A Patient’s Guide to Developmental Dysplasia of the Hip in Children
Introduction
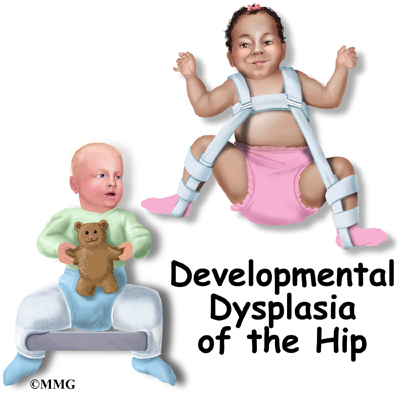
Developmental dysplasia of the hip (DDH), previously known as congenital hip dysplasia is a common disorder affecting infants and young children. The change in name reflects the fact that DDH is a developmental process that occurs over time. It develops either in utero (in the uterus) or during the first year of life. It may or may not be present at birth.
In this condition there is a disruption in the normal relationship between the head of the femur and the acetabulum (hip socket). DDH can affect one or both hips. It can be mild to severe. In mild cases called unstable hip dysplasia the hip is in the joint but easily dislocated. More involved cases are partially dislocated or completely dislocated. A partial dislocation is called subluxation.
This guide will help you understand
- what part of the hip is involved
- what causes the condition
- what treatment options are available
Anatomy
What part of the hip is affected?
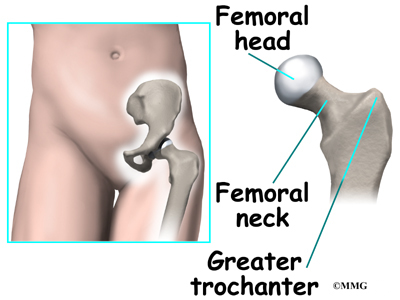
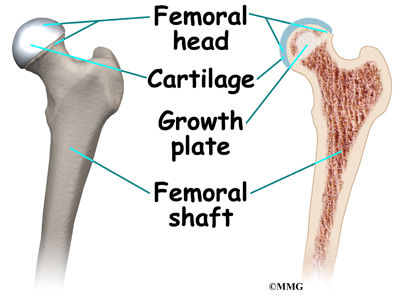
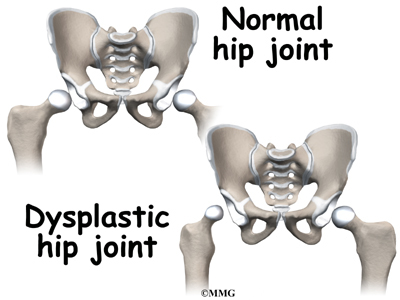
The hip joint is where the femur (thighbone) connects to the pelvis. The joint is made up of two parts. The upper end of the femur is shaped like a ball. It is called the femoral head. The femoral head fits into a socket in the pelvis called the acetabulum. This ball and socket joint is what allows us to move our leg in many directions in relation to the body.
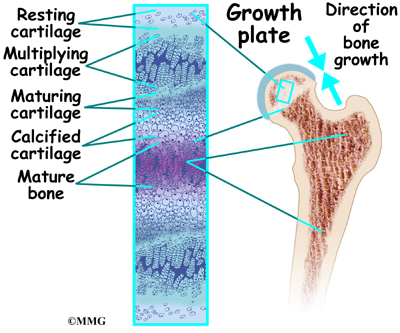
The right amount of pressure and contact between the surfaces of these two parts helps make sure the hip joint develops normally. Most of the acetabulum is cartilage at birth. The head of the femur inside the acetabulum helps shape the joint as it continues to form. In DDH the usual contact between the femoral head and the acetabulum is disrupted.
An abnormal position of the femoral head can result in a dysplastic hip. Sometimes the acetabulum is too shallow or sloping rather than a normal cup shape. It cannot hold the femoral head in place.
If the problem is not diagnosed and treated early, the soft tissues around the hip start to stretch out. There can be changes in the blood supply to the hip. Sometimes the hip joint tries to form another hip socket called a false acetabulum. Without the proper ligaments, soft tissues, and joint capsule to hold the femoral head in place, the false acetabulum creates even more problems.
Causes
How does this problem develop?
There isn’t one single known cause of DDH. In some cases there is laxity or looseness of the ligaments around the joint. This may be hereditary. In other cases the infant’s position may affect how the hip joint forms, either during growth inside the mother or after birth.
