A Patient’s Guide to Carpal Tunnel Syndrome
Introduction
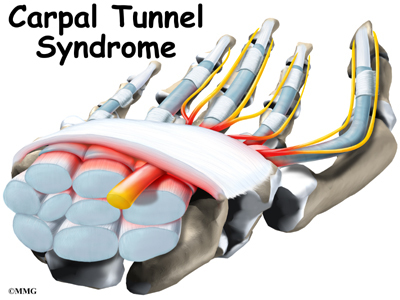
Carpal tunnel syndrome (CTS) is a common problem affecting the hand and wrist. Symptoms begin when the median nerve gets squeezed inside the carpal tunnel of the wrist, a medical condition known as nerve entrapment or compressive neuropathy. Any condition that decreases the size of the carpal tunnel or enlarges the tissues inside the tunnel can produce the symptoms of CTS.
This syndrome has received a lot of attention in recent years because of suggestions that it may be linked with occupations that require repeated use of the hands, such as typing on a computer keyboard or doing assembly work. Actually, many people develop this condition regardless of the type of work they do.
This guide will help you understand
- where the carpal tunnel is located
- how CTS develops
- what can be done for the condition
Anatomy
Where is the carpal tunnel, and what does it do?
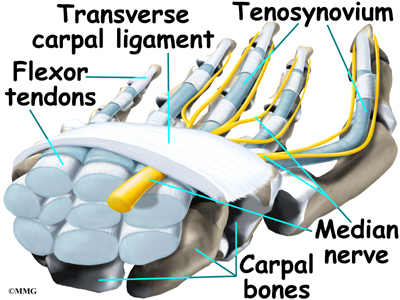
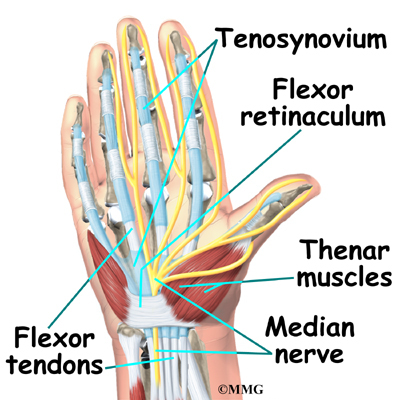
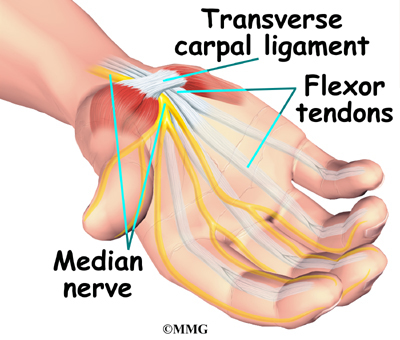
The carpal tunnel is an opening through the wrist to the hand that is formed by the bones of the wrist on one side and the transverse carpal ligament on the other. (Ligaments connect bones together.) This opening forms the carpal tunnel.
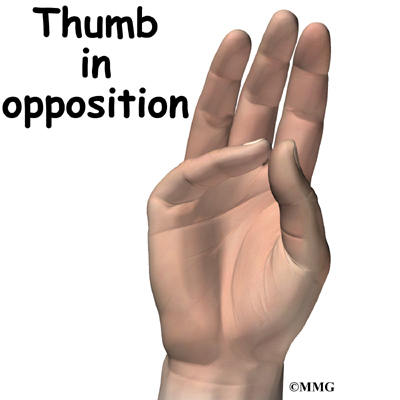
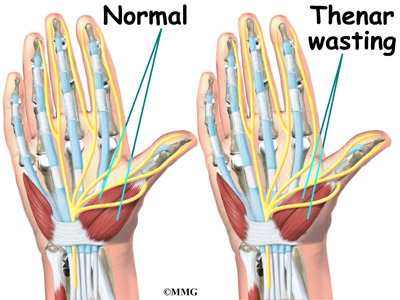
The median nerve passes through the carpal tunnel into the hand. It gives sensation to the thumb, index finger, long finger, and half of the ring finger. It also sends a nerve branch to control the thenar muscles of the thumb. The thenar muscles help move the thumb and let you touch the pad of the thumb to the tips of each finger on the same hand, a motion called opposition.
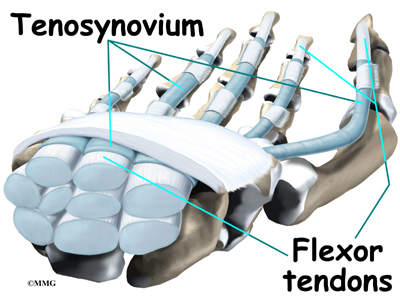
The median nerve and flexor tendons pass through the carpal tunnel. The median nerve rests on top of the tendons, just below the transverse carpal ligament. The flexor tendons are important because they allow movement of the fingers, thumb, and hand, such as when grasping. The tendons are covered by a material called tenosynovium. The tenosynovium is a slippery covering that allows the tendons to glide next to each other as they contract and relax to move the hand and fingers.
