rubbed over the sore area, an image appears on a screen. This type of test can sometimes show problems with collagen degeneration.
Treatment
What can I do to make my pain go away?
Nonsurgical Treatment
The key to nonsurgical treatment is to keep the collagen from breaking down further. The goal is to help the tendon heal.
If the problem is caused by acute inflammation, anti-inflammatory medications such as ibuprofen may give you some relief. If inflammation doesn’t go away, your doctor may inject the elbow with cortisone. Cortisone is a powerful anti-inflammatory medication. Its benefits are temporary, but they can last for a period of weeks to several months.
Your doctor may suggest using ultrasound to guide a needle into the sore area. The ultrasound gives a clear picture of areas in the tendon that contain scar tissue. Poking holes in the tendon breaks up scar tissue and gets the tendon to bleed. Bleeding in the tendon helps stimulate the healing response.
Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for tennis elbow, but recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Doctors commonly have patients with tennis elbow work with a physical or occupational therapist. At first, your therapist will give you tips on how to rest your elbow and how to do your activities without putting extra strain on your elbow. Your therapist may apply tape to take some of the load off the elbow muscles and tendons. You may need to wear an elbow strap that wraps around the upper forearm in a way that relieves the pressure on the tendon attachment.
Your therapist may apply ice and electrical stimulation to ease pain and improve healing of the tendon. Therapy sessions may also include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine to the sore area. This treatment is especially helpful for patients who can’t tolerate injections. Exercises are used to gradually stretch and strengthen the forearm muscles.
Because tendonosis is often linked to overuse, your therapist will work with you to reduce repeated strains on your elbow. When symptoms come from a particular sport or work activity, your therapist will observe your style and motion with the activity. You may be given tips about how to perform the movement so the elbow is protected. Your therapist can check your sports equipment and work tools and suggest how to alter them to keep your elbow safe.
Surgery
Sometimes nonsurgical treatment fails to stop the pain or help patients regain use of the elbow. In these cases, surgery may be necessary.
Tendon Debridement
When problems are caused by tendonosis, surgeons may choose to take out (debride) only the affected tissues within the tendon. In these cases, the surgeon cleans up the tendon, removing only the damaged tissue.
Tendon Release
A commonly used surgery for tennis elbow is called a lateral epicondyle release. This surgery takes tension off the extensor tendon. The surgeon begins by making an incision along the arm over the lateral epicondyle. Soft tissues are gently moved aside so the surgeon can see the point where the extensor tendon attaches on the lateral epicondyle.
The extensor tendon is then cut where it connects to the lateral epicondyle. The surgeon splits the tendon and takes out any extra scar tissue. Any bone spurs found on the lateral epicondyle are removed. (Bone spurs are pointed bumps that can grow on the surface of the bones.) Some surgeons suture the loose end of the tendon to the nearby fascia tissue. (Fascia tissue covers the muscles and organs throughout your body.) The skin is then stitched together.
This surgery can usually be done on an outpatient basis, which means that you don’t have to stay overnight in the hospital. It can be done using a general anesthetic or a regional anesthetic. A general anesthetic puts you to sleep. A regional anesthetic blocks only certain nerves for several hours. For surgery on the elbow, you would most likely get an axillary block to numb your arm.
View animation of the procedure
Rehabilitation
How soon can I use my elbow again?
Nonsurgical Rehabilitation
In cases where the tendon is inflamed, nonsurgical treatment is usually only needed for four to six weeks. When symptoms are from tendonosis, you can expect healing to take longer, usually up to three months. If your tendonosis is severe, it may take at least six months for complete healing.
After Surgery
Rehabilitation takes much longer after surgery. Immediately after surgery, your elbow is placed in a removable splint that keeps your elbow bent at a 90-degree angle. Your first few therapy sessions may involve ice and electrical stimulation treatments to help control pain and swelling from the surgery. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
You will gradually work into more active stretching and strengthening exercises. You just need to be careful to avoid doing too much, too quickly. Active therapy starts about two weeks after surgery. Your therapist may begin with light isometric strengthening exercises. These exercises work the muscles of the forearm without straining the healing tissues. You will use your own muscle power in active range-of-motion exercises.
At about six weeks, you start doing more active strengthening. As you progress, your therapist will teach you exercises to strengthen and stabilize the muscles and joints of the wrist, elbow, and shoulder. You will also do exercises to improve fine motor control and dexterity of the hand. Some of the exercises you’ll do are designed get your hand working in ways that are similar to your work tasks and sport activities. Other exercises will work your elbow in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow.
You may require therapy for two to three months. It could take four to six months to get back to high-level sports and work activities. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Golfer’s Elbow
A Patient’s Guide to Medial Epicondylitis (Golfer’s Elbow)
Introduction
Medial epicondylitis is commonly known as golfer’s elbow. This does not mean that only golfers have this condition. But the golf swing is a common cause of medial epicondylitis. Many other repetitive activities can also lead to golfer’s elbow: throwing, chopping wood with an ax, running a chain saw, and using many types of hand tools. Any activities that stress the same forearm muscles can cause symptoms of golfer’s elbow.
This guide will help you understand
- what parts of the elbow are affected
- what causes golfer’s elbow
- how to make the pain go away
Anatomy
What parts of the elbow are affected?
