A Patient’s Guide to Hallux Rigidus
Introduction
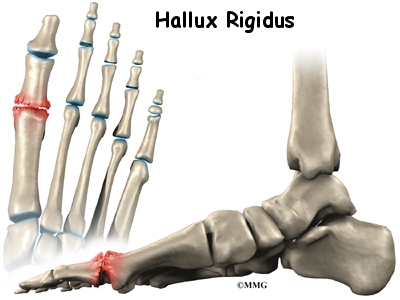
Hallux rigidus is a degenerative type of arthritis that affects the large joint at the base of the big toe. Degenerative arthritis results from wear and tear on the joint surface over time. The condition may follow an injury to the joint or, in some cases, may arise without a well-defined injury.
This guide will help you understand
- how hallux rigidus develops
- how the condition is diagnosed
- what can be done for the problem
Anatomy
Where does hallux rigidus occur?
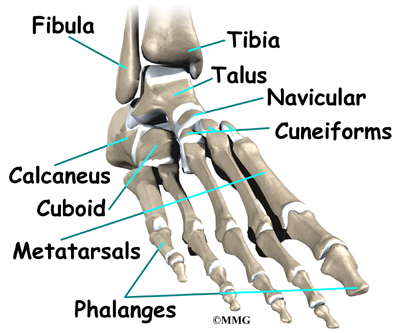
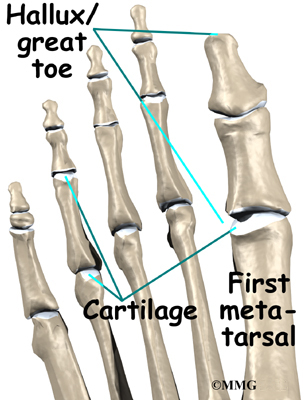
The joint at the base of the big toe is called the metatarsophalangeal, or MTP, joint. Like any other joint in the body, the joint is covered with articular cartilage, a slick, shiny covering on the end of the bone. If this material is injured, it begins a slow process of wearing out, or degeneration. The articular surface can wear away until raw bone rubs against raw bone.
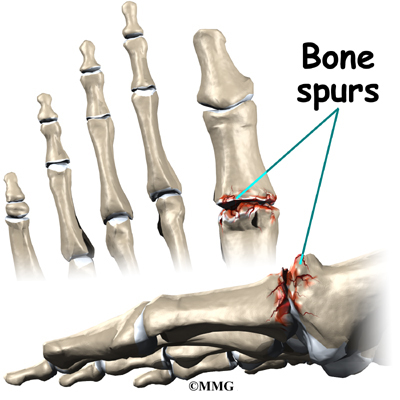
Bone spurs form around the joint as part of the degenerative process. The spurs, or bony outgrowths, may restrict the motion in the joint, especially the ability of the toe to bend upward when the foot moves forward.
Related Document: A Patient’s Guide to Foot Anatomy
Causes
Why do I have this problem?
Doctors remain uncertain about the true cause of hallux rigidus. Many surgeons feel that, in many cases, the condition begins with an injury to the articular cartilage lining the joint, such as from stubbing the big toe. The injury sets in motion a degenerative process that may last for years before symptoms occur that need treatment.
The condition can occur in younger adults but most often affects those who are 50 years old or older. Women seem to develop this problem more often than men. There may be a hereditary factor since two-thirds of patients have a positive family history. Patients who have other family members with hallux rigidus tend to have the problem in both feet (bilateral).
Other cases of hallux rigidus seem to arise without any type of serious injury. This suggests that there may be other reasons for the development of the condition. Minor differences in the anatomy of the foot may make it more likely that certain individuals develop hallux rigidus. This could be a slight change in the shape of the end of the bone (e.g., flatter than normal or oddly-shaped). The fascia (connective tissue) under the foot may be contracted (tight) increasing pressure on the MTP joint. These minor abnormalities may increase the stress that is placed on the joint while walking. Over many years, this may add up to degenerative arthritis of the joint.
