A Patient’s Guide to Anterior Lumbar Interbody Fusion
Introduction
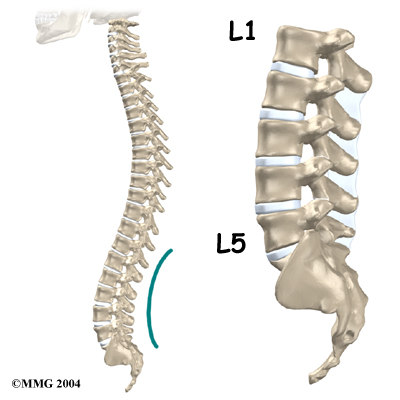
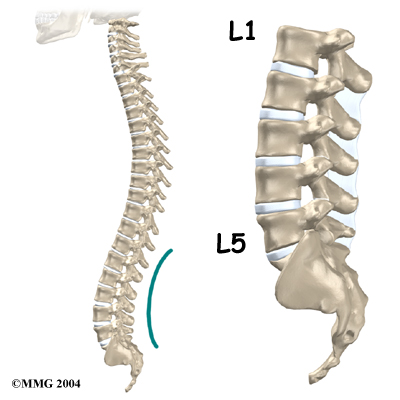
Anterior lumbar interbody fusion (ALIF) is a procedure used to treat problems such as disc degeneration, spine instability, and deformities in the curve of the spine. In this procedure, the surgeon works on the spine from the front (anterior) and removes a spinal disc in the lower (lumbar) spine. The surgeon inserts a bone graft into the space between the two vertebrae where the disc was removed (the interbody space). The goal of the procedure is to stimulate the vertebrae to grow together into one solid bone (known as fusion). Fusion creates a rigid and immovable column of bone in the problem section of the spine. This type of procedure is used to try and reduce back pain and other symptoms.
This guide will help you understand
- what surgeons hope to achieve
- what happens during surgery
- what to expect as you recover
Anatomy
What parts of the spine and low back are involved?
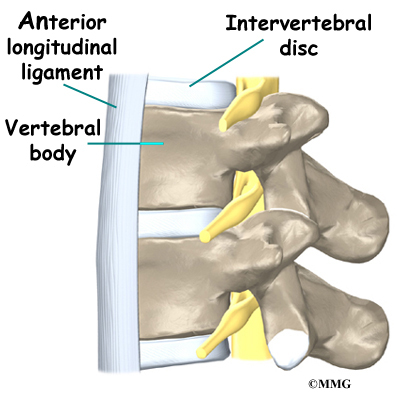
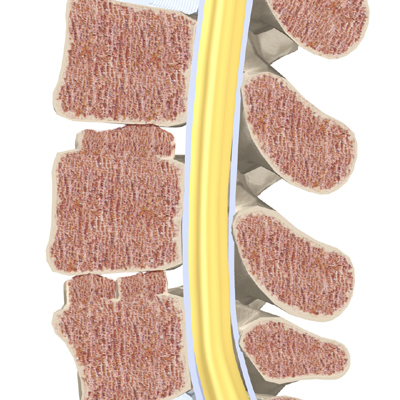
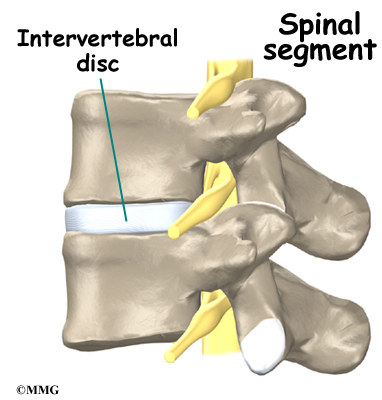
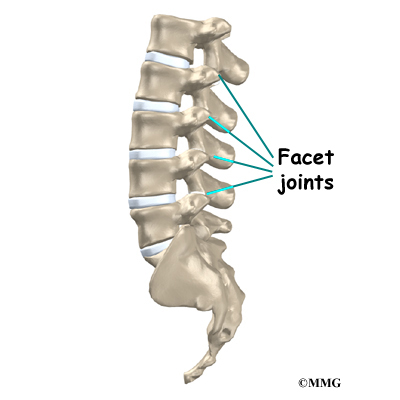
ALIF surgery is performed through the front (anterior). The structures in this area include the anterior longitudinal ligament, the vertebral bodies, and the intervertebral discs. The anterior longitudinal ligament attaches along the front of the spinal column. The vertebral bodies are the large blocks of bone that make up the front section of each vertebra.
