A Patient’s Guide to Nutrition and Your Spine
Introduction

You are what you eat. Is that simply a funny saying or is there some truth to that old adage? The spine is not something that usually comes to mind when one thinks about nutrition – but it should. Nutrition is important in having a healthy spine. Good nutrition also helps control pain and disability when we are suffering from many different types of spine conditions.
This guide will help you understand
- what is nutrition
- how nutrition affects the spine
- how nutrition affects injury, inflammation, and pain
- how to use good nutrition to get ready for and recover from spine surgery
How you eat and exercise (or don’t exercise) will make you more or less likely to have problems with your bones, joints, and connective tissue. This guide will help you learn how to use nutrition for healing after an injury. We will describe how you can make simple changes to your diet and other lifestyle habits. These changes can be helpful if you have a painful spine condition. You will learn how to tell if you have given the changes enough time to work for you. You’ll learn to know if it’s time to move on to other health care solutions for your problem.
Nutrition
What is nutrition?
Nutrients are the chemical elements that make up a food. Nutrients are the basics of what you eat that give your body what you need for “running the show”, that is, for metabolism. Certain nutrients such as carbohydrates, fats, and proteins provide energy. Other substances such as water, electrolytes, minerals, and vitamins are needed for metabolic processes.
Nutrition is all of the internal chemical changes that happen as a result of what we eat (or do not eat) each day. Good nutrition means that what we are swallowing is something that adds to our health. Once we have digested it, food has an important job to do in our body.
Good nutrition is needed for tissue growth and repair. We get good nutrition by eating foods and taking supplements that contain all the proper and necessary ingredients. We also get good nutrition by being able to completely digest the things we swallow. Then we must be able to absorb the nutrients into the blood and other body fluids. With the right nutrients given to the cells, metabolism, or the work of the body, can occur in the most efficient and healthy way.
By the definition above, we know that a lot of what we eat is not nutritional. When we eat a purple pill or swallow a blue-colored sports drink, what we are taking in has no job to do in our body. That purple or green coloring is not a chemical your body has any use for.
The same is true for things like the preservatives added to your cereal. These chemicals are put in so that the cereal doesn’t get moldy in the box. The same thing is true for traces of hormones and antibiotics left in our meat and dairy foods. When you eat French fries from a fast-food restaurant, the oil they have been cooked in has changed into a type of fat that can’t be used by your body. In fact, it has become something called a trans-fat. Trans-fats damage the walls of your body’s cells. This will make more work for your body.
Metabolism
What is metabolism?
Metabolism refers to all of the physical and chemical changes that are taking place in your body every moment. Making energy in the body is part of metabolism. All the physical work that occurs inside your cells is part of this process, too. It includes all the work and chemical changes that happen every day in your bones, connective tissues, body fluids, and organs.
Metabolism refers to the work of changing the chemical energy in nutrients into mechanical energy or heat in your cells.
Metabolism involves two basic processes. There is anabolism (building up) and catabolism (disintegration or breaking down). During anabolism the body works to change simple chemicals from what you have eaten into complex parts, like blood, bone, or connective tissue. During catabolism, complex parts are broken into simpler pieces. One catabolic process is the breaking down of an apple you have chewed and swallowed. It is broken down into water, fiber, vitamins, and minerals. The end of catabolism is usually something being passed out of the body. We are healthy when both anabolism and catabolism are in proper balance.
Our bodies have very good ways to know when food we eat is not useful and to get rid of it. But it takes up a lot of good nutrients to sort out what’s good and what’s not. Getting rid of damaging things you eat uses up energy in the cells, too.
Nutraceuticals
If you have aches and pains, if your joints are inflamed, or if you are overweight, your diet may not have enough good nutrition to get all the necessary work done. That is why nutraceuticals have become so important.
Nutraceutical is a new word, invented by Dr. Stephen DeFelice in 1989. It is a combination of the words nutritional and pharmaceutical. Nutraceuticals are dietary supplements that are sometimes also called functional foods. Many people take nutraceuticals to offset an inadequate or unhealthy diet.
Even with a good diet of fruits and vegetables, whole grains, and the right amount and kind of protein, the standard American diet usually does not have enough nutrition for all the work your body needs to get done. We grow our fruits and vegetables with lots of fertilizers. Chemicals from the fertilizers remain on it when it’s part of your meal. The same is true for pesticides and herbicides sprayed on the plants before harvest.
We harvest fruits and vegetables when they are not quite ripe. Then they are trucked thousands of miles to our stores. Food that is not quite ripe when picked means it doesn’t have its full nutritional value. Food harvested too early will not bruise as easily when it is loaded on and off trucks. It will look good when you buy it, but it won’t have all the nutrition you need to get from eating it.