Symptoms
What does hallux rigidus feel like?
The degeneration causes two problems–pain and loss of motion in the MTP joint. Without the ability of the MTP to move enough to allow the foot to roll through a full step, walking can become painful and difficult. Pain is most noticeable just before toe-off. Pain is increased when wearing shoes that have elevated heels. Bone spurs that develop with this condition can also put pressure on nearby nerves, causing numbness along the inside edge of the big toe.
Diagnosis
How do doctors identify the problem?
Diagnosis is usually apparent on physical examination, but X-rays are usually required to appreciate the extent of the degeneration and bone spur formation. X-rays also show the shape of the metatarsal head, amount of joint space, and presence of cartilage loss. This information can help direct treatment. MRIs or CT scans are only needed when the X-rays come back normal but some type of lesion is suspected.
Treatment
What can be done for the condition?
Nonsurgical Treatment
Treatment begins with anti-inflammatory medications to control the pain, swelling, heat, and redness of the degenerative arthritis. Special shoes that reduce the amount of bend in the toe during walking will also help the symptoms initially. A rocker type of sole allows the shoe to take some of the bending force, and may be combined with a metal brace in the sole to limit the flexibility of the sole of the shoe and reduce the motion needed in the MTP joint.
An injection of cortisone into the joint may give temporary relief of symptoms. Your doctor may suggest an injection in conjunction with trying special shoes to control your pain while walking. As with any injection into a joint, a small risk of infection exists with this procedure.
Surgery
Surgery may be suggested if all else fails. Several types of procedures are useful in treating this condition.
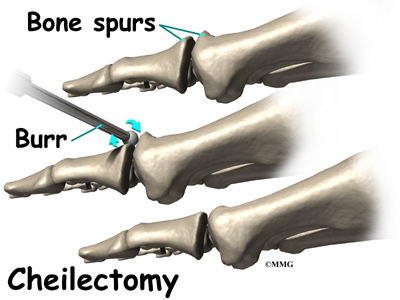
Cheilectomy
In some cases, bone spurs that form on the top of the joint can bump together when the big toe bends upward, or extends. This causes a problem when walking, because the big toe needs to bend upward when the foot is behind the body, getting ready to make the next step. The constant irritation when the bone spurs bump together leads to pain and difficulty walking.
A cheilectomy is a procedure to remove the bone spurs at the top of the joint so that they don’t bump together when the toe extends. This allows the toe to bend better and reduces the amount of pain while walking. To perform a cheilectomy, an incision is made along the top of the joint. The bone spurs that are blocking the joint from extending are identified and removed from both the bones that make up the joint. A little extra bone may be taken off to ensure that nothing rubs when the hallux is raised. The skin is closed and allowed to heal.
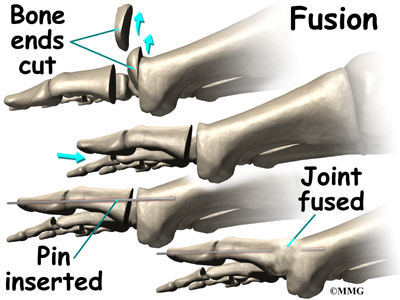
Joint Fusion
Many surgeons favor arthrodesis, or fusion, of the MTP joint to relieve the pain. To fuse a joint means to allow the two bones that form a joint to grow together and become one bone. The joint between the two bones is removed and the two bones are allowed to fuse. This results in a joint that no longer moves. Wearing a rocker-soled shoe is usually necessary following a fusion to improve your manner of walking, or gait.
View animation of joint surfaces removed
View animation of pin fixation
To perform a fusion, an incision is made into the MTP joint. The joint surfaces are removed. The two surfaces are then fixed with either a metal pin or screw, with the toe turned slightly upward to allow for walking. The bones are then allowed to fuse. The fusion usually takes about three months to become solid.