Golfer’s elbow causes pain that starts on the inside bump of the elbow, the medial epicondyle. Wrist flexors are the muscles of the forearm that pull the hand forward. The wrist flexors are on the palm side of the forearm. Most of the wrist flexors attach to one main tendon on the medial epicondyle. This tendon is called the common flexor tendon.
Tendons connect muscle to bone. Tendons are made up of strands of a material called collagen. The collagen strands are lined up in bundles next to each other.
Because the collagen strands in tendons are lined up, tendons have high tensile strength. This means they can withstand high forces that pull against both ends of the tendon. When muscles work, they pull on one end of the tendon. The other end of the tendon pulls on the bone, causing the bone to move.
The wrist flexor muscles contract when you flex your wrist, twist your forearm down, or grip with your hand. The contracting muscles pull on the flexor tendon. The forces that pull on the tendon can build when you grip a golf club during a golf swing or do other similar actions.
Causes
Why did I develop golfer’s elbow?
Overuse of the muscles and tendons of the forearm and elbow are the most common reason people develop golfer’s elbow. Repeating some types of activities over and over again can put too much strain on the elbow tendons. These activities are not necessarily high-level sports competition. Shoveling, gardening, and hammering nails can all cause the pain of golfer’s elbow. Swimmers who try to pick up speed by powering their arm through the water can also strain the flexor tendon at the elbow.
In some cases, the symptoms of golfer’s elbow are due to inflammation. In an acute injury, the body undergoes an inflammatory response. Special inflammatory cells make their way to the injured tissues to help them heal. Conditions that involve inflammation are indicated by -itis on the end of the word. For example, inflammation in a tendon is called tendonitis. Inflammation around the medial epicondyle is called medial epicondylitis.
However, golfer’s elbow often is not caused by inflammation. Rather, it is a problem within the cells of the tendon. Doctors call this condition tendonosis. In tendonosis, wear and tear is thought to lead to tissue degeneration. A degenerated tendon usually has an abnormal arrangement of collagen fibers.
Instead of inflammatory cells, the body produces a type of cells called fibroblasts. When this happens, the collagen loses its strength. It becomes fragile and can break or be easily injured. Each time the collagen breaks down, the body responds by forming scar tissue in the tendon. Eventually, the tendon becomes thickened from extra scar tissue.
No one really knows exactly what causes tendonosis. Some doctors think that the forearm tendon develops small tears with too much activity. The tears try to heal, but constant strain and overuse keep re-injuring the tendon. After a while, the tendons stop trying to heal. The scar tissue never has a chance to fully heal, leaving the injured areas weakened and painful.
Symptoms
What does golfer’s elbow feel like?
The main symptom of golfer’s elbow is tenderness and pain at the medial epicondyle of the elbow. Pain usually starts at the medial epicondyle and may spread down the forearm. Bending your wrist, twisting your forearm down, or grasping objects can make the pain worse. You may feel less strength when grasping items or squeezing your hand into a fist.
Diagnosis
How can my doctor be sure I have golfer’s elbow?
Your doctor will first take a detailed medical history. You will need to answer questions about your pain, how your pain affects you, your regular activities, and past injuries to your elbow.
The physical exam is often most helpful in diagnosing golfer’s elbow. Your doctor may position your wrist and arm so you feel a stretch on the forearm muscles and tendons. This is usually painful with golfer’s elbow. Other tests for wrist and forearm strength are used to help your doctor diagnose golfer’s elbow.
You may need to get X-rays of your elbow. The X-rays mostly help your doctor rule out other problems with the elbow joint. The X-ray may show if there are calcium deposits on the medial epicondyle at the connection to the flexor tendon.
Golfer’s elbow symptoms are very similar to a condition called cubital tunnel syndrome. This condition is caused by a pinched ulnar nerve as it crosses the elbow on its way to the hand. If your pain does not respond to treatments for golfer’s elbow, your doctor may suggest tests to rule out problems with the ulnar nerve.
Related Document: A Patient’s Guide to Cubital Tunnel Syndrome
When the diagnosis is not clear, the doctor may order other special tests, such as a magnetic resonance imaging (MRI) scan or ultrasound. An MRI scan uses magnetic waves to create pictures of the elbow in slices. The MRI scan shows tendons as well as bones.
Ultrasound tests use high-frequency sound waves to generate an image of the tissues below the skin. As the small ultrasound device is rubbed over the sore area, an image appears on a screen. This type of test can sometimes show collagen degeneration.
Treatment
How can I make my pain go away?
Nonsurgical Treatment
The key to nonsurgical treatment is to keep the collagen from breaking down further. The goal is to help the tendon heal.
If the problem is caused by inflammation, anti-inflammatory medications such as ibuprofen may give you some relief. If inflammation doesn’t go away, your doctor may inject the elbow with cortisone. Cortisone is a powerful anti-inflammatory medication. Its benefits are temporary, but they can last for a period of weeks to several months.
Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for golfer’s elbow, but recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Doctors commonly have their patients with golfer’s elbow work with a physical or occupational therapist. At first, your therapist will give you tips on how to rest your elbow and how to do your activities without putting extra strain on your elbow. Your therapist may apply tape to take some of the load off the elbow muscles and tendons. You may use an elbow strap that wraps around the upper forearm in a way that relieves the pressure on the tendon attachment.
