A Patient’s Guide to Nutrition and Surgery
Introduction
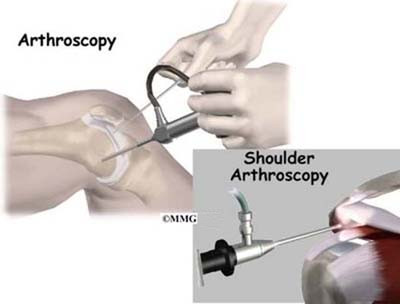
Surgery always means a certain amount of risk to your well being. Surgery is a deliberate, skillful injury to your body. It may take you several weeks to months to heal. Infections and blood loss are two possible complications that your surgeon will want to help you avoid.
You can do your part to make sure you heal well without problems. You can do this by choosing the most nutritious diet. Using supportive supplements for some weeks before having an operation is also helpful. Surgery is a big event. It makes sense to give yourself extra nutrition so you can replace any blood loss. Better nutrition can also help your incisions heal. Your diet and nutritional supplements will provide the raw materials your immune system needs to protect you against infection. These same nutritional elements are what you will use to repair your skin, nerves, blood vessels, muscle and bone. Getting good nutrition will help you make the best of your surgery.
This guide will help you understand
- basic vitamin and mineral information
- what specific vitamins and minerals do for you
- what relation vitamins have to surgery
Information
Some vitamins are water-soluble. This means they dissolve in liquid or fluids. Since your body is mostly made up of fluid, you can quickly and easily absorb water-soluble vitamins. They also leave the body quickly through fluid loss such as urination. They must be taken two or three times every day. This way you’ll keep enough in your system to meet the demands of the day. Each vitamin in the water-soluble B-vitamin group must be taken together in order for each one to work properly.
Other vitamins are fat-soluble. They are absorbed by fat cells. These can be taken just once a day or even just a few times a week. Fat-soluble vitamins are used up fast when you are under high-stress. This is true when you are in pain, when you are fighting infection, or when you are healing an injury.
Our appetites change when we are stressed. We can’t always eat as well as we would like. Taking nutritional supplements when you are extra stressed makes good sense.
Vitamins and Minerals
What do vitamins and minerals do for you?
Vitamin B12
Vitamin B12 is the largest and most complex of all the vitamins. You need vitamin B12 so your body can create energy from your dietary fats and proteins. B12 is needed for you to make hemoglobin. Hemoglobin carries oxygen in the red blood cells. Vitamin B12 is needed for your nerves to function properly and for your moods to stay even. It even helps your memory and brain function.
Vitamin B12 deficiency affects about 15 percent of the people over the age of 60. There are several reasons people are low in B12. Most of these are related to changes in the stomach lining. These changes occur with age, from drinking alcohol, or from infection with bacteria that live in stomach ulcers. Certain drugs such as acid blockers used for gastric reflux or Glucophage used for Type 2 diabetes can also affect the stomach lining.
Folate
The terms folic acid and folate can both be used to refer to this B-complex vitamin.
Folate plays a vital role the work and the growth of all your body cells. Not having enough folate causes a number of different problems in the cells. Some of your immune system white blood cells will be affected. A shortage of folate for the rapidly dividing cells of the bone marrow will result in fewer but larger red blood cells. This causes a type of anemia called megaloblastic or macrocytic anemia. The large, immature red blood cells that result do not carry oxygen normally. If you do not take in enough folate you will experience fatigue, weakness, and shortness of breath. Megaloblastic anemia from folate deficiency is the same as megaloblastic anemia resulting from vitamin B12 deficiency. Never take a folate supplement without making sure you have enough Vitamin B12.
Vitamin B6
Vitamin B6 is needed for the proper function of about 100 essential chemical reactions in the human body.
Vitamin B6 is needed to make heme, a component of hemoglobin. Hemoglobin is found in red blood cells. It is vital to the their ability to transport oxygen throughout your body.
People who are low in vitamin B6 have impaired immune function. This is especially true for the elderly. Sleep, pain, mood, memory, and clear thinking are also affected by a shortage of Vitamin B6. The stress of hospitalization for surgery causes many people to lose sleep. Increased pain and mood changes are also common. You may find your appetite is changed when you are in the hospital. And you may not eat as well as you should. Taking a supplement that contains all of the B vitamin complex, including Vitamin B6, will help decrease the effects of your stress.