Proper Balance
We face challenges our grandparents never knew. There are extra chemicals in our food and water. Our food supply just is not as nutrient-rich as we need it to be. A proper balance between protein and high fiber, starchy foods is important for good nutritional health.
It is important to understand that nutrients always work together. Nutraceuticals can help when you aren’t able to eat a perfectly balanced diet. The same is true when you can’t eat everything organic. Supplemental vitamins, minerals, amino acids, and fatty acids are the way to help yourself meet all the needs of your body. This includes growth and repair after injury. It’s also true for the metabolic work needed to feel good, be strong, and live well.
Healthy fats are needed to grow and repair normal connective tissue, bones, and body fluids. The fiber and carbohydrates in whole grains and fresh produce are what your body is designed to thrive on. The fats found in olive oil, deep ocean fish (like salmon and sardines), and nuts and seeds are all part of good nutrition.
Organically raised beef, poultry, and wild ocean fish give the best protein. When you can’t eat organically raised meats, you can decrease your exposure to damaging chemical residues. You can do this by removing all visible fat from the meat before you cook it.
Specific problems can be related to not enough (or too much) of a single vitamin or mineral. But the proper function of the human body requires the right amounts of ALL the nutrients. You can think of it like a recipe. Your soup will taste good when all the ingredients are there in the right balance. Having too much of some of the spices, or not enough salt, will make a pot of otherwise really good food taste terrible. The same is true for the nutrient “soup” in your body. You need to have the right amounts in the correct proportions to have all your body systems work at their best. Every vitamin, mineral, amino acid, and fatty acid has hundreds of jobs to do. None of these nutrients can work well if it is not in the right relationship with all of the other nutrients.
Nutrition and the Spine
How does nutrition affect the spine?
Nutrition will determine how strong your teeth, bones, and connective tissue are. We begin to build our skeleton and connective tissue before we are born. Our diet in childhood has a major effect on how strong we are as adults. What you eat during your whole life will decide how able you are to repair bones, cartilage, ligaments, tendons, and muscles.
Everyone has to replace body tissues due to normal every day wear and tear. Some of us also have repair work to do after injuries or surgery. The raw material for repair comes from our diet. Vitamin C, all of the B vitamins, vitamin D, vitamin K and the minerals calcium, magnesium, copper, zinc, boron and manganese are especially important for bone and connective tissue health. Drinking enough water is also essential.
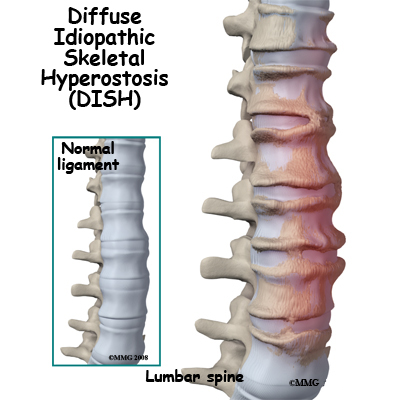
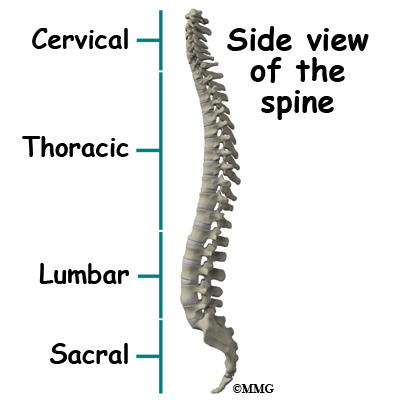
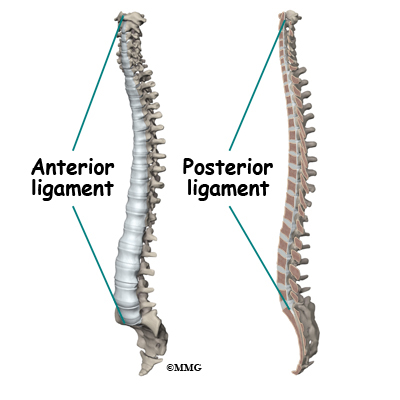
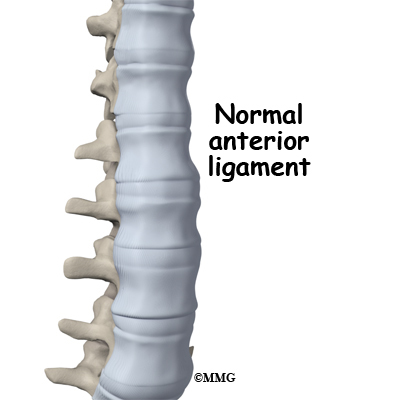
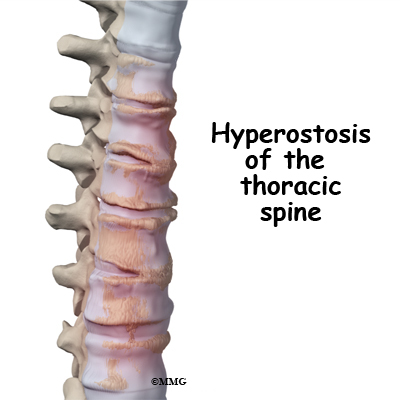
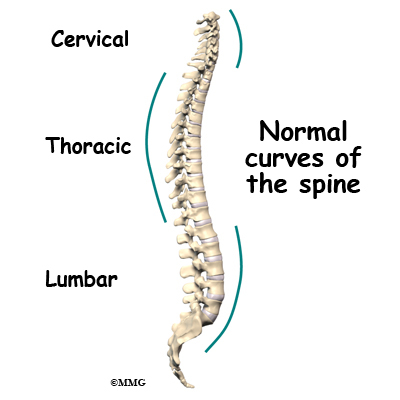