For example, a breech position (buttocks first position) in utero limits movement. It also puts the hips in a position with the hips bent, knees straight, and legs together. This position puts abnormal stresses on the joint that do not foster normal development.
Hip position and free hip movement remain important during the first months after birth. This is when the hip continues to develop and forms a deep socket and stable joint. An infant carried on a parent’s hip with the child’s hips bent and open wide is less likely to develop DDH. Infants in some cultures are swaddled or wrapped with the legs together and extended out straight. For example, in some Native American cultures infants are carried on a papoose board. The infant is wrapped on the papoose board with the legs straight down and bound together. An infant that spends a good deal of time in this position is at greater risk for DDH. DDH is more common in Chinese, Korean, and African American infants.
DDH is much more common in girls than boys. This may be linked with hormonal differences. Estrogens and a hormone called relaxin present during development in utero and still present at the time of birth may cause generalized laxity or looseness of the ligaments. The left hip is affected more than the right hip. Again, this is probably linked with position before birth. The most common position in utero places the child’s left hip next to the mother’s spine and limits hip motion.
Children with developmental disabilities who do not move normally or who can’t stand up and walk are also at risk for DDH.
Symptoms
What does this problem feel like?
The newborn, infant, or young child may not have any symptoms such as pain to signal a problem. There may be some differences in how the legs and buttocks look from side to side. Sometimes the problem isn’t noticed until the child starts to walk. If only one hip is affected, the child may walk with a limp. If DDH is present in both hips, the child may sway from side to side or waddle. When both hips are dislocated, it is sometimes very difficult to see an abnormality in the way the child walks.
Diagnosis
<How do doctors identify the problem?
Early diagnosis in the newborn and young infant is important to avoid major problems later. The physical examination performed by the pediatrician is the most important diagnostic tool. All newborns and infants should be screened as early as possible. Babies born breech or with a family history of DDH are of special concern.
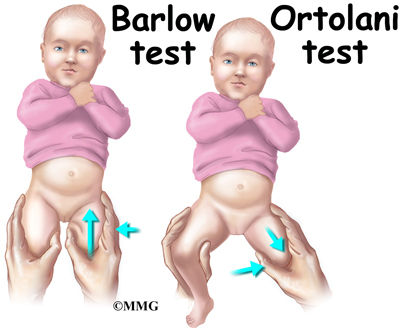
Special tests are performed by the doctor while the infant is still in the nursery, The doctor is trying to look for signs of an unstable hip. The two most reliable physical exam tests are Ortolani’s maneuver and Barlow’s test. These tests are designed to detect if the hip is sliding in and out of the acetabulum. To perform these tests, the doctor places the infant on a table in a supine position (on his or her back). The doctor then abducts the hips by moving the bent hips and knees apart. If the hip feels like it can be pushed out the back of the socket, this is considered abnormal. This is called a positive Barlow’s Test and is a sign of instability in the hip. As the hip is abducted further, the doctor might feel the ball portion (the femoral head) slide forward as it slips back into the socket. This is called a positive Ortolani Maneuver and is also a sign of hip instability. If either one of these tests are positive, the child will be watched closely or immediate treatment with a brace may be considered.
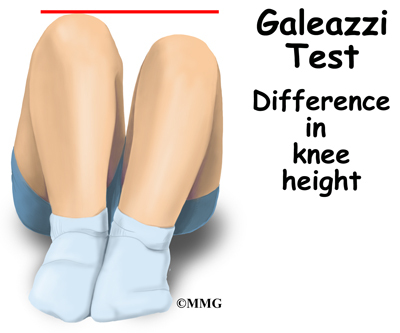
For the infant three months or older, Galeazzi’s or Allis’ test can be performed. The child is placed in the supine position with the hips and knees bent and the feet flat. The examiner looks for any unevenness between the knees. If one knee is lower than the other, there may be a dislocated hip on the lower side.
Since DDH can develop over time, repeated exams are advised. Well-baby check-ups should include repeated hip examination. This is done until the child begins to walk normally with no sign of a limp or altered gait (walking) pattern. The doctor also looks for changes in hip range of motion, uneven skin folds around the thighs and buttocks, and a difference in leg length from side to side.
X-rays aren’t reliable in infants but may be of some diagnostic value in the older child. Ultrasound is more accurate in the first six months of life.
Treatment
What treatment options are available?
The goal of treatment is to keep the femoral head in good contact with the acetabulum. A stable hip encourages the development of a normally shaped socket and rounded head of the femur. The proper hip position must be maintained for enough time to stabilize the joint. The hip should be flexed to 95 degrees and abducted (apart) at least 90 degrees. This position keeps the ball (the femoral head) in the best position and allows the ligaments and joint capsule to tighten up.
