Pain Management: A Patient’s Guide to Epidural Steroid Injections
Introduction
Epidural steroid injections (ESI) are commonly used to control back and leg pain from many different causes. These injections control pain by reducing inflammation and swelling. They do not cure any of the diseases they are commonly used for, but can control the symptoms for prolonged periods of time. In some cases, the ESI may be used to control the symptoms so that you can participate in a physical therapy program, become more active, and be better able to control the symptoms with a conservative program.
This guide will help you understand
- where the injection is given
- what your doctor hopes to achieve
- what you need to do to prepare
- what might go wrong
Anatomy
What parts of the body are involved?
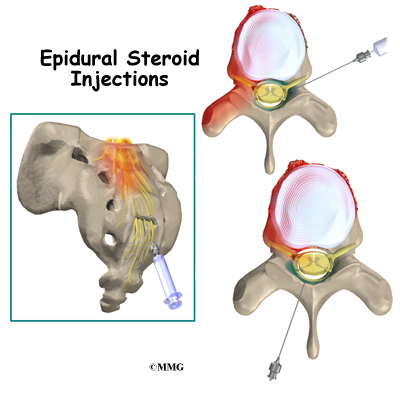
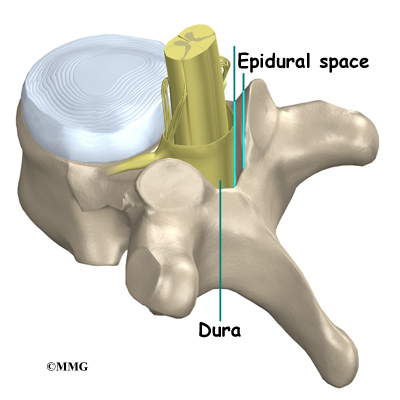
When doing an ESI, the doctor inserts a needle through the skin so that the tip of the needle is in the epidural space. This space is the area between the bony ring of the spine and the covering of the spine called the dura. The dura is the sac that encloses the spinal fluid and nerves of the spine. In the cervical spine and thoracic spine, the spinal cord also is contained within the dura and the spinal sac. The spinal cord actually stops at the second lumbar vertebra, so in the lower lumbar spine there are only spinal nerves running within the spinal sac.
The epidural space is normally filled with fat and blood vessels. Fluid such as the lidocaine and cortisone that is injected during an ESI is free to flow up and down the spine and inside the epidural space to coat the nerves that run inside the spinal canal.
There are several openings in the bones that surround the epidural space where a needle can be placed. An ESI can be performed by placing the needle in one of three of these openings. Each of these three types of ESI injections has advantages.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
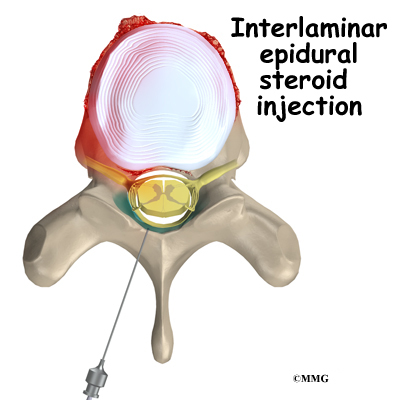
An interlaminar injection is performed by placing the needle directly in from the back of the spine between the lamina of two adjacent vertebra. The laminae (plural) form the outer rim of the bony ring of the vertebra. This places the tip of the needle in the back side of the spine. The advantage to this type of injection is that it is easy to do, even without the guidance of a fluoroscopic x-ray machine. The injection is usually done between the two vertebra that are most likely causing your pain. This puts the medications as close as possible to the problem. The disadvantage to this type of injection is that injected medication may stay in the back side of the spine away from the intervertebral disc.
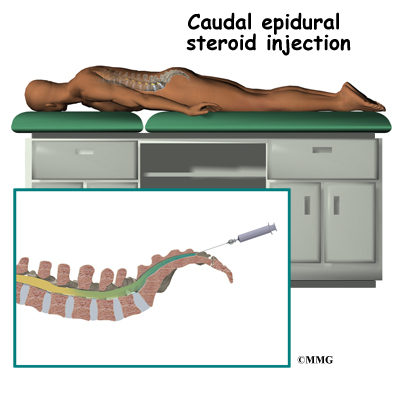
A caudal injection is also relatively easy to perform even without x-ray guidance. The caudal injection is performed at the very lower end of the spine through a small opening in the bones of the sacrum. The sacrum is made up of several vertebrae that fuse together during development to form a single large bone. This bone is where the pelvis connects to the spine.
