A Patient’s Guide to Bipartite Patella in Children
Introduction
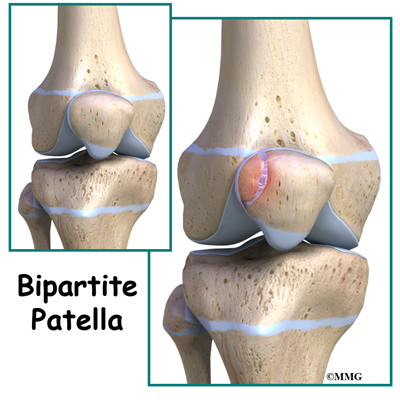
Bipartite patella is a congenital condition (present at birth) that occurs when the patella (kneecap) is made of two bones instead of a single bone. Normally, the two bones would fuse together as the child grows. But in bipartite patella, they remain as two separate bones. About one per cent of the population has this condition. Boys are affected much more often than girls.
This guide will help you understand
- what parts of the knee are involved
- how this condition develops
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What is the patella and what does it do?
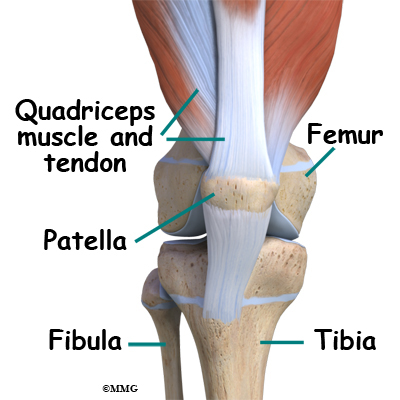
The knee is the meeting place of two important bones in the leg, the femur (the thighbone) and the tibia (the shinbone). The patella (kneecap) is the moveable bone that sits in front of the knee. This unique bone is wrapped inside a tendon that connects the large muscles on the front of the thigh, the quadriceps muscles, to the lower leg bone.
Related Document: A Patient’s Guide to Knee Anatomy
Causes
What causes this condition?
The patella starts out as a piece of fibrous cartilage. It turns into bone or ossifies as part of the growth process. Each bone has an ossification center. This is the first area of the structure to start changing into bone.
Most bones (including the patella) only have one primary ossification center. But in some cases, a second ossification center is present. Normally, these two centers of bone will fuse together during late childhood or early adolescence. If they don’t ossify together, then the two pieces of bone remain connected by fibrous or cartilage tissue. This connective tissue is called a synchondrosis.
The most common location of the second bone is the supero-lateral (upper outer) corner of the patella. But the problem can occur at the bottom of the patella or along the side of the kneecap.
Injury or direct trauma to the synchondrosis can cause a separation of this weak union leading to inflammation. Repetitive microtrauma can have the same effect. The cartilage has a limited ability to repair itself. The increased mobility between the main bone and the second ossification center further weakens the synchondrosis resulting in painful symptoms.
Symptoms
What does bipartite patella feel like?
Most of the time, there are no symptoms. Sometimes there is a bony bump or place where the bone sticks out more on one side than the other. If inflammation of the fibrous tissue between the two bones occurs, then painful symptoms develop directly over the kneecap. The pain is usually described as dull aching.There may be some swelling.
Movement of the knee can be painful, especially when bending the joint. Atrophy of the quadriceps and malalignment of the patella can lead to patellar tracking problems. Squatting, stair climbing, weight training, and strenuous activity aggravate the knee causing increased symptoms. For the runner, running down hill causes increased pain, tenderness, and swelling.
Diagnosis
How will my doctor diagnose this condition?
Most of the time, this condition is seen on X-rays of the knee that are taken for some other reason. This is referred to as an “incidental finding”. A radiolucent line is observed across the superior-lateral corner of the patella. This represents the extra ossification center and is seen most often in children between the ages of eight and 12. Sometimes, it is mistaken for a fracture of the patella. But since the problem usually affects both knees, an X-ray of the other knee showing the same condition can confirm the diagnosis.