Nonsurgical Treatment
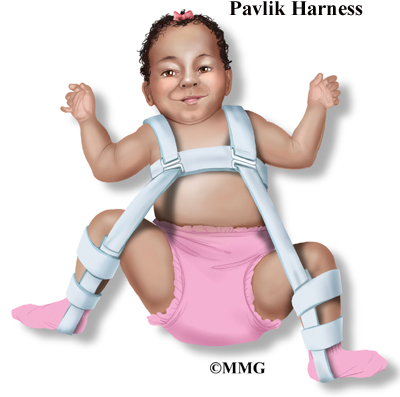
There are several ways to treat DDH depending on the child’s age and the severity of the condition. Double and triple diapering may be all that is needed in the first six weeks. If the problem persists, a special harness called the Pavlik harness can be used for three to nine months. The harness keeps the hip in flexion and abduction. It may be worn until the doctor can no longer move the hip in and out of the socket. In the older child, x-rays may be used to confirm that the hip is stable.
For children with developmental disabilities, a standing program may be required. Special standing boxes or equipment to hold them upright are used to give the hip the mechanical force it needs to develop normally.
Surgery
In the infant older than 6 months, the Pavlik harness may not work. The child may be too large to wear the harness or may be too active to keep the harness on all day. In this age group, a closed reduction under general anesthesia may be the best option. If the hip cannot be easily reduced, the child may be placed in traction to loosen the soft tissues around the hip. When the surgeon thinks it may be time to reduce the hip, the child is taken to the operating room and placed under general anesthesia. There the surgeon gently moves the hip and feels to see if the hip can be placed in the socket. Fluoroscopy is used to watch the bones of the pelvis and hip as they line up. Fluoroscopy is a type of x-ray where the surgeon can watch the x-ray picture on a TV screen.
Once the hip can be put back in the socket easily, the child is put in a hip spica cast from waist to toe. This cast holds both legs so that the hip joint remains in one position – in the socket while the soft tissues around the hip tighten to hold the hip reduced. The cast may be needed for several months to hold the hip in place. The cast usually is replaced every two weeks to one month while it is needed. Each time the cast is changed, the child is taken to the operating room and placed under general anesthesia. This treatment is called a closed reduction.
Surgery may be needed when the hip cannot be stabilized and kept in the socket. Surgery is more likely required in the child older than 18 months. Before the surgery, the child may be placed in traction to loosen the soft tissues around the hip. Then the child is put in a full hip spica cast from waist to toe. The cast may be needed for several months to hold the hip in place. An open reduction is a surgical procedure used most often in children two years old or older when hip dysplasia has not been corrected. During this operation, the surgeon removes any abnormal tissues that are keeping the femoral head from fitting inside the acetabulum and cuts any tight ligaments in the joint capsule around the hip joint. The surgeon may perform a tenotomy during the surgery to cut the tightly contracted tendons or muscles in the hip area. This relaxes the tight structures around the hip joint and allows the hip to be placed in the socket. These tissues grow back with scar tissue as the child heals. The child is usually placed in a spica cast after this type of surgery and will need to wear this cast for several months.
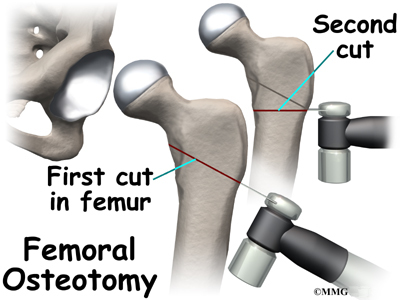
An operation called derotational osteotomy may be needed. In this surgical procedure, the femur is cut and rotated to make it easier to keep the femoral head inside the acetabulum. When this procedure is done, the soft tissues loosen up and the forces of the muscles tend to keep the femoral head reduced. Once again, the child is put in a spica cast for several months while the bone heals. A CT scan may be used to confirm successful reduction before removing the cast. A CT scan is a special type of x-ray that takes slices of the body. This allows a much better picture of the hip and acetabulum than plain x-rays.
In children older than 18 months, the problem may require additional surgery to change the acetabulum (socket) in addition to the femur (thighbone). The problem has been present longer and the anatomy has grown more distorted over the longer period of time. Your doctor may recommend surgery to change the way that the acetablum is aligned in this situation. There are many different types of pelvic osteotomies that have been designed and are still used.