Related Document: A Patient’s Guide to Hand Anatomy
Causes
What causes CTS?
Any condition that makes the area inside the carpal tunnel smaller or increases the size of the tissues within the tunnel can lead to symptoms of CTS. The carpal tunnel cannot expand so any condition that causes abnormal pressure in the tunnel can produce symptoms of CTS. And any increase in pressure within the carpal tunnel can reduce blood flow to the nerve, leading to loss of nerve function.
Various types of arthritis can cause swelling and pressure in the carpal tunnel. The way people do their tasks can put them at risk for problems of CTS. Some of these risks include
- force
- posture
- wrist alignment
- repetition
- temperature
- vibration
One of these risks alone may not cause a problem. But doing a task that involves several factors may pose a greater risk. And the longer a person is exposed to one or more risks, the greater the possibility of having a problem with CTS. However, scientists believe that other factors such as smoking, obesity, and caffeine intake may actually be more important in determining whether a person is more likely to develop CTS.
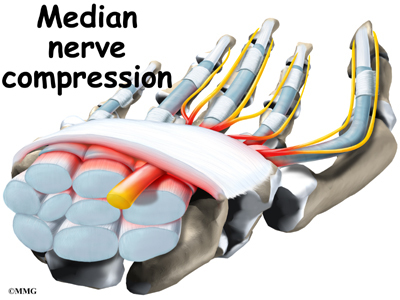
In other instances, CTS can start when the tenosynovium thickens from irritation or inflammation. This thickening causes pressure to build inside the carpal tunnel. But the tunnel can’t stretch any larger in response to the added swelling, so the median nerve starts to squeeze against the transverse carpal ligament. If the pressure continues to build up, the nerve is eventually unable to function normally.
When pressure builds on the median nerve, the blood supply to the outer covering of the nerve slows down and may even be cut off. The medical term for this is ischemia. At first, only the outside covering of the nerve is affected. But if the pressure keeps building up, the inside of the nerve will start to become thickened. New cells (called fibroblasts) form within the nerve and create scar tissue. This is thought to produce the feelings of pain and numbness in the hand. If pressure is taken off right away, the symptoms will go away quickly. Pressure that isn’t eased right away can slow or even stop the chances for recovery.
Trauma such as a wrist fracture, fracture/dislocation, infection, burns or other thermal injuries, bleeding disorders, and high-pressure injection injuries can result in a condition called i>acute carpal tunnel syndrome. This is much less common than the chronic compressive neuropathy caused by any of the risk factors described in this document.
A traumatic wrist injury may cause swelling and extra pressure within the carpal tunnel. The area inside the tunnel can also be reduced after a wrist fracture or dislocation if the bone pushes into the tunnel. Fractured wrist bones may later cause CTS if the healed fragments result in abnormal irritation on the flexor tendons.
Other conditions in the body can produce symptoms of CTS. Pregnancy can cause fluid to be retained, leading to extra pressure in the carpal tunnel. Diabetics may report symptoms of CTS, which may be from a problem in the nerve (called neuropathy) or from actual pressure on the median nerve. People with low thyroid function (called hypothyroidism) are more prone to problems of CTS. Tumors or cysts in the wrist, on the tendons, or in the carpal tunnel can also cause CTS.
Symptoms
What does CTS feel like?
One of the first symptoms of CTS is gradual tingling and numbness in the areas supplied by the median nerve. This is typically followed by dull, vague pain where the nerve gives sensation in the hand. The hand may begin to feel like it’s asleep, especially in the early morning hours after a night’s rest.
In the case of acute CTS, symptoms are sudden and severe, occurring over a matter of hours rather than weeks or months with the more chronic form of this condition.
Whether acute or chronic, pain associated with carpal tunnel syndrome may even spread up the arm to the shoulder. If the condition progresses, the thenar muscles of the thumb can weaken, causing the hand to be clumsy when picking up a glass or cup. If the pressure keeps building in the carpal tunnel, the thenar muscles may begin to atrophy (shrink).
Touching the pad of the thumb to the tips of the other fingers becomes difficult, making it hard to grasp items such as a steering wheel, newspaper, or telephone.
Diagnosis
How do doctors identify the condition?
Your doctor begins the evaluation by obtaining a history of the problem, followed by a thorough physical examination. Your description of the symptoms and the physical examination are the most important parts in the diagnosis of CTS. Commonly, patients will complain first of waking in the middle of the night with pain and a feeling that the whole hand is asleep.
