A Patient’s Guide to Endoscopic Carpal Tunnel Release
Introduction
Carpal tunnel syndrome (CTS) is a condition affecting the wrist and hand. While the most common surgical procedure for a carpal tunnel release is still the open-incision technique, some surgeons are using a new procedure, called endoscopic carpal tunnel release.
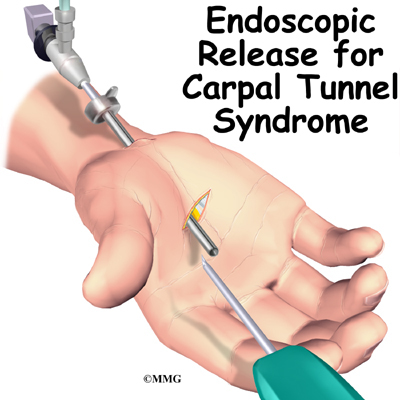
The procedure is done using an endoscope (a small, fiber-optic TV camera) to look into the carpal tunnel through a small incision just below the wrist. Using the camera allows the surgeon to release the ligament without disturbing the overlying tissues.
This guide will help you understand
- what part of the wrist is treated during surgery
- how surgeons perform the operation
- what to expect before and after the procedure
Related Document: A Patient’s Guide to Carpal Tunnel Syndrome
Anatomy
What part of the wrist is treated during surgery?
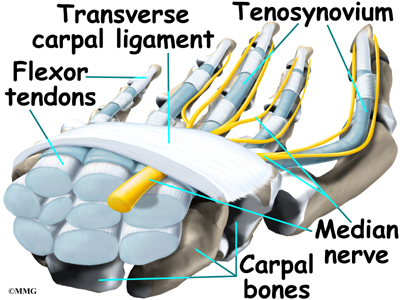
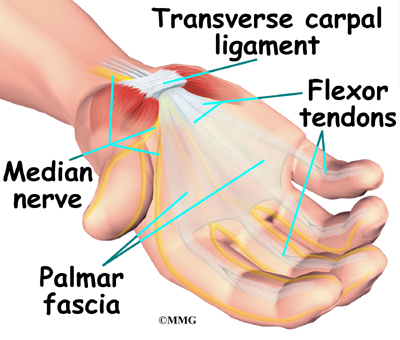
The carpal tunnel is an opening through the wrist into the hand that is formed by the bones of the wrist (carpal bones) on one side and the transverse carpal ligament on the other. (Ligaments connect bones together.) The transverse carpal ligament is at the base of the wrist and crosses from one side of the wrist to the other. (Transverse means across.) It is sometimes referred to as the carpal ligament.
The median nerve and the flexor tendons pass through the carpal tunnel. The median nerve rests on top of the tendons, just below the carpal ligament. Between the skin and the carpal ligament is a thin sheet of connective tissue called the palmar fascia.
Related Document: A Patient’s Guide to Hand Anatomy
Rationale
What does the surgeon hope to achieve?
The surgery releases the carpal ligament, taking pressure off the median nerve. By using the endoscope, surgeons can accomplish this without disrupting the nearby tissues.
Proponents of the procedure feel that patients heal faster, are able to use their hand faster, and have fewer problems of tenderness in the palmar incision. Other physicians are not convinced that this procedure for releasing the carpal ligament is better than the open-incision technique.
Related Document: A Patient’s Guide to Open Carpal Tunnel Release
The endoscopic method is more technically demanding and can be more expensive in most hospitals. There may be a higher complication rate with this procedure involving incomplete release of the carpal ligament or injury to the median nerve inside the carpal tunnel. As more and more surgeons choose to use this method, these questions will probably be resolved.
Preparation
What should I do to prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. This surgery can usually be done as an outpatient procedure, meaning you can leave the hospital the same day.
Surgical Procedure
What happens during the operation?
The surgery is occasionally done using a general anesthetic (one that puts you to sleep). More often, a regional anesthetic is used. A regional anesthetic blocks the nerves going to only a portion of the body. Injection of medications similar to lidocaine are used to block the nerves for several hours. This type of anesthesia could be an axillary block (only the arm is asleep) or a wrist block (only the hand is asleep). The surgery can also be performed by simply injecting lidocaine around the area of the incision.