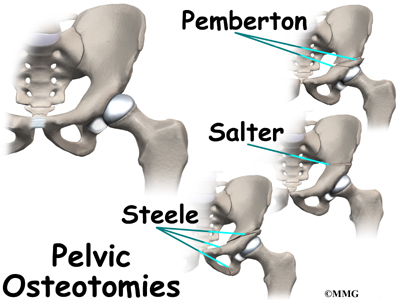
Several different types of osteotomies are used to tilt the acetabulum in a more horizontal angle to the floor. By doing this, the femoral head is less likely to slide up and out of the socket with weightbearing. These include the Steele, the Salter and the Pemberton osteotomies.
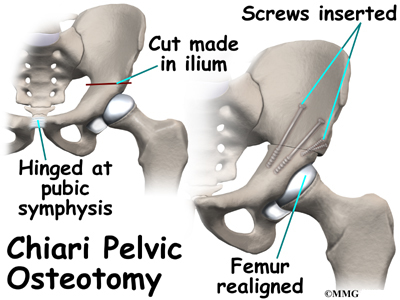
In the Chiari osteotomy, the bone of the pelvis just above the acetabulum is cut to allow the bone to slide out and form a new roof over the hip joint. This can stop the femoral head from sliding up and out of the socket. Over time this shelf of bone above the acetabulum remodels and forms a deeper acetabulum.
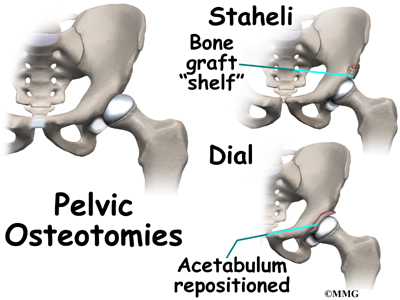
The Staheli osteotomy uses a bone graft placed just above the hip joint to create a new, wider roof, or shelf over the acetabulum. This keeps the femoral head from sliding up and out of the socket and, as it heals, makes a larger weightbearing surface to spread out the weight that needs to be transferred from the femoral head to the acetabulum and pelvis. The Dial osteotomy is not as common. In this procedure, the entire acetabulum is cut free of the pelvis and moved or dialed at the best angle and then allowed to heal in that position.
Young children have incredible powers of healing. Because the skeleton is still forming, many of the changes created at surgery will remodel dramatically and create a hip socket that will serve the child well into adulthood with minimal problems. All children that require surgery to address a dysplastic hip have a higher risk of developing wear and tear arthritis of the hip as they age into adulthood. Many will age well into their 40s and 50s before experiencing significant problems with the hip. Some may never have any additional problems.
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
The child in a Pavlik harness benefits from as much motion in the hip as possible – while still keeping the hip reduced. Motion allows for nutrition of the developing bone and cartilage inside the hip joint. The therapist will review positions to avoid such as sidelying with the top leg down toward the other leg past the midline. The harness must be used continuously until the hip is stable. Use may be gradually decreased to just nighttime wear before finally stopping.
For the infant in a harness, care must be taken not to set the harness in too much abduction. Abduction is the motion when the thighs are pulled away from one another. The Pavlik harness is designed to hold the legs bent at 95 degrees at the hip and abducted, or pulled apart, about 45 degrees each. The harness can be tightened too much, pulling the legs apart too much. Too much force into abduction can block the blood supply to the femoral head causing a condition called avascular necrosis. This is a serious complication that can prolong the treatment of the hip and may lead to other problems. Your surgeon or physical therapist should instruct you on how to correctly adjust the Pavlik harness. Make sure you understand how to do this properly. Ask questions if you do not feel you understand.
After Surgery
The child who has surgery will not be able to walk afterwards because of the spica cast. A special hole is cut open to allow the older child to go to the bathroom. Younger children remain in diapers. Your physical therapist will help the family with any special equipment needed for daily tasks and transportation. Special tips for positioning and handling will be reviewed as well.
Special care must be taken not to get the cast wet with water or urine. The cast may be removed and replaced only if the child grows and there are signs that the cast is too small or if there is evidence of skin breakdown. The child should be checked several times each day for changes in skin color or sensation. Leg or foot pain, cool or numb toes, or loss of motion in the feet must be reported to the physician right away.
Physical and occupational therapy is important during the postoperative period in the cast. Opportunities to move and develop gross motor skills are limited. The therapist will closely monitor overall gross and fine motor skills normally occurring during this time.