Vitamin B1 (thiamine or thiamin)
Vitamin B1 plays a critical role in making energy from food. It is needed for your heart, digestive system, and nervous system. Your muscles especially need vitamin B1 to work properly.
Thiamine deficiency is caused by not eating enough thiamine-rich foods. This occurs most often in low-income groups. Their diets are often high in carbohydrates. Alcoholism is linked with low intake of thiamine and other nutrients. Chronic alcohol use is the main cause of thiamine deficiency in higher income groups.
If you drink large amounts of tea and coffee (even decaf), you may end up with not enough thiamine. This is because of the action of certain enzymes in these drinks. Vitamin C and other antioxidants can protect your thiamine levels by preventing it from changing into an inactive form.
There are no known toxic effects from thiamine in food or from long-term oral supplementation (up to 200 mg/day).
Vitamin B2 (riboflavin)
Vitamin B2 is essential for changing the carbohydrates, fats, and proteins in your food into energy in your cells. It also helps manage drugs and environmental pollution in your liver.
If you do not have enough riboflavin you may not be able to absorb the iron you need to make hemoglobin in your red blood cells. Studies show that increasing your riboflavin intake will increase your red blood cell hemoglobin levels. Riboflavin improves your ability to prevent or recover from iron-deficiency anemia.
No toxic or adverse effects of high riboflavin intake in humans are known. High dose riboflavin therapy makes your urine a bright yellow color. This is a harmless side effect.
Vitamin B5 (pantothenate)
Pantothenic acid is essential to all forms of life. It is another of the vitamins you need to create energy from your food. Vitamin B5 is key to making the special fats that cover your nerves. This covering or lining is called a nerve sheath. It’s needed to pass messages along your nerves to all your tissues. Vitamin B5 helps regulate the production of cholesterol and your major hormones. B5 is needed to make hemoglobin to carry oxygen in your red blood cells. Your liver uses it to break down many drugs and environmental toxins.
Vitamin B5 will speed up wound healing. It can also increase the strength of scar tissue. Pantetheine is a form of vitamin B5 that can help lower your cholesterol and triglycerides if these are too high.
Pantothenic acid is not known to be toxic in humans. Diarrhea can occur with very high intakes (10 to 20 grams/day) of calcium D-pantothenate. Pantethine is generally well tolerated in doses up to 1,200 mg/day.
Vitamin B3 (niacin)
Vitamin B3 is also called nicotinamide or nicotinic acid. It is required for the proper function of more than 50 enzymes. Without it, your body would not be able to release energy or make fats from carbohydrates. Vitamin B3 is also used to make sex hormones and other important communicating molecules. People with high levels of vitamin B3 have less throat and mouth cancers. It can also help with cholesterol health. And it’s important for insulin-dependent diabetes. A severe lack of niacin will cause death from the disease called pellagra.
The usual advice is that you take a daily multivitamin/mineral supplement that will give you at least 20 mg of niacin daily. Higher doses of different forms of vitamin B3 can cause problems. This is true for people with liver disease, diabetes, or gout. It’s also true for anyone with active peptic ulcer disease, cardiac arrhythmias, inflammatory bowel disease, migraine headaches, and alcoholism.
Biotin
Biotin is one of the B-complex vitamins. It is needed for four important enzyme reactions in your body. These enzymes cause cell growth and immune system protection against bacterial and fungal infections. If you do not have enough biotin it can lead to depression, a sense of tiredness, and weakness. You may also notice a rash on your face and numbness and tingling of your hands or feet.
Pregnancy can cause a woman’s biotin levels to drop too low. This may cause birth defects. Not enough biotin can also cause problems with your blood sugar. This is especially true if you have diabetes. If you have brittle fingernails or notice increased hair loss, you may be low in biotin.
Biotin is not toxic even in higher doses. Biotin in capsule form is safe to take in doses up to 200 mg/day in people born with problems absorbing biotin. People with normal ability to digest biotin can take doses of up to 5 mg/day without problems.
Vitamin C (ascorbic acid)
Vitamin C is also known as ascorbic acid. It’s a water-soluble vitamin. Unlike most mammals, humans do not have the ability to make their own vitamin C. You have to get the vitamin C you need through what you eat and in the supplements you take.