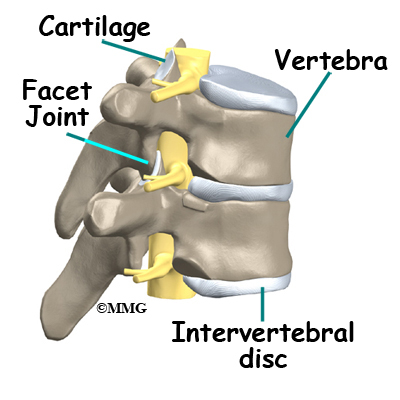
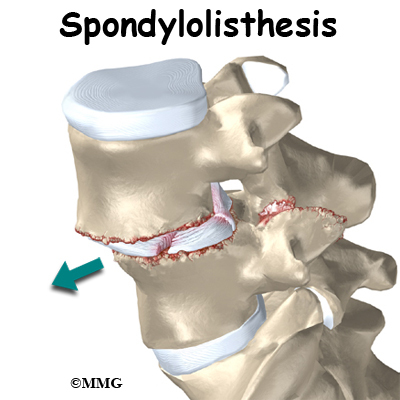
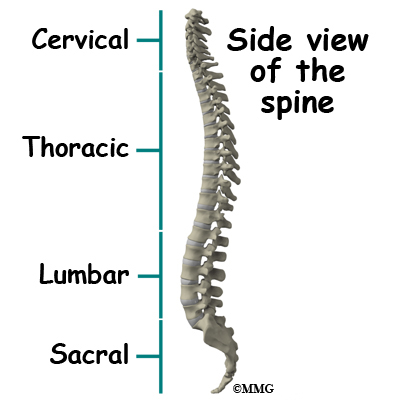
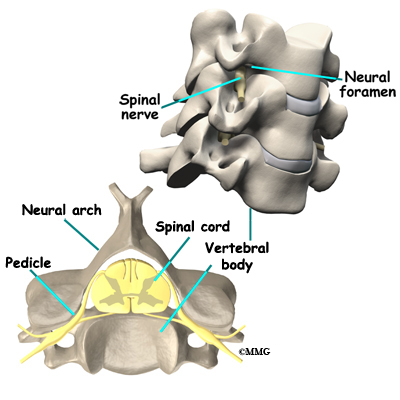
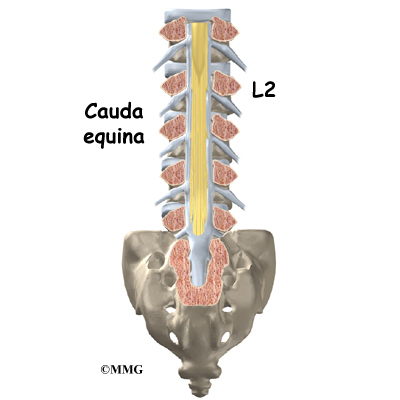
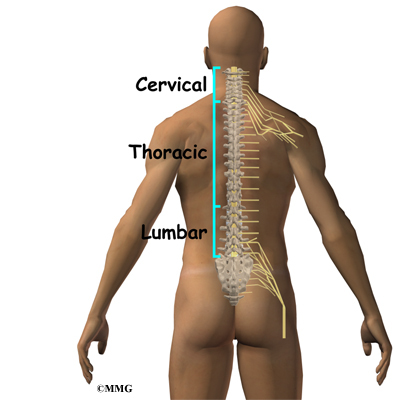
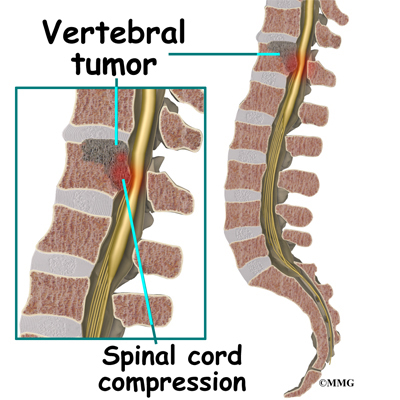
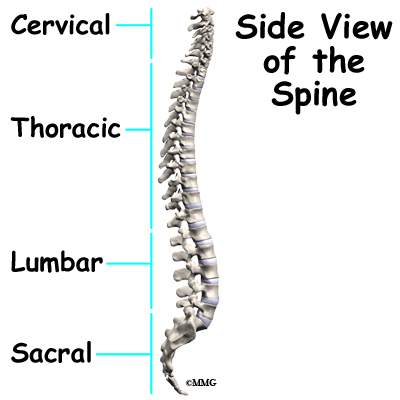
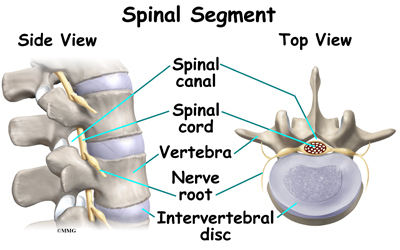
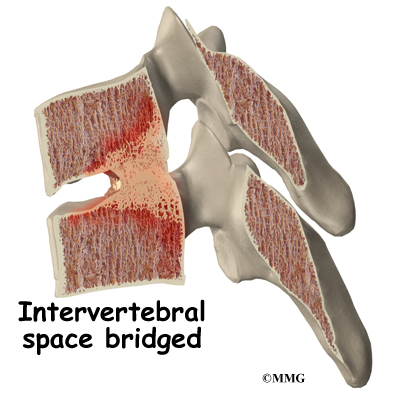
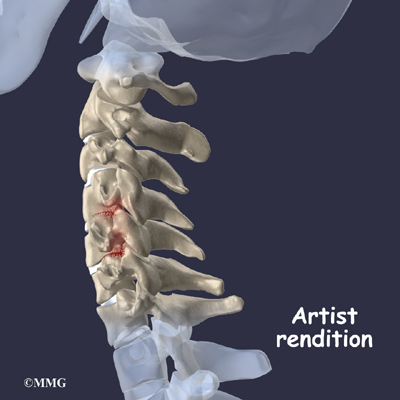
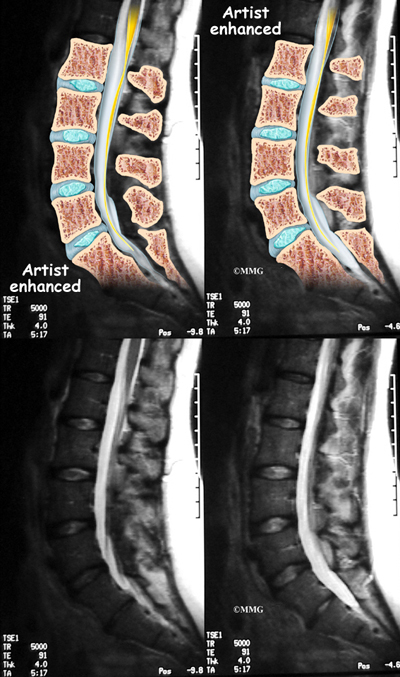
Your spine is your backbone. The bony pieces of the spine are called vertebrae. There are 33 of these bones. Between each vertebra is a disc made of tough cartilage with a fluid center. These discs provide the cushion that allows your backbone to bend and twist. Discs also act like shock absorbers as we walk, run, and jump. Each vertebral segment consists of bone next to bone with a cartilage cushion between. They are tied together with connective tissue, ligaments, and tendons.
Related Document: A Patient’s Guide to Lumbar Spine Anatomy
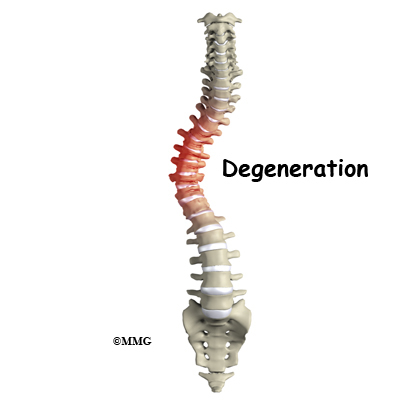
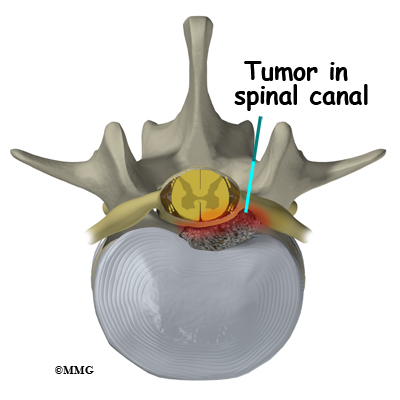
Degenerative disc disease is an example of damage to connective tissue that is affected by nutrition. Everyone is going to have a certain amount of damage to the spine. This occurs throughout a lifetime. The discs can flatten, and protrude from between the bones. In time, most people will have small tears in the outer layers of these discs. You are more likely to have injuries if you have poor nutrition. And you’re less likely to have good healing.