Your therapist may apply ice and electrical stimulation to ease pain and improve healing of the collagen. Therapy sessions may also include iontophoresis, which uses a mild electrical current to push anti-inflammatory medicine to the sore area. This treatment is especially helpful for patients who can’t tolerate injections. Exercises are used to gradually stretch and strengthen the forearm muscles.
Because tendonosis is often linked to overuse, your therapist will work with you to reduce repeated strains during activity. When symptoms are from a particular sport or work activity, your therapist will observe your style and motion with the activity. Your therapist may suggest ways to protect the elbow during your activities. Your therapist can also check your sports equipment and work tools and recommend ways to alter them to keep your elbow safe.
Surgery
Sometimes nonsurgical treatment fails to stop the pain or help patients regain use of the elbow. In these cases, surgery may be necessary.
Tendon Debridement
When problems are caused by tendonosis, surgeons may choose to take out (debride) only the affected tissues within the tendon. In these cases, the surgeon cleans up the tendon, removing only the damaged tissue.
Tendon Release
A commonly used surgery for golfer’s elbow is called a medial epicondyle release. This surgery takes tension off the flexor tendon. The surgeon begins by making an incision along the arm over the medial epicondyle. Soft tissues are gently moved aside so the surgeon can see the point where the flexor tendon attaches to the medial epicondyle.
The flexor tendon is then cut where it connects to the medial epicondyle. The surgeon splits the tendon and takes out any extra scar tissue. Any bone spurs found on the medial epicondyle are removed. (Bone spurs are pointed bumps that can grow on the surface of the bones.) Some surgeons suture the loose end of the tendon to the nearby fascia tissue. (Fascia tissue covers the muscles and organs throughout your body.)
The following images show each step
Your surgeon will look at the ulnar nerve, to make sure that it is not being pinched. If the nerve looks fine, the skin is then stitched together.
View animation of the Procedure
This surgery can usually be done on an outpatient basis, which means that you don’t have to stay overnight in the hospital. It can be done using a general anesthetic or a regional anesthetic. A general anesthetic puts you to sleep. A regional anesthetic blocks only certain nerves for several hours. For surgery on the elbow, you would most likely get an axillary block to numb your arm.
Rehabilitation
How soon can I use my elbow again?
Nonsurgical Rehabilitation
In cases where the tendon is inflamed, nonsurgical treatment is usually only needed for four to six weeks. When symptoms are from tendonosis, you can expect healing to take longer, usually up to three months. If the tendonosis is chronic and severe, complete healing can take up to six months.
After Surgery
Recovery from surgery takes longer. Immediately after surgery, your elbow is placed in a removable splint that keeps your elbow bent at a 90-degree angle. Ice and electrical stimulation treatments may be used during your first few therapy sessions to help control pain and swelling from the surgery. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasm and pain.
You will gradually work into more active stretching and strengthening exercises. You just need to be careful to avoid doing too much, too quickly. Active therapy starts about two weeks after surgery. Your therapist may begin with light isometric strengthening exercises. These exercises work the muscles of the forearm without straining the healing tissues. You will use your own muscle power in active range-of-motion exercises.
At about six weeks, you start doing more active strengthening. As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints of the wrist, elbow, and shoulder. You’ll also do exercises to improve fine motor control and dexterity of the hand. Some of the exercises you’ll do are designed to work your hand and elbow in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow.
You may need therapy for two to three months. It may take four to six months to get back to high-level sports and work activities. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
Olecranon Bursitis
A Patient’s Guide to Olecranon Bursitis
Introduction
Olecranon bursitis is inflammation of a small sac of fluid located on the tip of the elbow. This inflammation can cause many problems in the elbow.
This guide will help you understand
- how olecranon bursitis develops
- why the condition causes problems
- what can be done for olecranon bursitis
Anatomy
Where is the olecranon bursa, and what does it do?
A bursa is a sac made of thin, slippery tissue. Bursae occur in the body wherever skin, muscles, or tendons need to slide over bone. Bursae are lubricated with a small amount of fluid inside that helps reduce friction from the sliding parts.
The olecranon bursa is located between the tip, or point, of the elbow (called the olecranon) and the overlying skin. This bursa allows the elbow to bend and straighten freely underneath the skin.
Related Document: A Patient’s Guide to Elbow Anatomy
Causes
How does olecranon bursitis develop?
Bursitis is the inflammation of a bursa. The olecranon bursa can become irritated and inflamed in a number of ways.
In some cases, a direct blow or a fall onto the elbow can damage the bursa. This usually causes bleeding into the bursa sac, because the blood vessels in the tissues that make up the bursa are damaged and torn. In the skin this would simply form a bruise, but in a bursa blood may actually fill the bursa sac. This causes the bursa to swell up like a rubber balloon filled with water.
The blood in the bursa is thought to cause an inflammatory reaction. The walls of the bursa may thicken and remain thickened and tender even after the blood has been absorbed by the body. This thickening and swelling of the bursa is referred to as olecranon bursitis.
Olecranon bursitis can also occur over a longer period of time. People who constantly put their elbows on a hard surface as part of their activities or job can repeatedly injure the bursa. This repeated injury can lead to irritation and thickening of the bursa over time. The chronic irritation leads to the same condition in the end: olecranon bursitis.
