A Patient’s Guide to Back Pain in Children
Introduction
Until recently, a complaint of back pain in a child or adolescent was considered uncommon. It was usually associated with a certain condition such as tumor, curvature of the spine, a broken spinal bone, inflammation, or infection.
However, more recently, reports of back pain is much more common among children. By the age of 15, 20 to 70 percent of children will report back pain. It is seldom associated with a serious condition, particularly as age increases. Even though the majority of children will not have a serious condition, there is still a small portion that do.
This guide will give you a general overview of back pain in children. It will help you understand:
- What parts make up the spine
- What causes back pain in children
- How the diagnosis is made
- What treatment options are available
Anatomy
What parts make up the spine?
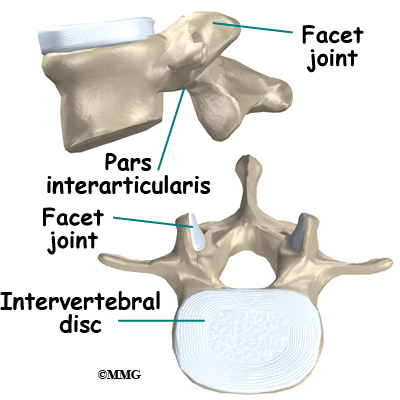
The spine is made up of a column of bones. Each bone, or vertebrae, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body, forming a canal for the spinal cord.
Facet joints are small joints on either side of the spine that allow motion. As the bones of the spine interlock, a facet joint is formed. Each vertebra will form two facet joints on either side. There is a pair at the top and a pair at the bottom of each vertebra. The area of the vertebrae bones that is between the upper and lower facet joints is called the pars articularis or pedicle.
Intervertebral discs form a cushion between the round blocks of bone making up the vertebral body. The area of the bone where the disc attaches to the vertebra is called an end plate. Discs are a collection of tough tissue similar to a ligament. They are filled with fluid when healthy.
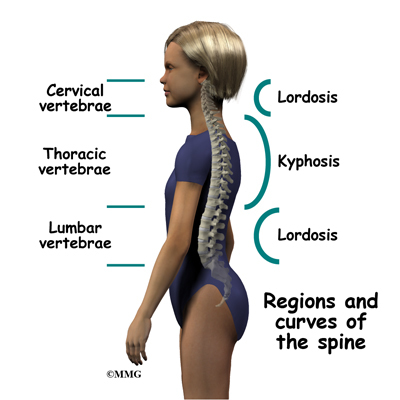
There are three general portions of the spinal column. The cervical or neck portion, the thoracic portion making up the mid-back, and the lumbar or lower portion. The lumbar portion connects with the pelvis at the sacrum.
There are specific curves associated with each region of the spine. When looking from the side, the cervical spine has an inward curve called a lordosis. The thoracic spine curves outward and is called a kyphosis. The lumbar spine usually has a lordosis. These three curves maintain balance of the spine in a forward and backward plane.
When these curves are exaggerated or absent, the condition is called scoliosis.
Causes
What can cause back pain in children?
There are several red flag warning signs that may suggest a specific cause for back pain. Night pain, constant pain, or pain that spreads into the buttocks or legs are some of them. Leg weakness or bowel and bladder problems can indicate nerve or spinal cord problems.
Conditions that can cause back pain are grouped into nonspecific, meaning the cause is unknown; and specific back pain, meaning there is an identified cause for the back pain.
Nonspecific back pain means that there is no specific structural reason or cause for back pain. Approximately 60 to 75 percent of children reporting back pain will have non-specific back pain. Their physical exam and X-rays will be normal. It is usually considered a muscle strain or from poor posture.
In some cases, non-specific back pain may be related to mood problems such as depression or anxiety. It sometimes is related to problems at school or with peers. Visits with a school counselor or psychologist may be recommended.
Approximately 25 to 40 percent of children will have changes in imaging studies (such as X-ray or MRI) that indicate a pathological (specific) cause for their back pain. These include the following:
Spondylolysis is a fracture of the pars interarticularis or pedicle(s), usually of the L5 or last lumbar vertebrae. This is most likely caused by an injury. It may also be caused by repetitive activity. The activities that most likely cause spondylolysis include extension (bending backwards) and rotation. Sports that put athletes at higher risk include ballet, gymnastics, football, high jumping, diving, rowing, and weight lifting.