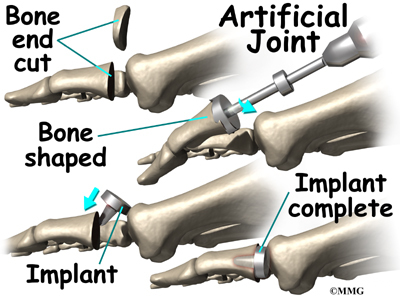
Artificial Joint Replacement
Some surgeons favor replacing the joint with an artificial joint, similar to what is done in the knee or hip, only much smaller. Replacing the joint with an artificial joint is usually recommended for moderately involved joints. (But, many surgeons think that arthrodesis or fusion still produces better results for patients with severe hallux rigidus).
In this procedure, one of the joint surfaces is removed and replaced with a plastic or metal surface. This procedure may relieve the pain and preserve the joint motion. The major drawback to this procedure is that the artificial joint probably will not last a lifetime and will require more operations later if it begins to fail.
View animation of proximal phalanx joint surface removed
View animation of proximal phalanx reamed
To perform an artificial joint replacement, an incision is first made on the top of the big toe over the MTP joint. Once the joint is entered, the arthritic joint surface of the proximal phalanx (the first bone of the big toe) is removed. The hollow marrow area of the proximal phalanx is prepared with special instruments so that the artificial joint surface will fit snugly into the bone. Different sized implants are tried, and the toe is moved through a range of motion to help determine if the fit is proper.
Once the surgeon is satisfied that everything fits, the artificial joint surface is implanted. The joint capsule and skin incision are then closed with small stitches.
There are actually several different ways to accomplish a joint replacement for hallux rigidus. A total joint replacement removes and replaces both sides of the joint. This type of procedure requires a conical stem that sits down inside the toe bones on either side of the joint. The implants can be made of ceramic, titanium, cobalt-chrome, or titanium combined with polyethylene (plastic) parts.
Metatarsal hemiarthroplasty replaces just one side of the joint — between the bone closest to the big toe joint (metatarsal) and the middle phalangeal bone. Limited studies have been done using this approach but patient satisfaction is reportedly high (100 per cent) with no implant failures or need for revision surgery.
Other Procedures
There are other surgical procedures that are slight variations of these three approaches. For example, cheilectomy may be combined with a phalangeal osteotomy. The surgeon removes a wedge-shaped piece of bone from the middle toe bone in order to take pressure off the joint. Some patients can be successfully treated with just the osteotomy procedure.
Another alternative approach (more for the younger patient) is the interpositional arthroplasty. In this procedure, the surgeon removes the base of the toe bone (phalange) and places a “spacer” in the hole left. The spacer is made up of a rolled up piece of tendon. The surgeon may have to release the tendon that inserts into the base of the phalange for this to work best. This decision is made at the time of the surgery.
Rehabilitation
What should I expect following treatment?
Nonsurgical Rehabilitation
If your doctor recommends nonsurgical treatment, you should begin to see some improvement in your symptoms within a few days. Anti-inflammatory medications may take up to seven to 10 days to become effective. A cortisone shot usually works within 24 hours. Alterations to your shoe wear may take several weeks to have an effect.
After Surgery
It will take about eight weeks before the bones and soft tissues are well healed. You may be placed in a wooden-soled shoe or a cast during this period to protect the bones while they heal. You will probably need crutches briefly. A physical therapist may be consulted to help you learn to use your crutches.
The incision is protected with a bandage or dressing for about one week after surgery. The stitches are generally removed in 10 to 14 days. However, if your surgeon used sutures that dissolve, you won’t need to have the stitches taken out.
During your follow-up visits, X-rays will probably be taken so that the surgeon can follow the healing of the bones if a fusion was performed. X-rays are also important if an artificial joint was used to make sure the implant is properly aligned and positioned.