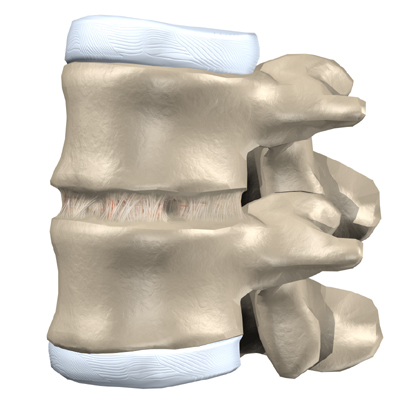
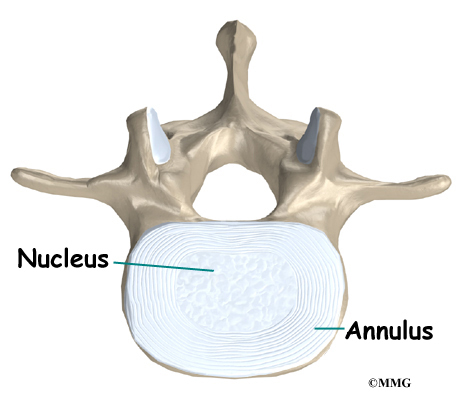
The intervertebral discs are the cushions between each pair of vertebrae.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
Rationale
What do surgeons hope to achieve?
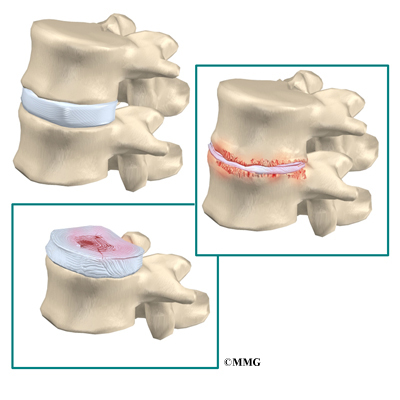
This procedure is often used to stop symptoms from lumbar disc disease. Discs degenerate, or wear out, as a natural part of aging and also from stress and strain on the back. Over time, the disc begins to collapse, and the space decreases between the vertebrae.
Related Document: A Patient’s Guide to Lumbar Dengenerative Disc Disease
When this happens, the openings around the spinal nerves (the neural foramina) narrow and may put pressure on the nerves. The long ligaments in the spine slacken due to the collapse in vertebral height. These ligaments may buckle and put pressure on the spinal nerves.
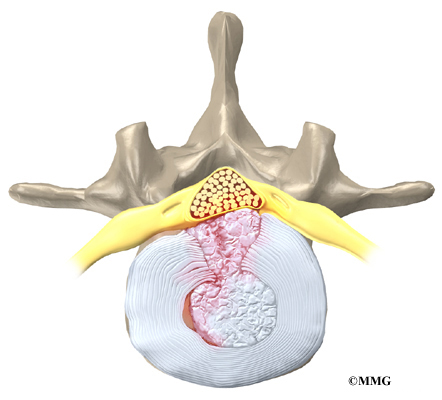
View animation of degeneration
Also, the outer rings of the disc, the annulus, weaken and develop small cracks. Tears in the outer annulus are painful because these tissues are rich with pain sensors. The nucleus in the center of the disc may press on the weakened annulus and actually squeeze out of the annulus (herniate). Inflammation from the nucleus as it escapes the annulus also causes pain. The nucleus normally does not come in contact with the body’s blood supply. However, a tear in the annulus puts the nucleus at risk for contacting this blood supply. When the nucleus herniates into the torn annulus, the nucleus and blood supply meet, causing a reaction of the chemicals inside the nucleus. This produces inflammation and pain.
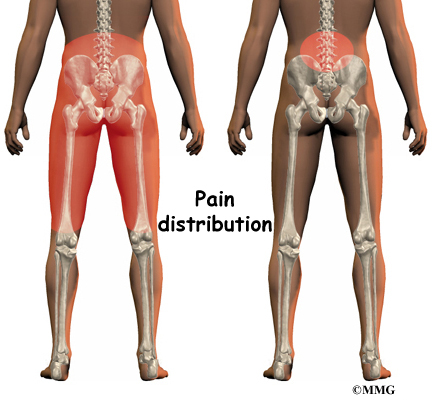
If the nucleus presses against the spinal nerves, symptoms of pain, numbness, and weakness may occur where the nerve travels. Pressure on the spinal nerves inside the spinal canal can also produce problems with the bowels and bladder, requiring emergency surgery.