Poor nutrition means not getting enough vitamins C, A, B6 and E, as well as the minerals zinc and copper. Daily wear and tear plus injuries from work, sports, or accidents can damage your spinal discs. Good nutrition and adequate hydration (getting enough fluids) play a vital role in your body’s ability to repair the damage and recover from the inflammation that causes the pain of back injury.
Connective tissue, like the cartilage between your joints and the ligaments and tendons that hold them together is made mostly of collagen. Collagen is a type of protein and water. Strong collagen fibers require a steady supply of dietary protein. They also need vitamin C along with vitamins A, B6, and E, and the minerals zinc and copper.
Building Bone with Good Nutrition
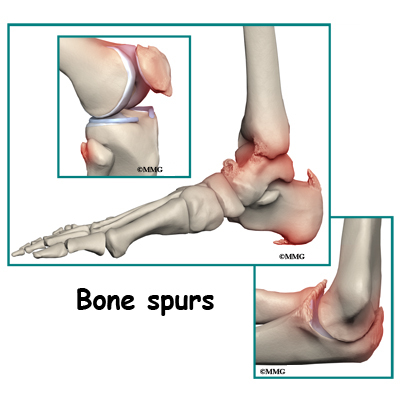
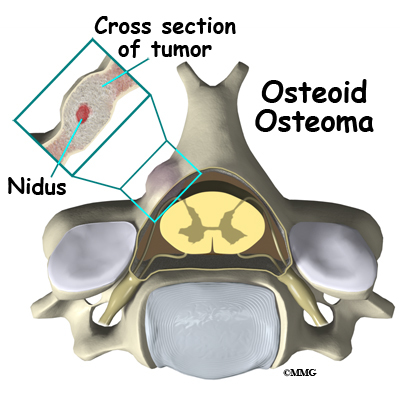
Joints are made and maintained, repaired, and protected with proper nutrition. Bone is made of minerals like calcium, phosphorus, magnesium, and boron. Bones also contain water and collagen. The upkeep and repair of bone and connective tissue requires the right amounts of vitamins and other nutrients working together.
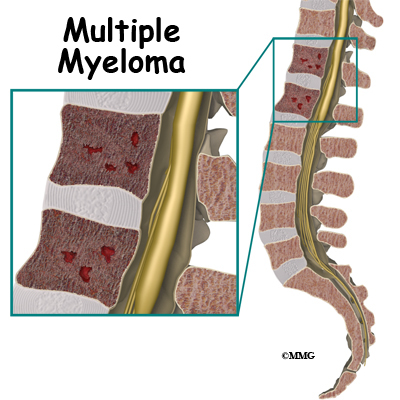
Another diet and nutrition-related bone disease is called osteoporosis. Osteoporosis means the bones are weakened, brittle, and can break easily. Lifestyle and nutritional factors can lead to the bone loss of osteoporosis. This includes what you eat during bone-building stages in childhood and adolescence. Nutrition throughout the adult years is also important to maintain good bone density. Calcium intake is a major factor for building bone density. You will find yourself with weakened bones if you do not get enough calcium. The same is true if you do not absorb or properly metabolize the calcium you do eat. You can also lose too much calcium through the urine because of dietary choices. Other conditions like chronic mental or emotional stress that cause inflammation of the digestive tract can prevent calcium absorption. A lack of proper acidity in the digestive tract can also make calcium pass through unabsorbed.
Vitamin D is essential for maintaining and regulating the health of bones and teeth along with many other functions in the body. It is a compound that is more of a hormone than a nutrient or vitamin and thus has an important role in regulating immune function and cell growth.
Vitamin D is needed to absorb calcium from the gut. It prevents bone loss and helps rebuild new bone. Vitamin D is needed for the enzymes that strengthen collagen. Collagen is a major component of bone and connective tissue. Vitamin D has also been shown to aid in nerve and muscle (neuromuscular) function.
How can you get enough vitamin D to ensure good body and bone health? Sunlight will produce vitamin D in your skin. Exposure of the skin to sunlight for five to 30 minutes between 10 am and 3 pm (in most geographical locations) twice a week is usually enough to make your own Vitamin D. As you get older, your capacity to produce vitamin D from sunshine slows down.
Diet may aid you but not with natural foods. Except for cod liver oil and some types of fish (salmon, tuna, mackerel, sardines), vitamin D is not found in what we eat. Only foods that have been fortified with vitamin D (e.g., milk, cereal, yogurt, orange juice) have any significant amounts of this vitamin.