Spondylolysis is a common cause for back pain in children, especially those that are active in sports. It may happen in four to five percent of children by the age of six, and up to six percent of adults. Spondylolyis is three times more common in boys than girls. Growth spurts and involvement in contact sports may explain the difference between boys and girls.
Early on, X-rays may not show a fracture. Special imaging such as MRI, CT, or SPECT bone scan may show signs of a stress fracture. Spondylolysis may cause pain in a particular spot in the low back and spasm of the muscles along the spine. Often it will cause pain into the buttocks or thighs. Spondylolysis will likely heal with a change in activity, rest, and avoiding hyperextension and rotation. Bracing may be helpful if symptoms do not get better.
Related Document: A Patient’s Guide to Lumbar Spondylolysis
Spondylolisthesis occurs when spondylolysis worsens or does not heal. It can cause slippage of one vertebra on the other. This slippage is called spondylolisthesis. The slippage is graded from I through IV, one being mild, IV often causing neurological symptoms.
Related Document: A Patient’s Guide to Lumbar Spondylolisthesis
Scoliosis or curvature of the spine may be a source of back pain in children. Most cases of scoliosis only require watching for worsening. However, some may need bracing and even surgery. Sometimes a scoliosis is caused by tumor or infection of the spine.
Related Document: A Patient’s Guide to Scoliosis
Scheuermann’s kyphosis is a deformity where there is wedging of three or more vertebrae in a row in the thoracic region. Wedging means that the vertebra is wider towards the back, and narrower towards the front. The vertebra has lost its usual rectangular shape. This causes increased curvature or forward bending of the spine. This curvature is called kyphosis. The curve from a sideways view can be 50 degrees or more. If the curvature is greater than 75 degrees, surgery to straighten the spine may be necessary.
Related Document: A Patient’s Guide to Scheuermann’s Disease
There may also be narrowing of the disc spaces between the vertebrae. Most of the time there are also Schmorl’s nodes seen in the endplate of a vertebral body or several vertebrae. On imaging studies these look like small hollowed areas.
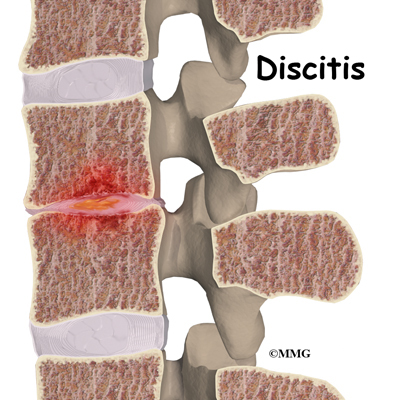
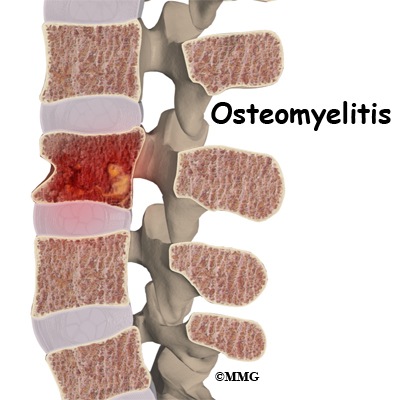
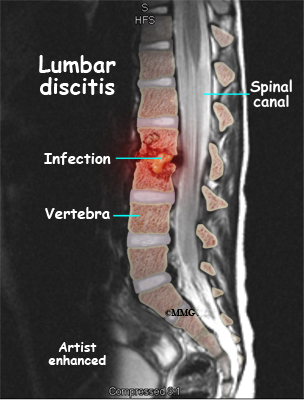
Discitis and vertebral osteomyelitis are rare in children. When a disc becomes inflamed and possibly infected, the condition is called discitis. If the vertebral bone becomes infected, the condition is called vertebral osteomyelitis.
Common symptoms of these conditions include refusal to crawl, sit, or walk and back pain. A limp and forward bending while placing the hands on thighs for support are also common signs. Fever of 102 degrees Fahrenheit or greater is common in vertebral osteomyelitis.