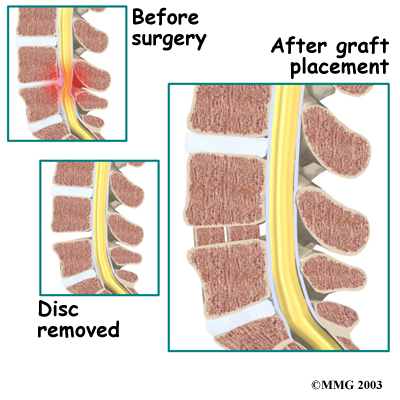
Discectomy is the removal of the disc (and any fragments) between the vertebrae that are to be fused. Taking out the painful disc is intended to alleviate symptoms. It also provides room for placing the bone graft that will allow the two vertebrae to fuse together. The medical term for fusion is arthrodesis.
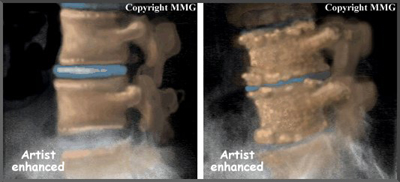
Once the disc is removed, the surgeon spreads the bones of the spine apart slightly to make more room for the bone graft. The bone graft separates and holds the vertebrae apart. Enlarging the space between the vertebrae widens the opening of the neural foramina, taking pressure off the spinal nerves that pass through these openings. Also, the long ligaments that run up and down inside the spinal canal are pulled taut so they don’t buckle into the spinal canal.
View animation of spreading vertebrae apart
View animation of graft fusion
If the fusion is successful, the vertebrae that are fused together no longer move against one another. Instead, they move together as one unit. This helps relieve the mechanical pain, which occurs in the moving parts of the back. Fusion also prevents additional wear and tear on the spinal segment that was fused. By fusing the bones together, surgeons hope to reduce future problems at the spinal segment.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
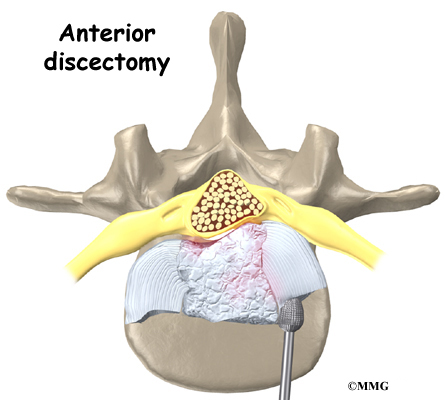
The patient is positioned on his or her back with a pad placed under the low back. An incision is made through one side of the abdomen. The large blood vessels that lie in front of the spine are gently moved aside. Retractors are used to gently separate and hold the soft tissues apart so the surgeon has room to work.
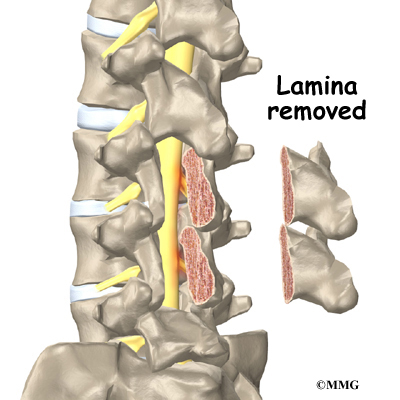
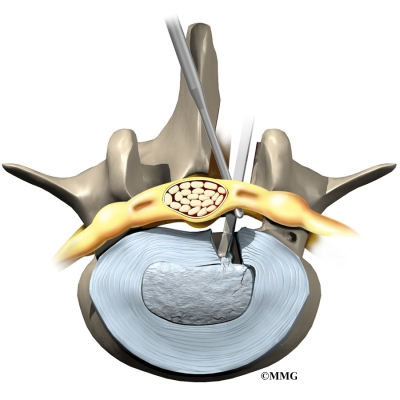
The surgeon inserts a needle into the disc. By taking an X-ray with the needle in place, the correct disc is identified. Forceps are used to open the front of the disc. Next, a tool is attached to the vertebrae to spread them apart. This makes it easier for the surgeon to see between the two vertebrae. A small cutting tool (a burr) is used to carefully remove the front half of the disc. A special surgical microscope may be used to help the surgeon see while removing pieces of disc material near the back of the disc space.
The surgeon shaves a layer of bone off the flat surfaces of the two vertebrae. This causes the surfaces to bleed. Bleeding stimulates the bone graft to heal and join the bones together.