Vitamin C is required to make collagen. Collagen is an important part of your blood vessels, tendons, ligaments, and bone. Vitamin C also plays an important role in making up your brain chemistry. Chemical balance is essential for how well you can think. Your moods may even be affected by changes in brain chemistry. Vitamin C is also needed to carry fat into cells for use as energy.
Vitamin C works well as an antioxidant. Even in small amounts vitamin C will protect essential molecules in your body. This includes proteins, lipids (fats), carbohydrates, and the genetic material of your cells. Vitamin C protects your cells from damage caused when you are exposed to toxins or pollutants. Powerful chemicals from smoking or medications can also damage cells.
Your ability to heal after surgery will depend on having proper blood flow to the surgical site. Vitamin C will help you heal from the trauma that is part of your surgery. Vitamin C allows blood vessels to be relaxed and open. You will deliver the most amount of blood to your injured tissues if you have enough vitamin C. Blood flow to injured areas is central to how well we heal. After surgery your circulation will be slowed by inactivity. If you have atherosclerosis or hardening of the arteries, your blood vessels are less able to relax. This adds to the challenge of recovering after an operation.
Adding vitamin C will improve the dilation(opening) of your blood vessels. This is important if you have certain health problems. This includes anyone with atherosclerosis, angina pectoris, congestive heart failure, high cholesterol, or high blood pressure. Improved blood vessel dilation can occur with a dose of 500 mg or more of vitamin C daily.
Vitamin A
Vitamin A is required for recovery from surgery. It is commonly known as the anti-infective vitamin. It is central to normal functioning of your immune system. Vitamin A is also needed to maintain the integrity and function of your skin and mucosal cells. Mucosal cells are the cells that line body cavities such as your mouth, intestines, and stomach. Vitamin A is important in making white blood cells. These are critical in the immune response that protects you against infection and promotes healing of your injuries.
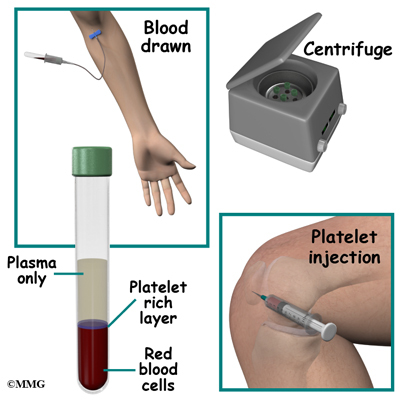
All kinds of blood cells depend on vitamin A. Blood cells come from parent cells called stem cells. Stem cells need vitamin A to mature into normal red blood cells, white blood cells, and platelets. All of these types of blood cells are needed by your immune system to respond to surgery.
When you enter a hospital or clinic for surgery, many things will stress you. You will also be exposed to bacteria and viruses that your system is not used to. You are at much higher risk for infection at this time. Infection will quickly use up your vitamin A stores. In this way, infection starts a vicious cycle, because not enough vitamin A is related to increased severity and likelihood of death from infectious disease. It is important to go into surgery with a good supply of vitamin A in your tissues. You will need to continue taking enough vitamin A to keep those levels high.
Vitamin A is also needed to move the iron you have stored in your tissues to the developing red blood cells. This is important for making hemoglobin, the oxygen carrier in red blood cells.
Losing a large amount of blood in surgery can cause iron deficiency anemia. If you do not have enough vitamin A, you are more likely to develop iron deficiency anemia. If you supplement with a combination of vitamin A and iron you will be less likely to have anemia than if you take either iron or vitamin A alone. The usual recommended dose of vitamin A is 2,500 IU (International Unit, a measure used for vitamins) of vitamin A. A safe alternative is up to 5,000 IU of vitamin A when at least 50 percent comes from beta-carotene.
Vitamin E
The main function of vitamin E in humans is as an antioxidant. Oxidation damages tissues when free radical ions (unpaired electron in an oxygen atom) are formed in your body. Free radical ions occur during normal function. They also develop when you are exposed to harmful factors like cigarette smoke or environmental pollutants. Other foreign chemicals such as food additives can also cause free radicals. Free radical ions will destroy your cell walls. Vitamin E, in the form of mixed tocopherols, is best suited to stop the damage caused by free radicals.