The opening at the tip of the sacrum leads directly to the epidural space. Fluid injected through this opening can flow upward through the epidural space to coat the nerves throughout the lower lumbar spine.
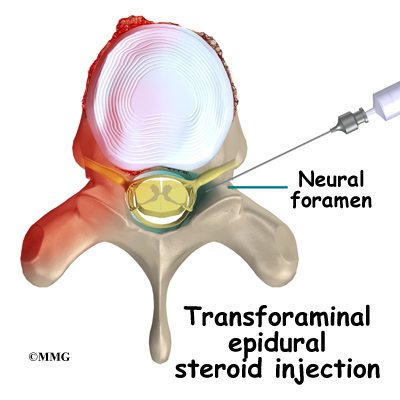
A transforaminal injection is a newer type of injection that is done from the side of the spine, through the neural foramen. The neural foramen is the opening where the nerve root exits the spine. There are two neural foramen between each vertebrae, one on each side.
The doctor places the tip of the needle into the neural foramen using the fluoroscopic x-ray machine to watch and guide the needle into the correct position. The advantage to this type of injection is that it places the medication in the front of the spinal canal, near the intervertebral disc. The disadvantage is that this type of injection requires using the fluoroscopic x-ray to guide the needle placement.
Rationale
What does my physician hope to achieve?
Your doctor is recommending an ESI to try and reduce your pain. The ESI may also reduce numbness and weakness. During an ESI the medications that are normally injected include an anesthetic and cortisone. An anesthetic medication (such as novacaine, lidocaine or bupivicaine) is the same medication that is used numb an area when you are having dental work or having a laceration sutured. The medication causes temporary numbness lasting 1 hour to 6 hours, depending on which type of anesthetic is used.
Cortisone is an extremely powerful anti-inflammatory medication. When this medication is injected around inflamed swollen nerves and connective tissues, it can reduce the inflammation and swelling. Reducing the inflammation reduces pain. Reducing swelling can allow the nerves to function better – reducing numbness and weakness.
These injections are temporary and may last from a couple of weeks to a couple of months. They may be used to reduce your symptoms so that you can more easily begin a physical therapy program with less pain. They may also be used to reduce symptoms and let the body repair the underlying condition. For example, most disc herniations cause a great deal of pain when they first happen. This is due to the chemicals that leak from the torn disc and inflame the nerves. Over several weeks to months, the disc heals enough to stop leaking these chemicals. If the cortisone can reduce the symptoms at the beginning, then when the cortisone injection wears off, the chemical irritation may be gone and the pain may not return. The cortisone itself does not heal the disc herniation.
In other conditions, the cortisone injection is repeated 1 to 3 times per year to help control the symptoms. This is usually recommended when surgery is too risky or you choose not to have surgery. For example, in older adults with spinal stenosis, this may be the less risky treatment. Spinal stenosis occurs when the spinal canal where the nerves travel is too tight. This results in inflammation and swelling of the nerves and soft tissues. The swelling makes the spinal canal even tighter. The nerves do not have enough room to function correctly and begin to cause pain, numbness and weakness. An ESI once every six months may reduce the swelling enough to reduce the pressure on the nerves and the symptoms of pain, numbness and weakness.
Preparations
How will I prepare for the procedure?
Your doctor may tell you to be “NPO” for a certain amount of time before the procedure. This means that you should not eat or drink anything for the amount of time before your procedure. This means no water, no coffee, no tea – not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You should tell your doctor if you are taking any medications that “thin” your blood or interfere with blood clotting. The most common blood thinner is coumadin. Other medications also slow down blood clotting. Aspirin, ibuprofen and nearly all of the anti-inflammatory medications affect blood clotting. So do medications used to prevent strokes such as Plavix. These medications usually need to be stopped 7 days prior to the injection. Be sure to let your doctor know if you are on any of these medications.