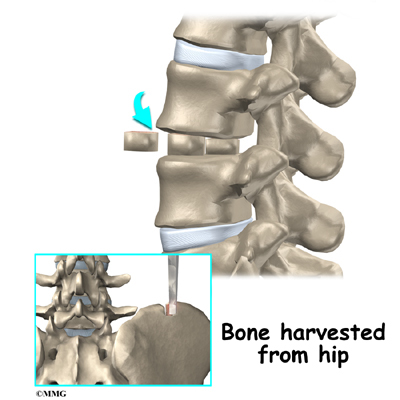
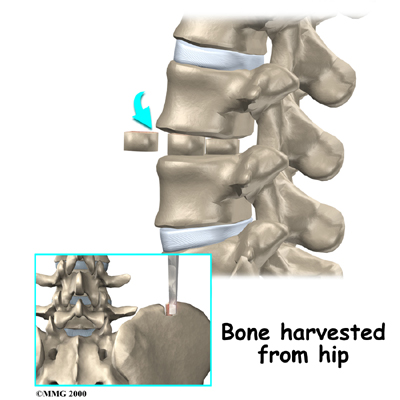
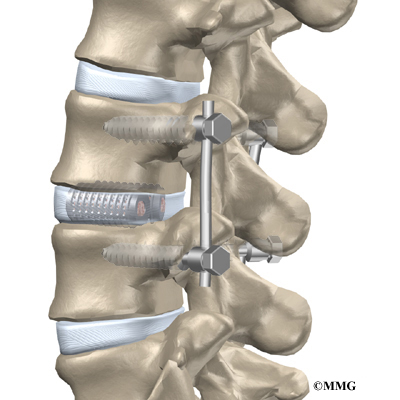
The surgeon measures the depth and height between the two vertebrae. Making a separate incision, the surgeon takes a section of bone from the top of the pelvis to use as a graft. The graft is measured to fit snugly in the space where the disc was taken out. The surgeon uses a traction device to spread the two vertebrae apart, and the graft is tamped into place.
Traction is released. Then the surgeon tests the graft by bending and turning the spine to make sure the graft is in the right spot and is locked in place. Another X-ray may be taken to double check the location and fit of the graft.
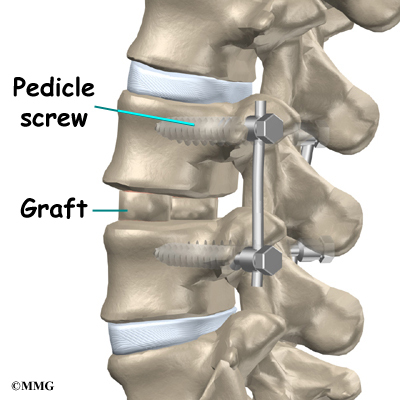
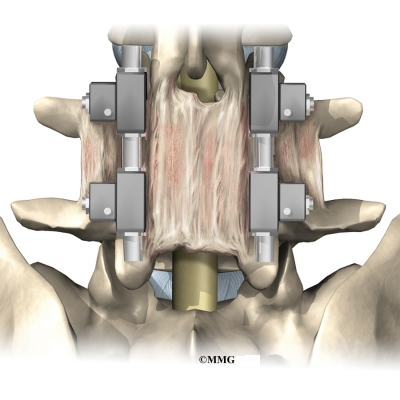
Most surgeons apply some form of metal hardware, called instrumentation, to prevent movement between the vertebrae. Instrumentation protects the graft so it can heal better and faster. One option involves screwing a strap of metal across the front surface of the spine over the area where the graft rests. A second method involves additional surgery through the low back, either on the same day or during a later surgery. In this operation, metal plates and screws are applied through the back of the spine, locking the two vertebrae and preventing them from moving.
Related Document: A Patient’s Guide to Posterior Lumbar Fusion
A drainage tube may be placed in the wound. The muscles and soft tissues are then put back in place. The skin is stitched together. The surgeon may place you in a rigid brace that straps across the chest, pelvis, and low back to support the spine while it heals.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following ALIF include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- blood vessel damage
- problems with the graft or hardware
- nonunion
- ongoing pain
This is not intended to be a complete list of possible complications.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don’t expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
View animation of pulmonary embolism
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin’s surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
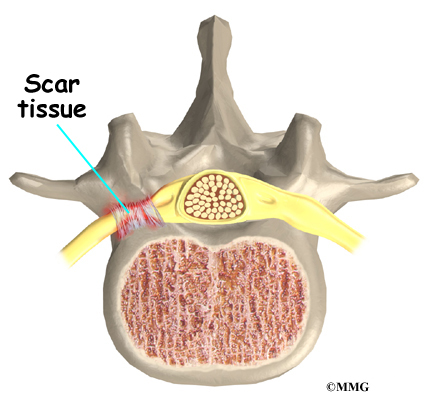
Nerve Damage
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to the spinal cord or spinal nerves can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Blood Vessel Damage
The abdominal aorta is the largest artery in the body. This major artery and the large veins that accompany it pass in front of the spine and split to go into each leg. The surgeon has to move these vessels aside to perform the anterior interbody procedure. The vessels can be injured, causing internal bleeding.