Once you have anesthesia, your surgeon will make sure the skin of your palm is free of infection by cleaning the skin with a germ-killing solution.
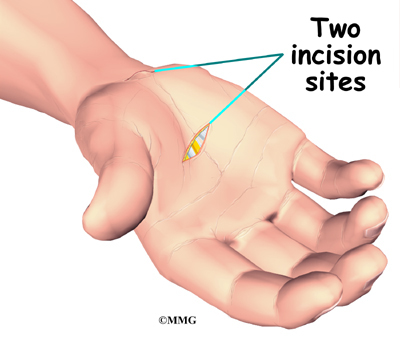
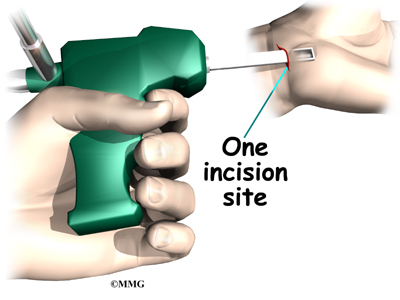
The surgeon nicks the skin to create a small opening just below the crease in the wrist where the palm starts. This opening allows the surgeon to place the endoscope into the carpal tunnel. Some surgeons make a second small incision within the palm of the hand.
The procedure using a single incision is becoming more popular. The incision allows the surgeon to open the carpal tunnel just below the carpal ligament.
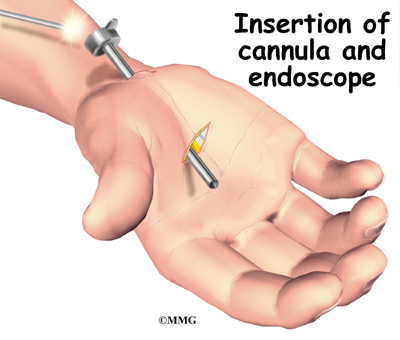
Once the surgeon is sure that the instruments can be passed into the carpal tunnel, a metal or plastic cannula (a tube with a slot on the side) is placed alongside the median nerve. The endoscope can be placed into the tube to look at the underside of the carpal ligament, making sure that the nerves and arteries are safely out of the way.
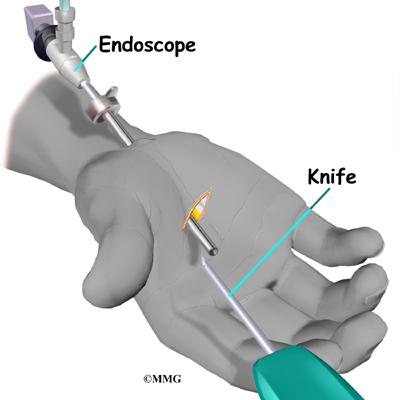
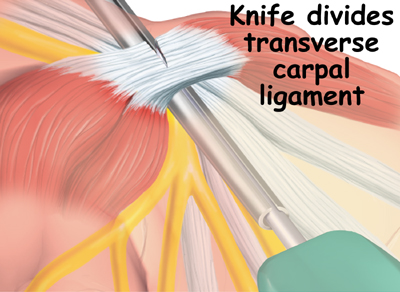
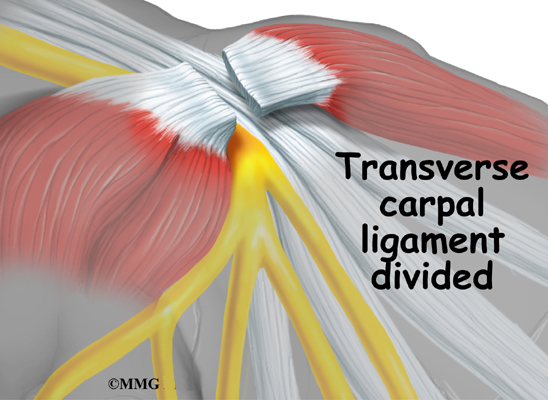
A special knife is inserted through the cannula. This knife has a hook on the end that cuts backwards when the knife is pulled back out of the cannula. Once the knife is pulled all the way back, the carpal ligament is divided, without cutting the palmar fascia or the skin of the palm.