Careful investigation usually shows that the little finger is unaffected. This can be a key piece of information to make the diagnosis. If you awaken with your hand asleep, pinch your little finger to see if it is numb also, and be sure to tell your doctor if it is or isn’t. Other complaints include numbness while using the hand for gripping activities, such as sweeping, hammering, or driving.
If your symptoms started after a traumatic wrist injury, X-rays may be needed to check for a fractured bone or a fracture with dislocation.
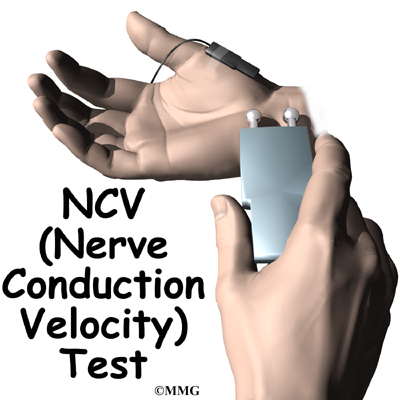
If more information is needed to make the diagnosis, electrical studies of the nerves in the wrist may be requested by your doctor. Several tests are available to see how well the median nerve is functioning, including the nerve conduction velocity (NCV) test. This test measures how fast nerve impulses move through the nerve.
Treatment
What can be done for CTS?
The American Academy of Orthopaedic Surgeons has published guidelines on the treatment of carpal tunnel syndrome. These guidelines reflect current research evidence and are included in this document. For the complete online version of the guidelines, see www.aaos.org/guidelines.
Nonsurgical Treatment
Activities that are causing your symptoms need to be changed or stopped if at all possible. Avoid repetitive hand motions, heavy grasping, holding onto vibrating tools, and positioning or working with your wrist bent down and out. If you smoke, talk to your doctor about ways to help you quit. Lose weight if you are overweight. Reduce your caffeine intake.
A wrist brace will sometimes decrease the symptoms in the early stages of CTS. A brace keeps the wrist in a resting position, not bent back or bent down too far. When the wrist is in this position, the carpal tunnel is as big as it can be, so the nerve has as much room as possible inside the carpal tunnel. A brace can be especially helpful for easing the numbness and pain felt at night because it can keep your hand from curling under as you sleep. The wrist brace can also be worn during the day to calm symptoms and rest the tissues in the carpal tunnel.
Anti-inflammatory medications may also help control the swelling and reduce symptoms of CTS. These include common over-the-counter medications such as ibuprofen and aspirin. Oral steroid medication may also offer some relief. In some studies, high doses of vitamin B-6 have been shown to help in decreasing CTS symptoms. Some types of exercises have also shown to help prevent or at least control the symptoms of CTS.
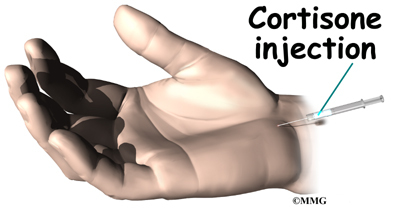
If these simple measures fail to control your symptoms, an injection of cortisone into the carpal tunnel may be suggested. This medication is used to reduce the swelling in the tunnel and may give temporary relief of symptoms.
A cortisone injection may help ease symptoms and can aid your doctor in making a diagnosis. If you don’t get even temporary relief from the injection, it could indicate that some other problem is causing your symptoms. When your symptoms do go away after the injection, it’s likely they are coming from a problem within the carpal tunnel. Some doctors feel this is a signal that a surgical release of the transverse carpal ligament would have a positive result.
Your doctor may suggest that you work with a physical or occupational therapist. The main focus of treatment is to reduce or eliminate the cause of pressure in the carpal tunnel. Your therapist may check your workstation and the way you do your work tasks. Suggestions may be given about the use of healthy body alignment and wrist positions, helpful exercises, and tips on how to prevent future problems. You might also receive treatments to reduce inflammation and to encourage normal gliding of the tendons and median nerve within the carpal tunnel.
Surgery
If all attempts to control your symptoms fail, surgery may be suggested to reduce the pressure on the median nerve. Surgery may not be advised if there is advanced nerve damage. Persistent pain and numbness may not go away with surgery. If you have muscle atrophy and weakness and/or loss of sensation, you may not be a good candidate for surgery.
And surgery may not be advised if electrodiagnostic studies show normal results. In such cases, patients seeking pain relief will be advised to continue with conservative (nonoperative) care.
In the case of acute CTS, surgery is required right away to decompress the nerve and save it from permanent damage. This is called nerve-sparing decompression. If a patient experiences a traumatic wrist or hand injury with worsening symptoms and increasing loss of hand function, carpal tunnel release is required.
When surgery is needed, several different surgical procedures have been designed to relieve pressure on the median nerve. By releasing the pressure on the nerve, the blood supply to the nerve improves, and most people get relief of their symptoms. However, if the nerve pressure has been going on a long time, the median nerve may have thickened and scarred to the point that recovery after surgery is much slower.