Vitamin E has been shown to improve immune system functions that decline as people age. It helps increase blood flow. It does this by preventing blood clots and relaxing blood vessel walls.
Some surgeons might worry that vitamin E will cause too much bleeding during surgery. The Food and Nutrition Board of the Institute of Medicine established a tolerable upper intake level (UL) for vitamin E supplements. The Food and Nutrition Board reviewed the research that’s been done. They published a statement that 1,000 mg/day of vitamin E would be the highest safe dose. The scientists at the Institute of Medicine have found that doses of vitamin E as high as 1,000 mg daily are unlikely to result in bleeding in almost all adults. 1,000 mg of vitamin E equals about 1,500 IU. Most supplements contain between 200 IU and 800 IU.
Some doctors advise patients to stop taking supplements with vitamin E before surgery. This will decrease the risk of excess blood loss. Other doctors want their patients to take vitamin E supplements for optimal recovery after surgery. They are comfortable with doses that are well within safe ranges. The usual recommendation is for not more than 400 IU daily.
Beta Carotene
Beta Carotene is converted to vitamin A in the liver as your body needs it. It is a powerful protector against infection. It is an antioxidant that supports your immune system. It also protects your vision. Beta-carotene protects the body from the irritating effects of smoke and other environmental pollutants. It promotes tissue healing. It may be helpful in preventing mouth and stomach ulcers.
Recently, studies showed that synthetic (man made) beta-carotene caused an increase in lung cancer in smokers. When natural beta-carotene was used, no increase in cancer was seen. Natural beta-carotene has been shown to have antioxidant activity that isn’t found in the synthetic form. The suggested dose of beta-carotene is 5 to 6 milligrams (10,000 IU) up to 15 mg (25,000 IU) per day.
Vitamin D
Vitamin D is a fat-soluble vitamin needed for normal calcium metabolism. You make vitamin D in your skin when you are in the sun without clothing or sunscreen shielding you. You can also get vitamin D from some foods.
Cells that are dividing rapidly are said to be proliferating. This is important for growth and wound healing. Vitamin D makes sure cell growth occurs properly.
Vitamin D regulates your immune system function during times of stress. Adequate vitamin D levels are important for decreasing the risk of high blood pressure.
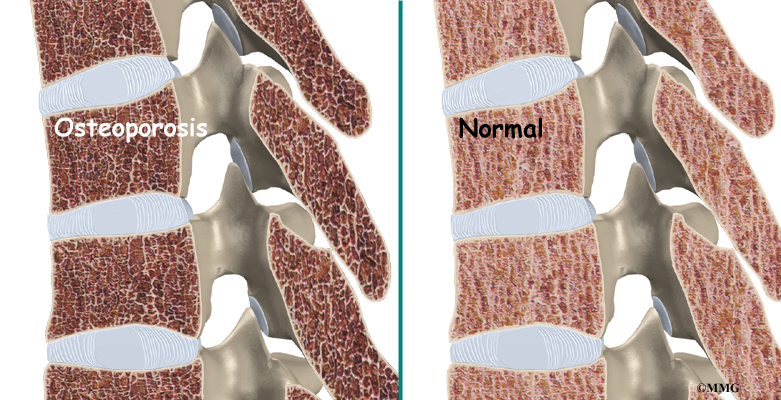
If you do not have enough vitamin D you will not absorb enough calcium. Then your body will steal calcium from your bones. This will increase your risk of osteoporosis and other health problems.
Vitamin D deficiency causes muscle weakness and pain. Taking 800 IU/day of vitamin D and 1,200 mg/day of calcium for three months will increase muscle strength. It can also decrease your risk of falling.
People with dark skin make less vitamin D on exposure to sunlight than those with light skin. The risk of vitamin D deficiency is high in dark-skinned people who live far from the equator. In the U.S., 42 percent of African American women between 15 and 49 years of age were vitamin D deficient compared to 4 percent of white women. The elderly are more likely to stay indoors or use sunscreen. This means they are less likely to make vitamin D in the skin.
Obesity increases the risk of vitamin D deficiency. Once vitamin D is made in the skin or ingested, it is deposited in body fat stores. Storage makes it less available especially to people with large amounts of body fat.
