A Patient’s Guide to Artificial Joint Replacement of the Finger
Introduction
If nonsurgical treatments are not successful in easing problems of finger arthritis, your doctor may recommend replacing the surfaces of the joint. Joint replacement surgery is called joint arthroplasty.
This guide will help you understand
- what parts make up the finger joint
- how the operation is performed
- what to expect before and after surgery
Anatomy
What parts of the finger are involved?
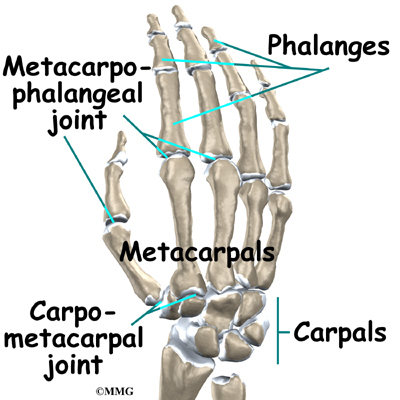
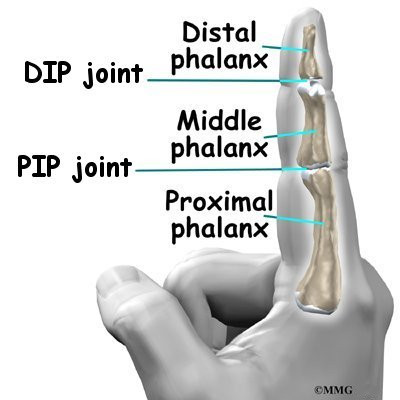
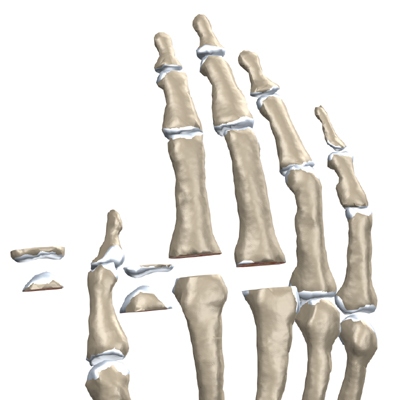
The finger joints work like hinges when the fingers bend and straighten. The main knuckle joint is the metacarpophalangeal joint (MCP joint). It is formed by the connection of the metacarpal bone in the palm of the hand to the finger bone, or phalanx. Each finger has three phalanges, separated by two interphalangeal joints (IP joints). The one closest to the MCP joint (knuckle) is called the proximal IP joint (PIP joint). The joint near the end of the finger is called the distal IP joint (DIP joint).
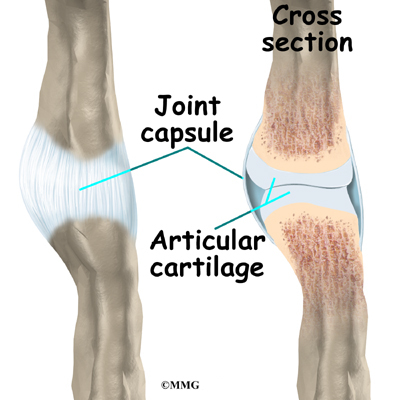
Ligaments are tough bands of tissue that connect bones together. Several ligaments hold each finger joint together. These ligaments join to form the joint capsule of the finger joint. The joint capsule is a watertight sac around the joint. The joint surfaces are covered with a material called articular cartilage. This material is the slick, spongy material that allows one side of a joint to slide against the other joint surface easily. When this material wears out, the joint develops a type of arthritis called osteoarthritis and becomes painful.
Related Document: A Patient’s Guide to Hand Anatomy
Rationale
What does the surgeon hope to achieve?
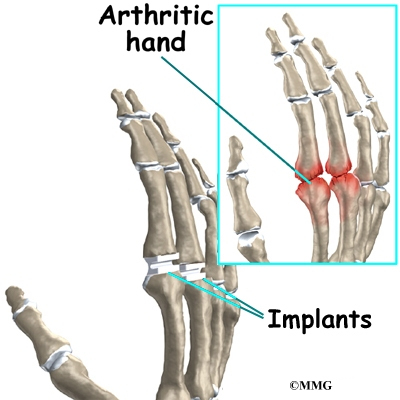
Arthritic joint surfaces can be a source of stiffness, pain, and swelling. The artificial joint is used to replace the damaged joint surfaces so patients can do their activities with freedom of movement and less pain.
Preparation
What should I do to prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. The length of time you spend in the hospital depends a lot on your recovery from anesthesia after surgery. In general, finger joint surgery can be done on an outpatient basis, meaning you can leave the hospital the same day.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let’s look first at the artificial finger joint itself.
The Artificial Finger Joint
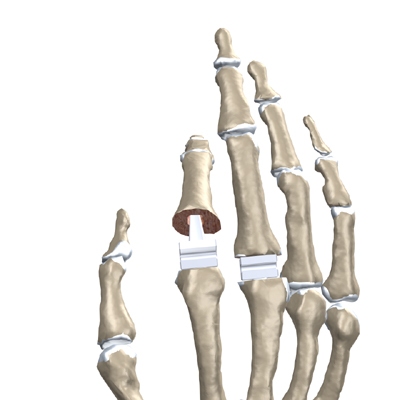
Surgeons use silicon plastic implants to replace the original joint surfaces. The artificial joint functions the same way a hinge on a door does.