Once the carpal ligament is divided, the median nerve is no longer compressed and begins to return to normal.
After the carpal ligament is released, the surgeon stitches just the skin openings and leaves the loose ends of the carpal ligament separated. The loose ends are left apart to keep pressure off the median nerve. Eventually, the gap between the two ends of the ligament fills in with scar tissue.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following endoscopic carpal tunnel release are
- anesthesia
- infection
- incision pain
- persistent symptoms
- incomplete ligament release
- hand weakness
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Infection is a possible complication after surgery, especially infection of the incision. Therefore, check your incision every day as instructed by your surgeon. If you think you have a fever take your temperature. If you have signs of infection or other complications, call your surgeon right away.
These are warning signs of infection or other complications:
- pain in your hand that is not relieved by your medicine
- discharge with an unpleasant odor coming from your incision
- swelling, heat, and redness along your incision
- chills or fever over 100.4 degrees Fahrenheit
- bright red blood coming from your incision
Incision Pain
Some patients report having pain along the palm incision, but this happens less than when people have an open release procedure. Sometimes people still feel some numbness and tingling after surgery, especially if they had severe pressure on the median nerve prior to surgery. When the thenar (thumb) muscles are notably shrunken (atrophied) from prolonged pressure on the median nerve, strength and sensation may not fully return even after having this type of surgery.
Persistent Symptoms
There is a small chance that problems of carpal tunnel syndrome don’t go away completely. Sometimes symptoms come back after having the endoscopic release surgery. A return of symptoms is rare, but the likelihood is greatest in workers who go back to a job where they hold on to vibrating tools for long hours.
Incomplete Ligament Release
Releasing the carpal ligament using an endoscope requires skill and experience. One drawback of this procedure is incomplete release of the carpal ligament. When this occurs, symptoms may not go away completely. Some patients end up needing a second surgery to completely release the carpal ligament.
Hand Weakness
Muscles that are used to squeeze and grip may seem weak after surgery. During normal gripping, the tendons of the wrist press outward against the carpal ligament. This allows the carpal ligament to work like a pulley to improve grip strength. People used to think that the tendons lose this mechanical advantage after the carpal ligament has been released. However, recent studies indicate that hand weakness is more likely from pain or swelling that occurs in the early weeks after the procedure. With the exception of patients who have severe atrophy at the time of surgery, most people achieve normal hand strength within two to four months of surgery. Those with severe atrophy commonly see improvements in hand strength, but they rarely regain normal size of the thenar muscles.
After Surgery
What happens immediately after surgery?
After surgery, the incision is wrapped in a soft dressing or simply covered with a bandage. Your surgeon may splint and wrap the wrist.
In the days following surgery, keep emergency phone numbers handy. Call your surgeon’s office if you feel your hand is not healing as it should.
Rehabilitation
What should I expect after surgery?
You’ll be scheduled to see your doctor in 10 to 12 days for a follow-up. Your surgeon may need to take out one or two of the stitches if they haven’t already been absorbed into your body.
Finger motions are safe to begin within one day after surgery. But you need to avoid heavy grasping or pinching with your hand for six weeks. These actions need to be avoided to keep the tendons from pushing out against the healing carpal ligament. After six weeks, you should be safe to resume gripping and pinching without irritating the wrist.
Your surgeon may have you work with a physical or occupational therapist for four to six weeks after the surgery. You’ll begin doing active hand movements and range-of-motion exercises. Therapists also use ice packs, soft-tissue massage, and hands-on stretching to help with the range of motion. When the stitches are removed, you may start carefully strengthening your hand by squeezing and stretching special putty with your hand and fingers. Therapists also use a series of fist positions to encourage the finger tendons to slide within the carpal tunnel.
As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints in the hand. Other exercises are used to improve fine motor control and dexterity. Some of the exercises you’ll do are designed to get your hand working in ways that are similar to your work tasks and sport activities.
Your therapist will help you find ways to do your tasks that don’t put too much stress on your hand and wrist. Before your therapy sessions end, your therapist will teach you a number of ways to avoid future problems.