Osteoporosis has many different causes and not enough vitamin D is one of them. Without enough vitamin D, you will not absorb enough calcium. Decreased vitamin D may lead to bone fractures. In order for vitamin D supplementation to be effective in preserving bone health, it has to be taken along with 1,000 to 1,200 mg/day of calcium.
Medical researchers are discovering that vitamin D is more important, and less toxic than once thought. The importance of vitamin D is causing changes in what we consider a safe and healthy intake. Because sunlight exposure is so different for each one of us, it is impossible to decide on a Recommended Daily Allowance (RDA). Therefore, experts have decided to talk about adequate intake levels. They start by assuming that no vitamin D is being made in the skin. This is based on the idea that people simply do not get outside enough. They don’t get enough sunlight. When they do go outside, they tend to cover up with sunscreen. And they wear clothing that covers most of their body.
Multivitamin supplements for children generally provide 200 IU (5 mcg) of vitamin D. Multivitamin supplements for adults usually have 400 IU (10 mcg) of vitamin D. Single ingredient vitamin D supplements may provide 400-1,000 IU of vitamin D, but 400 IU is the most commonly available dose. A number of calcium supplements may also provide vitamin D.
Medical experts have set a vitamin D dose recommendation of 400 to 800 IU/day for children and adults (based on age). For example, infants up to one year should take 600 IUs of VitaminD daily. Children one year old and adults up to age 70 are advised to take 600 IUs. Adults over age 70 should bump the recommended daily allowance up to 800 IUs.
Research published since 1997 suggests that vitamin D toxicity is very unlikely in healthy people at intake levels lower than 10,000 IU/day. Some adults are advised to take higher dosages of vitamin D (up to 2000 IUs per day). You may need more if you have a history of malabsorption (e.g., celiac disease, inflammatory bowel disease, cystic fibrosis, gastric bypass surgery).
Monitoring for signs of vitamin D toxicity is recommended for anyone taking more than 4000 IUs per day. Signs of toxicity include gastrointestinal distress (e.g., nausea, vomiting, poor appetite), weakness, weight loss, increased urination, and heart palpitations. Vitamin D toxicity doesn’t result from sun exposure. Certain medical conditions can increase the risk of too much blood calcium in response to vitamin D. Check with your doctor to be sure you do not have a condition that increases your risk for too much blood calcium. This is important before you take more than 800 IU of vitamin D for a long time.
Iron
Iron is required for a number of vital functions, including growth, reproduction, healing, and immune function. You need the right amount of iron for hundreds of proteins and enzymes.
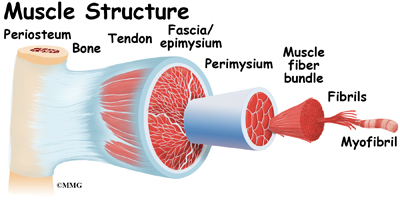
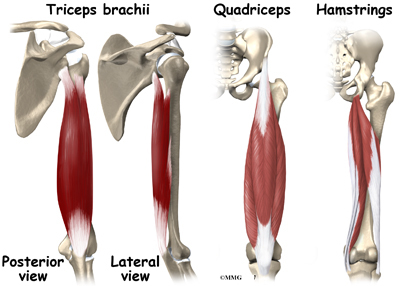
Heme is an iron-containing compound found in many biologically important molecules. Hemoglobin and myoglobin are heme-containing proteins. Hemoglobin has the vital role of carrying oxygen from your lungs to the rest of your body. Myoglobin is the molecule that supplies oxygen to your working muscles. These are needed for you to move and store your oxygen.
Cytochromes are heme-containing compounds that are needed for cellular energy production and therefore, to life. Cytochrome P450 is a family of enzymes that help make many important biological molecules. Cytochrome P450 helps your body use the drugs you need to take. It helps break down the pollutants you cannot avoid.
Copper
You must have enough copper in your system for normal iron metabolism and red blood cell formation. Anemia is a sign of copper deficiency. Copper is required for you to be able to move iron to your bone marrow for red blood cell formation.
Vitamin A deficiency will make iron deficiency anemia worse. Taking a combination of vitamin A and iron will protect you from anemia better than either iron or vitamin A alone.