The Operation
The procedure takes about two hours to complete. Surgery may be done using a general anesthetic, which puts you completely to sleep, or a local anesthetic, which numbs only the hand. With a local anesthetic you may be awake during the surgery, but you won’t be able to see the surgery.
Once you have anesthesia, your surgeon will make sure the skin of your hand is free of infection by cleaning the skin with a germ-killing solution.
An incision is made across the back of the finger joints that are to be replaced. The soft tissues are spread apart with a retractor. Special care is taken not to damage the nearby nerve that passes by the joint. The joint is exposed. The ends of the bones that form the finger joint surfaces are taken off, forming flat surfaces.
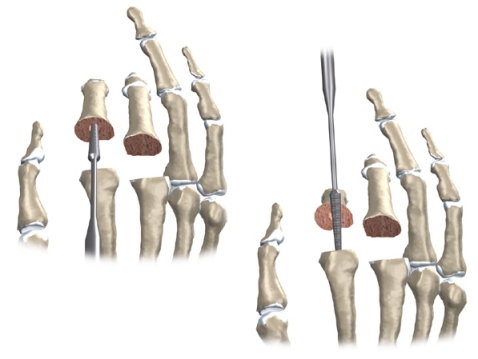
A burr (a small cutting tool) is used to make a canal into the bones that form the finger joint.
The surgeon then sizes the stem of the prosthesis to ensure a snug fit into the hollow bone marrow space of the bone. The prosthesis is inserted into the ends of both finger bones.
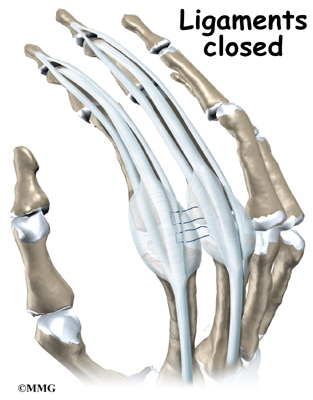
When the new joint is in place, the surgeon wraps the joint with a strip of nearby ligament to form a tight sac. This gives the new implant some added protection and stability.
The soft tissues are sewn together, and the finger is splinted and bandaged.
View animation of removing the joint surfaces
View animation of forming the canal in the bones of the finger
View animation of inserting the new finger joint
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following artificial finger joint replacement are
- anesthesia
- infection
- nerve damage
- prosthesis failure
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. Replacing the finger joint with an artificial joint is no different. You will probably be given antibiotics before the operation to reduce the risk of infection.
If an infection occurs you will most likely need antibiotics to cure it. You may need additional operations to drain the infection if it involves the area around either implant. In these cases, the artificial joint will need to be removed. The surgeon will most likely fuse the joint rather than attempt another artificial joint replacement.
Nerve Damage
All of the nerves and blood vessels that go to the finger travel across, or near, the finger joint. Since the operation is performed so close to these important structures, it is possible to injure either the nerves or the blood vessels during surgery. The result may be temporary if the nerves have been stretched by retractors holding them out of the way. It is uncommon to have permanent injury to either the nerves or the blood vessels, but it is possible.
Prosthesis Failure
One of the problems that occurs with artificial replacements is that they can fail. The older silicon-type prosthesis has been shown to break apart and fragment. Most types of prostheses can displace, or move out of the correct position, causing problems. Most of these problems will require a second operation to remove and replace the prosthesis.
After Surgery
What happens immediately after surgery?
After surgery, your finger will be bandaged with a well-padded dressing and a splint for support. The splint will keep the finger in a straightened position during healing. Some patients are placed in an arm-length cast with the finger in a straightened position for about three weeks after the prosthesis is implanted. Your surgeon will want to check your hand in five to seven days. Stitches will be removed after 10 to 14 days, though most of your stitches will be absorbed into your body. You may have some discomfort after surgery. You will be given pain medicine to control the discomfort you have.
You should keep your hand elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting up.
Rehabilitation
What should I expect during my rehabilitation?
A physical or occupational therapist will direct your recovery program. Recovery takes up to three months after a prosthesis is implanted.
The first few therapy treatments will focus on controlling the pain and swelling from surgery. Heat treatments may be used. Your therapist may also use gentle massage and other hands-on treatments to ease muscle spasm and pain.
Then you’ll begin gentle range-of-motion exercise. Strengthening exercises are used to give added stability around the finger joint. You’ll learn ways to grip and support items in order to do your tasks safely and with the least amount of stress on your new finger joint. As with any surgery, you need to avoid doing too much, too quickly.
Some of the exercises you’ll do are designed to get your hand and fingers working in ways that are similar to your work tasks and daily activities. Your therapist will help you find ways to do your tasks that don’t put too much stress on your finger joint. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.
The therapist’s goal is to help you keep your pain under control, improve your strength and range of motion, and regain your fine motor abilities with your hand and fingers. When you are well underway, regular visits to the therapist’s office will end. Your therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.