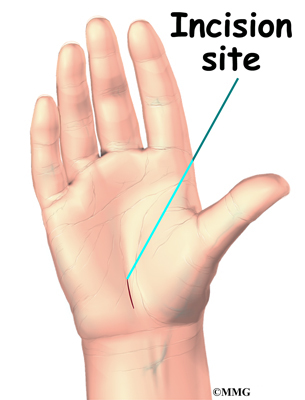
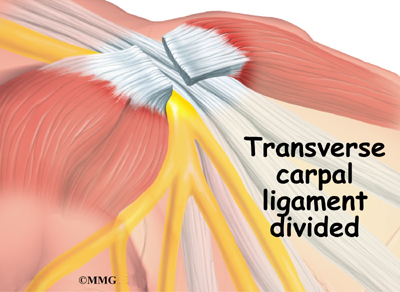
Open Release
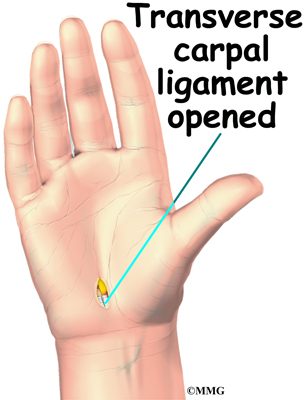
The standard surgery for CTS is called open release. Open surgical procedures use a small skin incision. In open release for CTS, an incision as small as one inch can be made down the front of the wrist and palm. By creating an open incision, the surgeon is able to see the wrist structures and to carefully do the operation. The surgeon cuts the transverse carpal ligament in order to take pressure off the median nerve.
After dividing the transverse carpal ligament, the surgeon stitches just the skin together and leaves the loose ends of the transverse carpal ligament separated. The loose ends are left apart to keep pressure off the median nerve. Eventually, the gap between the two ends of the ligament fills in with scar tissue.
Related Document: A Patient’s Guide to Open Carpal Tunnel Release
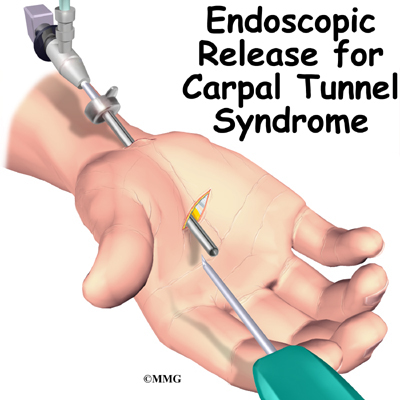
Endoscopic Release
Some surgeons are using a newer procedure called endoscopic carpal tunnel release. The surgeon merely nicks the skin in order to make one or two small openings for inserting the endoscope. An endoscope is a thin, fiber-optic TV camera that allows the surgeon to see inside the carpal tunnel as the transverse carpal ligament is carefully released.
Upon inserting the endoscope, the surgeon can see the wrist structures on a TV screen. A special knife is used to cut only the transverse carpal ligament. The palmar fascia and the skin over the wrist are not disturbed.
As in open release, the loose ends of the transverse carpal ligament are left apart after endoscopic release to keep pressure off the median nerve. The gap eventually fills in with scar tissue.
Related Document: A Patient’s Guide to Endoscopic Carpal Tunnel Release
Rehabilitation
What should I expect after treatment?
Nonsurgical Rehabilitation
If nonsurgical treatment is successful, you may see improvement in four to six weeks. You may need to continue wearing your wrist splint at night to control symptoms and keep your wrist from curling under as you sleep. Try to do your activities using healthy body and wrist alignment. Limit activities that require repeated motions, heavy grasping, and vibration in the hand.
After Surgery
It generally takes longer to recover after open carpal tunnel release. Pain and symptoms usually begin to improve, but you may have tenderness in the area of the incision for several months after surgery.
Patients who wait too long to seek medical advice sometimes have difficulty adjusting after surgery. Poor coping skills in the presence of persistent pain and numbness may result in disappointment or dissatisfaction with the results of surgery. Recovery may take longer than expected when nerve damage is severe. In some cases, symptoms are not entirely alleviated.
When the stitches are removed, your surgeon may have you work with a physical or occupational therapist for six to eight weeks. Treatments are used at first to ease pain and inflammation. Gentle massage to the incision can help reduce sensitivity in and around the incision and limit scar tissue from building up. Special exercises are used to encourage normal gliding of the tendons and median nerve within the carpal tunnel.
As you progress, your therapist will give you exercises to help strengthen and stabilize the muscles and joints in the hand, wrist, and arm. Other exercises are used to improve fine motor control and dexterity of the hand. Your therapist will work with you to help you do your daily and work activities safely and with the least amount of strain on your wrist and hand.