A recent study in an elderly population found that high iron stores were much more common than iron deficiency. Do not take nutritional supplements containing iron unless you know for sure you are low in iron. This is important if you are older than 60. If you are in a low normal range, and you’re having surgery in which a lot of blood loss is likely, a brief period of supplementation prior to surgery is worth considering. The usual dose for supplementing iron is between 18 mg and 45 mg daily.
Calcium
Calcium is the most common mineral in the human body. About 99 percent of the calcium in your body is found in your bones and teeth. The other one percent is found in your blood and soft tissue. Calcium levels in your blood and body fluids must be kept within a very narrow range for normal physiologic functioning. The functions of calcium are so vital to survival that the body will steal calcium from your bones. It does this to keep blood calcium levels normal when your calcium intake is too low. Although this complex system allows for rapid and tight control of blood calcium levels, it does so by stealing from your skeleton.
Calcium plays many important roles. It is vital in controlling the constriction (closing) and relaxation (opening) of your blood vessels. It also aids proper nerve impulses, muscle contraction, and release of your hormones.
Calcium is necessary for optimal activity of many of your proteins and enzymes. The binding of calcium ions is required to cause your blood to clot when you are injured. Calcium is a key factor for good recovery from any surgery involving your bones.
Only about 30 percent of the calcium in your food is actually absorbed in your digestive tract. You lose a certain amount of calcium in your urine every day. This depends on how much caffeine you drink. Too much or not enough protein in your diet will affect your calcium absorption and the strength of your bones. Taking extra calcium makes sense when recovering from bone surgery as well as to prevent bone loss.
After adult height has been reached, the skeleton continues to build bone up to age 30. Adult men and women should consume a least 1,000 mg/day of calcium. This will make sure you make the best skeleton you can have, and limits how much bone you lose later in life.
To minimize bone loss, older men and postmenopausal women should consume a total of 1,200 mg/day of calcium. Taking a multivitamin/multimineral supplement containing at least 10 mcg (400) IU/day of vitamin D will help to make sure you absorb enough calcium.
Magnesium
Magnesium plays important roles in the structure and the function of the human body. Over 60 percent of all the magnesium in your body is found in your bones. About 27 percent is found in muscle, while six to seven percent is found in other cells. Magnesium is required by many other nutrients, like vitamin D and calcium, to function properly.
Your system requires magnesium to turn fats and carbohydrates into energy in your cells. Magnesium is needed to create nerve impulses, muscle contractions, and the normal rhythm of your heart.
Proper wound healing after surgery requires the right amounts of calcium and magnesium in the fluid around the cells involved in the injury.
Several studies have found that elderly people tend to have low dietary intakes of magnesium. Intestinal magnesium absorption tends to decrease in older adults, too. And the amount of magnesium lost through urine tends to increase in older people. If you are older than 50 years and are extra stressed by injury, disease, or surgery, supplementing magnesium intake is important to be sure you have the nutrition you’ll need to recover fully.
If you are having surgery that involves your bones, magnesium is very important for the best outcome. The usual recommended dose of magnesium is 400 to 600 mg daily.
Boron
Boron is a trace mineral that is found in highest amounts in fruits, vegetables, nuts, and legumes (peas, beans, and lentils). It is required for mineral metabolism, brain function, and performance. It also helps maintain testosterone and estrogen hormone levels. Boron is important for the prevention of osteoporosis. It does this by affecting mineral metabolism and hormones needed for bone formation.
Research indicates boron improves the uptake of calcium and magnesium into bone. A lack of adequate boron is linked with arthritic changes in joints. Taking boron can decrease joint swelling and pain. It can also increase the levels of helpful sex hormones in post-menopausal women and older men.
The best dose of boron for prevention of osteoporosis and proper tissue function appears to be between 3-6 mg/day
Strontium Citrate
Strontium citrate is recommended for enhancing bone building when you have been diagnosed with fracture-prone brittle bones. Strontium will slow bone weakening and increase new bone formation. You are likely to see major increases in bone mineral density and enjoy reduced risk of fracture. Strontium is a unique, safe, and effective natural aid for osteoporosis resulting from multiple causes.
Strontium is absorbed best when taken away from food and calcium supplements. It is not advised for pregnant women or for those with kidney disease. The usual dose recommended is about 225 mg of elemental strontium three times daily.