The olecranon bursa can also become infected. This may occur without any warning, or it may be caused by a small injury and infection of the skin over the bursa that spreads down into the bursa. In this case, instead of blood or inflammatory fluid in the bursa, it becomes filled with pus. The area around the bursa becomes hot, red, and very tender.
Symptoms
What does olecranon bursitis feel like?
Olecranon bursitis causes pain and swelling in the area at the tip of the elbow. It may be very difficult to put the elbow down on a surface due to the tenderness. If the condition has been present for some time, small lumps may be felt underneath the skin over the olecranon. Sometimes these lumps feel as though something is floating around in the olecranon bursa, and they can be very tender. These lumps are usually the thickened folds of bursa tissue that have formed in response to chronic inflammation.
The bursa sac may swell and fill with fluid at times. This is usually related to your activity level, and more activity usually causes more swelling. Over time the bursa can grow very thick, almost like an elbow pad on the olecranon.
Finally, if the bursa becomes infected, the elbow becomes swollen and very tender and warm to the touch around the bursa. You may run a fever and feel chills. An abscess, or area of pus, may form on the elbow. If the infection is not treated quickly, the abscess may even begin to drain, meaning the pus begins to seep out.
Diagnosis
How do doctors identify the condition?
The diagnosis of olecranon bursitis is usually obvious from the physical examination. In cases where the elbow swells immediately after a fall or other injury to the elbow, X-rays may be necessary to make sure that the elbow isn’t fractured. Usually chronic olecranon bursitis is also easy to diagnose without any special tests.
If your doctor is uncertain whether or not the bursa is infected, a needle may be inserted into the bursa and the fluid removed. This fluid will be sent to a lab for tests. The results are used to determine whether infection is present. If so, the type of bacteria that is causing the infection is identified. Your doctor will use this information to know what antibiotic will work best to cure the infection.
Treatment
What can be done for olecranon bursitis?
Nonsurgical Treatment
Olecranon bursitis that is caused by an injury will usually go away on its own. The body will absorb the blood in the bursa over several weeks, and the bursa should return to normal. If swelling in the bursa is causing a slow recovery, a needle may be inserted to drain the blood and speed up the process. There is a slight risk of infection in putting a needle into the bursa.
View animation of draining the bursa
Chronic olecranon bursitis is sometimes a real nuisance. The swelling and tenderness get in the way and causes pain. This can create a hardship both at work and during recreational activities. Treatment usually starts by trying to control the inflammation. This may include a short period of rest. Medications such as ibuprofen and aspirin may be suggested by your doctor to control the inflammation and swelling. An elbow pad might be useful in making it easier to put the elbow on hard surfaces.
If the bursa remains filled with fluid, a needle can be inserted and the fluid drained. During the drainage procedure, if there is no evidence of infection, a small amount of cortisone can be injected into the bursa to control the inflammation. Again, there is a small risk of infection if the bursa is drained with a needle.
Your doctor may also prescribe professional rehabilitation to evaluate and treat the problems that are causing your symptoms. Your physical or occupational therapist may suggest the use of heat, ice, and ultrasound to help calm pain and swelling. You may be given tips and strategies to avoid repetitive elbow motion and to do your activities without putting extra pressure on your elbows.
If an infection is found to be causing the olecranon bursitis, the bursa will need to be drained with a needle, perhaps several times over the first few days. You will be placed on antibiotics for several days.
Surgery
Bursa Drainage
If the infection is slow to heal, the bursa may have to be drained surgically. This method is different than the nonsurgical drainage mentioned earlier. Surgery to drain the bursa begins with an incision to open the bursa. The skin and bursa are kept open by inserting a drain tube into the bursa for several days. This allows the pus to drain and helps the antibiotics clear up the infection.
Bursa Removal
Surgery is sometimes necessary to remove a thickened bursa that has not improved with any other treatment. Surgical removal is usually done because the swollen bursa is restricting your activity.
To remove the olecranon bursa, an incision is made over the tip of the elbow. Since the bursa is outside of the elbow joint, the joint is never entered. The thickened bursa sac is removed, and the skin is repaired with stitches. Your elbow may be placed in a splint to rest the elbow and prevent it from moving for a few days. This allows the wound to begin to heal and prevents bleeding into the area where the bursa was removed.
Some types of bursae will grow back after surgery, because the skin needs to slide over the olecranon smoothly. The body forms another bursa as a response to the movement of the olecranon against the skin during the healing phase. If all goes well, the bursa that returns after surgery will not be thick and painful, but more like a normal bursa.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
Chronic olecranon bursitis will usually improve over a period of time from weeks to months. The fluid-filled sac is not necessarily a problem. If it does not cause pain, it is not always a cause for alarm or treatment. The sac of fluid may come and go with variation in activity. This is normal.
After Surgery
If surgery is required, you and your surgeon will come up with a plan for your rehabilitation. You will have a period of rest. You will also need to start a careful and gradual exercise program. Patients often work with a physical or occupational therapist to direct the exercises for their rehabilitation program after surgery.