Procedure
What happens during the procedure?
When you are ready to have the ESI, you will be taken into the procedure area and an IV will be started. The IV allows the nurse or doctor to give you any medications that may be needed during the procedure. The IV is for your safety because it allows very rapid response if you have a problem during the procedure, such as an allergic reaction to any of the medications injected. If you are in pain or anxious, you may also be given medications through the IV for sedation during the procedure.
Most ESI procedures today are done with the help of fluoroscopic guidance. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure. This allows the doctor to watch where the needle goes as it is inserted. This makes the injection much safer and much more accurate. Once the needle is in the right location, a small amount of radiographic dye is injected. This liquid dye shows up on the xray image and the doctor can watch where it goes. The anesthetic medication and the cortisone will go in the same place, so the doctor wants to make sure that the injection will put the medication in the right place to do the most good. Once the correct position is confirmed, the anesthetic and cortisone are injected and the needle is removed.
You will then be taken out of the procedure room to the recovery area. You will remain in the recovery area until the nurse is sure that you are stable and do not have any allergic reaction to the medications. The anesthetic may cause some temporary numbness and weakness. You will be free to go when these symptoms have resolved.
Complications
What might go wrong?
There are several complications that may occur during or after the procedure. The ESI procedure is safe and unlikely to result in a complication, but no procedure is 100% foolproof. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Complications are uncommon, but you should know what to watch for if they occur. Like most procedures where medications are injected, there is always a risk of allergic reaction.
Probably the most common complication of an ESI is a wet tap. This occurs when the needle penetrates the spinal sac and enters the spinal fluid. This is the same thing that happens when your doctor performs a spinal tap or a spinal anesthetic. In itself, it is not dangerous. Because the epidural needle is larger than the spinal needle, the hole in the spinal sack may continue to leak and not seal itself off immediately. This causes a spinal fluid leak – or wet tap. This causes a very bad headache. The headache is worse when you are sitting or standing upright. It may cause nausea and vomiting. It will go away if you lie flat or with your head a bit lower than your feet. The headache occurs because the spinal fluid pressure in the skull decreases. That is why the headache goes away when you lie down – the spinal fluid pressure goes back to normal in your skull. Most spinal headaches go away in a few days when the hole in the spinal sac heals and closes. You may be instructed to stay flat for a couple of days until this occurs.
There are ways to speed up the healing of the puncture in the spinal sac. The most common treatment for a spinal headache that does not go away on its own is a blood patch. If the doctor sees that the spinal sac has been punctured before he removes the needle, this may be done at the time of the ESI. If not it may be done several days later if the headache has not gone away. This procedure involves taking a small amount of blood from a vein in your arm and injecting it into your back in the epidural space. The blood clots and “patches” the hole.
There are several other very rare possible complications of the ESI. These include epidural hematoma, epidural abscess and nerve damage. The epidural hematoma occurs when one of the small blood vessels around the spinal sac continues to bleed after the procedure. The bleeding can cause a large pocket of blood to form around the nerves putting too much pressure on the nerves. The epidural abscess is when an infection occurs inside the spinal canal. The infection can cause a large pocket of pus to form around the nerves and puts too much pressure on the nerves. Both of these complications will probably require surgery to correct or improve.
Finally, because the the injection is done inside the spinal canal, the spinal nerves can be damaged by the needle itself. This usually will recover and will not require any additional procedures to correct.
After Care
What happens after the procedure?
You will be able to go home soon after the procedure, probably within one hour. If all went as planned, you probably won’t have any restrictions on activity or diet.
Most doctors will arrange a followup appointment, or phone consult, within one or two weeks after the ESI to see how you are doing and what effect the procedure had on your symptoms.
You can return to physical therapy immediately.
One question that always comes up is “How many ESIs can I have?” There is no definite answer to that question. Most doctors would recommend that you limit the number of injections to 3-5 per year. The limit is not the injection but the amount of cortisone put in your body. Cortisone has bad side effects when you take the medication often – either as a pill or as an injection. The side effects are why doctors do not like to do these injections more often than necessary.