Zinc
Zinc is an essential trace element for all forms of life. Zinc deficiency has recently been recognized by a number of experts as an important public health issue. A diet very high in grains like wheat can cause zinc deficiency.
Nearly 100 different enzymes depend on zinc to complete chemical reactions. Almost all of your tissues use enzymes that require zinc.
You must have enough zinc to keep your immune system healthy. If you don’t have enough zinc, you are more likely to become ill from a number of different infectious bacteria or viruses.
If you are taking iron pills, you may not absorb zinc as well as you should. This may occur if you are taking iron before surgery for your red blood cells. If this applies to you, you should take some extra zinc.
Copper assists in the formation of hemoglobin and red blood cells by increasing iron absorption. It is needed for protein metabolism, cell reproduction, and to make healthy nerve cells. Zinc and copper need to be in proper amounts to each other for each to work well. The recommended ratio of zinc to copper for best function is approximately 8:1, or zinc 30 mg and copper 4 mg.
Manganese
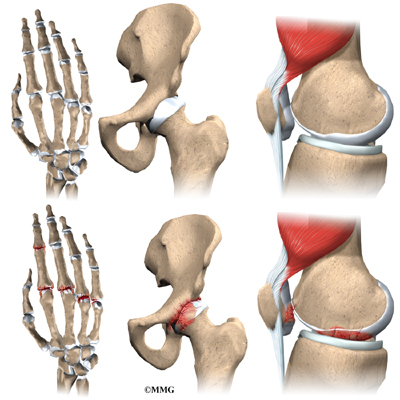
Manganese is a mineral element that is nutritionally essential especially for bone and joint strength.
It is part of the main antioxidant enzymes that work in your cells. Not enough manganese will cause abnormal skeletal development. Manganese is needed for the formation of healthy cartilage and bone.
It is also needed for healing after surgery. Wound healing is a complex process that requires increased production of collagen. Manganese is required for collagen formation in human skin cells.
If you are taking calcium, magnesium, or iron pills, you may not absorb manganese as well as you should. In certain situations, you may need to take some extra manganese. For instance, if you are supplementing with iron before surgery to increase your red blood cells, you may want to boost your manganese intake as well.
Women with osteoporosis have been found to have decreased blood levels of manganese. This improves when they take manganese supplements. A study in healthy postmenopausal women found that a supplement containing manganese (5 mg/day), copper (2.5 mg/day), and zinc (15 mg/day) in combination with a calcium supplement (1,000 mg/day) was more effective in preventing spinal bone loss than the calcium supplement alone.
Two recent studies have found that supplements with glucosamine, chondroitin sulfate, and manganese together will help to relieve pain due to mild or moderate osteoarthritis of the knee.
The usual recommended dose of manganese for adult women and men is between 5 and 10 mg daily.
Selenium
Selenium is a trace element that is essential in small amounts to the work of many other nutrients. This includes vitamin C, vitamin E, copper, zinc, and iron. It aids wound healing by regulating cell growth.
Your thyroid gland needs selenium for normal function. Thyroid hormone tells your body how fast to function. If your cells work too slowly, your healing from wounds and your daily tissue repair will not go well.
People who are low in selenium may be more likely to become ill when stressed by difficult events like surgery or exposure to bacteria and viruses. Taking selenium can improve the immune response even in people who have no symptoms of selenium deficiency.
Studies have shown over and over that people who live in areas with low soil selenium and low selenium in their food will have more death from cancer, especially cancer in men.
The usual recommendation for selenium supplementation is 400 mcg/day.
Chromium (polynicotinate)
Chromium (polynicotinate) is a nutritionally essential mineral. It acts to support your blood sugar and insulin functions. It also helps with your fat and protein metabolism. Normal insulin function is required to provide cellular energy and to prevent diabetes.
If you have kidney or liver disease, you may have problems with side effects from too much chromium. You should limit supplemental chromium intake to not more than 50 mcg daily.
Lysine
Lysine is an essential amino acid. It improves how well you absorb calcium and limits how much you lose through your kidneys. Lysine also contributes to strengthening bone.
There have been some reported cases in animal studies that high dose lysine may cause gallstones and increased cholesterol levels. Doses up to 1000 mg three times daily are commonly used for people who need extra lysine.