Elbow Arthritis
A Patient’s Guide to Osteoarthritis of the Elbow
Introduction
The elbow joint is injured less often than many other joints in the body. The most common injuries of the elbow joint are fractures and dislocations. Most elbow injuries tend to heal pretty well.
However, an elbow injury can lead to problems later in life. The injury changes the way the joint works just enough to cause extra wear and tear to the surfaces of the joint. Over time, the joint degenerates, causing pain and difficulty with daily activities. This condition is called osteoarthritis, degenerative arthritis, or posttraumatic arthritis.
This guide will help you understand
- how elbow osteorarthritis develops
- how elbow osteoarthritis is diagnosed
- what can be done to ease the pain and regain elbow movement
Anatomy
What parts of the elbow are affected?
The elbow joint is made up of three bones: the humerus bone of the upper arm, and the ulna and radius bones of the forearm.
The ulna and the humerus meet at the elbow and form a hinge. This hinge allows the arm to straighten and bend. The large triceps muscle in the back of the arm attaches to the point of the ulna (the olecranon). When the triceps muscle contracts, it straightens out the elbow. The biceps muscles in the front of the arm contract to bend the elbow.
View animation of hinge movement
The connection of the radius to the humerus and the ulna allows the forearm to rotate. The upper end of the radius is round. It turns against the ulna and the humerus as the forearm and hand turn from palm down (pronation) to palm up (supination).
View animation of pronation/supination
In the elbow joint, the ends of the bones are covered with articular cartilage. Articular cartilage is a slick, smooth material. It protects the bone ends from friction when they rub together as the elbow moves. Articular cartilage is soft enough to act as a shock absorber. It is also tough enough to last a lifetime, if it is not injured.
Causes
What causes osteoarthritis?
Osteoarthritis is caused by degeneration of the articular cartilage of a joint. Degeneration is wear that happens over time. Doctors use the term degenerative arthritis to describe the wear and tear of a joint over many years. Degenerative arthritis is another term for osteoarthritis.
View animation of degeneration
Related Document: A Patient’s Guide to Osteoarthritis
Some doctors use the term degenerative arthrosis. (Arthrosis just means that the joint is wearing out.) Arthritis is technically a condition of joint inflammation. Often, joints with osteoarthritis aren’t inflamed. The term arthritis should really only be used to describe true inflammatory conditions, such as gout, infection, and rheumatoid arthritis.
A bad sprain or fracture can actually damage the articular cartilage. The cartilage can also be bruised when too much pressure is put on the cartilage surface. Osteoarthritis (OA) may be idiopathic, meaning there isn’t a known reason for the condition. But most of the time, elbow osteoarthritis is linked with excess use of the arm.
The cartilage surface may not look any different. The injury often doesn’t show up until months later. Sometimes the damage to the cartilage is severe. Pieces of the cartilage can actually be ripped away from the bone. These pieces do not grow back. Usually they must be surgically removed. If the pieces aren’t removed, they may float around in the joint, causing it to catch. These pieces are referred to as loose bodies. They can also cause a lot of pain and do more damage to the joint surfaces.
Your body does not do a good job of repairing these holes in the cartilage surface. The holes fill up with scar tissue. Scar tissue is not as slick or rubbery as the articular cartilage.
An injury doesn’t have to damage the cartilage to start the process of osteoarthritis. Any injury to the elbow joint can change the way the joint works. For example, after an elbow fracture the bone fragments may not line up exactly. They heal slightly differently from their condition before the injury. Even this slight difference can cause the joint to begin the cycle of wear and tear.
A dislocation can also cause lasting damage. After the ligaments have been injured in a dislocation, the elbow joint may move differently. This change in movement alters the forces on the articular cartilage. It’s just like a machine, if the mechanism is out of balance, it wears out faster.
Over many years, this imbalance in joint mechanics can damage the articular cartilage. Since articular cartilage cannot heal itself very well, the damage adds up. Finally, the joint can no longer compensate for the damage, and the elbow begins to hurt.
Osteoarthritis of the elbow isn’t like OA of the hip or knee. Most of the time, the articular cartilage isn’t damaged. The joint space remains close to normal. The biggest changes are hypertrophic osteophyte (bone spur) formation and capsular contracture.
Capsular contracture refers to the process by which the capsule dries out and tightens up. The capsule has two layers: a fibrous covering that surrounds the joint and an inner lining. The inner layer is called the synovium. The synovial layer holds the lubricating fluid inside the joint.
Symptoms
What symptoms does osteoarthritis cause?
Pain and stiffness are the main symptoms of osteoarthritis of any joint. At first, the pain comes only with activity. Most of the time the pain lessens while doing the activity, but after resting for several minutes pain and stiffness increase. As the condition worsens, you may feel pain even when resting. The pain may interfere with sleep.
You may have swelling around your elbow. Your elbow joint may fill with fluid and feel tight, especially after using it. When all the articular cartilage is worn off the joint surface, you may begin hearing a squeak and feel a creak in the joint when you move your elbow. This creaking sensation is called crepitus.
Osteoarthritis eventually affects the elbow’s motion. The elbow joint is one of the most sensitive to injury. It quickly becomes stiff and loses motion. The first thing most people notice is that it becomes hard to completely straighten the arm. Later they find it hard to bend.
Loss of motion leads to weakness and decreased function. Carrying heavy objects at the side of the body with the elbow straight is especially difficult.