A very low fat diet will make it harder for you to absorb vitamin D from your food. Lack of sunshine and limited consumption of foods fortified with Vitamin D may mean you need to take a nutritional Vitamin D supplement. Your physician will help you decide what kind and how much to take for your age, health, and risk factors. Vitamin D supplementation may be based on current levels of vitamin D in your blood.
You may be someone who does not rebuild bone as quickly as you lose it. Nutritional deficiencies can make this problem worse. Caffeine-containing drinks like coffee and colas will cause increased loss of calcium through the urine. Cola drinks with high levels of phosphorus also disrupt calcium metabolism and healthy bones.
Magnesium is as essential as calcium for strong bones. As much as 50 per cent of your magnesium is found in your bones. Magnesium is required to move calcium into bone. Magnesium is also needed to make vitamin D active. A typical American diet contains much less than the recommended daily requirement for magnesium.
Magnesium is lost through the urine. This happens when people are stressed. Studies have shown something as common as loud noise levels will increase the loss of magnesium. Alcohol and many drugs used for heart disease and high blood pressure also cause magnesium loss. Bone repair calls for amounts of magnesium usually much higher than the recommended daily allowance.
L-lysine is an amino acid that you need to activate intestinal absorption of calcium. You will lose too much calcium through your kidneys if you do not have enough lysine. Lysine is an essential element for building the collagen framework. Minerals like calcium and magnesium weave into collagen to create bone.
You may need supplementation with these minerals, vitamins, and amino acids. This applies to you if you work indoors or don’t get out in the sun much. You are also at risk if you are elderly, or are a sedentary person who drinks a lot of coffee or cola drinks. If you do not digest well, or if you eat a very low fat diet, it may be important to use a good quality supplement to protect your bones.
Specific nutritional factors that will increase your risk of pain and inflammation are
- not enough omega 3 fatty acids from ocean fish
- not enough fruits and vegetables in the diet
- not enough vitamin D from sun exposure or fortified foods
- risk factors for vitamin D deficiency (e.g., older age, dark skin, use of sunscreen, obesity, kidney disease, liver disease, use of some medications, milk intolerant)
- not enough of the minerals potassium and magnesium
- not enough protein and high quality fat in the diet to control enzymes that produce inflammation
- too many sweets and starches in the diet, leading to weight gain and to excess insulin
- too many free radical ions from rancid and hydrogenated fats, low nutrient refined foods, chemical additives and residues
Nutrition and Inflammation
Inflammation is most often thought of as the redness, warmth, swelling, and pain that occur with an injury. The body responds this way whether it’s a surgical incision or a spider bite. Inflammation is also present in an infection like a strep throat or the achy, hot finger joints of rheumatoid arthritis.
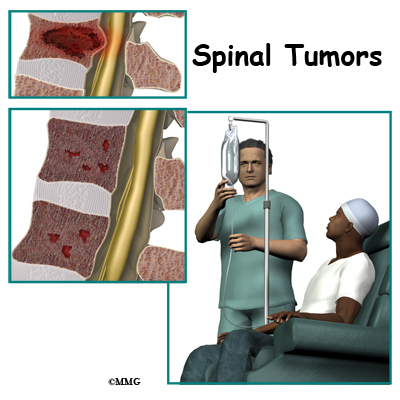
Wound healing and fighting infection are just some of the ways inflammation is activated. Inflammation is happening all the time in more or less obvious ways in your body. Medical science has begun to understand the connection between inflammation and most of the chronic degenerative diseases. Some of these diseases – like cancer, heart disease, or diabetes – develop quietly for many years before causing problems. We aren’t even aware they are present. Pain isn’t always a part of these diseases. People can be pain free even when a lot of tissue damage has occurred. Others conditions, like osteoarthritis, gall bladder disease, or degenerative disc disease, make their presence known. Pain with these conditions can range from mild to unbearable.
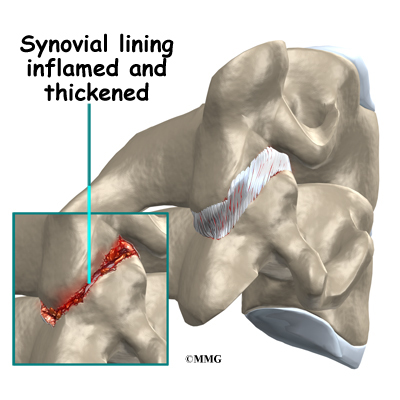
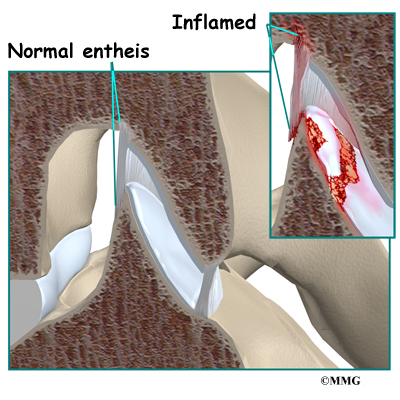
These conditions all have one thing in common. The tissues of the body parts involved are inflamed. The process of inflammation depends on a number of different chemical elements. These are called inflammatory mediators. Chemical mediators are released from certain kinds of white blood cells. These white blood cells are part of our immune system. First they travel to a target area. Then they cause a series of reactions that create the tissue changes we refer to as inflammation. At first this process is actually a repair response to some sort of injury or insult to the tissue. Later, the inflammatory process can become chronic and the cause of further injury.