With discitis, the disc will appear narrowed on an X-ray or an MRI. Discitis usually happens in children less than five years old.
In vertebral osteomyelitis, the vertebral bone and surrounding tissue including the disc can become infected. On X-ray or MRI the bone and/or tissue can show destruction. Vertebral osteomyelitis tends to affect older children and adolescents.
Both conditions are treated with rest, antibiotics by IV and by mouth. A brace to support the spine may be suggested. Surgery may be necessary in osteomyelitis, to clean out the infection and/or to stabilize the spine.
Tumors are a rare cause of back pain in children. A tumor of the spine is an abnormal growth of tissue in or around the spinal column. There are many different types of spinal tumors. They can be benign or malignant. Benign means that the tumor does not spread to other parts of the body. It can still cause destruction of vertebral bone or spinal tissue. Some benign tumors can come back after they have been removed. Benign tumors include osteoid osteoma, osteoblastoma, and aneurysmal bone cysts. Malignant tumors are tumors that can spread to other parts of the body. These include sarcoma, leukemia, and lymphoma.
Related Document: A Patient’s Guide to Spinal Tumors
Symptoms
Depending on the age of the child, they may or may not be able to tell you about their symptoms.
In a younger child, refusal to crawl, sit, or walk may indicate back pain.
In older children, symptoms may include:
- Pain involving the spine
- Spasm of the nearby muscles
- Decreased range of motion or stiffness in the back
- Stiffness and pain after prolonged sitting or standing
- Pain with loading the spine as when lifting and carrying
- Pain may refer to areas away from the spine itself. It may cause pain in the buttocks or legs
- Leg weakness or bowel and bladder problems can indicate nerve or spinal cord problems
- Difficulty walking
- Fever
Diagnosis
How will my doctor diagnose this condition?
Your doctor will perform an examination that will include your history. It will include questions about activity, spinal injuries, urination, bowel movements, weakness, what makes the pain better and worse, when does the pain occur, etc. Your doctor may also ask questions about school, home, and your moods.
A physical examination will be done as well. This will include looking at the back to evaluate the curves of the spine, spasm of the muscles, and for unusual markings of the skin or soft tissue along the spine. Your doctor will also want to watch you move or walk, and evaluate the range of motion of the spine. Neurological examination may include checking reflexes, sensation, and muscle strength.
Imaging studies
X-rays are recommended for all children complaining of back pain. Views of the spine from the front, the side, and part way in between (oblique) should be taken. X-rays will show bone as well as the disc spaces.
Magnetic resonance imaging (MRI) allows your doctor to look at slices of the area in question. The MRI machine uses magnetic waves, not X-rays to show the soft tissues of the body. This includes the spinal cord, nerves, and discs. It can also evaluate spinal bones. The test may require the use of dye in an IV. Sedation or anesthesia may be needed to help you lie still for this test.
A computed tomography (CT) scan may be ordered. It is best for evaluating problems with the vertebral bones. It is usually tolerated by children, however, exposes them to radiation. Sometimes, it may require dye in the spinal canal fluid for easier identification of the spinal cord and nerve root anatomy. When dye is injected for this purpose, the technique is called a myelogram.
Bone Scans, also called nuclear scans can be used to detect fracture, bone infection, or tumor. A radioactive tracer, Technetium, is injected into your vein. Where there is increase in metabolic activity the Technetium will be more concentrated. This occurs when there is inflammation, fracture, infection, or tumor. Some tumors in the spine can spread to other parts of the body, or come from cancer somewhere else in the body. A scan can be helpful to see if there are other areas in the body where the cancer may be.
SPECT stands for Single Photon Emission Computed Tomography. SPECT imaging is often added to provide information that is not available on routine bone scan images. It provides three-dimensional (3-D) views of the area examined. Following a bone scan you will remain on the exam table and the camera will rotate around the table while it takes pictures. SPECT imaging adds 30 to 60 minutes to the time of the nuclear scan. Sedation may be needed.
A biopsy of the spine may be required if an infection or tumor is found. In some cases tissue samples can be taken with a needle. Sometimes tissue for a biopsy is taken during a minor surgery. This allows the doctor a better view of the area he neeeds to biopsy. The tissue is then looked at under a microscope.