Diagnosis
How will my doctor know if I have osteoarthritis?
The diagnosis of osteoarthritis of the elbow begins with a medical history of the problem. Your doctor will ask may questions about your pain, how it affects your daily activities, and any past injuries to your elbow. Because osteoarthritis develops over a long time, you may be asked questions about things you did long ago.
For example, throwing athletes (such as baseball pitchers) have a higher risk of developing osteoarthritis of the elbow later in life. Men with a history of heavy use of the arm are also at risk. This includes manual laborers and weight lifters.
Your doctor will also do a physical examination of the elbow and possibly other joints in the body. The moving and prodding may hurt, but it is important that your doctor sees exactly where and when you feel pain. Your doctor will feel for catching sensations as the joint moves. Catching may be caused by loose fragments of cartilage and bone. (These fragments are sometimes called joint mice.)
You will probably need to get standard X-rays. X-rays are usually the best way to see what is happening with your bones. X-rays can help your doctor assess the damage and track how your joint changes over time. X-rays can also help your doctor see how many bone spurs are present and if there are any loose bodies in the joint. X-rays also show the size of the joint space and how much articular cartilage is left.
CT scans give a 3-D view to show the size and location of any bone spurs present. CT scans can reveal osteophytes that don’t appear on plain X-rays. CT scans also show the surgeon how close the bone spurs are to the ulnar nerve. This information is very useful when planning surgery to remove the spurs.
Your doctor may order blood tests if there is any question about the cause of your osteoarthritis. Blood tests can show certain systemic diseases, such as rheumatoid arthritis.
Related Document: A Patient’s Guide to Rheumatoid Arthritis
Treatment
What can be done to get rid of my pain?
Nonsurgical Treatment
In almost all cases, doctors try nonsurgical treatments first. Surgery is usually not considered until it has become impossible to control your symptoms.
The goal of nonsurgical treatment is to help you manage your pain and use your elbow without causing more harm. Your doctor may recommend nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, to help control swelling and pain. Other treatments, such as heat, may also be used to control your pain.
Rehabilitation services, such as physical and occupational therapy, have a critical role in the treatment plan for elbow osteoarthritis. The main goal of therapy is to help you learn how to control symptoms and maximize the health of your elbow. You’ll learn ways to calm your pain and symptoms. You may use rest, heat, or topical rubs.
You may be issued a special elbow splint to immobilize and protect the elbow. Resting the joint can help ease pain and inflammation. Range-of-motion and stretching exercises can improve your elbow flexibility. Strengthening exercises for the arm help steady the elbow and protect the joint from shock and stress. Your therapist will give you tips on how to get your tasks done with less strain on the joint.
To get rid of your pain, you may also need to modify or limit your activities. You may even need to change jobs, if your work requires heavy, repetitive motions with the hand and wrist.
An injection of cortisone into the elbow joint can give temporary relief. Cortisone is a powerful anti-inflammatory medication. It can very effectively relieve pain and swelling. Its effects are temporary, usually lasting several weeks to months. There is a small risk of infection with any injection into the joint, and cortisone injections are no exception.
Surgery
Eventually, it may be necessary to consider some type of surgical treatment. There are several operations to treat advanced osteoarthritis of the elbow. Your surgeon will consider many factors when deciding which procedure is best for you, including the severity of joint degeneration, your age, your activity level, and how you use your elbow.
Arthroscopic Debridement
If you are in an early stage of osteoarthritis, your doctor may recommend arthroscopic debridement. Other names for this procedure include arthroscopic ulnohumeral arthroplasty or osteocapsular arthroplasty.
Arthroscopic procedures use an arthroscope, a tiny TV camera that is inserted into the joint through a very small incision. The arthroscope allows the surgeon to see inside the elbow joint.
In arthroscopic debridement, the surgeon makes other small incisions for inserting special tools to get rid of bone spurs, remove loose bodies, or smooth the cartilage. Sometimes a capsular release is needed. The capsule is a fibrous covering around the joint. An incision is made in the tissue and the anterior (front) of the capsule is removed.
Your surgeon may also do lavage in the joint. Lavage involves rinsing the joint with a sterile saltwater solution. Lavage helps remove tiny debris that may be irritating the joint. The arthroscope allows the surgeon to watch what he or she is doing on a TV screen during the procedure.
The majority of patients treated with arthroscopic debridement for elbow osteoarthritis have less pain and more motion after surgery. Symptoms may come back in some patients, but they are usually less severe.
Related Document: A Patient’s Guide to Arthroscopy
Interposition Arthroplasty
Before the invention of high-quality artificial joints, surgeons used many techniques to keep the bone surfaces of arthritic joints from rubbing against each other. One of these techniques is distraction interposition arthroplasty. This procedure involves placing a piece of tendon or fascia between the bony surface of the elbow joint. (Fascia is a connective tissue, similar to tendon, that lies in a flat sheet. It covers the muscles and acts as a divider between different compartments of the body.)
As the joint heals, the tendon or fascia forms a cushion of thick, tough tissue between the bones. The tissue pads the ends of the bones and reduces pain while still allowing the elbow to move.
Interposition arthroplasty is rarely indicated but may be used in rare cases. It works fairly well in the elbow. It doesn’t work very well in the weight-bearing joints of the hip, knee, and ankle.