MRIs or bone scans are useful when a fracture is suspected but doesn’t show up on the X-rays. The presence of fibrocartilaginous material between the two bones helps confirm a diagnosis of bipartite patella. An MRI can show the condition of articular cartilage at the patellar-fragment interface. The lack of bone marrow edema helps rule out a bone fracture. CT scans will show the bipartite fragment but are not as helpful as MRIs because bone marrow or soft tissue edema does not show up, so it’s still not clear from CT findings whether the symptoms are from the fragment or fracture.
Treatment
What treatment options are available?
Most of the time, no treatment is necessary. Most people who have a bipartite patella, probably don’t even know it. But if an injury occurs and/or painful symptoms develop, then treatment may be needed.
Nonsurgical Treatment
Conservative care involves rest, over-the-counter nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen, and activity modification. Avoiding deep flexion such as squatting, excess use of the stairs, and resisted weight training are advised.
Separation of the synchondrosis can be treated with immobilization for four to six weeks. The knee is placed in full extension using a cylinder cast, knee immobilizer, or dynamic patellar brace. An immobilizer is a removable splint. It’s usually only taken off to wash the leg and remains in place the rest of the time. The dynamic brace immobilizes the knee in an extended (straight-leg) position with limited flexion (up to 30 degrees). The brace reduces pain by decreasing the pull on the patella from the quadriceps muscle. Once healing occurs and the cast or brace is no longer needed, then stretching exercises of the quadriceps muscle are prescribed.
Surgery
If conservative care with immobilization is not successful in alleviating swelling and pain, then surgery may be suggested. When the bipartite fragment is small, then the surgeon can simply remove the smaller fragment of bone. When the bipartite fragment is larger and also contains part of the joint surface, the surgeon may decide to try and force the two fragments to heal together or fuse. The connective tissue between the two fragments is removed first and the two bony fragments are then held together or stabilized with a metal screw or pin. This is called internal fixation. The two fragments of bone heal together or fuse, creating a solid connection between the two fragments. Although successful in reuniting the patella, the procedure may require several weeks of immobilization. As a result, knee stiffness may occur. This usually requires physical therapy once the bones have healed to regain strength and motion.
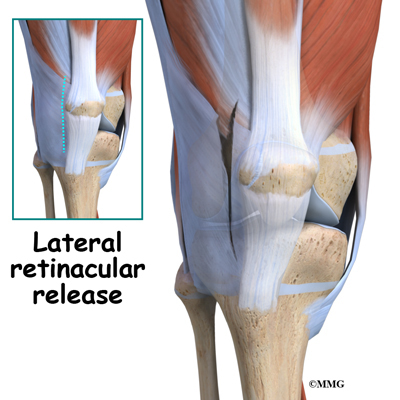
Another potential treatment option is a procedure called a lateral retinacular release. It may be beneficial to remove the constant pull of the vastus lateralis tendon (a part of the large quadriceps muscle of the thigh) where it attaches to the bone of the bipartite fragment of the upper, outer patella. Simply cutting this attachment reduces the constant pull on the bony fragment. Healing of the two fragments may occur as a result.
Rehabilitation
What should I expect after Treatment?
Nonsurgical Rehabilitation
Most patients respond well to activity modification and immobilization. When the X-ray shows complete ossification of the two bone fragments, then you’ll be able to return to your regular activities. If there is no improvement after three months of conservative care, then surgery is considered.
After Surgery
Usually, the removal of a bipartite patella is a simple surgery with prompt relief of pain and quick recovery. Athletes can expect full range of motion, a stable knee, and a fairly rapid return to normal activity (one to two months). But runners and other athletes who have had an extended time of immobility, muscle weakness and atrophy, loss of normal joint motion, and patellar tracking problems may require a special rehab program. A physical therapist will prescribe and monitor a rehabilitation program starting with range of motion and quadriceps strengthening exercises.
Athletes will be progressed quickly to restore full motion and strength. An aerobic program to improve cardiovascular endurance is often needed after so many months of inactivity. Proprioception and functional activities are added in order to prepare the individual to return to full sports participation. Proprioceptive exercises help restore the joint’s sense of position. Proprioceptive activities are needed to restore normal movement and prevent further injury.