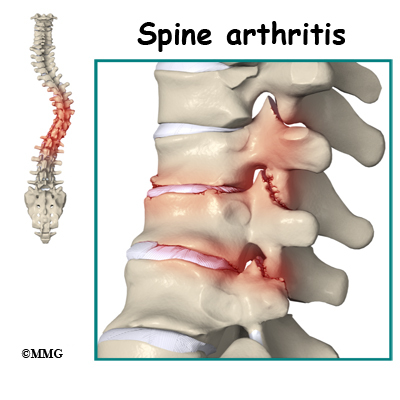
Inflammation and Back Pain
Healthy repair depends on good nutrition. Poor nutrition can lead to damaging inflammation in the joints of your spine. Inflammation causes the loss of the cellular framework that holds bone and connective tissues together. Studies show that some people with osteoarthritis have more rapid damage to their joints. This is because they have more inflammatory chemistry in their bodies.
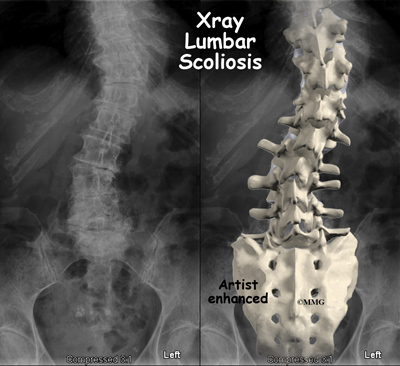
Back pain may or may not be present in people with bone or cartilage changes in their spine. For instance many people have x-ray images that show they have flat and bulging discs. Or they may have brittle bones. Yet they have no pain. It is inflammation that causes the tissue changes that create the sensation of pain.
Inflammation stimulates the growth of new blood vessels in joint tissues. This growth process also causes new nerves to grow in areas around joint cartilage. Doctors think this new nerve growth may be why back pain goes along with inflammation. The increased tissue activity and the swelling that comes with inflammation can make the new nerves very sensitive. All of the steps in this inflammatory process (new blood vessel growth, new nerve growth) keep each other going in a never-ending cycle. Stopping inflammation will relieve pain and slow down joint damage.
Back Pain and Obesity
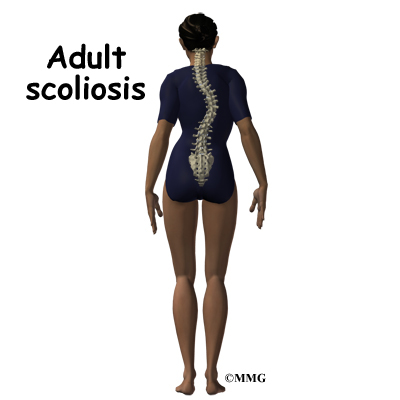
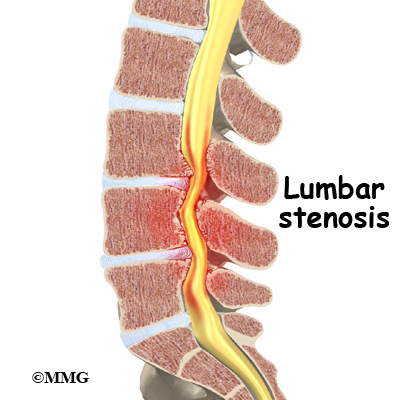
Abdominal obesity adds to spine problems in very important ways. Fat around your middle can cause strain on the muscles and ligaments that support your spine. The joints of your spine are especially vulnerable to daily wear and tear from lack of support.
Most of us get fat by eating too much of the kind of starchy, refined foods that call up more insulin. Insulin will signal enzymes in your body. These enzymes increase levels of inflammatory cells. They also increase cholesterol and constrict (close down) blood vessels. All of these actions help increase the levels of pain you feel from all over your body.
Abdominal fat is made of the type of cells most active at making the kind of chemistry that causes damaging inflammation to all of your joints. The more belly fat you have, the more inflammatory chemistry you are making. Some lean people are also at risk.
How does nutrition affect healing after injury or surgery?
Good circulation is needed to build and repair a surgical incision, injured bone, or connective tissue like cartilage and ligaments. Your blood vessels carry all the raw materials needed to maintain proper strength and function of your bone and connective tissues. Your blood vessels also carry away from these body parts all the waste material from normal wear and tear as well as from injuries. A diet that has too much starch and sweets, and not enough protein and healthy fats, will cause blood vessels to constrict. Then there is less blood flow to the areas that are injured and need repair.