Related Document: A Patient’s Guide to Interposition Arthroplasty of the Elbow
Elbow Fusion
A fusion surgery (also called arthrodesis) eliminates pain by making the bones of the joint grow together, or fuse, into one solid bone. Fusions were very common before the invention of artificial joints. Even today, joint fusions are commonly used in many different joints to get rid of the pain of arthritis.
An elbow fusion will greatly decrease the motion in your arm. However, it does leave you with a strong and pain-free elbow. People who need a good range of motion in their elbow should consider another type of operation, such as an elbow joint replacement.
Related Document: A Patient’s Guide to Elbow Fusion
Elbow Joint Replacement
Elbow joint replacement or total elbow arthroplasty (TEA) is not nearly as common as hip, knee, or shoulder replacement. This is true for a couple of reasons. Osteoarthritis in the elbow is not as common as osteoarthritis in weight-bearing joints.
Elbow joint replacement also has a higher complication rate than the more common replacement surgeries. Infection and slowed healing in the surgical incision are two complications of this type of procedure. Fracture, dislocation, and loosening are other problems reported with total elbow arthroplasty (TEA).
The elbow joint replacement is a good choice for patients who need improved motion rather than strength. Older patients who don’t need as much strength will probably prefer the results of elbow replacement surgery. They must be willing to accept low levels of activity involving the elbow. Patients with advanced rheumatoid arthritis are also good candidates for total elbow arthroplasty (TEA).
Related Document: A Patient’s Guide to Artificial Joint Replacement of the Elbow
Rehabilitation
When will I be able to use my elbow again?
Nonsurgical Rehabilitation
If you don’t need surgery, range-of-motion exercises for the elbow should be started as pain eases. These exercises are followed by a program of strengthening that may include shoulder and upper back exercises. You’ll be given tips on keeping your symptoms under control. You will probably progress to a home program within four to six weeks.
After Surgery
Your elbow will be bandaged with a well-padded dressing and an elbow splint for support. Physical or occupational therapy sessions may be needed for up to three months after surgery. The first few treatment sessions will focus on controlling the pain and swelling from surgery. You will then begin to do exercises that help strengthen and stabilize the muscles around the elbow joint. Your therapist will give you tips on ways to do your activities without straining your elbow.
Radial Tunnel Syndrome
A Patient’s Guide to Radial Tunnel Syndrome
Introduction
Radial tunnel syndrome happens when the radial nerve is squeezed where it passes through a tunnel near the elbow. The symptoms of radial tunnel syndrome are very similar to the symptoms of tennis elbow (lateral epicondylitis). There are very few helpful tests for radial tunnel syndrome, which can make it hard to diagnose.
This document will help you understand
- what parts of the elbow are affected
- the causes of radial tunnel syndrome
- ways to make the pain go away
Anatomy
What is the radial tunnel?
The radial nerve starts at the side of the neck, where the individual nerve roots leave the spine. The nerve roots exit through small openings between the vertebrae. These openings are called neural foramina.
The nerve roots join together to form three main nerves that travel down the arm to the hand. One of these nerves is the radial nerve. The nerve passes down the back of the upper arm. It then spirals outward and crosses the outside (the lateral part) of the elbow before it winds its way down the forearm and hand.
On the lateral part of the elbow, the radial nerve enters a tunnel formed by muscles and bone. This is called the radial tunnel.
Passing through the radial tunnel, the radial nerve runs below the supinator muscle. The supinator muscle lets you twist your right hand clockwise. This is the motion of using a screwdriver to tighten a screw.
After the radial nerve passes under the supinator muscle, it branches out and attaches to the muscles on the back of the forearm.
Related Document: A Patient’s Guide to Elbow Anatomy
Causes
What causes the pain of radial tunnel syndrome?
Pain is caused by pressure on the radial nerve. There are several spots along the radial tunnel that can pinch the nerve. If the tunnel is too small, it can squeeze the nerve and cause pain. Repetitive, forceful pushing and pulling, bending of the wrist, gripping, and pinching can also stretch and irritate the nerve.
Sometimes a direct blow to the outside of the elbow can injure the radial nerve. Constant twisting movements of the arm, common in assembly work, can also pinch the radial nerve and lead to radial tunnel syndrome.
Symptoms
What does radial tunnel syndrome feel like?
The symptoms of radial tunnel syndrome are tenderness and pain on the outside of the elbow. The symptoms of radial tunnel syndrome are very similar to the symptoms of tennis elbow. As in tennis elbow, pain from radial tunnel syndrome often starts near the lateral epicondyle. (The lateral epicondyle is a bony point on the outside of your elbow joint.) The pain gets worse when you bend your wrist backward, turn your palm upward, or hold something with a stiff wrist or straightened elbow.
One difference between radial tunnel syndrome and tennis elbow is the exact location of the pain. In tennis elbow, the pain starts where the tendon attaches to the lateral epicondyle. In radial tunnel syndrome, the pain is centered about two inches further down the arm, over the spot where the radial nerve goes under the supinator muscle. Radial tunnel syndrome may also cause a more achy type of pain or fatigue in the muscles of the forearm. Nerve pressure inside the radial tunnel leads to weakness in the muscles on the back of the forearm and wrist, making it difficult to steady the wrist when grasping and lifting. It can even lead to wrist drop, meaning the back of the hand can’t be cocked up. Skin sensation is not changed because the sensory portion of the radial nerve branches off above the elbow and does not enter the radial tunnel.