Problems with the Graft or Hardware
Fusion surgery requires bone to be grafted into the spinal column. The graft is commonly taken from the top rim of the pelvis. There is a risk of having pain, infection, or weakness in the area where the graft is taken.
After the graft is placed, the surgeon checks the position of the graft before completing the surgery. However, the graft may shift slightly soon after surgery to the point that it is no longer able to hold the spine stable. If the graft migrates out of position, it can cause injury to the nearby tissues. A second surgery may be needed to align or replace the graft and to apply metal plates and screws to hold it firmly in place.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can break. The surgeon may suggest another operation either to take out the hardware or to add more hardware to solve the problem.
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) When more than one level of the spine is fused at one time, there is a greater chance that nonunion will occur. (Fusion of more than one level means two or more consecutive discs are removed and replaced with bone graft.) If the joint motion from a nonunion continues to cause pain, the patient may need a second operation.
In the second procedure, the surgeon usually adds more bone graft. Metal plates and screws may also be added to rigidly secure the bones so they will fuse together.
Ongoing Pain
ALIF is a complex surgery. Not all patients get complete pain relief with this procedure. As with any surgery, patients should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are sometimes placed in a rigid body brace after surgery. This may not be necessary if the surgeon attached metal hardware to the spine during the surgery.
Patients usually stay in the hospital after surgery for up to one week. During this time, patients work daily with a physical therapist. The therapist demonstrates safe ways to move, dress, and do activities without putting extra strain on the back. The therapist may recommend that the patient use a walker for the first day or two. Before going home, patients are shown ways to help control pain and avoid problems.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal. Patients should avoid activities that cause the spine to bend back for at least six weeks. Patients are also cautioned against bending, lifting, twisting, driving, and prolonged sitting for up to six weeks. Outpatient physical therapy is usually started a minimum of six weeks after the date of surgery.
Rehabilitation
What should I expect as I recover?
Rehabilitation after ALIF can be a slow process. Many surgeons prescribe outpatient physical therapy beginning a minimum of six weeks after surgery. This delay is needed to make sure the graft has time to fuse. You will probably need to attend therapy sessions for two to three months. You should expect full recovery to take up to eight months. However, therapy can usually progress faster in patients who had fusion with instrumentation.
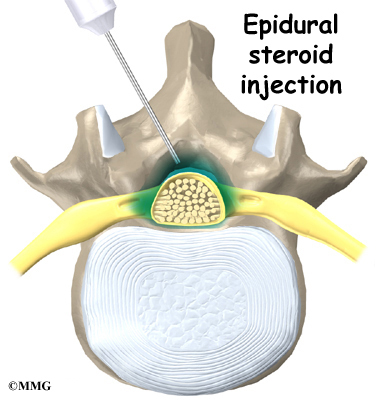
At first, treatments are used to help control pain and inflammation. Ice and electrical stimulation are commonly used to help with these goals. Your therapist may also use massage and other hands-on treatments to ease muscle spasm and pain.
Active treatments are slowly added. These include exercises for improving heart and lung function. Short, slow walks are generally safe to start with. Swimming and use of a stair-climbing machine are helpful in the later phases of treatment. Therapists also teach specific exercises to help tone and control the muscles that stabilize the low back.
Your therapist also works with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your back in safe positions as you go about your work and daily activities. Training includes positions you use when sitting, lying, standing, and walking. You’ll also work on safe body mechanics with lifting, carrying, pushing, and pulling.
As your condition improves, the therapist tailors your program to prepare you to go back to work. Some patients are not able to go back to a previous job that requires strenuous tasks. Your therapist may suggest changes in job tasks that enable you to go back to your previous job or to do alternate forms of work. You’ll learn to do these tasks in new ways that keep your back safe and free of strain.
Before your therapy sessions end, your therapist will teach you ways to avoid future problems.