Laboratory Studies
Blood tests may be requested to evaluate the blood for specific bacteria causing the infection. A complete blood count (CBC), especially in children under the age of 10 is important. There is a greater chance that back pain is from leukemia in children younger than 10. If there is an infection, the CBC may show an increase in the infection-fighting white blood cells. A C-reactive protein (C-RP) and erythrocyte sedimentation rate (ESR) may also show an increase when an infection is present. A blood culture may be necessary to help determine what bacteria are causing the infection in discitis or vertebral osteomyelitis.
A biopsy may be required to determine what bacteria are causing an infection. This will help your doctor choose the right antibiotic to treat the infection.
Treatment
What treatments are available?
Non-surgical treatment
Most treatment for back pain in children is non-surgical. Treatment of children with non-specific back pain includes change in activity and rest. Trunk strengthening and postural exercises with the help of a physical therapist may be useful. Short-term use of over-the-counter medications such as Ibuprofen (Advil, Motrin) may be beneficial. Weight loss may be recommended.
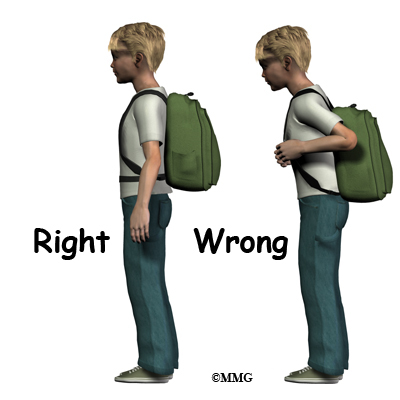
Carrying backpacks may sometimes be to blame for non-specific back pain. It is suggested that children wear their backpack using both shoulder straps. Making more frequent trips to the locker can decrease the weight of the backpack. Some children choose to use wheeled backpacks.
Treatment of non-specific back pain may include involving the school counselor or a psychologist. Children may complain of back pain when they are depressed or anxious. It may also indicate problems at home, in school, or with peers.
Bracing may also be required for proper treatment of some conditions.
Antibiotics either by IV and/or by mouth are necessary for the treatment of discitis and vertebral osteomyelitis.
Surgical treatment
Surgical treatment for back pain in children is rare.
If a tumor has been discovered as the source of your back pain, the treatment options will vary depending on the type of tumor found.
Some tumors are evaluated periodically on a watch and see basis. Surgery to remove the tumor is often recommended. If radiation or chemotherapy is required, you will be referred to an oncologist (cancer specialist). In the case of a tumor, radiation may begin as early as one to two weeks following surgery. Radiation usually lasts only 15 to 20 minutes per day for two to six weeks. Treatment options and the prognosis for many tumors have improved greatly in the past few years.
The spine may need to be stabilized due to scoliosis or kyphosis, or from the removal of a tumor or infection. Metal hardware such as screws, rods, plates, or cages may need to be used. The bone may also be supported by bone graft or bone cement.
Rehabilitation
What should I expect after treatment?
Non-surgical Rehabilitation
Periodic follow-up with your physician is required. Repeated or different imaging studies may be necessary, particularly if symptoms do not improve. Laboratory tests may need to be repeated.
Specific treatment by a physical therapist may be suggested. This treatment usually involves avoiding movements that could make the condition worse, posture training, as well as back and abdominal (core) strengthening. A physical therapist will also instruct you in safe lifting and proper body mechanics in other daily activities.
Surgical rehabilitation
If surgical intervention is required, your surgeon will require periodic follow-up visits. This could be on a long-term basis to watch for spinal deformity or recurrence of a tumor. Repeated or different imaging studies may be necessary. Laboratory tests may need to be repeated.
The amount of time you are hospitalized depends on the type of surgery required. After surgery, activity such as sitting, crawling, or walking are usually allowed as well as activities that do not require stretching of the spine or straining. Lifting is limited during the initial recovery period. You will likely be required to use a brace or corset after surgery to help with stability.
You may benefit from physical therapy and occupational therapy. Therapists can help with regaining strength, movement, coordination, and activities of daily living.