Diagnosis
How will my doctor know I have radial tunnel syndrome?
The diagnosis of radial tunnel syndrome can be difficult. Many cases are initially diagnosed as tennis elbow. Tests don’t always help tell the two conditions apart.
Your doctor will take a detailed medical history. You will be asked questions about your pain, your activities, and any past injuries to your elbow.
Your doctor will then do a physical examination to look for the most painful spot. The prodding and movement may hurt. But it is important that your doctor know exactly where and when you have pain. Pinpointing the source of the pain will be most helpful in determining whether you have radial tunnel syndrome or tennis elbow.
You may do some tests of the radial nerve. An electromyogram (EMG) tests to see if the muscles of the forearm are working properly. If the test shows a problem with the muscles, it may be caused by a problem with the radial nerve. The nerve conduction velocity (NCV) test measures the speed of an electrical impulse as it travels along the radial nerve. If the speed is too slow, then the nerve is probably pinched.
These tests are not very accurate in diagnosing radial tunnel syndrome. Many people who have radial tunnel syndrome will have normal EMG and NCV test results. Your doctor will consider all parts of the examination in diagnosing whether or not you have a problem with radial tunnel syndrome.
Treatment
How can I make my pain go away?
Treating radial tunnel syndrome can be frustrating, for you and your doctor. Getting your symptoms under control and helping you regain the use of your elbow can be a challenge.
Nonsurgical Treatment
The most important part of your treatment is to avoid the activity that caused the problem in the first place. You need to avoid repetitive activities that require your wrist to be repeatedly bent backwards. Repeated use of the wrist in twisting motions (such as using a screwdriver) also make the problem worse. If your work tasks caused your condition, you need to modify your work site or your duties. This is crucial for treatment to be successful. You need to take frequent breaks as you work and play. You also need to limit heavy pushing, pulling, and grasping.
If symptoms are worse at night, you may want to wear a lightweight plastic arm splint while you sleep. This limits your elbow movements at night and eases further irritation. This may let the elbow rest, giving the nerve time to recover from irritation and pressure.
Doctors commonly have their patients with radial tunnel syndrome work with a physical or occupational therapist. At first, your therapist will give you tips on how to rest your elbow and how to do your activities without putting extra strain on your elbow. Your therapist may apply ice and electrical stimulation to ease pain. Exercises are used to gradually stretch and strengthen the forearm and muscles.
Surgery
Sometimes symptoms of radial tunnel syndrome aren’t relieved, even after many months of nonsurgical treatment. In these cases, surgery may be the best treatment option. It is generally considered a last resort.
The goal of surgery for radial tunnel syndrome is to relieve any abnormal pressure on the nerve where it passes through the radial tunnel. The surgeon begins by making an incision along the outside of the elbow and down the forearm, near the spot where the radial nerve goes under the supinator muscle.
Soft tissues are gently moved aside so the surgeon can check the places where the radial nerve may be getting squeezed within the radial tunnel. The nerve can be pinched in many spots, so it is important to check all the areas that may be causing problems. Any parts of the tunnel that are pinching the nerve are cut. This expands the tunnel and relieves pressure on the nerve. At the end of the procedure, the skin is stitched together.
Radial tunnel surgery can usually be done as an outpatient procedure. This means you won’t have to stay in the hospital overnight. Surgery can be done using a general anesthetic, which puts you to sleep, or a regional anesthetic. A regional anesthetic blocks nerves in only one part of your body. In this case, you would have an axillary block, which would affect only the nerves of the arm.
Rehabilitation
What can I expect after treatment?
Nonsurgical Rehabilitation
If nonsurgical treatments are successful, you may see improvement in four to six weeks. Your physical or occupational therapist will work with you to ease symptoms and improve elbow function. Special exercises may be used to help the radial nerve glide within the radial tunnel. Treatment progresses to include strengthening exercises that mimic daily and work activities.
You may need to continue wearing your wrist strap during the day and the elbow pad or splint at night to control symptoms. Try to do your activities using healthy body and wrist alignment. Limit activities that require repeated hand and forearm motions, heavy grasping, and twisting motions of the arm and hand.
After Surgery
If you have surgery for radial tunnel syndrome, your elbow will be placed in a removable splint and wrapped in a bulky dressing following surgery. You will probably need to attend occupational or physical therapy sessions for six to eight weeks, and you should expect full recovery to take three to four months.
You’ll begin doing active forearm range-of-motion exercises one week after surgery. Therapists also use ice packs, soft-tissue massage, and hands-on stretching to improve range of motion.
When the stitches are removed, you may start carefully strengthening your hand and forearm by squeezing and stretching special putty. Therapists also use isometric exercises to improve forearm and hand strength without straining the tissues near the radial tunnel.
As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints in the wrist, elbow, and shoulder. Other exercises are used to improve fine motor control and dexterity of the hand.
Some of the exercises you’ll do are designed get your elbow working in ways that are similar to your work tasks and sport activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your elbow. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.