All of the chemical reactions that make up the work of growth and repair require good nutrition. Herbs, fruits, and vegetables contain the dietary sources of antiinflammatory chemistry needed for tissue healing. Plant foods have antioxidants that decrease the chemistry that triggers inflammation. This type of plant is called a flavonoid. Flavonoids are plants that have biologic and metabolic properties in the body. They also strengthen the healing process. They do this by knitting collagen fibers into tightly woven connective tissue. The result is well-knitted skin and blood vessels; dense bone; and strong, elastic ligaments and tendons.
What changes can you make to your diet and supplement choices if you have a spine condition?
It can be confusing to try to sort out what supplements to take. It’s not always easy to know what foods to eat or not eat to help with a spine-related problem. Different musculoskeletal conditions will have some different nutritional requirements. The form of each supplement will also be important, in terms of how useful it is for your condition.
For example, powdered nutrients in capsules or liquid forms are much more likely to be fully digested and absorbed. Tablets are often less expensive. But they don’t break down in many people’s digestive tracts.
Osteoporosis is an example of a spine-related condition with a clear link to nutritional status. Most people with osteoporosis will be advised to take at least a calcium/magnesium supplement. The best quality mineral supplements for osteoporosis are powdered and in the citrate form (for example, calcium citrate). Vitamin D should always be included in an osteoporosis formula.
Inflammatory conditions benefit from antioxidant nutrients like vitamin E. It must be natural vitamin E, not synthetic. It should always have mixed tocopherols in order to be most effective. Any inflammatory condition can be improved with the addition of at least five fish meals a week. A good, pure fish oil supplement taken daily can also help.
Here are some changes you can make to improve your spine condition. Most people will notice results in less than two weeks by following these general rules
- Drink at least eight large glasses of water or herbal tea daily. Avoid fruit juices or other beverages with coloring and preservatives added. This includes soda pop.
- Eliminate simple sugars. Get rid of sweets and starchy, refined white flour foods from your diet.
- Avoid packaged foods with added preservatives and colorings
- Take a high quality multiple vitamin/mineral supplements three times daily with each meal
- If you have any form of arthritis or any inflammatory condition, take a pure fish oil supplement. Most people are helped by one to three grams of combined omega 3 fatty acids daily. Look for EPA and DHA on the label.
- Add vitamin D3 to your supplements; make sure you are get 800 IU to 1000 IU daily. You may need more if you have a history of malabsorption (e.g., celiac disease, inflammatory bowel disease, cystic fibrosis, gastric bypass surgery)
Long-term dietary changes can benefit your spine condition. If you are overweight, ask a health professional to help you lose weight, especially abdominal fat. Most people can do this safely by
- eating fresh, raw, or steamed vegetables every day
- eating two or three pieces of fresh fruit every day
- eating five to seven fish meals a week
- eating three to six ounces of clean, lean beef, poultry, lamb, or game meat daily – eggs are also an excellent source of protein for most people
- using olive oil on salads and for cooking daily
- eating fresh nuts and seeds. Almonds, walnuts, and pumpkin seeds give us high quality, healthy fats
If you do not have a regular habit of exercise, invest in instruction with a professional who can teach you how to strengthen your muscles and protect your joints. Certain exercises will be very good for some spine conditions, and possibly harmful for others. An exercise professional is your best choice for guidance to design a safe, effective program just for your needs.
How long does it take to see results from these changes?
Many people who change their diets see results right away. The difference in body pain levels can be noticed in a matter of days. Reducing inflammation by stopping the triggers that sweets and starches create can be felt very quickly. The effects of diet changes are even more when added to the supportive chemistry of antioxidants. Dietary supplements can encourage your healing even more dramatically.
It can take some months of steady supplementation to rebuild your tissues after illness or injury. It depends on how deficient you are in certain nutrients. It may take three to six months for to experience the benefits of a specific supplement program. This time frame may vary based on your condition. Your doctor can advise you about this.
For expert help to start a nutrition plan for your spine health, see a nutritionist or contact a licensed naturopathic physician. Specially trained nutritionists may be available in your area. Many registered dietitians and conventionally trained nutritionists are limited in their ability to give personalized attention to in-hospital patients. You may have to look for an independent practitioner with more advanced training. The ongoing support of a progressive nutritionist can help you start new, healthy habits that will become a permanent part of your daily life.
Naturopathic doctors (NDs) are also available to help patients develop healthier nutritional habits for the spine. Naturopathic physicians practice the art and science of natural health care. They are trained at accredited medical colleges. Partnerships between medical doctors and naturopathic physicians are becoming more common all over the U.S. and Canada.